Abstract
The depressive symptoms have been associated with increased disabilities, and the depressive symptoms-related elevation of high C-reactive protein (CRP) has been proposed as a possible mechanism. We examined the relations between CRP and depressive symptoms among the middle-aged and elderly in China.
A longitudinal sample of the middle-aged and elderly (4404 men and 5055 women) who were interviewed in the 2011 China Health and Retirement Longitudinal Study was used. A multivariate logistic regression analysis was used to examine the effects of sociodemographic characteristics, lifestyle, activity status, physical exercise, systolic blood pressure, low-density lipoprotein (LDL), high-density lipoprotein (HDL), triglycerides, body mass index (BMI), and CRP levels on depressive symptoms.
The mean age in the study was 60.26 years [standard deviation (SD) ± 9.25; 46.56% men]. The mean CPR level was 2.79 mg/L (range, 0.01–178.10; SD ± 7.80). Depression scores ranged from 0 to 30 with a mean 8.65 (SD ± 6.33). The prevalence of depressive symptoms was 38.49% in the total population, 31.04% in men and 44.99% in men. Compared with baseline CRP levels (≤1.00 mg/L), the depressive symptoms are only weakly correlated with CRP levels among women [CRP 1.01–3.00 mg/L: odds ratio (OR) = 0.85, 95% confidence interval (CI) = 0.73–0.98; CRP 3.01–10.00 mg/L: OR = 1.25, 95% CI = 1.03–1.51; CRP >10 mg/L: OR = 1.41, 95% CI = 1.06–1.88]. After adjusting for age, education, marital status, hukou, residence, cigarette smoking, alcohol drinking, eating meals, activity status, major accidental injury, diseases, health status, physical exercise, systolic blood pressure, LDL, HDL, triglycerides, and BMI, depressive symptoms were not associated with subsequent high CPR levels among the middle-aged and elderly (CRP 1.01–3.00 mg/L: OR = 0.93, 95% CI = 0.83–1.03; CRP 3.01–10.00 mg/L: OR = 0.95, 95% CI = 0.82–1.10; CRP >10 mg/l: OR = 1.11, 95% CI = 0.88–1.39).
Our data do not support an association between CRP and depressive symptoms in both middle-aged and elderly men and women among china.
Keywords: body mass index, C-reactive protein, depressive symptoms, mid-aged and elderly
1. Background
Recently, depressive symptoms have become an important public health concern in general population in most countries. The Chinese population has begun aging and will continue to age rapidly in the future. In China, the prevalent of depressive symptoms is highly prevalent in elderly people,[1–3] and lead to increased risk of disabilities and mortality associated with chronic diseases.[4,5] The underlying mechanisms for depressive symptoms in elderly people remain unclear, but it is also possible that depressive symptoms may affect the development of chronic diseases through high sensitivity C-reactive protein (CRP). Depressive symptoms promote and maintain inflammatory responses by diminishing the immune system sensitivity.[6]
Several previous studies have examined the relationship between CRP and depressive symptoms.[7] However, the relationship between CRP and depressive symptoms is controversial, with several studies showing positive or null associations. Elovainio et al[8] conducted a study to investigate the correlation between depression and CRP in a representative sample of adults aged ≥30 years in Finland and found that inflammatory processes may induce depressive symptoms in men. Using a cross-sectional dataset of 641 healthy adults people aged 20 to 70 years enrolled at American Fallon Healthcare System, Ma et al[9] found that depression was correlated to hs-CRP levels in women, but not in men. Another research study conducted by Elovainio et al[10] showed that higher levels of depressive symptoms are associated with higher levels of CRP. Similar evidences of the positive associations have been found in other studies.[11–18] However, contradictory evidences have been found in several studies. Chaiton et al,[19] Douglas et al,[20] and Au et al[21] found no significance association between CRP and depressive symptoms in the general population.
Much of the literature has been limited by retrospective design and potential uncontrolled confounding. In addition, few studies have examined the association between CRP and depressive symptoms among general population in china. Therefore, this article focused on the relationship between CRP and depressive symptoms among the middle-aged and elderly in China after adjusting for potential confounders.
