Thank you all for attending the meeting. It has been an honor to serve as president and to plan this meeting with my fellow councillors of the Association of American Physicians (AAP), our executive director, and leaders in the American Society for Clinical Investigation (ASCI). In preparation for this presidential address, as most prior AAP presidents have done, I read the first 100 years of the AAP (1) and reviewed prior presidents’ presentations. Today, I will present a brief history of our society and the meeting. Then, in keeping with the aging theme of this year’s meeting, I will reflect on aging and research, and finally make a few predictions on what our meeting might look like in the future.
In the last decade of the 1800s, Luke Fildes, a noted artist of the time, was commissioned to create a painting (Figure 1). As for many artists at that time, the subject matter was left to his discretion, and so Fildes decided to paint something that was very meaningful to him. In 1877, his one-year-old boy had died. He had never forgotten the tragic event, but also the care of the physician that came to his home regularly to see the little boy. The focal point of the artwork is the physician, kneeling, gazing with a grave expression upon the child. The father is looking on from behind the chairs while the mother cradles her head in her arms, inconsolable. The painting, entitled The Doctor, “put on record the status of the doctor of the time” (The Times, March 17, 1891). Fildes’ painting showed a professional and compassionate physician to the world; it was widely reproduced and became a best seller. Many medical schools and doctor offices still display reproductions of the painting as the symbol of professional devotion of the physician. Yet, in 1877, there was very little that this physician could tangibly do to help the child, who was severely ill with pneumonia. Germ theory was not yet known. There were no antipyretics or antibiotics. Most certainly, the physician had not even washed his hands before seeing the child. This painting sets the framework of the time when the physician founders of the AAP came together. This small group of physicians knew that to advance their ability to care for their patients, research was essential. The golden age of medicine based on scientific study was fueled by this thinking, as well as by the progressive advances related to the industrial age. Faster and greater communication and travel, and deeper knowledge of pathology, biology, and chemistry all came together for rapid advances in medicine in the early 1900s. AAP was a major force in the development of scientific medicine.
Figure 1. The Doctor.
Luke Fildes, The Doctor. 1891, oil on canvas, 65 in × 95 in (166 cm × 242 cm), Tate Gallery, London. This work of art was meant “to put on record the status of the doctor of our time” (The Times, March 17, 1891).
The founders of the AAP were all young, generally in their mid-thirties to early forties, but most already full professors. Francis Delafield, William Draper, and James Tyson were physicians at Columbia, George Peabody at New York Hospital, William Pepper and William Osler at University of Pennsylvania, and Robert Edes a private practitioner in New York. Delafield suggested creating an association and invited them all to his home in Manhattan. Over dinner, they developed plans for the AAP, and decided upon having 100 members. The nomination and election processes were much the same as now: two members would nominate an individual, all would review, followed by ballot election, and then welcoming of new members at an annual meeting. They selected 85 people the first year, which did not leave many spots for new people in the coming years. Nevertheless, 85 individuals were welcomed to the first AAP meeting the following year in Washington, DC. The AAP constitution stated the primary goal of the society was to advance scientific and practical medicine. Another goal of the founders was to have a place to convene, develop community, and share science. The annual meeting was planned to offer opportunities to come together and share knowledge, always for the betterment of the patient. There was an honor in being nominated, in being selected. It meant that the individual had made a contribution that was spectacularly important, that transformed patient care, and that endured over time. The society wanted to recognize these physicians with membership. The contemporary mission of AAP stays true to all these goals.
The criteria for membership in AAP selected for leaders in science and medicine who pioneered research in medicine and initiated other impactful societies and journals. For example, Christian Herter was one of the early new members of AAP. He finished medical school at Columbia at age 18, then studied at Johns Hopkins with William Welch. When he returned to New York to practice medicine, he started a laboratory in his home, as there were no research laboratories at medical institutions at the time. He and John Abel from Johns Hopkins started the Journal of Biological Chemistry to widely disseminate research discoveries. The need for more and well-equipped laboratory facilities led to the creation of the Rockefeller Institute for Medical Research by several AAP members. From these beginnings, AAP grew and scientific medicine flourished. While the founders planned to have 100 members total, AAP now includes 2,200 members, with 60 new members inducted each year. The founders always intended that the AAP have a wide geographic distribution of American physicians. In fact, in their first cohort, they included five Canadians. Canadians have always been a major part of AAP, even serving as presidents of the society. In 1907, some AAP members, concerned about the increasing age and increasing difficulty in being inducted to AAP, created the ASCI. They called members in this new society the “young Turks,” based on the Turkish Nationalistic Revolution of the time, where the young were trying to overtake the old and redo the Turkish government.
