Abstract
Rationale:
Although the survival period of patients who undergo liver transplantation is improving due to advances in surgical techniques and medical treatment, there is a lack of detailed, sufficient data that compare the choice of anesthetic agent in post-liver transplant surgery to avoid liver injury.
Patient concerns:
The authors describe acute liver injury observed in a 61-year-old man who underwent liver transplantation surgery 13 years previously and who was on immunosuppressive therapy. The patient underwent bilateral total knee arthroplasty under general anesthesia, for which a total of 200 mg bupivacaine was injected into each knee after wound closure. Liver enzyme levels increased to more than 10 times the upper limit of normal after the conclusion of surgery and remained extremely high on postoperative day 1.
Diagnoses:
Clinical and laboratory findings were consistent with bupivacaine-induced liver injury. Intra-articular administration of bupivacaine after total knee arthroplasty is a widely used intraoperative analgesic method and complications are rare; nevertheless, the risk for inadvertent delivery into the systemic circulation remains.
Interventions:
Clinical presentations and hepatobiliary ultrasound examination allowed a conservative management.
Outcomes:
Serum liver enzyme levels normalized 12 days after surgery, and the patient was discharged 22 days after surgery.
Lessons:
Acute liver injury can lead to graft failure from late death after liver transplantation. Transplant recipients with long-term survival have the highest risk for anesthesia because of post-transplant complications, including diabetes, hypertension, and renal insufficiency. Clinicians should be aware that analgesic techniques and anesthetics may affect graft function.
Keywords: bupivacaine, drug-induced liver injury, liver transplantation
1. Introduction
Although advances and studies in surgical techniques and medical management have improved the survival rates of liver-transplant recipients, this patient population may experience complications that contribute to morbidity and mortality in the long-term period. These complications include diabetes mellitus, hypertension, and/or nephrotoxicity and are mainly due to prolonged immunosuppressive therapy.[1] In the case of post-transplant surgery, few reports have described the effect of anesthetic techniques on liver transplant recipients with long-term survival.
The main concerns in post-transplant anesthesia are related to surgical technique (e.g., incidence of intra- or postoperative bleeding), infections (viral, bacterial, or fungal), and functional status of the cardiopulmonary and renal systems. Furthermore, perioperative hemodynamic changes (hypotension, hypoxia, and ischemia) and hepatotoxic drugs may affect graft function.[1,2] The liver is a complex organ involved in synthetic, storage, and excretory functions that affect the entire body. Although alteration of liver function may result in mild symptoms, such as elevated levels of hepatic enzymes, or jaundice, it may also lead to death due to fulminant hepatic failure.[3]
In the case described herein, the patient was undergoing regular medical follow-up 13 years after liver transplantation; his preoperative evaluation did not reveal any abnormal findings. The patient underwent bilateral total knee arthroplasty (TKA) under general anesthesia with the administration of intra-articular bupivacaine for postoperative analgesia. Transaminase levels were elevated to >10 times the upper limit of normal range 3 hours after the conclusion of surgery. This case—in which acute liver injury developed as a significant complication—was possibly associated with intra-articular administration of bupivacaine.
2. Case report
Approval for the study by the institutional review board of Kyungpook National University Hospital was not necessary because it was a case report, based on the institutional policy. The patient provided informed consent for publication of this case and we anonymized the presented data. A 61-year-old man underwent elective bilateral TKA for degenerative osteoarthritis. He had been previously diagnosed with type 2 diabetes mellitus and stage 4 chronic kidney disease. The patient underwent living-donor liver transplantation 13 years previously for hepatitis B virus-related liver cirrhosis and experienced a non-ST-elevation myocardial infarction 11 years previously. He was undergoing regular follow-up and was being treated with insulin, oral hypoglycemic agent, calcium-channel blocker, diuretics, acetylsalicylic acid, clopidogrel, and tacrolimus. No significant abnormalities were observed on cardiac evaluation with electrocardiography, two-dimensional transthoracic echocardiography, 99mTc-methoxyisobutylisonitrile myocardial perfusion imaging, and measurement of cardiac enzyme levels performed preoperatively. Except for altered renal function, the preoperative evaluation yielded normal results. Previous anesthetic history included general anesthesia for liver transplantation 13 years previously and spinal anesthesia for ureteroscopic removal of calculi 3 years previously. He did not experience any complications on either occasion. Acetylsalicylic acid and clopidogrel were discontinued 5 days before TKA surgery to mitigate the risk for perioperative bleeding, and general anesthesia was chosen due to prolongation of bleeding time in the platelet function test.
