Abstract
Complicated Meckel's diverticulum represents a common etiology of acute abdomen in children. However, this condition is less frequent in adults. We reviewed the records of adult patients who underwent the surgical removal of complicated Meckel's diverticulum between 2001 and 2017 at 2 tertiary French medical centers. We then analyzed the clinical characteristics, mode of presentation, and management for all patients.
The Meckel's diverticulum was resected in 37 patients (24 males and 13 females). The mean patient age was 46.1 ± 21.4 years. The most common clinical presentations of complicated Meckel's diverticulum were diverticulitis (35.1%, n = 13), small-bowel obstruction (35.1%, n = 13), and gastrointestinal bleeding (29.8%, n = 11) (anemia, n = 1; hematochezia, n = 10). Age distribution was significantly different (P = .02) according to the 3 Meckel's diverticulum complications: patients with diverticulitis (P = .02) were statistically more frequently over 40 (P = .05), significantly older than patients with gastrointestinal bleeding who were more frequently <40 (P = .05). There was a preoperative diagnosis available for 15 of the 37 patients (40%). An exploratory laparoscopy was necessary to determine the cause of disease for the other 22 patients (60%). An intestinal resection was performed in 33 patients (89%) and diverticulectomy was performed in 4 patients (11%). There was heterotopic tissue found in only 6 patients (16%). Postoperative complications were as follows: 1 death by cardiac failure in a 92-year-old patient and 2 patients with postoperative wound infections. The follow-up time was 3 to 12 months.
The correct diagnosis of complicated Meckel's diverticulum in adults is difficult due to the lack of specific clinical presentation. As a result, exploratory laparoscopy appears to play a central role in cases of acute abdomen with uncertain diagnosis.
Keywords: diverticulitis, gastrointestinal hemorrhage, intestinal obstruction, Meckel's diverticulum, surgery
1. Introduction
Meckel's diverticulum (MD) is the most prevalent congenital anomaly of the gastrointestinal (GI) tract. The condition results from incomplete omphalomesenteric (vitelline) duct obliteration and affects approximately 2% of the general population.[1] MD is localized at the antimesenteric border of the ileum in the axis and continuity of the superior mesenteric artery. There is a 3:2 male-to-female prevalence ratio.[2] Complicated MD represents a significant cause of morbidity in children, and more than 50% of patients who develop complications are under 10 years of age.[3] However, this condition is reported to be less frequent in adults. MD usually remains asymptomatic throughout the patient's lifetime and is discovered incidentally on radiographic imaging, during endoscopy, or at the time of surgery.[4] The lifetime incidence rate of complications arising in patients with MD is approximately 4%.[5] The most common presentations associated with complicated MD are bleeding, intestinal obstruction, and diverticulitis. A limited number of studies have focused on this condition in the adult population. Therefore, the objective of this study was to investigate the clinical features of complicated MD in adults to guide general surgeons and improve early diagnosis.
2. Materials and methods
We retrospectively reviewed all adult patients more than 18 years old who underwent surgical removal of a complicated MD at European Georges Pompidou University AP HP hospital in Paris and Avicenne University APHP hospital in Bobigny, which are tertiary French medical centers.
We obtained a favorable ethical approval to conduct this study and to publish the results at the first session of 2018 (01012018). The databases at the Department of Pathology, European Georges Pompidou University APHP hospital in PAris, France and at Avicenne University APHP hospital in Bobigny, France were screened for surgical specimens of MD obtained between January 2001 and June 2017. The following data were collected by retrospective medical record review: demographic variables, preoperative diagnosis, diagnostic method, and pathology data. All patients had complete blood tests performed on the day of hospital admission. All computed tomography (CT) scans were performed with and without intravenous (IV) contrast. No oral contrast was routinely used. From 2001 to 2010, all CT examinations were obtained with 16-detectors scanners, and after 2010 with 64-detectors CT scans. However, for all examinations, the abdominal images were generally reconstructed and displayed with a 2.5-mm slice thickness using the conventional back projection and similar soft tissue filters, which provided basically the same image quality over the entire study. We separated the study period in 2 (before and after 2010) to compare the CT scan ability in preoperatively detecting a complicated MD.