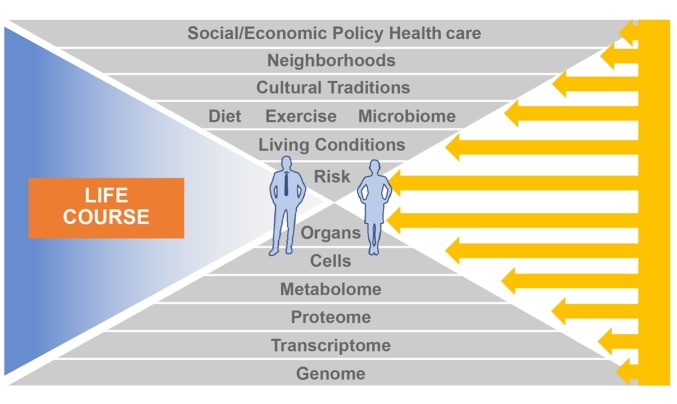
The formation of the ASCI was similar to the AAP. Sam Meltzer, a physician and researcher in New York, invited several members of AAP to his home one evening after the AAP meeting, and they created the ASCI and the process for membership. The first ASCI meeting was May 11, 1908, in Washington, DC. Because many of the inaugural members were AAP members, out of convenience, they held the ASCI meeting the day before the AAP meeting. Ever since then, AAP and the ASCI have met together annually in the spring. Today, about two-thirds of AAP members are dual members in the ASCI. In the late 1930s, Sam Meltzer and William Welch reflected that, “the young Turks are getting really old.” They decided to create a truly young society. Over the last two days of this meeting, we’ve heard about phenotypic age, biologic age, and chronologic age. Clearly, the AAP and ASCI members were looking at chronologic age when they suggested an age cutoff of 40 for a new society, the American Federation for Clinical Research (AFCR). Membership required age under 41 and at least one scientific publication. The annual meeting became a tri-society meeting — AAP, the ASCI, and AFCR. When the ASCI formed in 1908, it was a small society, and there was only a small bump in the yearly meeting attendance. When AFCR formed in 1940, meeting attendance increased tremendously (Figure 2). Ultimately, AFCR left the tri-society meetings, which resulted in fewer young scientists at the meetings. Fortunately, the American Physician Scientists Association (APSA) joined in with our meeting in 2006 and has become an important part of our joint meeting for interactions with trainees. Howard Hughes Medical Institute trainees joined in 2015 and are here again in 2018.
Figure 2. History of the annual meeting attendance.
Meeting attendance was recorded sporadically over the years, shown by black dots. Growth of the meeting occurred with formation of the ASCI, then AFCR, and with increasing membership of AAP and the ASCI over the years. AFCR (renamed American Federation of Medical Research) left the joint meeting in 1996, and APSA joined in 2006.
AAP and ASCI members include physician researchers who make an impact in many types of medical sciences. AAP membership selects for individuals who have made sustainable and enduring transformative contributions. This type of contribution usually takes many years, perhaps a lifetime to achieve. ASCI membership selects for those individuals who have made an early scientific discovery and achieved first independent support for their research. While AAP has never had an age cutoff for membership, the average age of AAP inductees is 57 and the average age of members is 68. The ASCI, in 1981, decided upon an age cutoff under 45. But in 2013, the ASCI council became concerned that the 45 cutoff was precluding many deserving of membership and so increased the age cutoff to 50. The ASCI average age of inductees this year is 45, and the average age of members is 50. This history provides the general concept, ever since creation of the ASCI, that ASCI members should be younger in chronological age than AAP members, and that there is a progression through the societies based on the first scientific impact (recognized by the ASCI) evolving into enduring transformative accomplishments (recognized by AAP).