2. Methods
2.1. Study sample
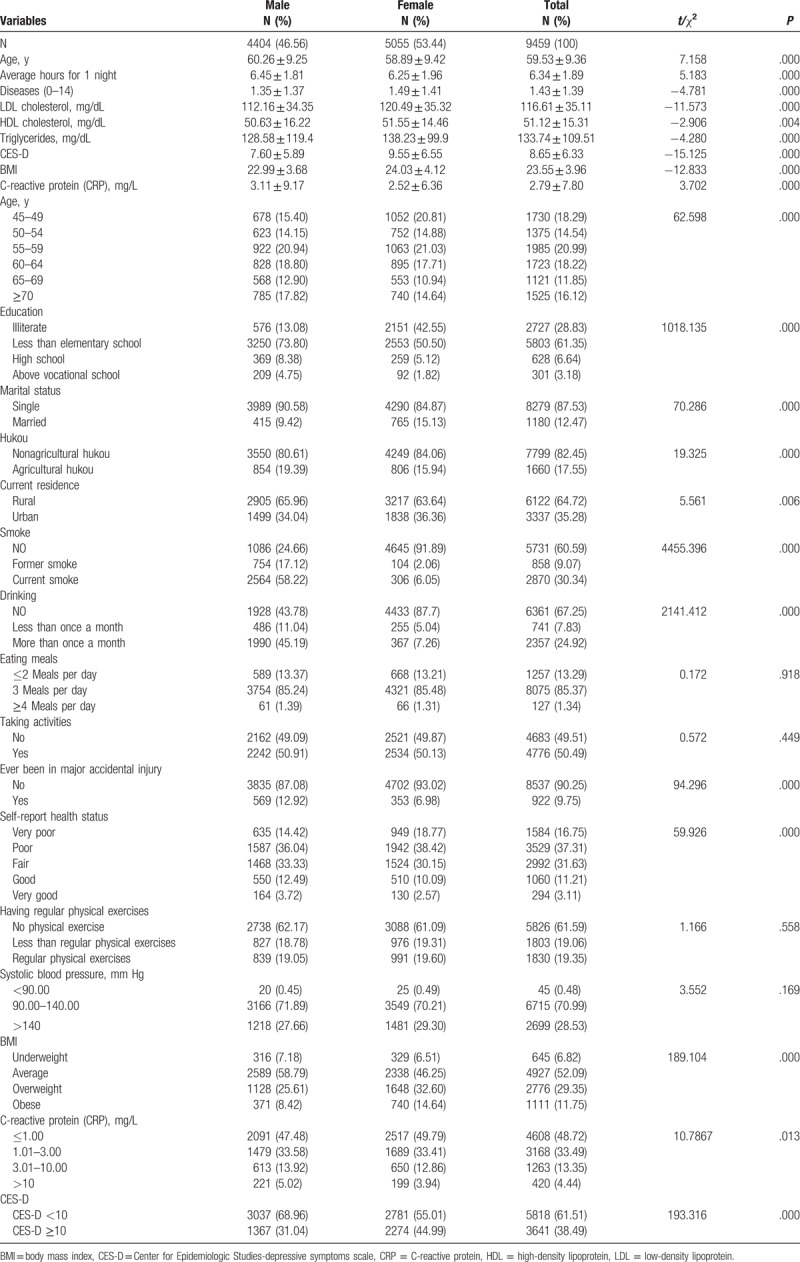
The 2011 Wave1of China Health and Retirement Longitudinal Study (CHARLS) sample (N = 9459) consists of 46.56% men [M = 60.26 years, standard deviation (SD) = 9.25; range, 45–93 years] and 53.44% women (M = 58.89 years, SD = 9.42; range, 45–96 years) participants; 6.64% and 3.18% of the respondents have completed high school and above vocational school education, respectively. By contrast, 28.83% of the respondents are illiterate or 61.35% received less than elementary school education; 64.72% of the participants live in rural, whereas 35.28% live in urban currently. Table 1 presents baseline characteristics of the sample for all variables in the research, and most variables based on our previous study.[22]
Table 1.
Baseline characteristics with full samples (N = 9459).