In all cases of GI bleeding, initial emergency explorations were gastroscopy, colonoscopy, and CT scans with and without IV contrast. We define obscure GI bleeding as a persistent or recurrent bleeding for which no definitive source has been identified by an initial evaluation. We define obscure GI bleeding as “occult,” when it was not visible (patients with anemia), and as “overt,” when it manifests with a continued passage of visible blood (patients with hematochezia).
Laparoscopy was used in 2 situations: first, when an MD was suspected by preoperative explorations and second, when a small-bowel bleeding was evidenced by video-capsule endoscopy (VCE) or endoscopies, laparoscopy was performed as the first step before intraoperative enteroscopy (IOE) to locate the bleeding. In some cases, an IOE was performed after to exclude another cause.
Quantitative values were compared using t test and Mann–Whitney test as required to compare 2 groups. To compare more than 2 groups, a Kruskal–Wallis test was used. Qualitative variables of the 3 groups (diverticulitis vs GI bleeding vs obstruction) were compared using chi-squared test. Statistical significance was P < .05. All analyses were performed using SAS for Windows (SAS Institute, Inc, Cary, NC).
3. Results
3.1. Age and sex distribution
A total of 37 patients underwent surgical removal of a complicated MD. There were 24 males and 13 females, and the male–female ratio was 1.8:1. The patient age range was 18 to 92 years, and the mean patient age was 46.1 ± 21.4 years (Fig. 1).
Figure 1.
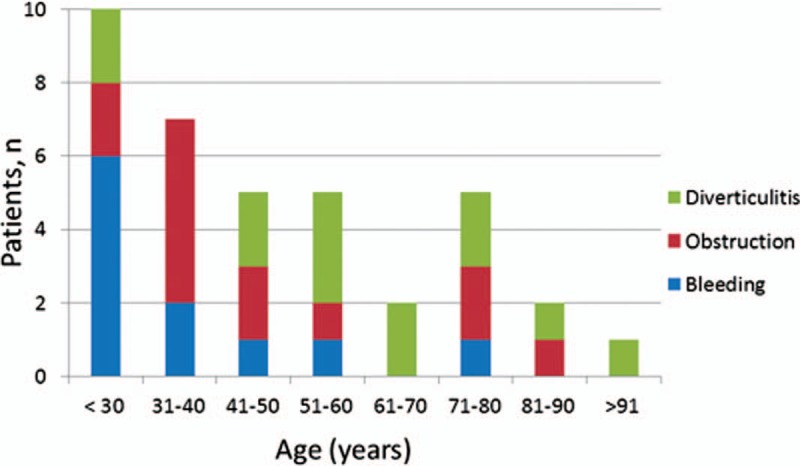
Frequency of complicated Meckel's diverticulum by age in 37 adult patients. Age of patient distribution was significantly different according to the 3 Meckel's diverticulum complications (P = .02): patients with diverticulitis were statistically more frequently over 40 (P = .05), patients with gastrointestinal bleeding were more frequently <40 and significantly younger than those with diverticulitis and intestinal obstruction (P = .05).
3.2. Clinical presentation
The most common clinical presentations of complicated MD included diverticulitis (35.1%, n = 13), small-bowel obstruction (35.1%, n = 13), and obscure GI bleeding (29.8%, n = 11). In 1 case, obscure GI bleeding was occult (anemia) and in 10 patients, it was overt (hematochezia) (Table 1). The age distribution in our cohort was significantly different according to the 3 MD complications (P = .02).
Table 1.
Demographical, clinical, and biological data associated with 37 complicated Meckel's diverticulum.