This concept allows us to start to think about our scientific research careers as physicians throughout all types of age. NIH has provided information on the age at which scientists are awarded a first grant (2). The percentage of funded investigators under age 45 has been dropping since 1990, and the percentage of funded investigators over age 60 has been increasing. This age distribution looks a lot like the global population trend. The world population trend shows that we are getting chronologically older, so that by 2050, one in five people will be over 60. This raises the question, is NIH funding merely reflective of the age of people available to apply for grants? It also raises the question, how old is old? As people achieve a longer life span, overall population chronological age increases, but the relative life expectancy of the population is younger (3). This was modeled by applying a definition of “old” being the average age of death in a population minus 15. Individuals would not be considered old until they reached that prospective age. This means that if a population is living longer, identifying someone as old after a fixed age doesn’t make sense; it should be relative to the life span.
Just like the general population, physicians in the United States are aging. One in four of the 800,000 physicians in practice today are over 65 (4), and they seem to be aging very successfully. Over 7,000 US physicians were surveyed on work/life balance, burnout, happiness, and then classified by years of working: fewer than 10 years, 10 to 20 years, or over 20 years (5, 6). The most satisfied, happiest physicians were those that had been working over 20 years, and were over 60. They had a strong psychological construct of optimism and purpose in life. While this study did not specifically evaluate research physicians, a recent study of the scientific workforce showed that the number of scientists over 55 is increasing at a pace that surpasses the general aging of the workforce (7). It seems physicians and scientists over 55 continue to work at a greater rate than the general population and are more satisfied in their work. This may be related to another kind of aging, generational aging, which is defined based on our experiences as a cohort. Different cohorts have different expectations of what is youth and what is aging. People in the baby boomer generation, born between 1946 and 1964, are devoted to their work, take little time off from work, aim for very high achievement to the exclusion of leisure activity, and when they think of retirement, wonder, what else would I do? The baby boomers were the first to really benefit from the longer life span brought about by the golden age of medicine. Baby boomers have unique and contrasting memories, including slide rules and calculators, typewriters and personal computers, landline phones and smart phones, regular mail and email. Baby boomer physicians started their careers with paper charts and radiographic films but now use electronic health records. The life and memory of a baby boomer is vastly different than a baby born in the last 10 years, Generation Z. A Gen Z child will never know a world that doesn’t have a smart device and will never know what it is to not know. Gen Z will have advantages over prior generations. They’re true digital natives. They receive and send multiple sources of information rapidly. They think, communicate, and consume in images, not words. They’re collaborative and want to work in teams. Some have speculated that Gen Z may be the last truly human generation because they are likely to be open to having neurocognitive implantable enhancement devices.
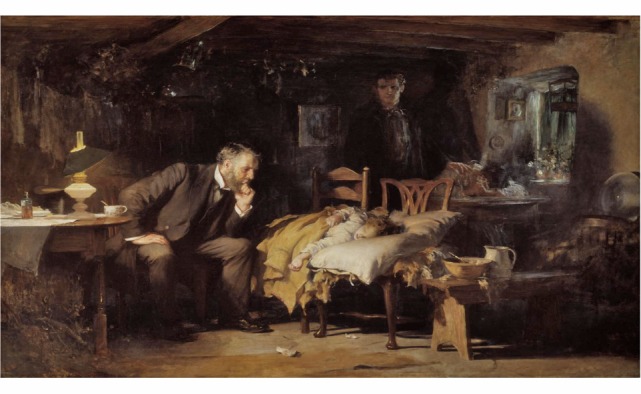
Generational age, prospective age, and chronological age should all be taken into consideration as we think about the future of scientific medicine. In the not-so-distant future, individuals will have their whole genome, epigenome, transcriptome, proteome, and metabolome data readily available to them and their health care providers (Figure 3). The information will provide new understanding of individual risks for disease. Collective individual risks of people will provide information on population risks. Real-time monitoring of diet, activity, home, neighborhood, and work environment over the life span will be easily obtained, and used in risk prediction for diseases. Ideally, as physician researchers, we will discover new ways to intervene in all the potential components of risk to prevent and/or reverse disease.
