Abstract
Rationale:
Due to the low incidence and lack of effective diagnostic measures for the diagnosis of metal allergy in patients undergoing total joint arthroplasty (TJA), diagnosis relies mainly on the exclusion of other causes, in particular infection. It remains a relatively unpredictable and poorly understood cause of implant failure. At present, skin patch testing, leukocyte migration inhibition test (LMIT) and lymphocyte transformation tests (LTT) are being commonly used to assess metal hypersensitivity.
This report presents both a case and literature review.
Patient concerns:
A 61-year-old female patient experienced continuous swelling and pain in the right knee joint for 9 months after a right-side total knee arthroplasty (TKA).
Diagnoses:
We believe this is the case report of metal allergy in TKA. The following were the reasons for this. First, no definite symptoms of infection during revision arthroplasty were observed, but with obvious hyperplasia of synovium. Furthermore, a frozen biopsy revealed an extremely low neutrophil count, which was considered to be caused by chronic inflammation. Second, the results of repeated post-operation reexaminations indicate a clear increase in the number of eosinophils, while no bacteria were found in the tissue bacterial smear performed during the operation. Third, improvements were clearly observed in the patient following synovectomy, revision of the polyethylene insert and anti-anaphylactic treatment.
Interventions:
The patient underwent synovectomy, revision of the polyethylene insert and anti-anaphylactic treatment.
Outcomes:
The patient's right knee remained mildly swollen; however, the pain has been relieved significantly. The range of motion could achieve 0 degrees of extension and 90 degrees of flexion.
Lessons:
No consensus has been reached about the best diagnostic criteria for this disease, and most physicians would consider it to be a possibility when other diseases including periprosthetic joint infection (PJI) have been excluded. Although this case followed the same course, the outcome following synovectomy and anti-anaphylactic treatment further confirmed our hypothesis.
Keywords: infection, metal allergy, revision, total-joint arthroplasty
1. Introduction
Total-joint arthroplasty (TJA) is one of the most successful and effective orthopedic operations performed during the last century. As a treatment for disabilities of the hip and knee, it can relieve pain, correct deformity, and improve the patient's quality of life. However, not all TJA patients benefit from significant pain relief and functional improvement. Some patients experience persistent pain following this procedure. The most common cause of unsatisfactory outcomes, aside from intraoperative technical error, is periprosthetic joint infection. However, one should not forget that metal hypersensitivity, though quite rare (<1% of TJA recipients), is also a potential cause of unresolved pain and should be regarded as a differential diagnosis in this situation.[1,2]
The authors present here a case suffering from persistent debilitating pain and swelling of the operated knee following total-knee arthroplasty (TKA). Initially, a diagnosis of periprosthetic joint infection (PJI) was made. However, following investigation, the evidence pointed to a diagnosis of metal hypersensitivity and anti-anaphylactic treatment produced satisfactory results.
2. Case report
A 61-year-old female patient was diagnosed with degenerative osteoarthritis of the right knee and underwent TKA (NexGen high-flex TKA; Zimmer, Warsaw, IN) in our institution in September 2012. During hospitalization, her recovery and rehabilitation were uneventful, and 7 days after operation, the patient was discharged. However, she complained of continuous low-grade fever, swelling, stiffness, as well as pain of the operated knee at each follow-up, over a period of 9 months, which had an adverse effect on her daily activities. Her only significant medical history was an allergy to jewelry.
On physical examination, the right knee was obviously swollen (Fig. 1), and the range of motion (ROM) was −5° of extension to 15° of flexion. Her white blood cell (WBC) count and neutrophil differentiation were normal, but eosinophil differentiation was significantly increased (0.87 × 109/L, reference 0.02–0.52 × 109/L). Furthermore, C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) were mildly elevated (CRP 23.1 mg/L, reference 0–8 mg/L; ESR 34 mm/L, reference 0–20 mm/L) and procalcitonin (PCT) was normal (0.10 pg/mL, 0–0.25 pg/mL). Knee aspiration revealed no evidence of bacterial infection. Radiographs demonstrated appropriate position and fixation of the cemented implants (Fig. 2), and a technetium-99m bone scan showed mild increased uptake around the prosthesis.