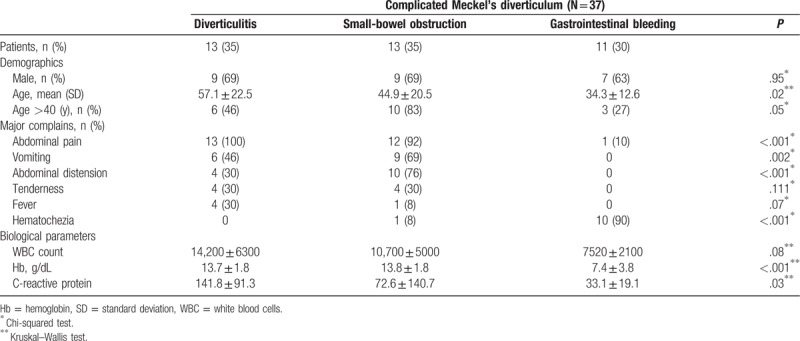
There were 13 patients who presented with diverticulitis (35.1%), including 11 patients with perforated diverticulitis. The mean age in patients with diverticulitis was 57.1 ± 22.5 years, and the group was statistically older than patients with GI bleeding (P = .02). Patients with complicated MD and diverticulitis were frequently older than 40 years of age (P = .05). Patients with complicated MD and GI bleeding were frequently younger than 40 years of age (P = .05).
The major complaints leading to explore MD in patients with diverticulitis were abdominal pain (100%), vomiting (50%), tenderness (33%), abdominal distension (33%), and fever (33%). There was a statistical correlation between abdominal pain and MD with diverticulitis (P < .001).
There was a small-bowel obstruction present in 13 patients (35.1%), including 4 patients who presented with band, 5 patients who presented with volvulus, and 4 patients who presented with intussusception. The mean age of patients with small-bowel obstructions was 44.9 ± 20.5 years. In addition, 83% of patients in this group were older than 40 years old. The major complaints prior to surgery in this patient group were abdominal pain (92%), abdominal distension (83%), vomiting (75%), and tenderness (33%). The presence of vomiting and abdominal distension were correlated with MD with small-bowel obstruction (P = .002 and P < .001, respectively).
There was lower GI bleeding in 11 patients (29.8%), and 10 of these patients (91%) presented with obscure GI bleeding (of unknown origin after gastroscopy and colonoscopy) that required multiple blood transfusions. The mean age in this group was 34.3 ± 12.6 years. The patients with GI bleeding were frequently younger than 40 years old (73%). Patients presenting with GI bleeding were statistically younger than the patients with diverticulitis or obstruction (P = .02). The major complaints leading to further medical explorations in this group were hematochezia (10 patients, 91%) and refractory iron deficiency anemia in 1 patient. Hematochezia was strongly correlated with MD with lower GI bleeding (P < .001). The blood hemoglobin (g/dL) and C-reactive protein levels were statistically lower in patients with MD with GI bleeding (P < .001 and P = .03, respectively) (Table 1).
3.3. Diagnostic method
CT scans with IV contrast were performed in all 37 patients of our population on the day of hospital admission. In addition, we performed successive GI endoscopy and VCE in patients presenting with GI bleeding (11 patients). A technetium pertechnetate scan (Meckel's scan) or enteroscan was performed in 2 patients in whom CT, GI endoscopy, and VCE were not informative.
The preoperative diagnosis of MD was determined in 15 of 37 patients (40%) (Table 2). Computed tomography (CT) was used to diagnose 9 of these 15 patients (60%), with 5 patients in the “diverticulitis” group, and 4 patients in the “small-bowel obstruction” group. However, none of the patients in the “GI bleeding” group were correctly diagnosed by CT. VCE guided the diagnosis in 4 patients (36%) presenting with MD with GI bleeding. In 1 patient, the Meckel's scan detected a hot spot in the lower right abdomen that indicated GI bleeding. In another patient, an enteroscan revealed a digestive hemorrhage.
Table 2.
Diagnostic method and surgical management in 37 patients with complicated Meckel's diverticulum.