2.2. CRP measures
Venous blood samples were taken by the Center for Disease Control (CDC) station, and then immediately stored frozen at −20°C and transported to the Chinese CDC in Beijing within 2 weeks where they were placed in a deep freezer and stored at −80°C until assay at CMU laboratory. Low-density lipoprotein (LDL), high-density lipoprotein (HDL), and triglycerides were analyzed by the Youanmen Center for Clinical Laboratory at Capital Medical University using the enzymatic colorimetric test, and CRP was measured with immunoturbidimetric assay. We categorized CRP into 4 categories of CRP levels: ≤1.00, 1.01 to 3.00, 3.01 to 10.00, and >10 mg/L, the categorization has been used widely in previous studies.[17,23,24]
2.3. Depressive symptoms measures
The Chinese version of the Center for Epidemiologic Studies-Depression scale (CES-D) with a high reliability and validity has been widely used to measure depressive symptoms among Chinese.[25–28] It is a self-reported questionnaire that consists of 10 questions. Participants with a score of 10 or higher on the CES-D were classified as depressed.[29] The construct validity was 0.61 and the Cronbach alpha coefficient was 0.80.
2.4. Statistical analysis
Our data were used mean ± SD (continuous data) and number and percentage (categorical data) to express. Differences between men and women, or between the depressive symptoms and those with the normal or CRP categories were evaluated by t test or chi-square test, and chi-square test was followed by Bonferroni adjustment. The associations of depressive symptoms and CRP levels were first used binary logistic regression models, as appropriate. Then binary logistic regression models adjusting for 18 potential confounders [age, education, marital status, hukou, residence, cigarette smoking, alcohol drinking, eating meals, activity status, major accidental injury, diseases, health status, physical exercise, systolic blood pressure, LDL, HDL, triglycerides, and body mass index (BMI)] [30] were conducted to examine the odds ratio (OR) for depressive symptoms across a range of CRP. All data were analyzed by using SPSS version 17.0.
