Abstract
Parent-adolescent relationship quality and affective functioning have been implicated in eating disorder development. This study examined whether maternal and paternal hostility interact to explain adolescents’ eating disorder symptoms and whether parental hostility effects are more pronounced among adolescents with high emotional reactivity. A sample of 699 adolescents, ages 11–12 years, reported their parents’ hostility and their own eating disorder symptoms, and parents reported adolescents’ emotional reactivity. Results from structural equation modeling indicated that for emotionally reactive adolescents, paternal hostility was positively associated with eating disorder symptoms at both high and low levels of maternal hostility. In addition, eating disorder symptoms were amplified when both parents were high in hostility. Findings from this study lend support for the role of emotional reactivity in the link between parent hostility and eating disorder symptoms during adolescence.
Early adolescence represents an important developmental stage for eating disorder research, as it is the time frame during which problematic patterns of thinking and behavior related to eating and body size tend to emerge (Lam & McHale, 2012; McKnight Investigators, 2003; Sancho, Arija, Asorey, & Canals, 2007; Striegel-Moore & Bulik, 2007). Proposed risk factors for eating pathology include biological (e.g., genetic vulnerability), cultural (e.g., thin ideal internalization), social (e.g., family functioning, peer weight related teasing) and psychological factors (e.g., affective disturbances, weight concerns; Haworth-Hoeppner, 2000; Jacobi, Hayward, de Zwaan, Kraemer, & Agras, 2004; Keel & Forney, 2012; Striegel-Moore & Bulik, 2007; Wade, Bulik, & Kendler, 2001). Identifying the mechanisms by which modifiable risk factors for eating disorders operate may inform prevention and early intervention efforts. Eating disorders may develop via multiple pathways, and pathways may be characterized by interactions between multiple risk factors (Jacobi et al., 2004; Levine & Smolak, 1992). Thus, a transactional model that addresses interactions between risk factors may best illuminate the development of eating disorders (Rosen, 1996). Little research, however, has explored how risk factors within families and individual characteristics such as affective functioning may interact to influence development of eating disorder symptoms. The current study focuses on parent-adolescent relationship quality, specifically perceived paternal and maternal hostility, and adolescent emotional reactivity, and explores whether and how interactions between them explain disordered eating symptoms among early adolescents.
Parent-Adolescent Relationship Quality
The quality of adolescents’ family relationships may influence adolescents’ body image concerns and disordered eating. Lam and McHale (2012) found that adolescents with lower levels of maternal acceptance and higher levels of paternal conflict than usual reported increased weight concerns the following year. Among monozygotic twins, women with anorexia nervosa or bulimia nervosa retrospectively report more parental conflict and criticism than their unaffected twin (Wade, Gillespie, & Martin, 2007). Patients with eating disorders characterize their family environments as highly critical toward them, and their relationship with their parents as lacking in affection, love, and acceptance (Haworth-Hoeppner, 2000). High expressed emotion within the family, characterized by family members’ criticism, hostility, and emotional intrusiveness, is associated with greater eating disorder pathology and predicts worse eating disorder recovery outcomes (Butzlaff & Hooley, 1998; Hedlund, Fichter, Quadflieg, & Brandl, 2003). In contrast, adolescents who perceive their family environments as warm, trusting, close, fun, and less conflictual are less likely to exhibit disordered eating symptoms (Cance, Loukas, & Talley, 2015). Despite the majority of research considering negative family dynamics as a risk factor for disordered eating (e.g., Jacobi et al., 2004), limited research indicates that adolescents’ disordered eating may predict increased parent-adolescent conflict. Spanos and colleagues found that among monozygotic twins, the twin with disordered eating reported more conflict with their parents than the unaffected twin (Spanos, Klump, Burt, McGue, & Iacono, 2010). However, this association was significant in mid adolescence, and not early adolescence, and thus may reflect a developmental difference in the direction of effect between early and mid adolescence (Spanos et al., 2010).
Although most research has either examined the influence of mothers in the development of eating disorders or averaged mothers’ and fathers’ influence, emerging evidence suggests that the effects of negative parent-adolescent relationships may differ according to parent gender. For example, greater mother-adolescent conflict predicted increased weight concerns for adolescent girls, but not boys, whereas greater father-adolescent conflict predicted increased weight concerns for both adolescent girls and boys (May, Kim, McHale, & Crouter, 2006). These results suggest that paternal conflict may have a broader effect on adolescent weight concerns than maternal conflict. It may be that although mothers tend to be more involved in childrearing activities than fathers, fathers become involved in serious parenting issues (e.g., intervening in adolescent risky behaviors), which may be characterized by increased conflict and negative affect (May et al., 2006). This idea is consistent with other research that has found paternal lack of affection is associated with disordered eating or weight problems during adolescence or early adulthood, even after controlling for childhood eating issues (Johnson, Cohen, Kasen, & Brook, 2002). Indeed, a recent meta-analysis concluded that father-child conflict has a greater impact on disordered eating than mother-child conflict (Gale, Cluett, & Laver-Bradbury, 2013). To date, little research has examined the relative contributions of maternal and paternal hostility to disordered eating during early adolescence within a single model. To establish a comprehensive understanding of how parent-child relationship quality influences eating disorder development, it is important to examine how the dynamic between both parents and the adolescent is associated with eating disorder symptoms.