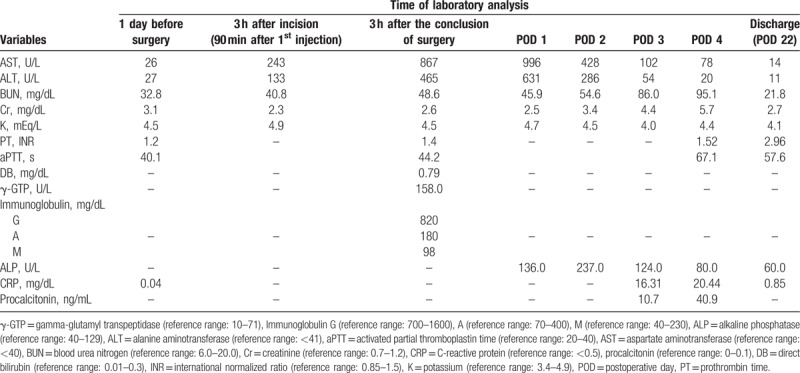
The patient received no premedication. Preoperative antibiotics, cefetezole 1 g with normal saline 100 mL, were administered. General anesthesia was induced using propofol 2 mg/kg, and cisatracurium 0.5 mg/kg was administered to facilitate endotracheal intubation. Mechanical ventilation was performed using a mixture of air in 50% oxygen, and anesthesia was maintained with desflurane, remifentanil, and an infusion of cisatracurium. Pulse oximetry, electrocardiography, measurement of bispectral index, and invasive arterial blood pressure monitoring were performed continuously. Blood pressure and heart rate were maintained to within 20% of preanesthetic values without vasoactive drugs. Intra-articular injection was performed by the surgeon without consulting or notifying the anesthetist. At the completion of wound closure, and 15 minutes after tourniquet deflation, a mixture of 0.5% bupivacaine 20 mL (Myungmoon Pharm, Seoul, Korea), ketorolac 30 mg (ketocin, Myungmoon Pharm, Seoul, Korea), morphine 5 mg, and epinephrine 0.25 mg (total volume, 50 mL) was injected into each knee joint as a single bolus using a 20-gauge needle (Fig. 1). Arterial blood gas analysis 3 hours after the first incision revealed a potassium level of 5.8 mmol/L. Laboratory investigations were performed at the same time for accuracy, and revealed a serum potassium level of 4.9 mmol/L, and aspartate transaminase (AST) and alanine transaminase (ALT) levels were 243 and 133 U/L, respectively. Tracheal extubation was performed when the patient began obeying verbal commands, and spontaneous respiration was restored. The patient was alert and transferred to the ward after observation in the post-anesthesia care unit for 1 hour. Hemodynamic variables were stable and no abnormal findings were noted during this period.
Figure 1.
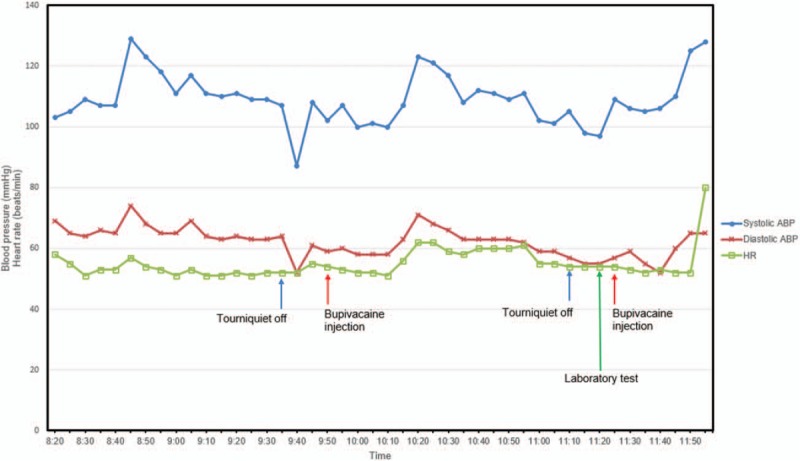
Intraoperative vital signs. ABP = arterial blood pressure, HR = heart rate.