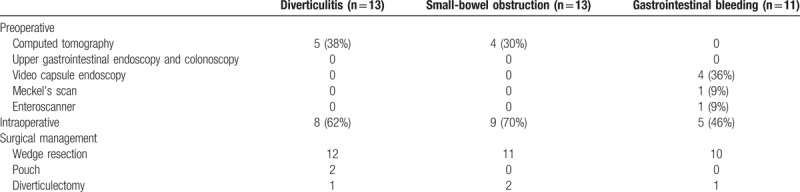
CT scan ability in preoperatively detecting a complicated MD before (2/22) and after 2010 (5/15) was not significantly different (P = .438).
The diagnosis of MD was not possible in 22 patients (60%) and an exploratory laparoscopy was necessary to determine the cause of disease. There were 7 patients (53%) in the “diverticulitis” group, 9 patients (69%) in the “small-bowel obstruction” group, and 5 patients (46%) in the “GI bleeding” group. There were 2 patients in the “GI bleeding” group who required an IOE to exclude another cause of bleeding.
Laparoscopy was used in 2 situations: first, when an MD was suspected by preoperative explorations, a laparoscopy was performed and second, when a small-bowel bleeding was evidenced by VCE or endoscopies, laparoscopy was performed as the first step before IOE to locate the bleeding.
3.4. Histopathological findings
A histopathological analysis was performed in all resected diverticula. Within the cohort of 37 resected diverticula, there were 6 patients (16%) with histologically abnormal tissue that contained ectopic gastric or pancreatic mucosa. There were 3 patients who presented with intussusception, and the other 3 patients presented with lower GI bleeding. Malignancies were not identified in any patients.
3.5. Surgical management
The surgical removal of complicated MD was performed in all 37 patients included in our study. An intestinal resection was performed in 33 patients (89%) and a diverticulectomy was performed in 4 patients (11%) (Table 2). There were 2 patients treated with intestinal resection who required a stoma. Both of these patients presented with perforated diverticulitis.
3.6. Surgical outcomes
In our study, all patients underwent surgery successfully. A remission of the symptoms was achieved in all cases. Postoperative complications were as follows: 1 death by cardiac failure in a 92-year-old patient; and 2 postoperative wound infections. The follow-up time was 3 to 12 months.
4. Discussion
Our data indicate that diverticulitis, small-bowel obstruction, and GI bleeding were the most common clinical presentations in adults and were present in 35.1%, 35.1%, and 29.8% of patients, respectively.
We also found that the patient age distribution in our cohort was significantly different according to the 3 MD complications (P = .02): patients with diverticulitis were statistically more frequently over 40 years old (P = .05), significantly older than patients with GI bleeding who were more frequently <40 years old. According to our knowledge, this is the first report that has examined the association between the clinical presentation and the age in adults presenting with MD complications. Few other studies[6,7] also reported a decreasing frequency of complicated MD with age, but they did not analyze separately each mode of clinical presentation and the age at onset of complications.
Diverticulitis and small-bowel obstruction are the most common presentations in adult series. Patients with diverticulitis account for 41% to 58% of the complicated MD population,[4,5,8–11] and our study shows a similar proportion (35.1%). Furthermore, small-bowel obstruction accounts for 23% to 41% of patients,[5,7,9–11] and our study shows a similar percentage (35.1%). Finally, GI bleeding accounts for 8% to 18% of patients.[5,9–11] Our study shows GI bleeding was present in 29.8% of patients. This higher rate could be related to a bias in patient selection. Our 2 university hospitals are tertiary centers involved in the management of obscure GI bleeding.[12]
The study by Park et al[7] reported a higher proportion of GI bleeding (38%) and a lower proportion of diverticulitis (28%), which contrasts the finding reported by other studies. The difference could be explained by the inclusion of patients between 11 and 20 years old in the adult population. Within the 180 adult patients examined in the study, there were 57 (32%) cases <20 years old. Thus, by choosing an 11-year-old age cut-off for adults, their “adult population” represents a pediatric population. Previous studies reported the clinical presentations of the disease may differ between pediatric populations and adults.