Emotional Reactivity and Disordered Eating Pathology
Another important area of inquiry for understanding eating disorder development is adolescents’ affective functioning. Difficulties with emotion regulation are thought to underlie eating disorders; evidence suggests that patients with eating disorders exhibit elevated emotion regulation difficulties, and those with bulimia nervosa and binge eating disorder, may engage in disordered eating behaviors as a maladaptive coping strategy for negative emotions (Brockmeyer et al., 2014; Fairburn, Cooper, & Shafran, 2003; Harrison, Sullivan, Tchanturia, & Treasure, 2010; Polivy & Herman, 2002; Stice, Shaw, & Nemeroff, 1998). Although emotion regulation has been studied extensively in relation to eating disorders (Polivy & Herman, 2002; Stice et al., 1998), relatively little research has investigated whether the observed mismatch in coping resources and environmental demands may in part be due to elevated emotional reactivity (Fairburn et al., 2003). However, an exploratory study found that adolescents with eating disorders exhibited elevated emotional reactivity compared to their peers (Nock, Wedig, Holmberg, & Hooley, 2008). In addition, a recent model suggests that emotional reactivity may have a key role in disordered eating behaviors. According to Haynos and Fruzetti’s model (Haynos & Fruzzetti, 2011), there are transactional effects between emotional vulnerabilities (e.g., emotional reactivity), social environment (e.g., feedback from others), and physical state (e.g., weight loss). According to this model, for individuals with elevated emotional reactivity and a history of invalidating feedback from others, negative events lead to heightened emotional arousal and negative affect, which these individuals then attempt to mitigate through disordered eating (Haynos & Fruzzetti, 2011). Components of the model feed into each other so that the cycle perpetuates. This model acknowledges that multiple emotional (e.g., reactivity and regulation) and contextual (e.g., parenting styles) factors work in transactional relations to produce and maintain disordered eating behaviors, and emphasizes the contributing role of emotional reactivity to disordered eating (Haynos & Fruzzetti, 2011). The theorized interaction between affective and contextual factors may be applied to understand subclinical disordered eating behaviors that emerge in adolescence.
The Link between Family Environment and Adolescent Emotional Reactivity
The link between parent hostility and adolescent emotional reactivity in the development of eating disorders may be best understood by examining the development of emotion regulation within family contexts. Previous research indicates that family climate and parenting styles are key factors that shape adolescent emotional reactivity and emotion regulation skills. Children who grow up in family climates characterized by negative emotions are more likely to exhibit elevated emotional reactivity and poor emotion regulation skills because their parents model emotion dysregulation and such environments lead to emotional insecurity among children (Morris, Silk, Steinberg, Myers, & Robinson, 2007). In addition, negative parenting styles, including parent hostility, criticism, dismissiveness, and punitiveness, have been linked to heightened negative affect and emotion regulation deficits among children (Morris et al., 2007; Thompson & Meyer, 2007). Taken together, these findings suggest that family context contributes to children’s emotional reactivity and regulation. Given the previously established link between parent-adolescent relationship quality and eating disorder symptoms and preliminary findings linking emotional reactivity with eating disorder symptoms, the logical next step is to examine how these factors may interact to jointly contribute to the development of eating disorders.
The Current Study
The primary objective of this study was to advance understanding of the complex interplay of paternal and maternal hostility, adolescent emotional reactivity, and eating disorder symptoms in early adolescence. Prior research has implicated the quality of parent-child relationships in disordered eating and affective functioning and suggests a link between affective functioning and eating disorders. However, there is limited research on the link between emotional reactivity and eating disorder symptoms, and no study to date has examined whether parent-child relationship quality and emotional reactivity interact to contribute to eating disorder symptoms. Elucidating the links between these factors is a necessary first step toward clarifying the role of emotional reactivity in the development of eating disorders and refining current models of eating disorder development. Furthermore, improving the accuracy of these models will enhance the design and in turn, effectiveness of eating disorder prevention programs. As there is a paucity of research examining the influence of both fathers and mothers on the development of eating disorders, we examined the main effects of father-adolescent relationships and mother-adolescent relationships as well as their interaction effects simultaneously in the same model. We predicted that a) the source of parent hostility would differentially affect the presence of eating disorder symptoms among adolescents, such that paternal hostility would have a more potent effect than maternal hostility, b) eating disorder symptoms would be amplified when both parents’ hostility levels were high, and c) adolescent emotional reactivity would moderate the association between paternal and maternal hostility and eating disorder symptoms.
Method
Participants
Participants included 699 adolescents, ages 11–12 (50.2% female) sourced from the public dataset produced by NICHD Study of Early Child Care and Youth Development (SECCYD), a large, multi-site, four-phase longitudinal study of healthy development. Phase I began in 1991 and Phase IV concluded in 2007. All data used in the current study was derived from 6th grade assessments collected during Phase III. Parent ethnicity was predominantly European American (65.2% of fathers and 68.1% of mothers), followed by African American (5.4% of fathers and 5.2% of mothers), Hispanic/Latino (3.6% of fathers and 4.3% of mothers), Asian American (2.0% of fathers and 2.3% of mothers), and other (2.1% of fathers and 4.1% of mothers), with 21% of fathers and 16% of mothers not reporting ethnicity. Mean annual family income fell in the range of $60,000–80,000 at the time of the 6th grade assessment. Mean educational attainment for mothers and fathers was greater than a bachelor’s degree. A total of 25 participants were excluded because they were missing data on the outcome variables. Not all participants completed all other measures, so full information maximum likelihood structural analyses were used.
Procedures
Data were collected via interview at participants’ homes and laboratory playrooms. All study procedures were approved by participating universities’ institutional review boards and participants provided informed consent/assent. Additional information on the SECCYD dataset and study procedures may be found at: https://www.nichd.nih.gov/research/supported/seccyd/Pages/overview.aspx#instruments (National Institutes of Health, 2012).
