Abstract
A novel approach to advanced electronic health record (EHR) skills training was developed in a large healthcare organization to improve high-quality EHR documentation, while reducing stressors linked to physician burnout.
The 3-day intensive EHR education intervention covered best practices in EHR documentation and physician well-being. The specialty physician faculty used interactive teaching including demonstration, facilitation, and individual coaching. Laptops were provided for hands-on practice. Mixed-method evaluation included real-time feedback, daily surveys, and post-activity surveys to measure participant learning and satisfaction, and also collection of performance data from the EHR to measure use of order sets designed to improve quality of care.
Since 2014, 46 trainings were held with 3500 physicians. Most physicians (85%–98% across all programs) reported improved quality, readability, and clinical accuracy of documentation; fewer medical errors; and increased efficiency in chart review and data retrieval due to the training. Seventy-eight per cent estimated a time savings of 4 to 5 minutes or more per hour. Physician performance data from the EHR showed significant improvement in use of order sets for several critical health conditions such as sepsis, stroke, and chest pain of possible cardiac cause.
This advanced EHR training for physicians was well-received and improved physicians’ use of several order sets designed to improve quality of care. EHR training programs such as this may have impact on the safety, quality, accuracy, and timeliness of care and may also help reduce physician burnout by improving critical skills and reducing time interfacing with all aspects of a patient's health record.
Keywords: EHR, electronic health record, electronic medical record, health care, healthcare providers, healthcare quality, healthcare safety, health informatics, health information technology, medical documentation, medical education, physician burnout, physician education, physician wellness, training
1. Introduction
Most healthcare organizations have adopted the use of electronic health records (EHRs) and provide initial training for clinicians.[1,2] While there is a great deal of evidence to show that hands-on learning and spaced repetition are highly effective to sustain learning,[3] there is little evidence in the literature showing that this is being done to support EHR learning after initial training. Additionally, most articles on EHR describe training on the technology, and not on the impact of technology on the individual users.[4–6] Nothing was found to describe a human-centered approach to EHR training.
A 2016 research study by the American Medical Association concluded that “for every hour physicians provide direct clinical face time to patients, nearly 2 additional hours are spent on EHR and desk work within the clinic day (p. 753).”[7] Outside of office hours, physicians spend another 1 to 2 hours of personal time each night doing additional computer work.[7] The study also noted that unintentional consequences of the time spent documenting in the EHR are gradually gaining recognition including impact on performance metrics, impaired communication with patients, increased career dissatisfaction, and burnout among physicians.[7]
Kaiser Permanente Southern California has taken a novel systems approach to ongoing EHR training for physicians, in ambulatory and inpatient care, to address retention and reinforcement of training, and also the challenges of physician burnout related to time spent on EHR documentation. In this article, we describe the advanced EHR education approach that Kaiser Permanente Southern California designed, developed, implemented, and evaluated involving physicians from all specialties to ensure high-quality and accurate documentation, while reducing some of the key stressors linked to physician burnout.
2. Methods
2.1. Education program rationale and goals
The initial concept for the educational intervention evolved from leadership discussions on 2 levels: a desire to help physicians manage their EHR in-basket workload, and increasing concerns about the literature describing physician burnout and suicide rates.[8] With healthcare reform, changes in practices, and the implementation of EHR systems, physicians were reporting that lack of time was the biggest barrier to improving many aspects of their practice.[7,9] The initial approach to reduce in-basket workload through EHR training, and job stress through a wellness program, evolved into a long-term strategy for an EHR advanced training, with a goal of reducing EHR time by 5 minutes per hour, improving overall EHR skills, and integrating wellness into physicians’ everyday practice.
2.2. Program implementation
In 2009, the first small-scale version of the current EHR advanced training was developed as a local follow-up to initial training that all physicians received. In 2011, an emergency department (ED) 3-day region-wide intensive advanced EHR training was piloted. This was designed to advance high-quality documentation, while reducing key stressors linked to physician burnout. The success of the ED training led to the development of this education intervention for physicians from all 30 specialties in the Kaiser Permanente Southern California region. Executive leadership sponsorship was secured to support scheduling of physicians out of clinic for the full 3-day activity, and to provide the resources needed to manage implementation. An average of 75 physicians attended each training, with 3 to 4 trainings taking place concurrently at a hotel away from the physicians’ day-to-day work. From 2014 to 2016, 8 specialty-specific trainings were developed: Adult Primary Care, Pediatrics, Obstetrics/Gynecology, In-patient, Surgery, Medical Specialties, Psychiatry, and Emergency Medicine. Additional activities continue to be developed, including 1 for the Anesthesia specialty. While all specialties were invited to the training, the Pathology and Radiology specialties’ needs and workflows are different enough from the other medical specialties that few of these physicians attended, though some did attend and found it valuable. It is expected that over the next 5-year period, there will be opportunities to provide this educational intervention to all physicians in Kaiser Permanente Southern California region.