Serum transaminase levels were elevated to >10 times the upper limit of normal range 3 hours after the conclusion of surgery. The patient did not complain of any specific symptoms other than surgical site pain. Viral markers and immunological tests were all negative, and there were no hypotensive or hypoxic episodes during the perioperative period (Fig. 1). On postoperative day 1, hepatobiliary ultrasound examination revealed normal echotexture and echogenicity of the parenchyma of the transplanted liver, with no focal lesions. Doppler spectral wave pattern was normal; intrahepatic, inferior vena cava, portal venous, and hepatic artery blood flows were also normal, and no specific findings were visualized in the pancreas or spleen. A gastroenterologist and a liver transplant surgeon who evaluated the patient suggested that drug-induced liver disease (DILI) may have occurred during surgery. Ceftezole was administered during the postoperative period.
On postoperative day 3, the patient complained of dyspnea, and suddenly developed hypotension (systolic blood pressure of <90 mmHg), high fever (>39 °C), and oliguria. Persistent hypoxia on arterial blood gas analysis and pulmonary edema on chest radiography were noted. The patient was admitted to the intensive care unit, and deep vein thrombosis and pulmonary thromboembolism were considered. Although deep vein thrombosis was noted in both peroneal veins, pulmonary thromboembolism was not found on computed tomography. Postoperative evaluation using transthoracic echocardiography also revealed no specific abnormality. After admission to the intensive care unit, mechanical ventilation and continuous renal replacement therapy were started. On postoperative day 5, the patient was weaned from mechanical ventilation and transferred to the general ward after extubation. Serum AST/ALT levels normalized 12 days after surgery, and the patient was discharged 22 days after surgery. The laboratory test results are summarized in Table 1.
Table 1.
Flow chart of laboratory test results.
3. Discussion
Because the liver is an important organ actively involved in drug metabolism, adverse effects of anesthetic agents are mainly suspected when liver enzyme levels are elevated after surgery performed under anesthesia. It is difficult, however, to establish causal relationships between hepatic damage and toxic factors. Therefore, to date, extensive evaluations of hepatotoxicity due to anesthetic agents have not been performed. Currently used anesthetics are believed to have little effect on postoperative hepatic function, and may result in elevation of transaminase levels without specific symptoms.[4]
In our case of post-transplant surgery, transaminase levels rose rapidly after intra-articular administration of bupivacaine after TKA. There are many contributing factors that can potentially affect hepatic function during surgery, including hepatotoxic drugs, and/or anesthetic-, graft-, or surgery-related factors. Furthermore, decreased immunity due to anesthesia or the surgery itself, or immunological hypersensitivity could have a significant effect on liver function.[1,2] Our patient did not receive any blood products, and severe hypotension or massive blood loss, which could cause intraoperative hepatic ischemia, were not observed during surgery. The surgical site was also not associated with the hepatobiliary system. The patient was undergoing long-term immunosuppressive therapy after liver transplantation, and immunosuppressed patients are at risk for infection, which may increase transaminase levels. However, the presence of an infection was ruled out preoperatively, with no leukocytosis and a normal C-reactive protein level.
Considering the anesthetic technique, it is known that inhalation anesthetics have little effect on postoperative liver function or only increase transaminase levels without symptoms in non-transplant surgery of liver-transplant recipients.[2] Halothane, enflurane, isoflurane, and desflurane produce a reactive intermediate that binds to a specific liver protein, which can act as an antigen and trigger an immune response that directly causes liver damage. This trifluoroacetylated protein appears in all patients exposed to halothane; however, the immune response is seen in a small number of cases on repeated exposure. Among fluorinated inhalation anesthetics, desflurane appears to have the lowest metabolic rate, and hepatotoxicity due to repeated exposure after halothane inhalation is rare.[5,6] In the present case, anesthesia during liver transplantation was maintained with sevoflurane, and there was no history of exposure to halothane or enflurane. Furthermore, halothane-associated hepatotoxicity also is a type of immune-mediated reaction, but the patient had no clinical symptoms of pruritus or rash, and had a normal immunological test.