Figure 1.
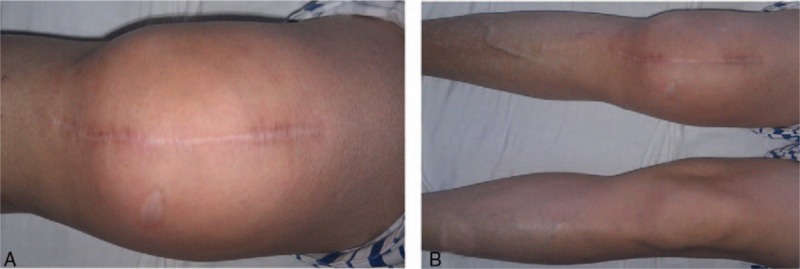
The patient's right knee is obviously swollen.
Figure 2.
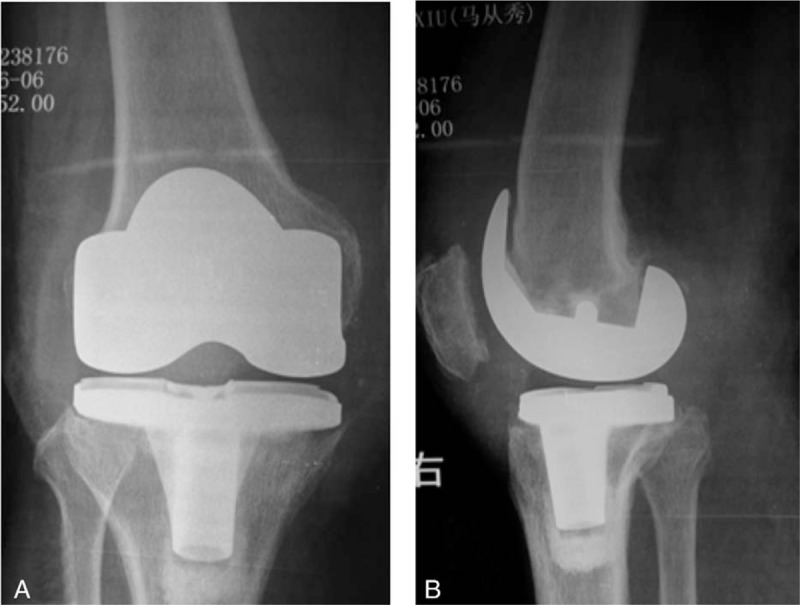
The implant is fixed well and the position is appropriate. (A) Anteroposterior radiograph. (B) Lateral radiograph.
As there was a possibility of PJI, she was scheduled for a debridement and revision TKA. However, no significant signs of infection were found during the operation. The only finding was obvious hyperplasia and hyperemia of synovial tissues surrounding the implant, particularly in the suprapatellar pouch (Fig. 3). A frozen biopsy revealed an extremely low volume of neutrophils, but a large amount of lymphocytes, which was verified by a postoperative pathology report (Fig. 4). The implant was well fixed and there is no evidence of PJI. Therefore, after examining all the available evidence, a diagnosis of metal hypersensitivity was made intraoperatively. Only the polyethylene tibial insert was changed as the implant was well fixed (Fig. 5). To suppress the allergic reaction, anti-anaphylactic treatment (promethazine hydrochloride, 25 mg im qd) was initiated immediately after the revision surgery.
Figure 3.
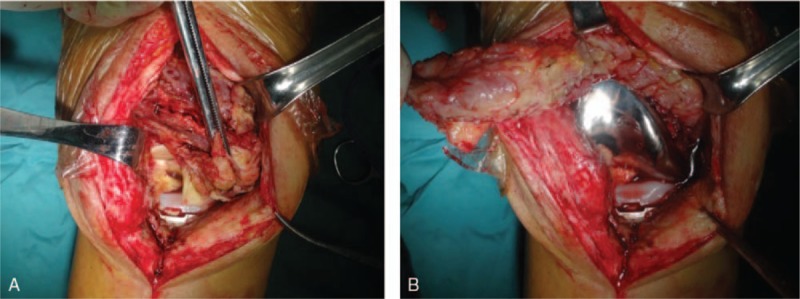
The image shows both hyperplasia and congestion of the synovial tissues. The implant was fixed well and prosthetic joint infection was not observed.