2.3. Instructional design
Education content and methodology were designed to engage physicians in optimizing EHR skills and wellness, and support transfer of learning back to the workplace. The training opened with a video message of support and encouragement from an executive leadership sponsor to the physicians attending. Education content addressed objectives of implementing best practices in EHR documentation to improve efficiency, reliability, and patient safety. This included overcoming workflow challenges, creating accurate and timely orders and notes, and using decision-support order sets designed with evidence-based protocols and clinical guidelines. Additionally, participants received a notebook with screen shots of correct documentation practices, definitions, order set maps, data retrieval information, best practices, regulatory requirements, and examples and tips for writing electronic notes. Didactic sessions were kept to a minimum.
Education content also addressed physician well-being, with a focus on wellness tips, time to exercise, eating healthy meals, and learning relaxation techniques. Faculty members were specialty physician peers who were trained to address workflow and EHR performance issues. They used highly interactive methods of instruction including demonstration, facilitated group discussion, and individual coaching for participants who were provided with laptops linked to their clinic computer for hands-on practice and “build time” to personalize tools. These were designed to help return 5 minutes per hour back to each physician in their clinic work, through reduced in-basket time and optimization of the EHR system. Humorous vignettes were interspersed to reduce the impact of 3 long days of learning. Support personnel were on-site to work directly with the physicians. All methodologies were purposefully designed to help reinforce learning throughout the training and support the transfer of learning back into the workplace. Additional approaches included video examples, optional EHR laboratories for additional hands-on “build time” to personalize tools on their clinic computer, and trained support personnel back at their workplace.
2.4. Evaluation methods
This education intervention was evaluated using mixed methods and multiple data sources: just-in-time feedback, end-of-day surveys, post-activity surveys, and collection of performance data from the EHR.
-
1.
Just-in-time feedback was designed to respond to participants’ immediate learning needs. This was accomplished by a computer tool that allowed participants to type in questions that were monitored by faculty, who could respond immediately by adding or clarifying content.
-
2.
End-of-day surveys were designed to assess participants’ perceived value and remaining challenges on the topics addressed that day. This was done via another computer-based tracking tool, with results reviewed daily by faculty and adjustments made to the next day of training as needed.
-
3.
Post-activity surveys were designed to collect qualitative and quantitative data, to assess self-reported competence and performance, and also perceived impact of this education intervention on physician practice. Surveys were conducted both immediately after the 3-day training to assess the participants’ intent to change based on session objectives, and 3 months post-training to assess perceptions of self-reported behavioral change as a result of participating in this education intervention. Specific questions addressed whether the training resulted in improvements in evidence-based ordering, decreased time used to respond to patient messages in the in-basket, maximized EHR functionality for greater quality, improved clinical accuracy, and reduced documentation time, and also increased efficiency in chart review, data retrieval, and searching for patient information.
-
4.
EHR performance data were tracked for the subset of physicians who completed the Emergency Medicine or Inpatient trainings in 2016. Among this group, physicians’ use of specialty-specific EHR order sets was measured in the year preceeding the training and the year after the training, that is, 2015 and 2017. Order sets are a grouping of orders for procedures, laboratories, and medications that are linked to a condition such as stroke or sepsis. These are tied to evidence-based clinical practice guidelines for treating this condition and provide a 1-stop place to effectively order the right things at the right time for a patient with a specific condition. Order sets are built in the system as a decision support tool to improve safety, physician accuracy, efficiency, and performance, and also patient care. Improvements in the use of these order sets indicate that protocols are being followed and are more likely to ensure that orders linked to a patient's condition(s) are not missed or delayed. Rates of specific order set usage were calculated for patients treated by physicians who participated in the training, by retrieving a list of order sets used, and numbers of patients hospitalized or seen in the ED. Rates of order set use per 10,000 patients were calculated by year (2015, pretraining vs 2017, post-training). Relative risks and 95% confidence intervals (CIs) were estimated to test for differences in order set use in 2017 compared with 2015. Statistical analysis was performed using Stata, version 14.2 (StataCorp: College Station, TX).