Measures
Eating Disorder Symptoms.
Twelve items from the Child’s Eating Habits and Body Self-Image scale (Harter, 1988) measuring body image concerns and weight control behaviors were used to create a latent variable of eating disorder symptoms. Weight control behaviors (α = .51) included six items (e.g., “During the past month, which of the following did you do: vomit to lose weight or to keep from gaining weight?”) rated on a 4-point scale ranging from 0 (Not at all) to 3 (Almost every day). Body image concerns were assessed using six items from the Index of Physical Self Image subscale (e.g., “How happy are you about the way you look?”) measuring body image satisfaction (α = .91), rated on a 4-point Likert scale from 1 (Very unhappy) to 4 (Very happy). Higher scores on both scales indicate greater pathology, and the physical self image and weight control behavior scales were significantly correlated (r = .23, p < .001).
Parent Hostility.
Adolescents used the Parental Hostility subscale of the Parental Warmth Report (Conger et al., 2002; Conger & Ge, 1999) to rate eight items (e.g., “When you and your [mother/father] spend time talking or doing things together, how often does your [mother/father] criticize you or your ideas?”) rated on a 4-point scale from 1(Never) to 4 (Always). Ratings were summed, with higher scores representing greater parental hostility (α = .73 and α = .80 for ratings of mother and father respectively).
Adolescent Emotional Reactivity.
Mothers and fathers used the parent report of Children’s Reactions scale (Shields & Cicchetti, 1997) to rate 19 items (e.g., “When my child feels an emotion, either positive or negative, my child feels it strongly”) on 4-point scales from 1 (Not at all/Never) to 4 (A lot/Always). Higher scores indicate greater adolescent emotional reactivity (α = .79 and α = .73 for mother and father reports respectively). Mother and father ratings of adolescent emotional reactivity were averaged to create a composite score (r = .41, p < .001).
Data Analytic Plan
Descriptive analyses were conducted to determine normality of distributions and univariate and multivariate outliers for all study variables. Based on Kline’s guidelines (Kline, 2011), skewness and kurtosis were acceptable for all variable distributions. In addition, we tested whether demographic variables were significantly linked to the predictor variables and based on this analyses, included adolescent sex and family income as covariates in the analytic models. To address our research goals, we estimated a two group moderation structural equation model in AMOS version 23. Overall model fit indices included χ2 value, degrees of freedom, corresponding p value, root mean square error of approximation (RMSEA), and Confirmatory Fit Index (CFI). An RMSEA value less than .06 and a CFI value equal to or greater than .95 were considered a good fit (Hu & Bentler, 1999). A series of models were tested comparing low and high emotional reactivity groups to determine the moderating effects of emotional reactivity in the link between maternal and paternal hostility and eating disorder symptoms. Based on computational instruments designed by Preacher and Coffman (2006), our sample size allowed for sufficient power (.80) to test a covariance structure using RMSEA (MacCallum, Browne, & Sugawara, 1996).
We formed low emotional reactivity (below median of the emotional reactivity scores, n = 369) versus high emotional reactivity (above median, n = 330) groups using a median split, based on each individual’s emotional reactivity composites averaged between maternal and paternal reports. The low/high emotional reactivity groups were formed for testing moderating effects of quantitative differences in emotional reactivity using a multiple group SEM; they may not represent clinically meaningful or qualitatively different sub-groups. These two groups differed significantly on the outcome, eating disorder symptoms, t(696) = −3.40, p = .001. A Configural Invariance model was fit first in which all parameters were freely estimated across the two groups and used in comparisons to the subsequent models. In subsequent models, we imposed equality constraints hierarchically to test invariance between the low and high emotional reactivity groups with respect to the effect of maternal hostility on eating disorder symptoms (Equal Direct Mother Hostility), the effect of paternal hostility on eating disorder symptoms (Equal Direct Father Hostility), and the effect of the interaction term on eating disorder symptoms (Equal Interaction). Significant interactions were probed by testing the significance of the simple slopes at both high (1 SD above the mean) and low (1 SD below the mean) values of the predictors (Preacher, Curran, & Bauer, 2006).
Results
Descriptive statistics and correlations for all study variables appear in Table 1. Twenty-four cases were identified as multivariate outliers due to significant Mahalanobis distances (p < .001); however, the pattern of results did not change with and without the identified cases. Therefore, these outliers were included. Multivariate GLM analyses with potential demographic covariates (age, adolescent sex, ethnicity, and family income) predicting the eating disorder symptoms outcome revealed adolescent sex (p = .03) and family income (p = .02) were significant predictors of eating disorder symptoms, whereas age was not (p = .83). Thus, adolescent sex and family income were included as covariates in the analysis.
Table 1.