Figure 4.
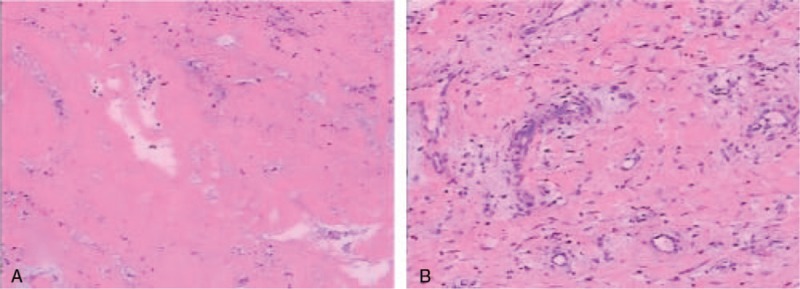
Photomicrograph of the tissues showing hyperplasia, glassy degeneration, and mucoid degeneration of fibrous tissue and blood vessel. Acute or chronic inflammatory cell infiltrates are present in the necrotic tissue.
Figure 5.

The metal implant is fixed well and prosthetic joint infection is absent in the intraoperative presentation.
At day 3 postoperatively, intraoperative multiple site bacteria culture results returned negative. The differentiation of WBC and neutrophils was normal. ESR, CRP, and PCT were mildly increased, but eosinophil differentiation was still significantly increased (1.30 × 109/L, reference 0.02–0.52 × 109/L). The patient experienced significant symptom relief and was discharged home on postoperative day 14.
At 4 years of follow-up, the patient's right knee remained mildly swollen; however, the pain has been relieved significantly. The ROM could achieve 0° of extension and 90° of flexion. The levels of all inflammatory markers were within the normal range and eosinophil differentiation was also normal.
3. Literature review
3.1. Prevalence of metal hypersensitivity
Strictly speaking, the prevalence of metal hypersensitivity discussed in this report was determined by the positive rate by 1 specific testing method, but did not cover the real incidence of this issue. In the general population, the prevalence is 10% to 15%[2,5,11] and the most common allergy-inducing metals are nickel (19.7–24.4%), cobalt (2–8.8%), and chromium (2.4–5.9%).[12] In some cases, cross-hypersensitivity reactions have been observed for all three metals.[3] However, the prevalence of metal allergy can be influenced by multiple factors. For example, female patients are more sensitive to nickel[25] and male patients to chromate.[13] The prevalence of metal hypersensitivity varies according to the status of the implant: it is found in 20% to 25% of patients with well-functioning implants and in approximately 60% of patients with poorly functioning implants or loosening prosthesis.[2,11] This phenomenon may be caused by the fact that the hypersensitivity reaction is elicited by continuous contact with metal ions; therefore, a loosening prosthesis could release more ions than an intact implant, thus inducing an allergic reaction.[14] Modern implants are all coated with plasma spray to limit metal ion exposure[2,15]; however, such coating could also provide a rough surface, which may increase the available area for ion release.
The most common composition of metallic implants for orthopedic surgery includes stainless steel, titanium alloy, cobalt-chromium-molybdenum alloy, and zirconium alloy.[7,8] Since these alloys contain different types of metals (stainless steel: 19% chrome, 15% nickel, 4% molybdenum, and 1% nickel, cobalt-chromium-molybdenum: 67% chrome, 30% cobalt, 2% molybdenum, and 1% nickel, titanium alloy: 91% titanium, 5% aluminum, 3.9% vanadium, and 0.1% nickel), their allergenicity varies substantially.[2,6,16] Stainless steel is widely used in internal fixation for trauma patients; therefore, metal allergy is more common in trauma patients than in patients undergoing TJA.