The Kaiser Permanente Southern California Institutional Review Board determined that our program evaluation was not human subjects’ research.
3. Results
In all, 3500 physicians from 30 specialties completed a total of 46 trainings from 2014 to 2016. Just-in-time feedback and end-of-day surveys were used to make minor daily adjustments to the training to meet individual participant needs. The feedback included suggestions on the speed of the presentation delivery and clarification of content. The changes were immediately integrated into the delivery and not further analyzed.
3.1. Post-activity surveys
Results from the survey conducted immediately after and 3 months after training were consistent across all specialties. Most physicians (85 to 98% across all trainings) self-reported improved quality, readability, and clinical accuracy of documentation, and also fewer medical errors, and increased efficiency in chart review and data retrieval. The majority of physicians (78%) reported an estimated time savings of 4 to 5 minutes or more per hour; 98% said they would recommend the training to their peers. Some of the most compelling survey responses were in the comments about which part of the course made the most impact or difference. Participant comments included the following:
-
1.
“This is potentially life altering and liberating”
-
2.
“I had already cashed out my retirement funds. After only two days of (this training), I now feel like I have another 10 years work left in me!”
-
3.
“This course is a true action to improve our lives and reduce physician burnout. Letting us get through our day earlier due to the automation and efficiency taught in this course allows us to go home on time and actually use the gym, and do the things that we have not been doing when we get burned out. So thank you so much to those whom make this course possible. Might be a life saver for one or two of us.”
-
4.
“I really was dreading coming to this conference but have really learned so much. Time passes so quickly. I love how we learn a trick and then get to “build” before moving on.
-
5.
“I really liked the little extra touches like yoga, healthy food and stretching with our ergonomics staff.”
-
6.
“Southern California Permanente Medical Group spends a lot of money on physician wellness and trying to prevent physician burnout. Of all the programs they have, I think this is the most effective. Being efficient in the office reduces stress on the provider, creates a positive atmosphere and ultimately makes for happier patients. Every provider should experience this.”
-
7.
“The faculty staff [sic] was AMAZING. The information and time to work on the taught material was invaluable BUT the course content, format and faculty made it even more invaluable. I cannot express how much this is needed- especially in a time we need to work more efficiently and prevent burn out.”
The areas that were reported as the biggest challenges after leaving the training were breaking of old patterns, worrying about not remembering what was learned, and not having enough time to continue to build personalized content.
3.2. EHR performance data
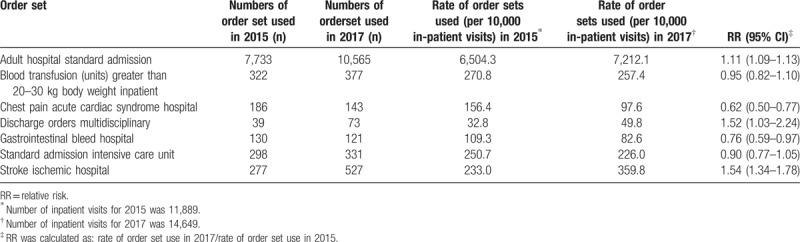
Tables 1 and 2 show ED and Inpatient order set usage results between 2015 and 2017 among physicians who completed the training in 2016. Order sets are designed to improve quality of care, help ensure protocols are being followed, and orders linked to patient's condition(s) are not missed or delayed. There were significant changes in the use of many ordersets post training.
Table 1.
Rates of use of selected emergency department order sets in 2015 and 2017, among emergency medicine physicians who completed the advanced EHR skills training (Kaiser Permanente HealthConnect Essentials) in 2016.
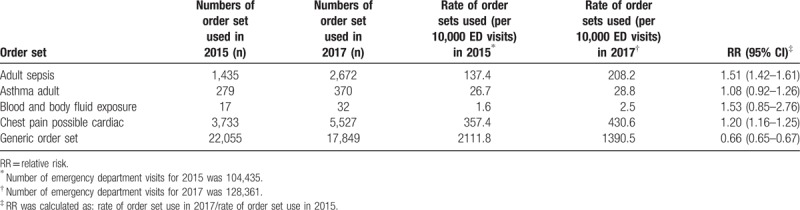
Table 2.