It could be argued that antibiotics may be a cause of hepatotoxicity. In the perioperative period, the patient received ceftezole sodium, a cephalosporin antibiotic. Ceftezole sodium rarely causes hepatotoxicity, and the patient's liver function test had normalized under maintenance of the same antibiotics. This was analogous to a negative re-challenge test to ceftezole. The patient exhibited no abnormal findings on liver ultrasonography, Doppler, or computed tomography performed after surgery. Therefore, intra-articular injection of bupivacaine was the most likely cause of hepatic injury in this case.
Bupivacaine is extensively metabolized by the hepatic cytochrome P450 system, and amide local anesthetics are not known to directly cause hepatocellular toxic effects in cases of regional or local anesthesia. However, their metabolism may be inhibited in cases of severe chronic liver disease. In patients with severe liver disease, the serum concentration of amide local anesthetics may increase 3 to 4 times over that of normal patients, suggesting that systemic toxicity may occur after administration of these local anesthetics. Systemic toxicity from amide local anesthetics manifests itself mainly as neurological and cardiovascular complications, whereas bupivacaine-induced liver injury and cholestasis have been reported with continuous epidural or local administration for the treatment of chronic or postoperative pain. These reports suggest that bupivacaine-induced liver injury could be caused by an allergic reaction or toxic metabolites.[7–9]
Toxicity could be associated with absolute plasma levels or the rate of absorption of the local anesthetic. In previous studies, the intra-articular dose of bupivacaine for TKA was approximately 75 to 225 mg,[10–12] and in these investigations, bupivacaine was administered while leaving the tourniquet inflated for a few minutes. The effect of tourniquet inflation is an independent factor affecting the peak plasma level of bupivacaine. Longer tourniquet inflation time after bupivacaine injection results in increased local tissue binding and decreased peak plasma level.[12] Therefore, the plasma level cannot be directly predicted from the dose administered: it depends on the rate of absorption and the rate of clearance from the body. Our patient was administered a total of 200 mg of bupivacaine as a single intra-articular injection after deflation of the tourniquet, and the timing of the injection provided an opportunity for access to the systemic circulation. It is possible that systemic local anesthetic toxicity, such as central nervous system toxicity, could be masked by general anesthesia. In addition, the patient complained of surgical site pain immediately after the operation despite the analgesic injection. We postulate that rapidly increased plasma concentration of bupivacaine was the most likely etiology in this case.
The mechanism of bupivacaine-induced liver injury remains unclear. The reaction to the drug may be unrelated to duration or a dose-dependent effect of toxicity. AST/ALT levels increased more than tenfold; direct bilirubin, alkaline phosphatase, and gamma-glutamyl transpeptidase levels also increased, and a degree of cholestasis could be suggested by high alkaline phosphatase levels. These parameters met the diagnostic criteria for DILI, and acute liver injury was suspected.[13] DILI has a wide range of manifestations and several causative agents have been implicated; however, there is a lack of objective diagnostic tests and a clear line of management. DILI remains a diagnosis of exclusion based on detailed history and a prudent interpretation of blood tests, hepatobiliary imaging, and liver biopsy.[13] In this case, no other drugs that could lead to hepatotoxicity were administered, and liver function gradually recovered with time. Although this case has not been proven histologically by liver biopsy, we suggest that hepatotoxicity occurred due to massive absorption of bupivacaine.
Importantly, our patient presented with special features that need to be considered. First, although bupivacaine may directly affect hepatic function, hepatotoxicity may also be related to underlying disease, preoperative status, and previous medication. Because all previously reported bupivacaine-induced liver injuries were in patients free of pre-existing liver disease, it is difficult to clarify the relationship between pre-existing conditions and liver injury. As a result, we could not predict the effect of intra-articular bupivacaine injection on hepatic function in this particular patient with long-term survival after liver transplantation. Second, the most unfortunate aspect of this case was that the analgesic treatment was performed by the surgeon without considering the specific features of the patient. In particular, this confirms, once again, that communication between the surgeon and anesthetist during surgery is important to the patient.