3. Results
The characteristics of our study subjects are shown in Table 1. 4404 (46.56%) of the participants were men, and 5055 (53.44%) of the participants were women. The average ages of the male and female participants were 60.26 ± 9.25 and 58.89 ± 9.42 years, respectively. Among all of the participants, 6.82% were underweight, 29.35% were overweight, and 11.75% were obese. Furthermore, regarding the men, 7.18% were underweight, 25.48% were overweight, and 8.16% were obese, whereas 6.51%, 32.60%, and 14.64% of the women were underweight, overweight, and obese, respectively. The mean value of the CRP was 2.79 ± 7.80 mg/L. The prevalence of depressive symptoms was 38.49% in the total population, 31.04% in men and 44.99% in women. Significant differences in distribution were observed between men and women in all of the variables, except eating habits, activity status, regular physical exercise, and systolic blood pressure.
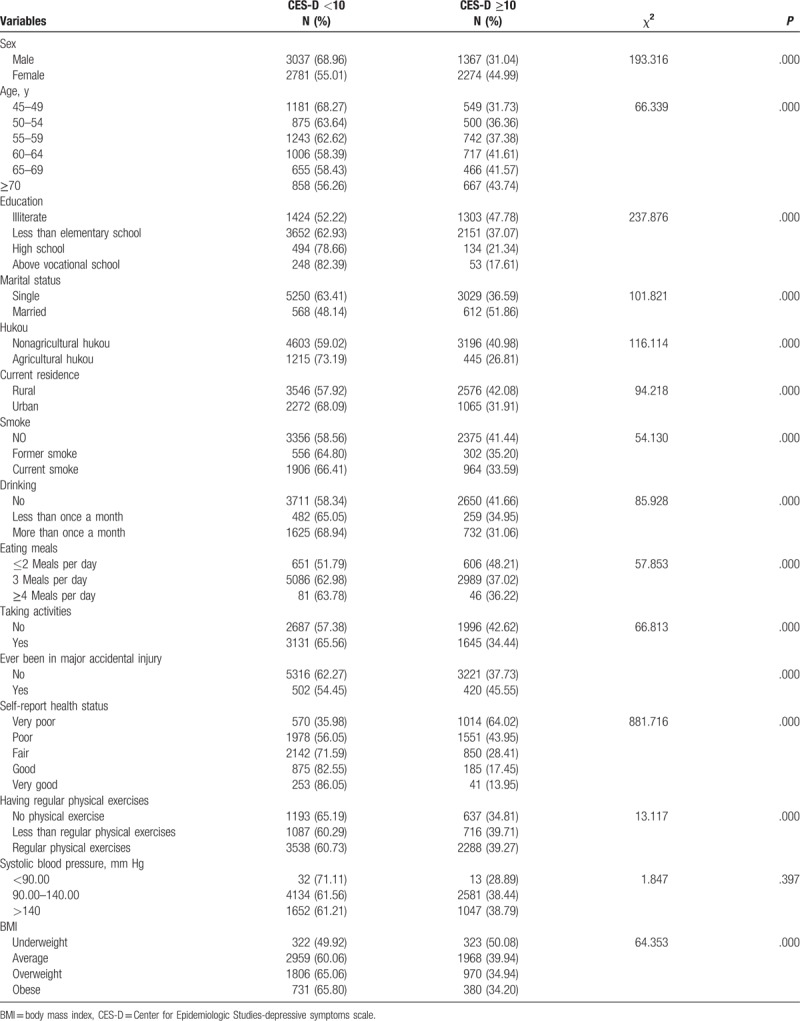
Tables 2 and 3 show the relationship of various characteristics and BMI in the participants. Only marital status, eating habits, activity status, major accidental injury, and physical exercise were not significantly different between the CRP groups in males (Table 2), and in females, only education, alcohol consumption, eating habits, major accidental injury, self-report health status, physical exercise, and CES-D categories were not significantly different between the CRP groups (Table 3). Table 4 shows the significantly different variables among the CES-D groups. The prevalence of depressive symptoms, assessed by the CES-D, differed among the variables except systolic blood pressure.
Table 2.
Baseline characteristics in male study population (N = 4404).
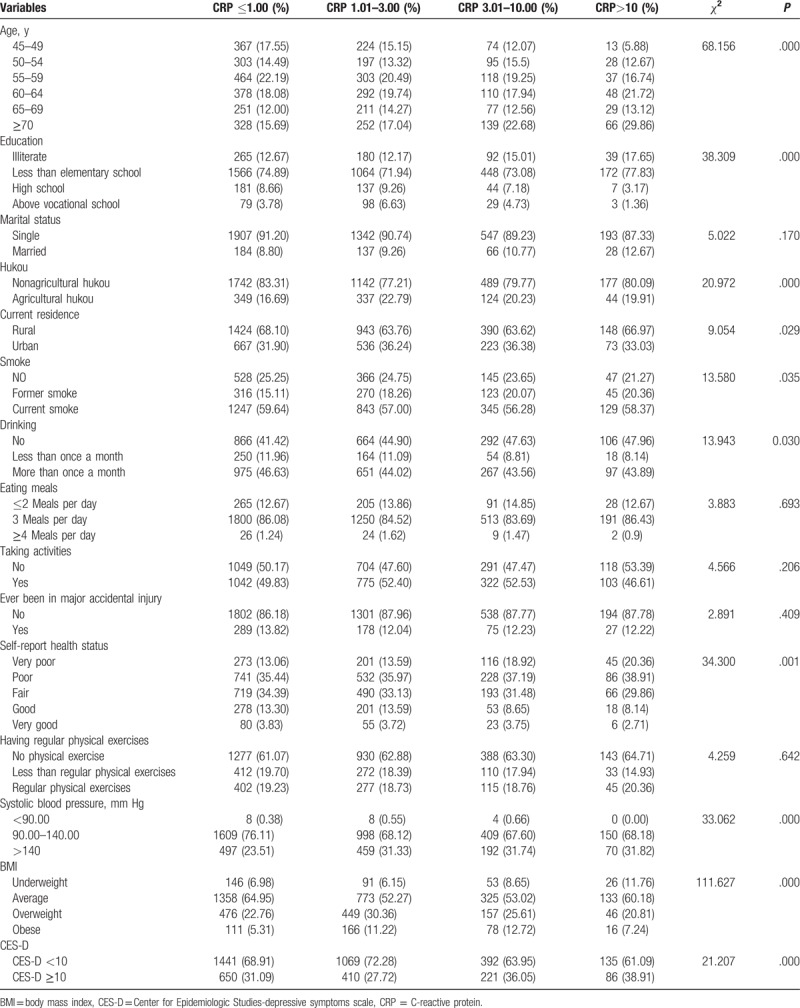
Table 3.
Baseline characteristics in female study population (N = 5055).