Figure 3. Precision and population health determinants.
The lower triangle shows unique biological components for individual risk of disease, and the upper triangle shows behavioral, environmental, and societal determinants of risk for individuals and populations. The determinants integrated over the life course will reveal opportunities for interventions (right side arrows) aimed at specific components to modify, prevent, or treat disease.
Considering the vast changes over the past 133 years of the AAP, what will the society be like in 2050? What will the meeting be like? I am certain that there will be a meeting in April of 2050, because we have been meeting together regularly in the spring since 1887. The meeting will likely be in Chicago, because we’ve only moved the meeting twice between 1887–2000, and we’ve been in Chicago just since 2001. We will all be chronologically older, just like the rest of the world, but we will not be old. We will still be passionate about science and physician-led science, because that’s our core mission. We will still be inducting physicians that are doing transformative work, and striving to inspire young scientists, but the type of science and how it is done will certainly be different. The meeting will be at the peak of the digital age, which should be as great or greater than the industrial age experienced in the late 1800s and through the early 1900s by our founders. The increasing volumes of data, ease and speed of analytics, technologic advances in data sciences, and inductees with unique capabilities developed since birth, altogether promise a rapid pace of discoveries and, importantly, faster translation and greater implementation for benefits to human health. It is exciting, and perhaps a bit overwhelming, to think about all the possibilities. But, as stated by Abraham Lincoln, “The best thing about the future is that it comes only one day at a time.” I hope to be at the meeting in 2050 with all of you, listening to the presidential address.
Acknowledgments
Thank you to Lori Ennis for detailed information on AAP and the annual meetings, John Hawley for information on ASCI membership, and Allison Janocha for expert editorial assistance with the manuscript.
Version 1. 10/01/2018
Print issue publication
Footnotes
Reference information: J Clin Invest. 2018;128(10):4204–4207. https://doi.org/10.1172/JCI124523.
This article is adapted from a presentation at the 2018 AAP/ASCI/APSA Joint Meeting, April 21, 2018, in Chicago, Illinois, USA.
References
- 1. Harvey AM, ed. The Association Of American Physicians 1886–1986: A Century Of Progress In Medical Science. 1st ed. Philadelphia, Pennsylvania, USA: Williams & Wilkins; 1986. [Google Scholar]
- 2.Lauer M, Tabak L, Collins F. Opinion: the next generation researchers initiative at NIH. Proc Natl Acad Sci U S A. 2017;114(45):11801–11803. doi: 10.1073/pnas.1716941114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sanderson WC, Scherbov S. Faster increases in human life expectancy could lead to slower population aging. PLoS One. 2015;10(4):e0121922. doi: 10.1371/journal.pone.0121922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. AMN Healthcare. 2016 Survey of Physicians 55 and Older. AMN Healthcare website. https://www.amnhealthcare.com/industry-research/survey/2016-physician-survey/ Accessed August 28, 2018.
- 5.Dyrbye LN, Varkey P, Boone SL, Satele DV, Sloan JA, Shanafelt TD. Physician satisfaction and burnout at different career stages. Mayo Clin Proc. 2013;88(12):1358–1367. doi: 10.1016/j.mayocp.2013.07.016. [DOI] [PubMed] [Google Scholar]
- 6.Depp CA, Jeste DV. Definitions and predictors of successful aging: a comprehensive review of larger quantitative studies. Am J Geriatr Psychiatry. 2006;14(1):6–20. doi: 10.1097/01.JGP.0000192501.03069.bc. [DOI] [PubMed] [Google Scholar]
- 7.Blau DM, Weinberg BA. Why the US science and engineering workforce is aging rapidly. Proc Natl Acad Sci U S A. 2017;114(15):3879–3884. doi: 10.1073/pnas.1611748114. [DOI] [PMC free article] [PubMed] [Google Scholar]