Abstract
Human gut associated lymphoid tissues (GALT) play a key role in the acute phase of HIV infection. The propensity of HIV to replicate in these tissues however, is not fully understood. Access and migration of naïve and memory CD4+ T cells to these sites is mediated by interactions between integrin α4β7, expressed on CD4+ T cells, and MAdCAM, expressed on high endothelial venules. We report here that MAdCAM delivers a potent costimulatory signal to naïve and memory CD4+ T cells following ligation with α4β7. Such costimulation promotes high-levels of HIV replication. An anti-α4β7 mAb that prevents mucosal transmission of SIV blocks MAdCAM signaling through α4β7 and MAdCAM-dependent viral replication. MAdCAM costimulation of memory CD4+ T cells is sufficient to drive cellular proliferation and the up-regulation of CCR5, while naïve CD4+ T cells require both MAdCAM and retinoic acid to achieve the same response. The pairing of MAdCAM and retinoic acid is unique to the GALT, leading us to propose that HIV replication in these sites is facilitated by MAdCAM-α4β7 interactions. Moreover, complete inhibition of MAdCAM signaling by an anti-α4β7 mAb, an analogue of a clinically approved therapeutic (vedolizumab), highlights the potential of such agents to control acute HIV infection.
Introduction
Most HIV infections throughout the world occur following the exposure of host mucosal surfaces to virus. The subsequent events that allow irreversible establishment of HIV infection remain poorly defined. Studies of mucosal transmission in the SIV/Rhesus macaque (RM) nonhuman primate model indicate that suboptimally activated CD4+ T cells are the initial targets of infection1,2. Various lines of evidence suggest that because the frequency of these cells, and the amount of virus that they produce are low, infection of these cells may fail to establish irreversible infection in the host2,3. The establishment of an irreversible infection is instead believed to involve passing of the virus from suboptimally activated cells in the genital and rectal mucosa to fully activated CD4+ T cells, some of which migrate into draining lymph nodes2,3. A key determinative step then occurs as these cells traffic to inductive sites in gut tissues, most notably Peyer’s Patches (PPs) and mesenteric lymph nodes (MLNs)4. There appear to be an intrinsic relationship between HIV/SIV replication during acute infection (AI) and the trafficking/homing of target cell in GALT5–7. The high level of virus replication in PPs and MLNs is a central event and a primary source of viremia in AI. It is this aspect of AI that has led to the concept that both HIV and SIV are predominantly gut-tropic viruses8,9.
Proviral DNA is also found in the lamina propria (LP), the major effector site within gut associated lymphoid tissues (GALT)10. Importantly, during AI, massive loss of memory CD4+ T cells occurs along with the degradation of LP ultra-structure11–13. Damage to the LP is considered a major factor in the development of advanced HIV disease8. It is generally assumed that the burst of viral replication in GALT occurs because of the high frequency of activated CD4+/CCR5+ T cells that appear within these sites. Lymphocyctes trafficking through PPs and MLNs however, are subject to unique regulatory stimuli, raising the possiblity that these tissues possess additional features rendering them particularly permissive to infection.
Migration of CD4+ T cells from the genital and rectal mucosa to PPs and MLNs is a regulated process that requires those cells to extravasate through the high endothelial venules (HEVs) that service GALT(Supplementary Figure 1)5,7. Extravasation is achieved by a series of receptor-counter receptor interactions involving proteins expressed on both the surfaces of circulating lymphocytes and HEVs14. These interactions have been described as a multi-step adhesion cascade15. A number of components of this adhesion cascade are common to extravasation of lymphocytes into many tissues, yet trafficking of lymphocytes into PPs and MLNs is somewhat unique in that it is mediated predominantly by the interaction of integrin α4β7 (α4β7) and L-selectin (CD62L) on the surface of lymphocytes, with MAdCAM and L-selectin-specific ligands on the endothelial cells15–17. These interactions are regulated by dynamic changes in the expression levels of L-selectin, and in the expression levels, aggregated state and conformation of α4β7. Importantly, α4β7 is the only integrin capable of binding to MAdCAM16. It is the tissue-specific expression of MAdCAM on the surface of gut HEVs that defines α4β7 as the gut homing integrin. Thus, MAdCAM is central to the trafficking of CD4+ T cells to PPs and MLNs and is therefore linked in an inexorable way to the gut-tropic nature of HIV.