4. Conclusion
In summary, we have described bupivacaine-induced liver injury caused by intra-articular injection after TKA. Despite the limited incidence of bupivacaine-induced liver injury, clinicians should be aware of the possible increase in plasma concentration of intra-articular bupivacaine depending on the tourniquet status or patient condition. As was the case with our patient, a variety of transplant recipients with long-term management may present for either elective or emergency non-transplant surgery. Therefore, perioperative considerations in the transplant population also require dedicated studies investigating appropriate anesthetic management and follow-up guidelines for cases of non-transplant surgery.
Author contributions
Conceptualization: Jeong Eun Lee.
Data curation: Jeong Eun Lee.
Formal analysis: Jeong Eun Lee.
Supervision: Kyung-Hwa Kwak.
Writing – original draft: Jeong Eun Lee.
Writing – review & editing: Jeong Eun Lee.
Jeong Eun Lee orcid: 0000-0002-7069-6264
Footnotes
Abbreviations: ALT = alanine transaminase, AST = aspartate transaminase, DILI = drug-induced liver disease, TKA = total knee arthroplasty.
Ethical approval: This case is not a clinical trial and just incidental interventional process so ethical approval was not necessary.
No potential conflict of interest relevant to this article was reported.
References
- [1].Moreno R, Berenguer M. Post-liver transplantation medical complications. Ann Hepatol 2006;5:77–85. [PubMed] [Google Scholar]
- [2].Kostopanagiotou G, Smyrniotis V, Arkadopoulos N, et al. Anesthetic and perioperative management of adult transplant recipients in nontransplant surgery. Anesth Analg 1999;89:613–22. [DOI] [PubMed] [Google Scholar]
- [3].Marrone G, Vaccaro FG, Biolato M, et al. Drug-induced liver injury 2017: the diagnosis is not easy but always to keep in mind. Eur Rev Med Pharmacol Sci 2017;21(suppl):122–34. [PubMed] [Google Scholar]
- [4].Yoon JH, Cho SH, Kim CS, et al. Comparisons of propofol, enflurane, sevoflurane, and desflurane anesthesia in laparoscopic cholecystectomy on postoperative liver enzyme levels. Korean J Anesthesiol 2005;49:18–24. [Google Scholar]
- [5].Njoku D, Laster MJ, Gong DH, et al. Biotransformation of halothane, enflurane, isoflurane, and desflurane to trifluoroacetylated liver proteins: association between protein acylation and hepatic injury. Anesth Analg 1997;84:173–8. [DOI] [PubMed] [Google Scholar]
- [6].Koblin DD. Characteristics and implications of desflurane metabolism and toxicity. Anesth Analg 1992;75(suppl):S10–6. [PubMed] [Google Scholar]
- [7].Rosenberg PH, Veering BT, Urmey WF. Maximum recommended doses of local anesthetics: a multifactorial concept. Reg Anesth Pain Med 2004;29:564–75. [DOI] [PubMed] [Google Scholar]
- [8].Chintamaneni P, Stevenson HL, Malik SM. Bupivacaine drug-induced liver injury: a case series and brief review of the literature. J Clin Anesth 2016;32:137–41. [DOI] [PubMed] [Google Scholar]
- [9].Yokoyama M, Ohashi I, Nakatsuka H, et al. Drug-induced liver disease during continuous epidural block with bupivacaine. Anesthesiology 2001;95:259–61. [DOI] [PubMed] [Google Scholar]
- [10].Lombardi AV, Jr, Berend KR, Mallory TH, et al. Soft tissue and intra-articular injection of bupivacaine, epinephrine, and morphine has a beneficial effect after total knee arthroplasty. Clin Orthop Relat Res 2004;125–30. [DOI] [PubMed] [Google Scholar]
- [11].Browne C, Copp S, Reden L, et al. Bupivacaine bolus injection versus placebo for pain management following total knee arthroplasty. J Arthroplasty 2004;19:377–80. [DOI] [PubMed] [Google Scholar]
- [12].Katz JA, Kaeding CS, Hill JR, et al. The pharmacokinetics of bupivacaine when injected intra-articularly after knee arthroscopy. Anesth Analg 1988;67:872–5. [PubMed] [Google Scholar]
- [13].Chalasani NP, Hayashi PH, Bonkovsky HL, et al. ACG Clinical Guideline: the diagnosis and management of idiosyncratic drug-induced liver injury. Am J Gastroenterol 2014;109:950–66. [DOI] [PubMed] [Google Scholar]