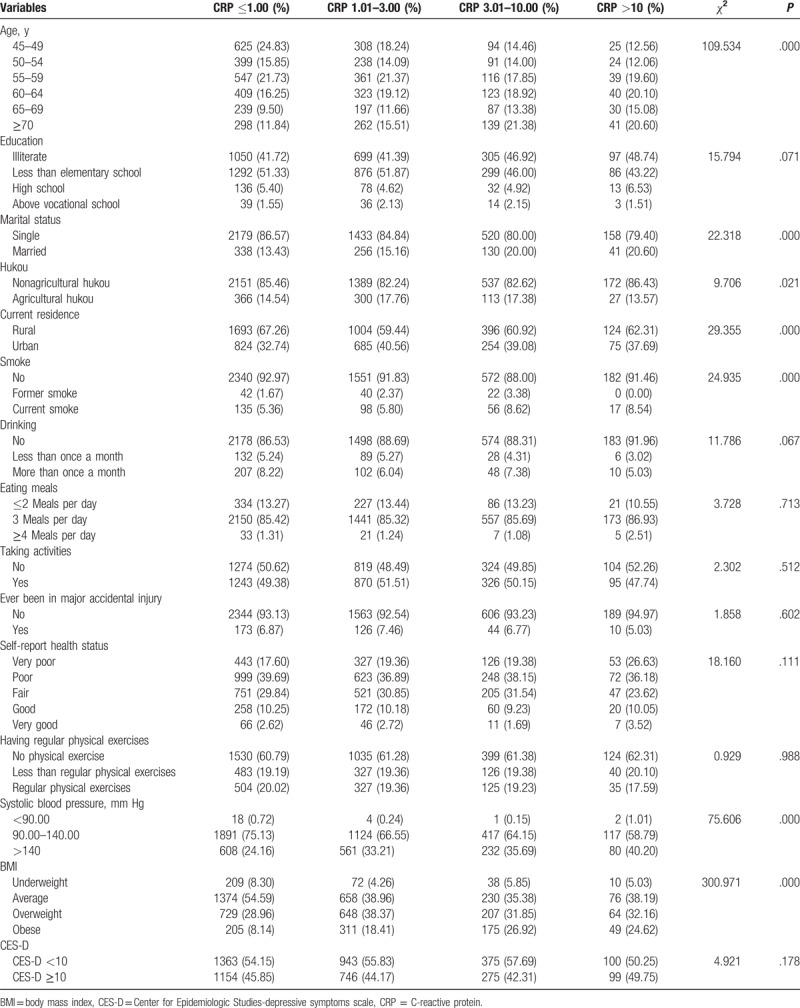
Table 4.
Relationship of various characteristics and depressive symptoms, chi-square test analyses of variance followed by Bonferroni adjustment (N = 9459).
To examine the association between CRP and depressive symptoms, we estimated depressive symptoms equation using binary logistic regression. The crude ORs and the associated 95% confidence intervals (CIs) are shown in Table 5. We controlled for the sociodemographic characteristics (age, education, marital status, hukou, residence), health behaviors (cigarette smoking, alcohol drinking, eating meals, activity status, physical exercise), health conditions (major accidental injury, diseases, health status), systolic blood pressure, and metabolic measures (LDL, HDL, triglycerides, and BMI), the estimation results of the depressive symptoms equation are reported in Table 6. Compared with baseline CRP levels (CRP ≤1.00 mg/L), the depressive symptoms are only weakly correlated with CRP levels among women (CRP 1.01–3.00 mg/L: OR = 0.85, 95% CI = 0.73–0.98; CRP 3.01–10.00 mg/L: OR = 1.25, 95% CI = 1.03–1.51; CRP >10 mg/L: OR = 1.41, 95% CI = 1.06–1.88). Several potential confounding factors were associated with CRP. After adjusting for age, sex, education, marital status, hukou, current residence, smoking habit, alcohol consumption, eating habits, activity status, major accidental injury, chronic diseases, health status, physical exercise, systolic blood pressure, LDL, HDL, triglycerides, and BMI, no association between CRP and depressive symptoms were observed in secondary analyses that stratified by sex (male, female).
Table 5.
Estimated crude odds ratios of depressive symptoms.
Table 6.
adjusting odds ratios and 95% confidence interval for C-reactive protein and depressive symptoms.