In the pediatric population, GI bleeding and small-bowel obstruction are the most common presentations, and diverticulitis is rare.
GI bleeding usually presents as obscure overt (meaning with hematochezia) and massive bleeding that requires blood transfusions. Bleeding accounts for 44% to 59% of complicated MD in children.[2,3,13]
Small-bowel obstruction revealing a complicated MD accounts for 38% to 40% in children[13–15] and usually presents with intussusception or volvulus.[13] Diverticulitis is less frequently reported in children than in adults (12–14%).[13,14]
The clinical arguments are nonspecific and rarely lead to the diagnosis of complicated MD. Moreover, despite the advancement of technology, the use of diagnostic methods, including multidetector CT, upper GI endoscopy and colonoscopy, technetium pertechnetate scan, or VCE, are unable to diagnose complicated MD in adults.
In our series, a preoperative diagnosis of complicated MD was possible in 15 patients (40%).
The diagnostic accuracy of CT scanning for the detection of MD was previously considered too low for clinical use because it is not possible to distinguish between diverticulum and intestinal loops.[16] The modern multidetector CT can use IV injection of iodinated contrast and/or peroral bowel opacification to increase the detection of MD and complications such as diverticulitis.[17] In our series, MD was detected by CT in 5 of the 13 patients (38%) with diverticulitis and in 4 of the 13 patients (30%) with small-bowel obstruction. However, CT was unable to diagnose the 9 patients with GI bleeding.
Despite the regular increase in the power of multidetector CT scans in our 2 hospitals, the CT scan ability to preoperatively diagnose MD was not significantly improved: CT scan made the preoperative diagnosis of complicated MD in 4/22 cases before 2010 and in 5/15 cases after 2010 (P = .438). Complete exploration of small-bowel is difficult, and identifying the bleeding site of a GI hemorrhage remains challenging. Upper GI endoscopy and colonoscopy play minimal roles because MD is inaccessible for evaluation.[18] Technetium-99m-labeled erythrocyte scintigraphy is also referred to as the Meckel's scan and has an overall positive yield of approximately 50%.[19] Another interesting diagnostic tool is VCE, which is reported to be a highly sensitive (95%) and specific (75%) technique that detects bleeding in patients with obscure GI bleeding.[20]
The 9 patients in our series presenting with obscure GI bleeding were diagnosed using VCE in 3 patients (36%) and 99mTc-pertechnetate-scintigraphy in 1 patient (9%).
The preoperative diagnosis of complicated MD was not possible in 21 patients (60%), and an exploratory laparoscopy was necessary to determine the cause of disease. In our study, laparoscopy was used in 2 situations: first, when an MD was suspected by preoperative explorations and second, when a small-bowel bleeding was evidenced by VCE or endoscopies, laparoscopy was performed as the first step before IOE to locate the bleeding.
In 2 patients in the “GI bleeding” group, an IOE was performed to exclude other causes of bleeding. IOE is an excellent method of exploring the entire small bowel and has a diagnostic yield of 80% when combined with explorative laparotomy.[12] However, when an intraoperative cause for GI bleeding is discovered, the use of IOE is not recommended to exclude other causes due to his high morbidity.[21]
The surgical management of complicated MD should consist of a wedge resection with primary anastomosis. A laparoscopic approach for complicated MD has proven safe and feasible in pediatric and adult populations.[22] In addition, diverticulectomy using linear staplers was reported as safe if the resected specimen is inspected to ensure all ectopic mucosa are removed.[23]
The management of an uncomplicated MD is still controversial. Historically, the prophylactic removal of uncomplicated MD was not recommended due to the low lifetime incidence of complications.[5,6,24] A prophylactic diverticulectomy has been proposed for incidental MD at any age up to 80 because of the increasing lifetime risk of surgery for MD-related complications.[25] Finally, previous authors proposed removing MD in patients with the following risk factors for complications: age younger than 50 years old, male, length of diverticulum more than 2 cm, and presence of histologically abnormal tissue.[7]
The main bias of our series is its retrospective nature. The number of complicated resected MD could have been lowered because some of complicated MD could have been misinterpreted or misclassified, for example, as jejuna diverticula. In addition, the number of uncomplicated resected MD was unfortunately not recorded. However, the guidelines of our 2 surgery departments are not to remove uncomplicated MD. This number was probably very low.