3.2. Laboratory tests for metal hypersensitivity
Clinical symptoms of metal hypersensitivity include local or systemic allergic dermatitis, such as eczema, urticaria, bullous eruption, erythema multiforme, and vasculitis.[17,18] Surgical site pain, aseptic inflammation, and prosthetic loosening are also common manifestations.[5] Different metal ions may induce diverse allergic symptoms, for example: nickel ions may create implant loosening, and release of chrome can cause eczema and other skin problems.[19,20]
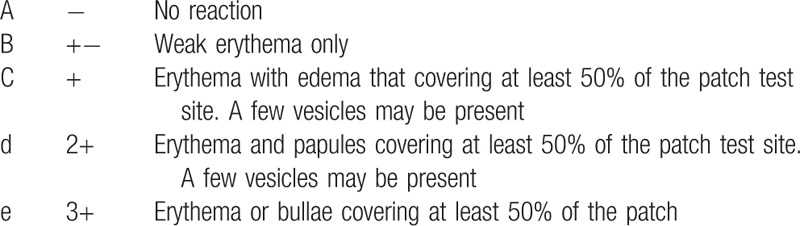
With respect to standard laboratory examinations, the skin patch test, leukocyte migration inhibition test (LMIT), and lymphocyte transformation test (LTT) are the most popular diagnostic tests for metal hypersensitivity. None of the tests have been universally accepted and applied. The skin patch test is easier and cheaper than in vitro tests; therefore, it is more widely used in clinical settings and is more suitable for larger-scale screening. However, the antigen-presenting cells (APCs) localized to the skin are dendritic cells and epidermal Langerhans cells, while systemic APCs are macrophages and monocytes. This difference invalidates this test.[4,10,21] According to previous reports, the sensitivity of patch test is as high as 100%, but its specificity is quite low (64%). Although a diagnosis of metal hypersensitivity can be excluded with confidence following a negative patch test result, a positive test result may not provide much valuable information.[11] In fact, many patients with positive patch test results may never display any symptoms of metal hypersensitivity.[15,21] The reaction grading of the skin patch test is listed in (Table 1).[22]
Table 1.
The reaction grading of skin patch test.
The most common in vitro diagnostic tests for metal hypersensitivity are LMIT and LTT. The LMIT measures the limitation of leukocyte migration by detecting migration inhibitory factor or leukocyte migration inhibition factor (LIF). Those 2 factors can prevent lymphocytes from leaving a site where foreign antigens are present.[9] Thus, a positive result indicates an active immune response and metal sensitivity, and is closely associated with swelling, pain, and allergic dermatitis. After removing the allergen, the result of the test may turn negative,[2,19] therefore a serial test could be used to monitor response to therapy. The LTT measures the proliferation of lymphocytes activated by metal ions and indicates the cellular immune function. In that test, a radioactive marker is added to lymphocytes, and the proliferation factor is calculated by measuring radiation counts per minute of the incorporated marker.[23] LTT is more reliable than the skin patch test and is currently more widely performed than LMIT, but its clinical practicability is limited by the high cost and need for a specialized lab.[2,24]
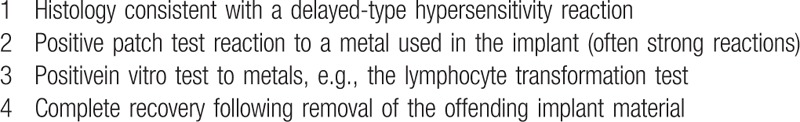
Thyssen et al have proposed objective diagnostic criteria for allergic metal dermatitis overlying the implant (Table 2) and objective criteria for metal-allergy-related prosthesis loosening, pain, and chronic inflammation (Table 3).[19]
Table 2.
The objective diagnostic criteria of allergic metal dermatitis overlying the implant.