Descriptive Statistics and Correlations for Parent Hostility, Emotional Reactivity, Weight Control Behaviors, and Perception of Self-Image among Early Adolescents.
| PH_M | PH_F | ER | WCB | PSI | Sex | Income | M | SD | Range | |
|---|---|---|---|---|---|---|---|---|---|---|
| PH_M | --- | 1.43 | .32 | 1.00–3.50 | ||||||
| PH_F | .58*** | --- | 1.38 | .35 | 1.00–3.75 | |||||
| ER | .08* | .10* | --- | 3.28 | .46 | 1.90–4.60 | ||||
| WCB | .12** | .12** | .09* | --- | .63 | .44 | .00–2.40 | |||
| PSI | .22*** | .27*** | .10** | .23** | --- | −3.44 | .59 | −4.00–1.00 | ||
| Sex | −.00 | −.06 | .13** | .03 | .08* | --- | --- | --- | --- | |
| Income | −.15** | −.11** | −.12** | −.12** | −.04 | .01 | --- | 12.59 | 4.14 | 1.00–23.00 |
Note. PH_M = Parent Hostility mother report; PH_F = Parent Hostility father report; ER = Emotional Reactivity (averaged mother and father reports); WCB = Weight Control Behaviors; PSI = Perception of Self Image; Sex = Adolescent Sex; Income = Annual Household Income before Taxes.
p < .05
p < .01
p < .001
To test the two group moderation model, a series of nested models were estimated and model fit comparisons are shown in Table 2. For the first model (Configural Invariance Model) including the direct effect of parental hostility on eating disorder symptoms, model fit was good. Then, we imposed an equality constraint between the low and high emotional reactivity groups with respect to the direct effect of mother hostility on eating disorder symptoms (Equal Direct Mother Hostility). Model fit was good, and adding an equality constraint did not significantly degrade the model fit. Next, we added an equality constraint between the low and high emotional reactivity groups with respect to the direct effect of father hostility on eating disorder symptoms (Equal Direct Father Hostility). Model fit was good, and adding an equality constraint did not significantly degrade the model fit. Finally, we imposed an equality constraint between the low and high emotional reactivity groups (Equal Interaction) with respect to the effect of the interaction of mother and father hostility on eating disorder symptoms. Model fit was good, however the imposed equality constraint significantly degraded the model fit. Therefore, the Equal Direct Father Hostility model was considered the best-fitting model.
Table 2.
Comparisons of Two-Group Nested Models for Emotional Reactivity, Mother Hostility, Father Hostility, and Eating Disorder Symptoms.
| Model | χ2 | df | p | CFI | RMSEA | p(close) | Δχ2 | Δ df | p(d) |
|---|---|---|---|---|---|---|---|---|---|
| 1. Configural invariance | 9.88 | 10 | .45 | 1.00 | .00 | .99 | |||
| 2. Equal direct mother hostility | 10.77 | 11 | .46 | 1.00 | .00 | .99 | .89 | 1 | .35 |
| 3. Equal direct father hostility | 10.84 | 12 | .54 | 1.00 | .00 | 1.00 | .07 | 1 | .79 |
| 4. Equal interaction | 20.93 | 13 | .07 | .99 | .03 | .93 | 10.09 | 1 | .001 |
Note. CFI = comparative fit index; RMSEA = root mean square error of approximation; p(close) = probability of a close fit to the data; Δχ2 = difference in likelihood ratio tests; Δ df = difference in df; p(d) = probability of the difference tests. Best fitting model is in bold.
Standardized estimates for the best-fitting model are shown in Figure 1. For both the low and high emotional reactivity groups, higher maternal hostility was significantly associated with higher eating disorder symptoms, b = .39, SE = .14, p = .01, as was higher paternal hostility, b = .66, SE = .13, p < .001. A significant interaction emerged for mother and father hostility in relation to eating disorder symptoms for the high emotional reactivity group, b = −.56, SE = .27, p = .04, but not for the low emotional reactivity group, b = −.45, SE = .29, p = .12. The simple effect slopes for the high emotional reactivity group are presented in Figure 2. The interaction revealed that within the high emotional reactivity group, higher paternal hostility was associated with elevated eating disorder symptoms in the context of both high, b = .14, p = .04, and low, b = .31, p = .001, levels of maternal hostility, and the magnitude of the association between paternal hostility and eating disorder symptoms was greater among adolescents with low maternal hostility than those with high maternal hostility. In addition, adolescents with both high maternal and paternal hostility exhibited the highest levels of eating disorder symptoms.
Figure 1. Two-group moderation model to test the effect of parent hostility on eating disorder symptoms.
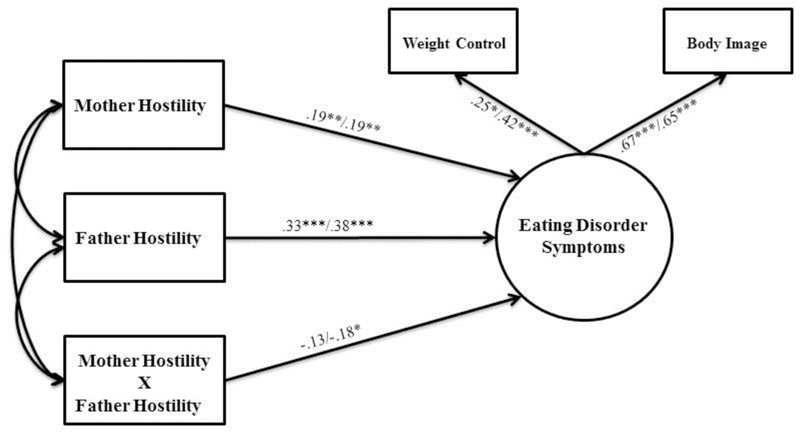
Note.Standardized parameter estimates are presented; first estimates are for the low emotional reactivity group and second for the high emotional reactivity group. Covariances for parent hostility were as follows: mother hostility ↔ father hostility = .07(.01), p <.001; mother hostility ↔ mother X father hostility = .04(.01), p <.001; father hostility ↔ mother X father hostility = .05(.01), p <.001. Coefficients for the sex and income covariates are not shown for the purpose of clarity: sex ↔ mother hostility = −.002(.01), p = .77/−.001(.01), p = .95; sex ↔ father hostility = −.01(.01), p = .48/−.02(.01), p = .10; sex ↔ mother X father hostility = .004(.01), p = .38/−.01(.01), p = .15; income ↔ mother hostility = −.21 (.07), p = .001/−.17 (.08), p = .03; income ↔ father hostility = −.09(.07), p = .20/−.20(.09), p = .03; income ↔ mother X father hostility = −.04(.04), p = .27/−.10(.05), p = .05; sex → eating disorder symptoms = .11, p = .16; income → eating disorder symptoms = −.06, p = 48.