Our series counts a small number of patients. However, complicated MD is a rare and unusual condition and prospective data have poor chances to be performed.
5. Conclusion
The diagnosis of complicated MD in adults remains a challenge. The diagnosis of complicated MD should be considered in any adult patient with obscure GI bleeding especially in patients <40 years old. A complicated MD should be evocated in case of acute small-bowel obstruction in a patient with neither past history of neither abdominal surgery nor evidence of hernia. In addition, the occurrence of MD-related diverticulitis is more frequently observed in patients over than 40 years old but cannot be easily differentiated for other small-bowel diverticulitis. There is a central role for exploratory laparoscopy when an unclear abdominal process is observed to correct the diagnosis of complicated MD.
Author contributions
Conceptualization: Jean-Marc Chevallier, Marco Gucci, Philippe Wind, Richard Douard.
Data curation: Alina Parvanescu, Matthieu Bruzzi, Camille Tilly, Marco Gucci, Philippe Wind.
Formal analysis: Thibault Voron, Marco Gucci, Richard Douard.
Investigation: Alina Parvanescu.
Methodology: Alina Parvanescu, Thibault Voron, Richard Douard.
Project administration: Richard Douard.
Software: Matthieu Bruzzi.
Supervision: Richard Douard.
Validation: Richard Douard.
Writing – original draft: Alina Parvanescu.
Writing – review & editing: Matthieu Bruzzi, Franck Zinzindohoué, Jean-Marc Chevallier, Philippe Wind, Anne Berger, Richard Douard.
Footnotes
Abbreviations: CT = computed tomography, GI = gastrointestinal, IOE = intraoperative enteroscopy, IV = intravenous, MD = Meckel's diverticulum, VCE = video-capsule endoscopy.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Johns TN, Wheeler JR, John FS, et al. Meckel's diverticulum and Meckel's diverticulum disease: a study of 154 cases. Ann Surg 1959;150:241–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Tseng YY, Yang YJ. Clinical and diagnostic relevance of Meckel's diverticulum in children. Eur J Pediatr 2009;168:1519–23. [DOI] [PubMed] [Google Scholar]
- [3].Menezes M, Tareen F, Saeed A, et al. Symptomatic Meckel's diverticulum in children: a 16-year review. Pediatr Surg Int 2008;24:575–7. [DOI] [PubMed] [Google Scholar]
- [4].Yamaguchi M, Takeuchi S, Awazu S. Meckel's diverticulum. Investigation of 600 patients in Japanese literature. Am J Surg 1978;136:247–9. [DOI] [PubMed] [Google Scholar]
- [5].Soltero MJ, Bill AH. The natural history of Meckel's diverticulum and its relation to incidental removal. A study of 202 cases of diseased Meckel's diverticulum found in King County, Washington, over a fifteen year period. Am J Surg 1976;132:168–73. [DOI] [PubMed] [Google Scholar]
- [6].Leijonmarck CE, Bonman-Sandelin K, Frisell J, et al. Meckel's diverticulum in the adult. Br J Surg 1986;73:146–9. [DOI] [PubMed] [Google Scholar]