4. Discussion
In our study, we investigated the association between CRP and depressive symptoms among the middle-aged and elderly in China. Based on the Chinese version of the CES-D, the prevalence of depressive symptoms was 31.04% in men and 44.99% in women. The prevalence of depressive symptoms was higher compared with previous survey results. In the sample collected from the 1999 and 2003 Surveys of Health and Living Status of the Elderly in Taiwan,[30] the prevalence of depressive symptoms as measured by the CES-D (above the cutoff of 10) was 27.9% in men and 36.2% in women in 2003. The prevalence of depressive symptoms in the Elderly Health Centers between July 1998 to December 2000, in a study conducted in a population aged 65 or older using the Geriatric Depressive Symptoms Scale criteria, was 4.9% in men and 7.9% in women.[31] The rates estimated were slightly higher than the respective rates of 29.2% and 41.1% reported by Woo et al.[32] Such discrepancies between our results and the previous studies may be a result of methodological differences in diagnosis and the healthy worker effect.
In our results a high level of CRP at baseline was associated with depressive symptoms in men, but not in women. However, it was no longer significant after adjustment for sociodemographic characteristics (age, education, marital status, hukou, residence), health behaviors (cigarette smoking, alcohol drinking, eating meals, activity status, physical exercise), health conditions (major accidental injury, diseases, health status), systolic blood pressure, and metabolic measures (LDL, HDL, triglycerides, and BMI). Previous studies have shown that the association between CRP and depressive symptoms is often attenuated by controlling confounders such as BMI.[33–35] It is likely due to the confounder in the CPR-depressive symptoms relationship. However, most studies support a positive association between CRP and depressive symptoms both in men and women.[11–18,36,37] The mechanisms for the association between CRP and depressive symptoms are unclear, but various hypotheses have been develop to explain the relationship since CRP cannot cross the blood-brain barrier, and directly affect emotion regulating area in the brain.[21]
4.1. Strengths and limitations
There are several limitations of our study. First, the relationship between CRP-depressive symptoms in the elderly becomes seriously more complex, we only consider the confounders as possible as we can, but there are some unknown factors. Secondly, the relationship between CRP and depressive symptoms should be studied prospectively. Our study investigated depressive symptoms in the mid and elderly participant through a cross-sectional study. Follow-up study was relatively short to comprehensively observe changes in the next step. The last, most of the exposure and outcome measures of the study were based on a subjective report and the self-reported questionnaire. Our study has several strengths. Firstly, the study was based on a nationwide survey. Secondly, we conducted the analyses according to sex. Thirdly, it is interesting that the study has shown the null result which provides an opportunity to understand the other underlying mechanism between inflammation and depressive symptoms.
5. Conclusions
The result recently conducted studies demonstrate a high level of CRP at baseline was associated with depressive symptoms in men, but not in women. However, after adjusting the potential confounders, our data do not support the association between CRP and depressive symptoms in both men and women in China. Paying more attention to the role of CRP in depressive symptoms provides an opportunity to understand the underlying mechanisms between inflammation and depressive symptoms.
Acknowledgments
The authors are grateful to the participants, and thanks also to members of the CHARLS.
Author contributions
LZ conceived and drafted the manuscript. J-lL, L-lZ, L-Lg, HL, and DL helped revise the manuscript.
Formal analysis: Lin Zhang.
Writing – original draft: Lin Zhang.
Writing – review and editing: Jin-long Li, Li-li Zhang, Lei-lei Guo, Hong Li, Dan Li.
Footnotes
Abbreviations: BMI = body mass index, CES-D = Center for Epidemiologic Studies-depressive symptoms scale, CHARLS = China Health and Retirement Longitudinal Study, CI = confidence interval, CRP = C-reactive protein, HDL = high-density lipoprotein, LDL = low-density lipoprotein, OR = odds ratio, SD = standard deviation.
Funding: CHARLS was supported by the NIA.
Consent for publication: All of the authors have read and approved the manuscript.
Availability of the data: Http://charls.ccer.edu.cn/zh-C.
Ethics approval and consent to participate: The study is publically available (http://charls.ccer.edu.cn/zh-CN) with no direct contact with the individual participants.
The authors have no conflicts of interest to disclose.