* p < .05; ** p < .01, *** p < .001
Figure 2.
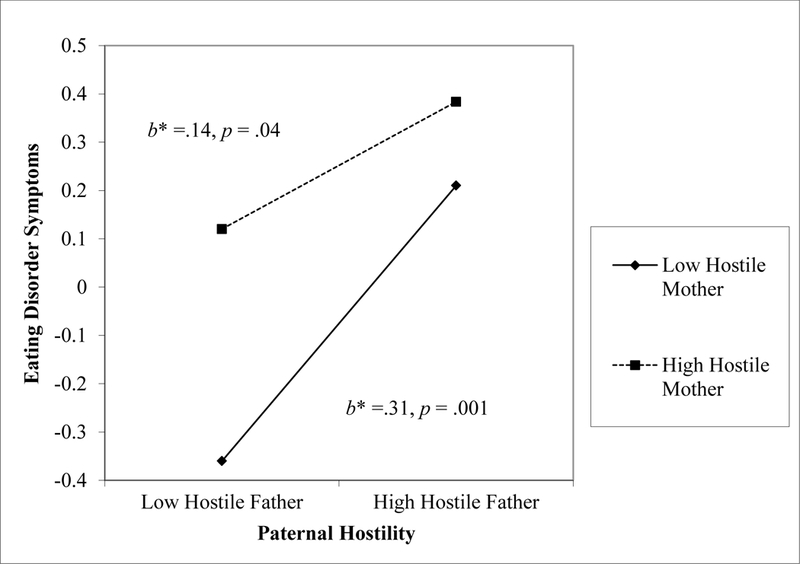
Interaction for maternal and paternal hostility contributing to eating disorder symptoms within the high emotional reactivity group
To rule out alternative explanations for our findings, we tested for possible differences in variances and mean levels of maternal and paternal hostility in the high versus the low reactivity groups. Levene’s homogeneity of variance test statistic was statistically significant for fathers (F(1, 697) = 6.45, p = .01; M = 1.34, SD = .31 in the low reactivity group, M = 1.42, SD = .39 in the high reactivity group) but not mothers (F(1, 697) = .90, p = .34; M = 1.40, SD = .30 in the low reactivity group, M = 1.46, SD = .34 in the high reactivity group), which suggests that there were unequal variances in father hostility and equal variances in mother hostility between the high and low reactivity groups. The greater variability in father hostility within the high reactivity group compared to the low reactivity group may have contributed to the significant interaction effect detected in the high but not low reactivity group. However, a paired t-test examining mean differences in maternal and paternal hostility revealed that mothers (M = 1.43, SD = .32) were significantly more hostile than fathers (M = 1.38, SD = .35; t(698) = 4.16, p < .001), thus eliminating the possibility that the seemingly stronger effects of paternal hostility are due to the fact that fathers showed greater hostility than mothers did.
Discussion
This study examined the complex interplay of emotional reactivity and both paternal and maternal hostility and how they are associated with eating disorder symptoms in early adolescence. Prior research has implicated poor parent-adolescent relationship quality as a predictor of disordered eating in healthy and clinical samples and limited research has linked high emotional reactivity with disordered eating in clinical samples. However, this is the first study to test how the interaction between both maternal and paternal hostility with adolescent emotional reactivity is associated with eating disorder symptoms among adolescents. Our results confirm the hypothesized yet understudied role of emotional reactivity in eating disorder symptoms (Nock et al., 2008), suggesting that emotional reactivity merits further investigation as a risk factor for eating disorders. Our results further show that both maternal and paternal hostility are associated with eating disorder symptoms for adolescents regardless of the level of emotional reactivity. Findings regarding the interaction between maternal and paternal hostility were consistent with our hypothesis that emotional reactivity moderates the association between parent hostility and disordered eating symptoms. Specifically, adolescents high in emotional reactivity who perceived both parents to be hostile towards them were more likely to exhibit disordered eating attitudes and behaviors.
Results from this study support the use of a transactional model to understand eating disorder symptoms in adolescence. Indeed, as a transactional model of development might predict, the association between parent hostility and eating disorder symptoms was moderated by an individual characteristic, emotional reactivity. Although we did not directly test Haynos and Fruzetti’s emotion dysregulation model of anorexia nervosa (Haynos & Fruzzetti, 2011), our findings from a subclinical adolescent sample are consistent with this particular transactional model. It seems reasonable to conclude that early adolescents with high emotional reactivity may engage in disordered eating behaviors as a maladaptive method of coping with negative emotions. Adolescents who experience higher levels of hostility from their parents likely experience negative emotions more frequently than their peers with warm parents and are also at higher risk for elevated emotional reactivity (Morris et al., 2007). Consequently, the combination of parental hostility and high emotional reactivity may lead to greater disordered eating symptoms. These results represent an important advance in the conceptualization of eating disorder development and in understanding the effects that negative parenting styles may have on adolescent emotional reactivity and psychological and physical health outcomes.