A subset of integrins, most notably LFA-1, but also α4β7, in addition to functioning as homing receptors, deliver costimulatory signals to CD4+ T cells18–21. The natural ligand of LFA-1 is ICAM and through its interaction with, LFA-1, ICAM can synergize with CD28 in promoting T cell activation22,23. Central to this process is the role of LFA-1 in stabilizing immunological synapses (IS). Similar to the LFA-1/ICAM interaction, α4β7 mediates costimulatory signals to T cells through its interaction with MAdCAM, and it also synergizes with CD28. Increased adhesion does not adequately account for this synergy. Signaling through α4β7 and CD28 can be separated in space and time such that MAdCAM and CD80/86 (B7-1 and B7-2, respectively) can appear on separate cells (remote costimulation) and MAdCAM signaling can also precede CD80/86 mediated costimulation (priming)18,23. This raises the possibility that MAdCAM expressed on the surface of HEVs can participate in the activation and proliferation of migrating T cells as they pass into inductive sites (PP, MLN) of GALT.
α4β7+/CD4+ T cells play a central role in mucosal transmission of HIV and SIV 24–28. These cells, which can be found circulating in blood and in all peripheral lymph nodes are also present in the genital mucosa29. The base-line levels of circulating α4β7+/CD4+ T cells is stable, but varies among individuals27,30. Studies from the Rhesus macaque/SIV model of HIV transmission have shown thatα4β7+/CD4+ T cells are among the first cells infected and depleted following transmission31,32, a finding that is consistent with the depletion of these cells early after infection in humans33. Moreover, their frequency in mucosal tissues has been correlated with susceptibility to infection26,28. We recently reported that a monoclonal antibody (mAb) specific for α4β7 (anti-α4β7 mAb), when delivered intravenously, protected 6/12 Rhesus macaques from vaginal infection by a highly infectious and pathogenic strain of SIV (SIVMac251)24. The capacity of the anti-α4β7 mAb to protect Rhesus macaques from infection underscores the critical role that α4β7 expressing cells play in mucosal transmission. However, it is unclear where along the pathway between the vaginal mucosa and GALT α4β7+/CD4+ T cells are first infected, and how the anti-α4β7 mAb blocked transmission.
Considering the critical role of cellular activation in HIV infection, and recognizing that α4β7+/CD4+ T cells are infected early in transmission, we asked whether MAdCAM-mediated signaling through α4β7 could enhance the susceptibility of CD4+ T cells to infection and promote viral replication. In addition, we asked whether the anti-α4β7 mAb used to block SIV transmission could inhibit MAdCAM-mediated viral replication by inhibiting costimulation.
Results
MAdCAM ligation of Integrin-α4β7 promotes HIV replication
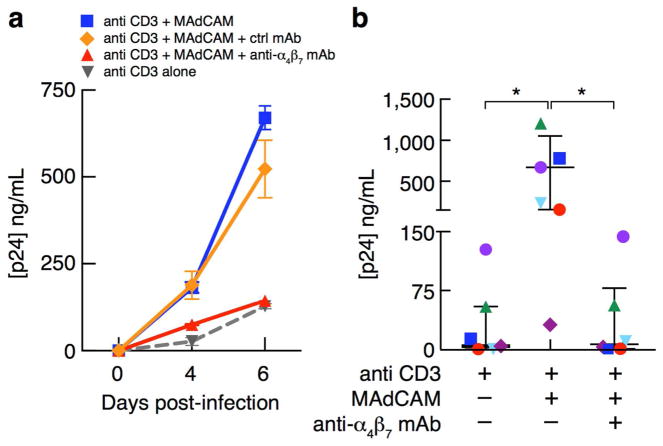
To determine whether MAdCAM-mediated cell signaling could promote viral replication we carried out in vitro infections of freshly isolated CD4+ T cells obtained from healthy donors with the CCR5-tropic isolate HIV SF162. To mimic antigen-mediated stimulation through the T cell receptor (TCR), we utilized the well-established procedure of culturing cells with an anti-CD3 monoclonal antibody (anti-CD3)34. Primary CD4+ T cells were added to wells pre-coated with anti-CD3 or anti-CD3 in combination with recombinant human MAdCAM-1 Ig (MAdCAM). After 48 hours, cultures were inoculated with HIV in the presence/absence of a pre-determined optimal concentration of anti-α4β7. Cell supernatants were sampled 4 and 6 days post infection, and viral replication was assessed by p24 antigen ELISA. While anti-CD3 alone induced relatively low levels of viral replication, cellular stimulation with anti-CD3 in the presence of MAdCAM resulted in robust HIV replication (Figure 1a). Addition of the anti-α4β7 mAb abrogated the high levels of viral replication observed with anti-CD3+MAdCAM, while addition of a control antibody had no effect. Similar results were obtained with primary cells from six independent donors (Figure 1b) and in experiments utilizing a CXCR4 tropic HIV isolate (Supplementary Figure 2). We therefore conclude that signaling directly through α4β7 by MAdCAM promotes viral replication in vitro.