Rate of use of selected inpatient order sets in 2015 and 2017, among hospitalist physicians who completed the advanced EHR skills training (Kaiser Permanente HealthConnect Essentials) in 2016.
The ED results showed the following:
A 51% increase in use of the Adult Sepsis order set
A 20% increase in use of the Chest Pain/Possible Cardiac order set
A 34% decrease in use of the Generic order set
The ED results showed no significant changes in the Adult Asthma and Blood and Body Fluid Exposure order set use.
Inpatient results showed the following:
A 54% increase in use of the Stroke-Ischemic Hospital order set
A 52% increase in use of the Discharge Orders-Multidisciplinary order set
A 11% increase in use of the Adult Hospital Standard Admission order set
A 48% decrease in use of the Chest Pain Acute Cardiac Syndrome Hospital order set
A 24% decrease in use of the Gastrointestinal Bleed Hospital order set
Inpatient results showed no significant changes in the Blood Transfusion and the Standard Admission Intensive Care Unit order set use.
4. Discussion
A thorough review of the literature revealed that this is the largest group of physician cohorts to be tracked on multiple variables in the use of EHR to improve clinical performance, patient care, and physician wellness. An estimated savings of 4 to 5 minutes per hour could translate to 40 to 60 minutes per day on EHR documentation. This was a desired outcome related to physician wellness, considering that time spent on EHR documentation had earlier been reported as a stressor. Additional survey responses, as noted, showed physicians’ improvement in their performance and patient care.
The order set increases in ED Adult Sepsis, ED Chest Pain/Possible Cardiac, and Inpatient Stroke-Ischemic are significant, as they are 3 areas where timeliness of getting these patients treated is critical to reduce morbidity risks and mortality.[10–12] All of these order sets support early detection, diagnosis, and treatment.
The decrease in the ED generic order set is significant, demonstrating that physicians are moving toward using more specific order sets and away from using a more generic one (which has greater risks of missing a customized order for patients).
The ED Adult Asthma order set use was already performing well. A small increase is showing appropriate improvement. The ED Blood and Body Fluid Exposure order set had a high penetration level from the first 2 years of the training (a 42% increase), so only a small increase was reflected between 2015 and 2017.
Inpatient order set increases in Adult Hospital Standard Admissions and Discharge Orders-Multidisciplinary were significant in that these order sets are designed to drive towards improvements that meet regulatory requirements, Health Effectiveness Data and Information Set (HEDIS) measures, and publicly reported gaps. The Inpatient Chest Pain Acute Cardiac Syndrome order set was previously used for all chest pain, so the decrease in use of this is showing that this order set is now being used specifically for Acute Cardiac Syndrome, which is the correct use of this order set. This is also the case for the Inpatient Gastrointestinal Bleed order set where a more specific order set has replaced this more generic one.
Optimizing EHR skills has had an impact on patient safety and care. It has begun to lessen the burden of a large portion of physicians’ daily work, by improving critical skills and reducing time interfacing with all aspects of a patient's health record. These results are limited to the short-term outcomes from 2014 to 2017. The duration will need to be expanded to document the long-term impact of this education intervention on physician wellness, clinical performance, and patient care. A potential factor that may have influenced results was the implementation of additional clinical training on related concurrent organization-wide clinical initiatives, such as sepsis care improvement. This was considered, but not analyzed, because the organization-wide initiatives focused on clinical training and results, whereas this program focused on EHR training and related results.
Broader applications of this educational intervention could be considered. This approach can support multiple forms of crucial medical documentation, considering the wider field of health information technology. This training approach could also be adapted for use in other medical settings outside of Kaiser Permanente. In addition, it might be helpful to develop similar educational interventions for other staff who regularly interface with the electronic medical record.
The past 4 years have consistently demonstrated that this innovative education intervention—which integrates physician wellness approaches with clinical EHR training—is contributing to improved physician performance and well-being. As participants improve their productivity, efficiency, and patient care, they may rediscover a pathway back to the reason they initially entered health care.
Next steps for this education intervention include continuing improvements in training delivery and outcomes. To sustain improvements in the Southern California region, physician educators from the various medical centers are reaching out to the leadership at their sites to implement site-based education. Adjunct strategies are being added such as on-line education, and a website for collaboration and education reinforcement resources. Furthermore, regions within the Kaiser Permanente Healthcare system are beginning to adopt a similar education process, with an aim to achieve similar outcomes.
5. Other information: lessons for practice
-
1.