Findings from the current study also help elucidate the differential association between maternal and paternal hostility and eating disorder symptoms during early adolescence. Our results revealed that both maternal hostility and paternal hostility were independently linked to elevated eating disorder symptoms for adolescents with low emotional reactivity. For adolescents with high emotional reactivity, those with high maternal and paternal hostility exhibited the most eating disorder symptoms. However, paternal hostility was positively associated with eating disorder symptoms at both high and low levels of maternal hostility. This finding supports our hypothesis that the source of parent hostility is differentially associated with eating disorder symptoms, and paternal hostility has a particularly potent effect on eating disorder symptoms during early adolescence. This conclusion is strengthened by the finding that adolescents perceived mothers as significantly more hostile than fathers. However, it is important to note that although there was a statistically significant difference in maternal and paternal hostility, the difference in effect size was small (d = .15). Therefore, this difference may not be clinically meaningful, and our findings represent preliminary evidence and warrant replication. It is possible that the differential effects of paternal and maternal hostility on disordered eating behaviors may be traced back to differences in the types of parenting behaviors that mothers and fathers engage in, as suggested by May and colleagues (May et al., 2006), or differences in the meanings that adolescents ascribe to mothers’ and fathers’ hostility.
Interestingly, the association between paternal hostility and eating disorder symptoms was stronger at low levels of maternal hostility. The difference in the strength of association between paternal hostility and eating disorder symptoms across levels of maternal hostility may be due to increases in paternal hostility having greater salience for adolescents with low maternal hostility compared to adolescents with high maternal hostility. This finding underscores the importance of examining how characteristics of both mother-adolescent and father-adolescent relationships are associated with disordered eating and body image concerns.
The finding that father hostility had unequal variance across low and high emotional reactivity groups may explain, in part, why we detected an interaction within the high reactivity group but not the low reactivity group. The greater variability in hostility among fathers with highly reactive adolescents is consistent with literature suggesting that there is greater variability in the parenting roles that fathers assume compared to mothers; their relatively less scripted roles as parents means that there is more room for variation in the ways that fathers interact with difficult children (McBride, Schoppe, & Rane, 2002). Thus, this difference in variability reflects gendered differences in parenting behaviors.
Overall, our findings were consistent with previous work that suggests fathers may have a differential impact on adolescent disordered eating and body image concerns than mothers (Gale et al., 2013; Johnson et al., 2002; May et al., 2006). Our results are notable because the roles fathers have in promoting and maintaining body image concerns and disordered eating have traditionally been understudied. By neglecting to include fathers in research on family influences, we may overlook key factors that influence the development and onset of risk factors for eating disorders in early adolescence. Future research should further clarify how paternal and maternal hostility may operate differentially to impact eating disorder symptoms among adolescents.
The current study has several limitations. We were restricted to a cross-sectional design and could not follow participants’ development longitudinally because measures of the variables of interest were not administered together on multiple years of the SECCYD study. Thus, we cannot draw causal conclusions about the links between parent hostility, emotional reactivity, and disordered eating symptoms. Indeed, there may be a bidirectional relation between parent-adolescent relationship quality and eating disorder symptoms, such that adolescents who perceive hostility from their parents may experience negative affect, and in turn exhibit eating disorder symptoms, and parents, perhaps out of concern and frustration, may respond to their adolescents’ disordered eating behaviors in a manner adolescents construe as hostile. Similarly, there may be reciprocal effects between adolescents’ emotional reactivity and parents’ hostility. Another limitation was that our sample was also predominantly Caucasian, well-educated, and middle class, therefore our findings may not be generalizable to other more ethnically and socioeconomically diverse populations. Thus, replication using longitudinal designs in diverse populations is warranted. Our study focuses on early adolescence as it represents a key developmental period for the emergence of body image concerns and disordered eating; however, it will be crucial for future research to examine whether the relations among hostility, emotional reactivity, and disordered eating changes across development to inform the development of age-appropriate intervention programs. For example, family environment may lose salience relative to peer influences during late adolescence and emerging adulthood (Ata, Ludden, & Lally, 2007). As such, it will also be important to consider the contribution of hostility within peer networks and romantic relationships at later stages of development.
Despite these limitations, this study represents an important advance in research on parent-youth relationships and eating disorder symptoms in early adolescence. We demonstrate that the association between paternal and maternal hostility and eating disorder symptoms varies depending on adolescent emotional reactivity, which lends support for a transactional model of eating disorder development. These findings may help inform prevention programs aimed at reducing disordered eating among early adolescents; such programs could target parent-adolescent relationship quality and consider adolescents’ emotional reactivity. For example, mindfulness interventions reduce emotional reactivity and aid in treatment of eating disorders (Wanden-Berghe, Sanz-Valero, & Wanden-Berghe, 2010). Thus, including mindfulness training in eating disorder prevention programs may be particularly useful for adolescents with high emotional reactivity. In addition, there are empirically supported school-based family intervention programs that reduce psychopathology by augmenting parent-adolescent relationship quality (e.g., The Adolescent Transitions Program; Connell & Dishion, 2008). It may be beneficial to integrate key components from mindfulness and family-centered intervention programs with current best practices in eating disorder prevention (see Stice, Shaw, & Marti, 2007 for a review). Improving the efficacy of prevention programs by targeting multiple interacting risk factors for eating disorders may mitigate the incidence of disordered eating and body image concerns in early adolescence and lead to a lower prevalence of clinically diagnosable eating disorders in later years.
Acknowledgments:
This work was supported by NIH funding (DA036017). We are grateful to the SECCYD study participants and research staff. The Study of Early Child Care and Youth Development was conducted by the NICHD Early Child Care Research Network, and was supported by NICHD through a cooperative agreement that calls for scientific collaboration between the grantees and the NICHD staff. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Child Health and Human Development or the National Institutes of Health. We thank Susan McHale for providing editorial assistance.