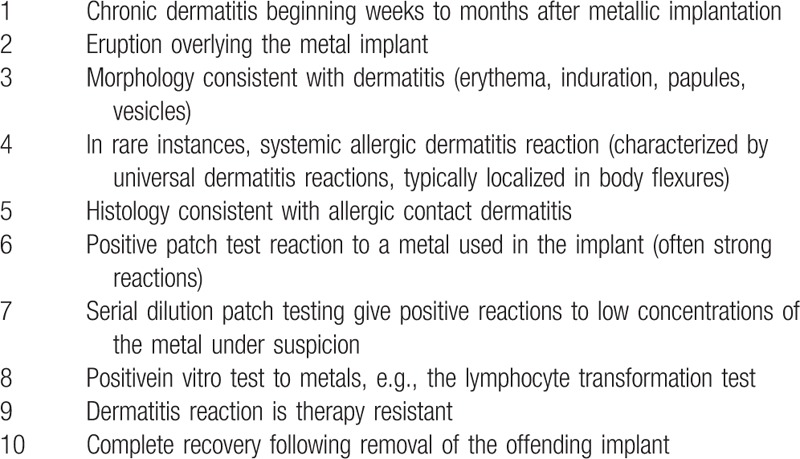
Table 3.
Objective criteria that metal allergy related implant loosening, pain, and chronic inflammation.
3.3. Treatment for implant hypersensitivity
Allergen removal is always the most effective treatment for all types of hypersensitivities. However, since revision surgery is associated with significant trauma, cost, and inferior survivorship of the prosthesis, nonsurgical treatment is considered to be the first choice in the setting of metal hypersensitivity following TJA. For mild eczema and other dermatitis, local dermatologic treatment is the treatment of choice. If the allergic symptoms are systemic, oral prednisolone may be a good choice. Radiosynoviorthesis has been reported to be effective in the treatment of recurrent joint effusions after total-knee replacement.[26] If all of the abovementioned options fail to produce satisfactory results, the prosthesis should be removed and revised with an oxidized zirconium Zr-2.5Nb alloy (Oxinium; Smith & Nephew, Memphis, TN).[6,27,28] Other implant options include Oxinium components for the femoral side and hardened titanium for the tibial side,[29] or revision with a titanium-niobium (Biomet or Stryker) prosthesis.[31,32]
4. Conclusion
Metal hypersensitivity following TJA is a poorly studied issue due to its extremely low incidence, vague clinical manifestations, and diagnostic difficulty. At present, no consensus has been reached to determine the best diagnostic criteria for this disease and most physicians would consider it only when other diseases like PJI have been excluded.[30] In our case, PJI also had to be excluded. Initially, the patient was diagnosed with an infection and debridement as well as revision surgery was planned. However, no signs of infection or positive culture results were demonstrated intra- and postoperatively. Instead, we observed an elevated eosinophil count, positive history of metal jewelry allergy, and significant hyperplasia of synovial tissues leading to the hypothesis of metal hypersensitivity.[33–35] A satisfactory outcome was achieved following synovectomy and anti-anaphylactic treatment, which further confirmed our hypothesis. Nevertheless, longer term follow-up is needed to better appreciate the progression of this condition.
Author contributions
Conceptualization: Yao He.
Data curation: Wei Bao.
Formal analysis: Wei Bao.
Investigation: Wei Bao, Jun Yuan Fuan, Yao He.
Supervision: Ming Yue Liao.
Writing – original draft: Wei Bao.
Wei Bao orcid: 0000-0003-3118-8109
Footnotes
Abbreviations: APCs = antigen-presenting cells, CRP = C-reactive protein, ESR = erythrocyte sedimentation rate, LIF = leukocyte migration inhibition factor, LMIT = leukocyte migration inhibition test, LTT = lymphocyte transformation test, PCT = procalcitonin, PJI = periprosthetic joint infection, ROM = range of motion, TJA = total-joint arthroplasty, TKA = total-knee arthroplasty, WBC = white blood count.
Ethical approval was not necessary for this manuscript, because it was a case report. Informed written consent was obtained from the patient for publication of this case report and accompanying images.
The authors report no conflicts of interest.