Advanced EHR education can improve crucial documentation that impacts quality, safety, accuracy, and timeliness of care.
-
2.
Combining EHR education content with physician wellness approaches, in a highly interactive, personalized, hands-on workshop setting, results in improved physician performance and well-being.
-
3.
The continuous feedback, learning, and improvement help facilitate ongoing communication with leadership, faculty, and participants to keep this education intervention fresh, with on-going support from all stakeholders.
Acknowledgments
We give special thanks to the following individuals for their dedication to improving the practice of medicine through excellence in education: Dixie Shearouse, MHA; Christine M. Ruygrok, RN, MBA; Mark Eastman, MD; and Gregorio Saccone, MD, for their vision and leadership of this program; Edward Ellison, MD, Todd Sachs, MD; and Annie J. Russell, RN, MSN, MBA for leading the organization and always sponsoring ways to improve patient care, physician/staff wellness, and improvements in medicine; Melanie Moore, MAEd; Davida Becker, PhD; Adam Bernier, and Agnella Izzo Matic, PhD, for help with medical writing, editing and data analysis.
Author contributions
Conceptualization: Kenneth E. Robinson, Joyce A. Kersey.
Data curation: Kenneth E. Robinson, Joyce A. Kersey.
Formal analysis: Kenneth E. Robinson, Joyce A. Kersey.
Methodology: Kenneth E. Robinson, Joyce A. Kersey.
Project administration: Kenneth E. Robinson, Joyce A. Kersey.
Resources: Kenneth E. Robinson, Joyce A. Kersey.
Validation: Kenneth E. Robinson, Joyce A. Kersey.
Writing – original draft: Joyce A. Kersey.
Writing – review & editing: Kenneth E. Robinson, Joyce A. Kersey.
Footnotes
Abbreviations: ED = emergency department, EHR = electronic health record.
Funding: Funding for the education program described in this article was provided by Southern California Permanente Medical Group.
The authors report no conflicts of interest.
References
- [1].Office of the National Coordinator for Health Information Technology. Office-based Physician Electronic Health Record Adoption. Health IT Quick Stat #50; December 2016. Available at: https://dashboard.healthit.gov/quickstats/pages/physician-ehr-adoption-trends.php. Accessed February 8, 2017. [Google Scholar]
- [2].Office of the National Coordinator for Health Information Technology. Non-federal acute care hospital electronic health record adoption. Health IT Quick Stat #47; May 2016. Available at: https://dashboard.healthit.gov/quickstats/pages/FIG-Hospital-EHR-Adoption.php. Accessed February 8, 2017. [Google Scholar]
- [3].Brown PC, Roediger HL, III, McDaniel MA. Make it Stick: the Science of Successful Learning. Cambridge, MA: Belknap Press; 2014. [Google Scholar]
- [4].Bornstein S. An integrated EHR at Northern California Kaiser Permanente. Appl Clin Inform 2012;3:318–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Pantaleoni JL, Stevens LA, Mailes ES, et al. Successful physician training program for large scale EMR implementation. Appl Clin Inform 2015;6:80–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Rizer MK, Kaufman B, Sieck CJ, et al. Top 10 lessons learned from electronic medical record implementation in a large academic medical center. Perspect Health Inf Manag 2015;12:1g. [PMC free article] [PubMed] [Google Scholar]
- [7].Sinsky C, Colligan L, Prgomet M, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med 2016;165:753–60. [DOI] [PubMed] [Google Scholar]
- [8].Peckham C. Medscape Physician Lifestyle Report 2017; January 11, 2017. Available at: http://www.medscape.com/features/slideshow/lifestyle/2017/overview. Accessed June 8, 2017. [Google Scholar]
- [9].Babbott S, Manwell LB, Brown R, et al. Electronic medical records and physician stress in primary care: results from the MEMO study. J Am Med Inform Assoc 2014;21:e100–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: International guidelines for management of severe sepsis and septic shock: 2012. Critical Care Med 2013;41:580–637. [DOI] [PubMed] [Google Scholar]
- [11].Antman EM, Hand M, Armstrong PW, et al. 2007 focused updated of the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients with ST-Elevation Myocardial Infarction). J Am Coll Cardiol 2008;151:210–47. [DOI] [PubMed] [Google Scholar]
- [12].Jauch EC, Saver JL, Adams HP, et al. Guidelines for the early management of patients with acute management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013;44:870–947. [DOI] [PubMed] [Google Scholar]