Figure 1.
MAdCAM stimulation promotes HIV replication. (a) Primary CD4+ T cells cultured for three days in the presence of stimulatory ligands – either anti CD3 alone or anti CD3 + MAdCAM, in the presence of anti-α4β7 mAb or a control mAb (Synagis). Three days post-stimulation, cells were infected with the HIV isolate SF162 and viral replication was assessed by measuring the concentration of p24 antigen in cell supernatants 4 and 6 days post-infection. (b) Replication of HIV-SF162 in CD4+ T cells isolated from 6 independent donors, in the presence of stimulatory ligands as described in (a). The concentration of viral p24 antigen in culture supernatants on day 6 post-infection is shown. *P < 0.05 (two-tailed parametric paired t-test).
MAdCAM ligation of α4β7 promotes CD4+ T cell proliferation
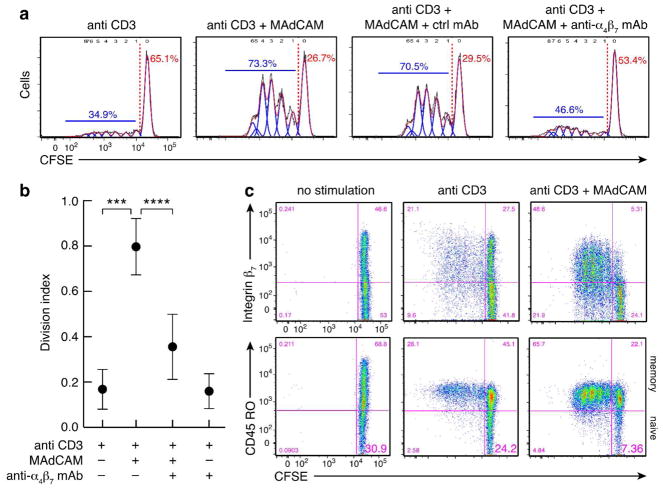
To better understand the signaling events mediated through α4β7 and the antiviral effect of anti-α4β7 mAb we evaluated the capacity of MAdCAM to enhance cellular proliferation using a standard CFSE dye dilution assay. A culture protocol similar to that described above was employed. While anti-CD3 mAb alone generated minimal cellular proliferation, the inclusion of MAdCAM in culture increased proliferation signficantly (Figure 2a–b). Proliferation was inhibited by addition of the anti-α4β7 but not by a control mAb. Phenotypic analysis of the proliferating CD4+ T cells using a non- competetive mAb against the integrin-β7 revealed proliferation was limited largely to the β7+ population, again implicating a central role of α4β7 in MAdCAM mediated cellular proliferation (Figure 2c). Further analysis revealed that the relative proportion of CD45RO− cells decreased in the presence of MAdCAM-Ig while the majority of CFSE diluted cells expressed CD45RO (Figure 2c). This observation suggests that MAdCAM-mediated costimulation induced proliferation of the CD45RO− cell population and drove these cells towards a CD45RO+ cell phenotype. With this in mind, we sought to assess directly the manner in which MAdCAM costimulation impacts recently activated CD45RO−/CD4+ T cells, and whether this mode of costimulation supports viral replication in this subset of cells.