References
- [1].Jones CA, Beaupre LA, Johnston DW, et al. Total joint arthroplasties: current concepts of patient outcomes after surgery. Rheum Dis Clin North Am 2007;33:71–86. [DOI] [PubMed] [Google Scholar]
- [2].Hallab N. Metal sensitivity in patients with orthopaedic implants. J Clin Rheumatol 2001;7:215–8. [DOI] [PubMed] [Google Scholar]
- [3].Cadosch D, Chan E, Gautschi OP, et al. Metal is not inert: role of metal ions released by biocorrosion in aseptic loosening - current concepts. J Biomed Mater Res A 2009;91:1252–62. [DOI] [PubMed] [Google Scholar]
- [4].Caicedo MS, Desai R, McAllister K, et al. Soluble and particulate Co-Cr-Mo alloy implant metals activate the inflammasome danger signaling pathway in human macrophages: a novel mechanism for implant debris reactivity. J Orthop Res 2009;27:847–54. [DOI] [PubMed] [Google Scholar]
- [5].Basko-Plluska JL, Thyssen JP, Schalock PC. Cutaneous and systemic hypersensitivity reactions to metallic implants. Dermatitis 2011;22:65–79. [PubMed] [Google Scholar]
- [6].Gao X, He RX, Yan SG, et al. Dermatitis associated with chromium following total knee arthroplasty. J Arthroplasty 2011;26: 665.e13-6. [DOI] [PubMed] [Google Scholar]
- [7].Thienpont E, Berger Y. No allergic reaction after TKA in a chrome-cobalt-nickel-sensitive patient: case report and review of the literature. Knee Surg Sports Traumatol Arthrosc 2013;21:636–40. [DOI] [PubMed] [Google Scholar]
- [8].Hallab NJ, Jacobs JJ. Biologic effects of implant debris. Bull NYU Hosp Jt Dis 2009;67:182–8. [PubMed] [Google Scholar]
- [9].Hallab NJ, Caicedo M, Finnegan A, et al. Th1 type lymphocyte reactivity to metals in patients with total hip arthroplasty. J Orthop Surg 2008;3:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Hallab NJ, Caicedo M, Epstein R, et al. In vitro reactivity to implant metals demonstrates a person-dependent association with both T-cell and B-cell activation. J Biomed Mater Res A 2010;92:667–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Granchi D, Cenni E, Tigani D, et al. Sensitivity to implant materials in patients with total knee arthroplasties. Biomaterials 2008;29:1494–500. [DOI] [PubMed] [Google Scholar]
- [12].Uter W, Rämsch C, Aberer W, et al. The European baseline series in 10 European Countries, 2005/2006 - results of the European Surveillance System on Contact Allergies (ESSCA). Contact Dermatitis 2009;61:31–8. [DOI] [PubMed] [Google Scholar]
- [13].Basketter DA, Briatico-Vangosa G, Kaestner W, et al. Nickel, cobalt and chromium in consumer products: a role in allergic contact dermatitis? Contact Dermatitis 1993;28:15–25. [DOI] [PubMed] [Google Scholar]
- [14].Savarino L, Granchi D, Ciapetti G, et al. Ion release in patients with metal-on-metal hip bearings in total joint replacement: a comparison with metal-on-polyethylene bearings. J Biomed Mater Res 2002;63:467–74. [DOI] [PubMed] [Google Scholar]
- [15].Niki Y, Matsumoto H, Otani T, et al. Screening for symptomatic metal sensitivity: a prospective study of 92 patients undergoing total knee arthroplasty. Biomaterials 2005;26:1019–26. [DOI] [PubMed] [Google Scholar]
- [16].Osman RB, Elkhadem AH, Ma S, et al. Titanium versus zirconia implants supporting maxillary overdentures: three-dimensional finite element analysis. Int J Oral Maxillofac Implants 2013;28:e198–208. [DOI] [PubMed] [Google Scholar]
- [17].Kubba R, Taylor JS, Marks KE. Cutaneous complications of orthopedic implants. A two-year prospective study. Arch Dermatol 1981;117:554–60. [PubMed] [Google Scholar]