References
- [1].Hua Y, Wang B, Wallen GR, et al. Health-promoting lifestyles and depression in urban elderly Chinese. PLoS One 2015;10:e0117998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Su D, Wu XN, Zhang YX, et al. Depression and social support between China’ rural and urban empty-nest elderly. Arch Gerontol Geriatr 2012;55:564–9. [DOI] [PubMed] [Google Scholar]
- [3].Ma X, Xiang YT, Li SR, et al. Prevalence and sociodemographic correlates of depression in an elderly population living with family members in Beijing, China. Psychol Med 2008;38:1723–30. [DOI] [PubMed] [Google Scholar]
- [4].Schoevers RA, Geerlings MI, Beekman AT, et al. Association of depression and gender with mortality in old age. Results from the Amsterdam Study of the Elderly (AMSTEL). Br J Psychiatry 2000;177:336–42. [DOI] [PubMed] [Google Scholar]
- [5].Schoevers RA, Geerlings MI, Deeg DJ, et al. Depression and excess mortality: evidence for a dose response relation in community living elderly. Int J Geriatr Psychiatry 2009;24:169–76. [DOI] [PubMed] [Google Scholar]
- [6].Carney RM, Freedland KE, Miller GE, et al. Depression as a risk factor for cardiac mortality and morbidity: a review of potential mechanisms. J Psychosom Res 2002;53:897–902. [DOI] [PubMed] [Google Scholar]
- [7].Kuo HK, Yen CJ, Chang CH, et al. Relation of C-reactive protein to stroke, cognitive disorders, and depression in the general population: systematic review and meta-analysis. Lancet Neurol 2005;4:371–80. [DOI] [PubMed] [Google Scholar]
- [8].Elovainio M, Aalto AM, Kivimaki M, et al. Depression and C-reactive protein: population-based Health 2000 Study. Psychosom Med 2009;71:423–30. [DOI] [PubMed] [Google Scholar]
- [9].Ma Y, Chiriboga DE, Pagoto SL, et al. Association between depression and C-reactive Protein. Cardiol Res Pract 2010;2011:286509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Elovainio M, Keltikangas-Jarvinen L, Pulkki-Råback L, et al. Cardiovascular Risk in Young Finns Study. Depressive symptoms and C-reactive protein: the Cardiovascular Risk in Young Finns Study. Psychol Med 2006;36:797–805. [DOI] [PubMed] [Google Scholar]
- [11].Danner M, Kasl SV, Abramson JL, et al. Association between depression and elevated C-reactive protein. Psychosom Med 2003;65:347–56. [DOI] [PubMed] [Google Scholar]
- [12].Ford DE, Erlinger TP. Depression and C-reactive protein in US adults: data from the Third National Health and Nutrition Examination Survey. Arch Intern Med 2004;164:1010–4. [DOI] [PubMed] [Google Scholar]
- [13].Pikhart H, Hubacek JA, Kubinova R, et al. Depressive symptoms and levels of C-reactive protein: a population-based study. Soc Psychiatry Psychiatr Epidemiol 2009;44:217–22. [DOI] [PubMed] [Google Scholar]
- [14].Matthews KA, Schott LL, Bromberger JT, et al. Are there bi-directional associations between depressive symptoms and C-reactive protein in mid-life women? Brain Behav Immun 2010;24:96–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Bjerkeset O, Romild U, Smith GD, et al. The associations of high levels of C-reactive protein with depression and myocardial infarction in 9258 women and men from the HUNT population study. Psychol Med 2011;41:345–52. [DOI] [PubMed] [Google Scholar]
- [16].Daly M. The relationship of C-reactive protein to obesity-related depressive symptoms: a longitudinal study. Obesity (Silver Spring) 2013;21:248–50. [DOI] [PubMed] [Google Scholar]
- [17].Wium-Andersen MK, Orsted DD, Nielsen SF, et al. Elevated C-reactive protein levels, psychological distress, and depression in 73, 131 individuals. JAMA Psychiatry 2013;70:176–84. [DOI] [PubMed] [Google Scholar]
- [18].Song BM, Lee JM, Choi W, et al. Association between C reactive protein level and depressive symptoms in an elderly Korean population: Korean Social Life, Health and Aging Project. BMJ Open 2015;5:e006429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Chaiton M, O’Loughlin J, Karp I, et al. Depressive symptoms and C-reactive protein are not associated in a population-based sample of adolescents. Int J Behav Med 2010;17:216–22. [DOI] [PubMed] [Google Scholar]