Figure 2.
The anti-α4β7 mAb inhibits MAdCAM-mediated CD4+ T cell proliferation. (a) Cellular proliferation in primary CD4+ T cells cultured for 5 days in the presence of anti CD3 alone, anti CD3 + MAdCAM, anti CD3 + MAdCAM + a control mAb (Synagis), or anti CD3 + MAdCAM + anti-α4β7 mAb. Proliferation was measured by CFSE dye dilution: red, draw model sum; blue, draw model components; black, total division profile. The percent of diluted CFSE labeled cells (divided cells) is shown in blue, above the blue bar, and undiluted (undivided) cells is shown in red. (b) Division of primary CD4+ T cells isolated from 5 independent donors and stimulated with ligands as in (a), represented by a division index (measure of the average number of divisions). * P < 0.0001 (two tailed parametric paired t test). (c) The expression of Integrin-β7 (y-axis, top row) and CD45RO (y-axis, bottom row) on CD4+ T cells stimulated for 5 days with anti CD3 or anti CD3 + MAdCAM is shown by CFSE dye (x-axis).
MAdCAM ligation of α4β7 activates naïve CD4+ T cells
It is well established that shedding of CD62L from the surface of naïve CD4+ T cells represents an early marker of cellular activation 35,36. In this regard, we set out to assess the manner by which MAdCAM costimulation influences the expression/shedding of CD62L on both CD45RO− and CD45RO+ CD4+ T cells, and whether these effects were impacted by anti-α4β7z Ab. Using the same protocol described above for assessing proliferation, we analyzed the amount of CD62L shed from CD4+ T cells by quantifying loss of CD62L expression. We observed a significant reduction in the surface expression of CD62L on the CD45RO− subset of CD4+ T cells five hours post exposure to anti-CD3 and MAdCAM (Figure 3a). Anti-α4β7 mAb inhibited this effect. When gating on the α4β7+/CD45RO− CD4+ T cell population, we found loss of CD62L expression by ~10-fold in the presence of anti-CD3 plus MAdCAM relative to anti-CD3 alone in cells from four independent donors (Figure 3b). Loss of expression also occurred on CD45RO+/CD4+ T cells, but to a much lesser extent. To further interrogate the memory CD4+ T cell subset, we subdivided the CD45RO+ cells into the integrin β7+ and integrin β7− populations, with representative gating shown (Figure 3c). In line with our previous observation, significant CD62L shedding was apparent only on those cells expressing α4β7, and not on the α4β7− population (Figure 3d). In all of these experiments, loss of expression of CD62L in the presence of MAdCAM was fully abrogated by anti-α4β7 mAb.
Figure 3.
MAdCAM stimulation promotes loss of CD62L expression. (a) Expression of CD62L (y-axis) and CD45RO (x-axis) on purified, primary, CD4+ T cells 5 hours post-stimulation with anti CD3 alone, anti CD3 + MAdCAM, anti CD3 + MAdCAM + anti-α4β7 mAb, or anti CD3 + MAdCAM + control mAb (Synagis). Cells below the black dashed line reflect loss of CD62L expression. In CD45RO− of CD45RO+ cells, the percent of CD62L expressing cells is labeled in red or blue respectively. (b) The percent loss of CD62L expression (y-axis) in either CD45RO− or CD45RO+ subsets of CD4+ T cells from four independent donors, treated as in (a). (c) A representative dot plot illustrating the expression of Integrin-β7 (y-axis) by CD45RO (x-axis) on unstimulated CD4+ T cells, with red boxes around the β7+/CD45RO+ and β7−/CD45RO+ subsets. (d) The percent loss of CD62L expression on purified CD4+ T cells subdivided into the CD45RO+/β7+ and CD45RO+/β7− populations as in (c) and treated as in (a). *P < 0.05 (two-tailed parametric paired t-test).