Footnotes
The authors have no conflicts of interest to report.
References
- Ata RN, Ludden AB, & Lally MM (2007). The effects of gender and family, friend, and media influences on eating behaviors and body image during adolescence. Journal of Youth and Adolescence, 36, 1024–1037. doi: 10.1007/s10964-006-9159-x [DOI] [Google Scholar]
- Brockmeyer T, Skunde M, Wu M, Bresslein E, Rudofsky G, Herzog W, & Friederich HC (2014). Difficulties in emotion regulation across the spectrum of eating disorders. Comprehensive Psychiatry, 55, 565–571. doi: 10.1016/j.comppsych.2013.12.001 [DOI] [PubMed] [Google Scholar]
- Butzlaff RL, & Hooley JM (1998). Expressed emotion and psychiatric relapse: A meta-analysis. Archives of general psychiatry, 55, 547–552. doi: 10.1001/archpsyc.55.6.547 [DOI] [PubMed] [Google Scholar]
- Cance JD, Loukas A, & Talley AE (2015). The differential associations of internalizing symptoms and family and school relationships with disordered eating attitudes among early adolescents. Journal of Social and Personal Relationships, 32, 41–56. doi: 10.1177/0265407514523551 [DOI] [Google Scholar]
- Conger RD, & Ge X (1999). Conflict and cohesion in parent-adolescent relations: Changes in emotional expression from early to mid-adolescence In Cox M & Brooks-Gunn J (Eds.), Conflict and cohesion in families: Causes and consequences (pp. 185–206). Mahwah: Erlbaum. [Google Scholar]
- Conger RD, Wallace LE, Sun Y, Simons RL, McLoyd VC, & Brody GH (2002). Economic pressure in African American families: A replication and extension of the family stress model. Developmental Psychology, 38, 179–193. doi: 10.1037/0012-1649.38.2.179 [DOI] [PubMed] [Google Scholar]
- Connell AM, & Dishion TJ (2008). Reducing depression among at-risk early adolescents: three-year effects of a family-centered intervention embedded within schools. Journal of Family Psychology, 22, 574–585. doi: 10.1037/0893-3200.22.3.574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z, & Shafran R (2003). Cognitive behaviour therapy for eating disorders: A “transdiagnostic” theory and treatment. Behaviour Research and Therapy, 41, 509–528. doi: 10.1016/S0005-7967(02)00088-8 [DOI] [PubMed] [Google Scholar]
- Gale CJ, Cluett ER, & Laver-Bradbury C (2013). A review of the father-child relationship in the development and maintenance of adolescent anorexia and bulimia nervosa. Issues in Comprehensive Pediatric Nursing, 36, 48–69. doi: 10.3109/01460862.2013.779764 [DOI] [PubMed] [Google Scholar]
- Harrison A, Sullivan S, Tchanturia K, & Treasure J (2010). Emotional functioning in eating disorders: attentional bias, emotion recognition and emotion regulation. Psychological Medicine, 40, 1887–1897. doi: 10.1017/S0033291710000036 [DOI] [PubMed] [Google Scholar]
- Harter S (1988). Manual for the self-perception profile for adolescents. Denver, CO: University of Denver. [Google Scholar]
- Haworth-Hoeppner S (2000). The critical shapes of body image: The role of culture and family in the production of eating disorders. Journal of Marriage and Family, 62, 212–227. doi: 10.1111/j.1741-3737.2000.00212.x [DOI] [Google Scholar]
- Haynos AF, & Fruzzetti AE (2011). Anorexia nervosa as a disorder of emotion dysregulation: Evidence and treatment implications. Clinical Psychology: Science and Practice, 18, 183–202. doi: 10.1111/j.1468-2850.2011.01250.x [DOI] [Google Scholar]
- Hedlund S, Fichter MM, Quadflieg N, & Brandl C (2003). Expressed emotion, family environment, and parental bonding in bulimia nervosa: A 6-year investigation. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity, 8, 26–35. doi: 10.1007/BF03324986 [DOI] [PubMed] [Google Scholar]
- Hu L, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6, 1–55. doi: 10.1080/10705519909540118 [DOI] [Google Scholar]
- Jacobi C, Hayward C, de Zwaan M, Kraemer HC, & Agras WS (2004). Coming to terms with risk factors for eating disorders: Application of risk terminology and suggestions for a general taxonomy. Psychological Bulletin, 130, 19–65. doi: 10.1037/0033-2909.130.1.19 [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Kasen S, & Brook JS (2002). Childhood adversities associated with risk for eating disorders or weight problems during adolescence or early adulthood. American Journal of Psychiatry, 159, 394–400. doi: 10.1176/appi.ajp.159.3.394 [DOI] [PubMed] [Google Scholar]
- Keel PK, & Forney KJ (2013). Psychosocial risk factors for eating disorders. International Journal of Eating Disorders, 46, 433–439. doi: 10.1002/eat.22094 [DOI] [PubMed] [Google Scholar]
- Kline RB (2011). Principles and practice of structural equation modeling. (3rd ed.). New York, NY: Guilford Press. [Google Scholar]
- Lam CB, & McHale SM (2012). Developmental patterns and family predictors of adolescent weight concerns: A replication and extension. International Journal of Eating Disorders, 45, 524–530. doi: 10.1002/eat.20974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine MP, & Smolak L (1992). Toward a model of the developmental psychopathology of eating disorders: The example of early adolesence In Crowther JH, Tennenbaum DL, Hobfoll SE, & Parris Stephens M (Eds.), The etiology of bulimia nervosa: The individual and familial context. (pp. 59–80). Washington D.C.: Hemisphere Publishing Corporation. [Google Scholar]