- [18].Eben R, Walk R, Summer B, et al. Implant allergy register - a first report [in German]. Orthopade 2009;38:557–62. [DOI] [PubMed] [Google Scholar]
- [19].Thyssen JP, Menné T, Schalock PC, et al. Pragmatic approach to the clinical work-up of patients with putative allergic disease to metallic orthopaedic implants before and after surgery. Br J Dermatol 2011;164:473–8. [DOI] [PubMed] [Google Scholar]
- [20].Jacobs JJ, Hallab NJ. Loosening and osteolysis associated with metal-on-metal bearings: a local effect of metal hypersensitivity? J Bone Joint Surg Am 2006;88:1171–2. [DOI] [PubMed] [Google Scholar]
- [21].Schalock PC, Menné T, Johansen JD, et al. Hypersensitivity reactions to metallic implants - diagnostic algorithm and suggested patch test series for clinical use. Contact Dermatitis 2012;66:4–19. [DOI] [PubMed] [Google Scholar]
- [22].Drake LA, Ceilley RI, Cornelison RL, et al. Guidelines of care for contact dermatitis. Committee on Guidelines of Care. J Am Acad Dermatol 1995;32:109–13. [DOI] [PubMed] [Google Scholar]
- [23].Jacobs JJ, Campbell PA, T Konttinen Y, et al. How has the biologic reaction to wear particles changed with newer bearing surfaces? J Am Acad Orthop Surg 2008;16(Suppl 1):S49–55. [DOI] [PubMed] [Google Scholar]
- [24].Thomas P, Bandl WD, Maier S, et al. Hypersensitivity to titanium osteosynthesis with impaired fracture healing, eczema, and T-cell hyperresponsiveness in vitro: case report and review of the literature. Contact Dermatitis 2006;55:199–202. [DOI] [PubMed] [Google Scholar]
- [25].Lai DW, Saver JL, Araujo JA, et al. Pericarditis associated with nickel hypersensitivity to the Amplatzer occluder device: a case report. Catheter Cardiovasc Interv 2005;66:424–6. [DOI] [PubMed] [Google Scholar]
- [26].Mayer-Wagner S, Mutzel B, Mayer W, et al. Radiosynoviorthesis for treating recurrent joint effusions after endoprosthetic knee replacement. Clin Nucl Med 2012;37:727–31. [DOI] [PubMed] [Google Scholar]
- [27].Thakur RR, Ast MP, McGraw M, et al. Severe persistent synovitis after cobalt-chromium total knee arthroplasty requiring revision. Orthopedics 2013;36:e520–4. [DOI] [PubMed] [Google Scholar]
- [28].Post ZD, Orozco FR, Ong AC. Metal sensitivity after TKA presenting with systemic dermatitis and hair loss. Orthopedics 2013;36:e525–8. [DOI] [PubMed] [Google Scholar]
- [29].Thomsen M, Rozak M, Thomas P. Pain in a chromium-allergic patient with total knee arthroplasty: disappearance of symptoms after revision with a special surface-coated TKA - a case report. Acta Orthop 2011;82:386–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Osmon DR, Berbari EF, Berendt AR, et al. Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis 2013;56:e1–25. [DOI] [PubMed] [Google Scholar]
- [31].Holt G, Murnaghan C, Reilly J, et al. The biology of aseptic osteolysis. Clin Orthop Relat Res 2007;460:240–52. [DOI] [PubMed] [Google Scholar]
- [32].Thyssen JP, Jakobsen SS, Engkilde K, et al. The association between metal allergy, total hip arthroplasty, and revision. Acta Orthop 2009;80:646–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Firestone TP, Eberle RW. Surgical management of symptomatic instability following failed primary total knee replacement. J Bone Joint Surg Am 2006;88(Suppl 4):80–4. [DOI] [PubMed] [Google Scholar]
- [34].Salin JW, Lombardi AV, Jr, Berend KR, et al. Acute gouty arthropathy after total knee arthroplasty. Am J Orthop (Belle Mead NJ) 2008;37:420–2. [PubMed] [Google Scholar]
- [35].Bunting D, Kampa R, Pattison R. An unusual case of pigmented villonodular synovitis after total knee arthroplasty. J Arthroplasty 2007;22:1229–31. [DOI] [PubMed] [Google Scholar]