To determine whether the activation of naïve cells upon MAdCAM signaling was limited to CD62L loss of expression or was reflective of a broader degree of lymphocyte activation, we monitored the expression of additional cellular activation markers. We found that CD69 was up-regulated within 5 hours of anti CD3+MAdCAM treatment, in a manner that was entirely inhibited by the anti-α4β7 mAb (Supplementary Figure 3a). To evaluate the capacity of MAdCAM-α4β7 interactions to specifically activate isolated naïve CD4+ T cells, we purified the CD45RO− subset of cells by negative bead selection and stimulated the cells with anti CD3+MAdCAM as described above, and observed increased expression of two additional well-defined activation markers, Ki-67 and CD25 (Supplementary Figure 3b–c). Consistant with these observations, stimulation with MAdCAM drove naïve CD4+ T cells into the S phase of the cell cycle (Supplementary Figure 4). Interestingly, we also noted that MAdCAM upregulated the expression of CCR5 (Supplementary Figure 3d). We conclude that MAdCAM interactions with integrin α4β7 promote the rapid activation of both memory and naïve CD4+ T cells subsets. The shedding of CD62L is particularly noteworthy insofar as it participates directly in lymphocyte homing to gut inductive sites through a direct interaction with MAdCAM 35,36.
Retinoic acid acts as a cofactor for MAdCAM costimulation of naïve CD4+ T cells
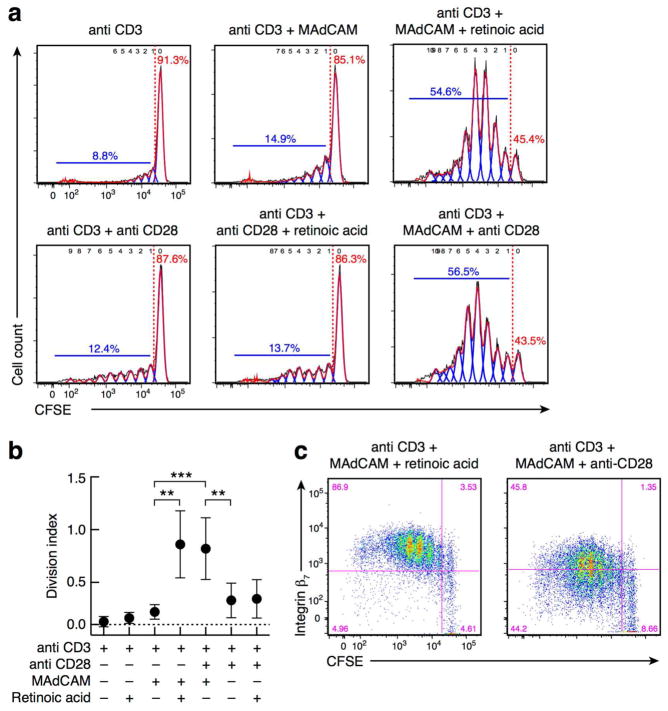
The results presented above raised the possibility that anti-CD3+MAdCAM treatment alone was sufficient to activate and induce the proliferation of CD45RO− naïve CD4+ T cells. To test this possibility directly we purified CD45RO−/CD4+ T cells by negative bead selection (96–99% purity) and carried out anti-CD3+MAdCAM stimulation and CFSE dye dilution measurements as described above. Although MAdCAM stimulation of naïve cells upregulated markers of activation (shown above), cells stimulated by this manner failed to proliferate (Figure 4a–b). To understand why naïve cells in isolation failed to proliferate we considered the fact that the average level of expression of α4β7 on CD45RO− cells is ~ 50–200 fold lower than that on CD45RO+/CD4+ T cells. Within PPs the surface expression of α4β7 on naïve T cells is up-regulated by retinoic acid (RA)37. With this in mind, we exposed CD45RO− CD4+ T cells simultaneously to anti- CD3+MAdCAM and RA, and under these conditions we observed robust cellular proliferation (Figure 4a–b). To determine whether the capacity of RA to enhance proliferation was specific to MAdCAM costimulation we treated CD45RO−/CD4+ T cells with anti-CD3 and RA in the absence of MAdCAM, and observed no increase in proliferation over anti-CD3 alone (Supplementary Figure 5). We next asked whether RA could enhance other costimulatory signals. To this end we exposed naïve cells to a suboptimal amount of anti-CD28, and found that RA was unable to induce proliferation under this condition (Figure 4a–b).
Figure 4.