- [7].Park JJ, Wolff BG, Tollefson MK, et al. Meckel diverticulum: the Mayo Clinic experience with 1476 patients (1950–2002). Ann Surg 2005;241:529–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Chen JJ, Lee HC, Yeung CY, et al. Meckel's diverticulum: factors associated with clinical manifestations. ISRN Gastroenterol 2014;2014:390869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Groebli Y, Bertin D, Morel P. Meckel's diverticulum in adults: retrospective analysis of 119 cases and historical review. Eur J Surg 2001;167:518–24. [DOI] [PubMed] [Google Scholar]
- [10].Stone PA, Hofeldt MJ, Campbell JE, et al. Meckel diverticulum: ten-year experience in adults. South Med J 2004;97:1038–41. [DOI] [PubMed] [Google Scholar]
- [11].Diamond T, Russell CF. Meckel's diverticulum in the adult. Br J Surg 1985;72:480–2. [DOI] [PubMed] [Google Scholar]
- [12].Douard R, Wind P, Berger A, et al. Role of intraoperative enteroscopy in the management of obscure gastrointestinal bleeding at the time of video-capsule endoscopy. Am J Surg 2009;198:6–11. [DOI] [PubMed] [Google Scholar]
- [13].Huang CC, Lai MW, Hwang FM, et al. Diverse presentations in pediatric Meckel's diverticulum: a review of 100 cases. Pediatr Neonatol 2014;55:369–75. [DOI] [PubMed] [Google Scholar]
- [14].St-Vil D, Brandt ML, Panic S, et al. Meckel's diverticulum in children: a 20-year review. J Pediatr Surg 1991;26:1289–92. [DOI] [PubMed] [Google Scholar]
- [15].Durakbasa CU, Okur H, Mutus HM, et al. Symptomatic omphalomesenteric duct remnants in children. Pediatr Int 2010;52:480–4. [DOI] [PubMed] [Google Scholar]
- [16].Rossi P, Gourtsoyiannis N, Bezzi M, et al. Meckel's diverticulum: imaging diagnosis. Am J Roent 1996;166:567–73. [DOI] [PubMed] [Google Scholar]
- [17].Kawamoto S, Raman SP, Blackford A, et al. CT detection of symptomatic and asymptomatic Meckel diverticulum. AJR 2015;205:281–91. [DOI] [PubMed] [Google Scholar]
- [18].Szold A, Katz LB, Lewis BS. Surgical approach to occult gastrointestinal bleeding. Am J Surg 1992;163:90–2. [DOI] [PubMed] [Google Scholar]
- [19].Tabibian JH, Wong Kee Song LM, Enders FB, et al. Technetium-labeled erythrocyte scintigraphy in acute gastrointestinal bleeding. Int J Colorectal Dis 2013;28:1099–105. [DOI] [PubMed] [Google Scholar]
- [20].Hartmann D, Schmidt H, Bolz G, et al. A prospective 2-center study comparing wireless capsule endoscopy with intraoperative enteroscopy in patients with obscure GI bleeding. Gastrointest Endosc 2005;61:826–32. [DOI] [PubMed] [Google Scholar]
- [21].Voron T, Rahmi G, Bonnet S, et al. Intraoperative enteroscopy: is there still a role? Gastrointest Endosc Clin N Am 2017;27:153–70. [DOI] [PubMed] [Google Scholar]
- [22].Hosn MA, Lakis M, Faraj W, et al. Laparoscopic approach to symptomatic Meckel diverticulum in adults. JSLS 2014;18:00349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Chan KW, Lee KH, Mou JW, et al. Laparoscopic management of complicated Meckel's diverticulum in children: a 10-year review. Surg Endosc 2008;22:1509–12. [DOI] [PubMed] [Google Scholar]
- [24].Peoples JB, Lichtenberger EJ, Dunn MM. Incidental Meckel's diverticulectomy in adults. Surgery 1995;118:649–52. [DOI] [PubMed] [Google Scholar]
- [25].Cullen JJ, Kelly KA, Moir CR, et al. Surgical management of Meckel's diverticulum: an epidemiologic, population-based study. Ann Surg 1994;220:564–9. [DOI] [PMC free article] [PubMed] [Google Scholar]