- MacCallum RC, Browne MW, & Sugawara HM (1996). Power analysis and determination of sample size for covariance structure modeling. Psychological Methods, 1, 130–149. doi: 10.1037//1082-989X.1.2.130 [DOI] [Google Scholar]
- May AL, Kim JY, McHale SM, & Crouter AC (2006). Parent-adolescent relationships and the development of weight concerns from early to late adolescence. International Journal of Eating Disorders, 39, 729–740. doi: 10.1002/eat.20285 [DOI] [PubMed] [Google Scholar]
- McBride BA, Schoppe SJ, & Rane TR (2002). Child characteristics, parenting stress, and parental involvement: Fathers versus mothers. Journal of Marriage and Family, 64, 998–1011. doi: 10.1111/j.1741-3737.2002.00998.x [DOI] [Google Scholar]
- McKnight Investigators. (2003). Risk factors for the onset of eating disorders in adolescent girls: Results of the McKnight longitudinal risk factor study. American Journal of Psychiatry, 160, 248–254. doi: 10.1176/ajp.160.2.248 [DOI] [PubMed] [Google Scholar]
- Morris AS, Silk JS, Steinberg L, Myers SS, & Robinson LR (2007). The role of family context in the development of emotion regulation. Social Development, 16, 361–388. doi: 10.1111/j.1467-9507.2007.00389.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Health. (2012). Study overview. Retrieved from https://www.nichd.nih.gov/research/supported/seccyd/Pages/overview.aspx#instruments
- Nock MK, Wedig MM, Holmberg EB, & Hooley JM (2008). The emotion reactivity scale: Development, evaluation, and relation to self-injurious thoughts and behaviors. Behavior Therapy, 39, 107–116. doi: 10.1016/j.beth.2007.05.005 [DOI] [PubMed] [Google Scholar]
- Polivy J, & Herman CP (2002). Causes of eating disorders. Annual Review of Psychology, 53, 187–213. doi: 10.1146/annurev.psych.53.100901.135103 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Coffman DL (2006). Computing power and minimum sample size for RMSEA. Retrieved from http://quantpsy.org
- Preacher KJ, Curran PJ, & Bauer DJ (2006). Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics, 31, 437–448. doi: 10.3102/10769986031004437 [DOI] [Google Scholar]
- Rosen K (1996). The principles of developmental psychopathology: Illustration from the study of eating disorders In Smolak L, Levine MP, & Striegel-Moore RH (Eds.), The developmental psychopathology of eating disorders: Implications for research, prevention, and treatment (pp. 3–29). Mahwah, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Sancho C, Arija MV, Asorey O, & Canals J (2007). Epidemiology of eating disorders. European Child & Adolescent Psychiatry, 16, 495–504. doi: 10.1007/s00787-007-0625-0 [DOI] [PubMed] [Google Scholar]
- Shields A, & Cicchetti D (1997). Emotion regulation among school-age children: The development and validation of a new criterion Q-sort scale. Developmental Psychology, 33, 906–916. 10.1037//0012-1649.33.6.906 [DOI] [PubMed] [Google Scholar]
- Spanos A, Klump KL, Burt SA, McGue M, & Iacono WG (2010). A longitudinal investigation of the relationship between disordered eating attitudes and behaviors and parent child conflict: A monozygotic twin differences design. Journal of Abnormal Psychology, 119, 293–299. doi: 10.1037/a0019028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, & Nemeroff C (1998). Dual pathway model of bulimia nervosa: Longitudinal support for dietary restraint and affect-regulation mechanisms. Journal of Social and Clinical Psychology, 17, 129–149. doi: 10.1521/jscp.1998.17.2.129 [DOI] [Google Scholar]
- Stice E, Shaw H, & Marti CN (2007). A meta-analytic review of eating disorder prevention programs: Encouraging findings. Annual Review of Clinical Psychology, 3, 207–231. doi: 10.1146/annurev.clinpsy.3.022806.091447 [DOI] [PubMed] [Google Scholar]
- Striegel-Moore RH, & Bulik CM (2007). Risk factors for eating disorders. American Psychologist, 62, 181–198. doi: 10.1037/0003-066X.62.3.181 [DOI] [PubMed] [Google Scholar]
- Wade TD, Bulik CM, & Kendler KS (2001). Investigation of quality of the parental relationship as a risk factor for subclinical bulimia nervosa. International Journal of Eating Disorders, 30, 389–400. [DOI] [PubMed] [Google Scholar]
- Wade TD, Gillespie N, & Martin NG (2007). A comparison of early family life events amongst monozygotic twin women with lifetime anorexia nervosa, bulimia nervosa, or major depression. International Journal of Eating Disorders, 40, 679–686. doi: 10.1002/eat [DOI] [PubMed] [Google Scholar]
- Wanden-Berghe RG, Sanz-Valero J, & Wanden-Berghe C (2010). The application of mindfulness to eating disorders treatment: A systematic review. Eating Disorders: The Journal of Treatment and Prevention, 19, 34–48. doi: 10.1080/10640266.2011.533604 [DOI] [PubMed] [Google Scholar]
- Thompson RA, & Meyer S (2007). Socialization of emotion regulation in the family In Gross JJ (Ed.), Handbook of emotion regulation (1st ed., pp. 249–268). New York: Guilford Press. [Google Scholar]