- [20].Douglas KM, Taylor AJ, O’Malley PG. Relationship between depression and C-reactive protein in a screening population. Psychosom Med 2004;66:679–83. [DOI] [PubMed] [Google Scholar]
- [21].Au B, Smith KJ, Gariepy G, et al. The longitudinal associations between C-reactive protein and depressive symptoms: evidence from the English Longitudinal Study of Ageing (ELSA). Int J Geriatr Psychiatry 2015;30:976–84. [DOI] [PubMed] [Google Scholar]
- [22].Zhang L, Liu K, Li H, et al. Relationship between body mass index and depressive symptoms: the “fat and jolly” hypothesis for the middle-aged and elderly in China. BMC Public Health 2016;16:1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Ridker PM. Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Circulation 2003;107:363–9. [DOI] [PubMed] [Google Scholar]
- [24].Cepeda MS, Stang P, Makadia R. Depression is associated with high levels of C-reactive protein and low levels of fractional exhaled nitric oxide: results from the 2007–2012 National Health and Nutrition Examination Surveys. J Clin Psychiatry 2016;77:1666–71. [DOI] [PubMed] [Google Scholar]
- [25].Zhang J, Norvilitis JM. Measuring Chinese psychological well-being with Western developed instruments. J Pers Assess 2002;79:492–511. [DOI] [PubMed] [Google Scholar]
- [26].Wang JN, Sun W, Chi TS, et al. Prevalence and associated factors of depressive symptoms among Chinese doctors: a cross-sectional survey. Int Arch Occup Environ Health 2010;83:905–11. [DOI] [PubMed] [Google Scholar]
- [27].Liu L, Chang Y, Fu J, et al. The mediating role of psychological capital on the association between occupational stress and depressive symptoms among Chinese physicians: a cross-sectional study. BMC Public Health 2012;12:219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Yu J, Li J, Cuijpers P, et al. Prevalence and correlates of depressive symptoms in Chinese older adults: a population-based study. Int J Geriatr Psychiatry 2012;27:305–12. [DOI] [PubMed] [Google Scholar]
- [29].Boey KW. Cross-validation of a short form of the CES-D in Chinese elderly. Int J Geriatr Psychiatry 1999;14:608–17. [DOI] [PubMed] [Google Scholar]
- [30].Chang HH, Yen ST. Association between obesity and depression: evidence from a longitudinal sample of the elderly in Taiwan. Aging Ment Health 2012;16:173–80. [DOI] [PubMed] [Google Scholar]
- [31].Li ZB, Ho SY, Chan WM, et al. Obesity and depressive symptoms in Chinese elderly. Int J Geriatr Psychiatry 2004;19:68–74. [DOI] [PubMed] [Google Scholar]
- [32].Woo J, Ho SC, Lau J, et al. The prevalence of depressive symptoms and predisposing factors in an elderly Chinese population. Acta Psychiatr Scand 1994;89:8–13. [DOI] [PubMed] [Google Scholar]
- [33].Elovainio M, Keltikangas-Jarvinen L, Pulkki-Raback L, et al. Depressive symptoms and C-reactive protein: the cardiovascular risk in Young Finns Study. Psychol Med 2006;36:797–805. [DOI] [PubMed] [Google Scholar]
- [34].Almeida OP, Norman PE, Allcock R, et al. Polymorphisms of the CRP gene inhibit inflammatory response and increase susceptibility to depression: the Health in Men Study. Int J Epidemiol 2009;38:1049–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Stewart JC, Rand KL, Muldoon MF, et al. A prospective evaluation of the directionality of the depression-inflammation relationship. Brain Behav Immun 2009;23:936–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].van den Biggelaar AH, Gussekloo J, De Craen AJ, et al. Inflammation and interleukin-1 signaling network contribute to depressive symptoms but not cognitive decline in old age. Exp Gerontol 2007;42:693–701. [DOI] [PubMed] [Google Scholar]
- [37].Luukinen H, Jokelainen J, Hedberg P. The relationships between high-sensitivity C-reactive protein and incident depressed mood among older adults. Scand J Clin Lab Invest 2010;70:75–9. [DOI] [PubMed] [Google Scholar]