RA combined with MAdCAM drives costimulation of naïve CD4+ T cells. (a) Purified naïve CD45RO−/CD4+ T cells stained with CFSE dye (x-axis), then stimulated for 5 days with anti CD3 alone or anti CD3 + MADCAM, with the addition of either RA or anti CD28. The blue bar marks cellular proliferation in CFSE diluted cells with the percent of either divided or undivided cells indicated in blue or red, respectively, as in (Figure 2a). (b) Division index of purified naïve CD45RO−/CD4+ T cells isolated from 7 independent donors and stimulated as in (a). * P < 0.008 (two-tailed parametric paired t-test). (c) The expression of Integrin-β7 (y-axis) by CFSE (x-axis), on purified naïve CD45RO−/CD4+ T cells, stimulated for 5 days with anti CD3 + MAdCAM + RA or anti CD3 + MAdCAM + anti CD28.
Lehnert and colleagues have reported that MAdCAM and anti-CD28 can act synergistically18. In fact, when we combined MAdCAM+anti-CD28 we observed levels of naïve CD4+ T cell proliferation comparable to that observed with MAdCAM+RA (Figure 4a–b). However, the two conditions appear to involve phenotypically distinct cells: whereas RA increased surface expression of α4β7, no such increase was observed with anti-CD28 (Figure 4c). This suggests that these two conditions, either addition of RA, or addition of anti-CD28, in the presence of MAdCAM, promote distinct patterns of cellular differentiation. Since certain T cell subsets that are relevant to the pathogenesis of HIV and SIV infection, including Treg and TH17 cells, express α4β7 29,38,39, further investigation is required to understand the impact of MAdCAM on differentiation of naïve T cells in a more complete way.
Retinoic acid combined with MAdCAM supports viral replication in recently activated naive CD4+ T cells
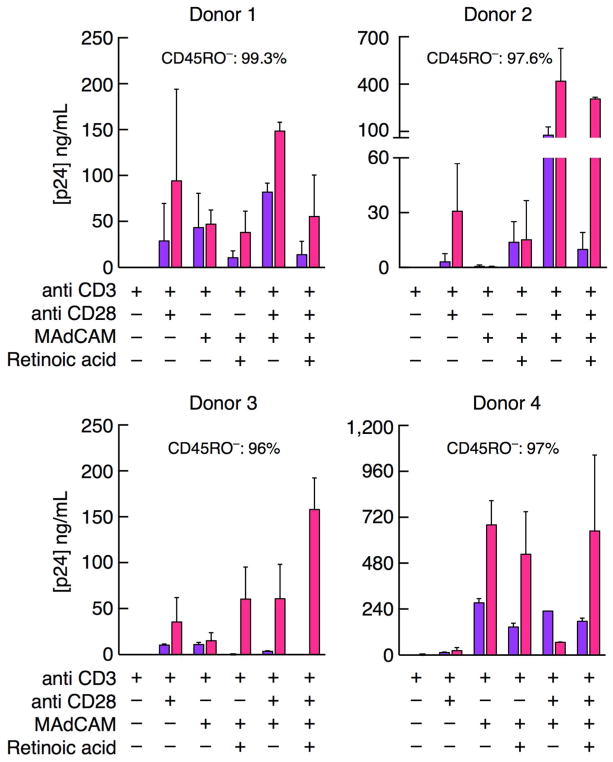
Having shown that MAdCAM activates naïve cells, we asked whether MAdCAM might enable recently activated naïve CD4+ T cells to support viral replication. Considering that once inside PPs, these cells are exposed to RA, we also assessed the impact of RA on viral replication, exclusively in the CD45RO− naïve CD4+ T cell population. Naïve cells from four healthy donors were stimulated with anti-CD3 and combinations of MAdCAM, RA and anti-CD28 (Figure 5). As before, virus was added 48 hours later. In general, the conditions that promoted proliferation of naïve CD4+ T cells in isolation (Figure 4) also facilitated high levels of viral replication (Figure 5).
Figure 5.
Naïve CD4+ T cells stimulated with RA and MAdCAM support viral replication. Replication of HIV SF162 in purified CD45RO−/CD4+ T cells from 4 independent donors, where cells were stimulated with anti CD3 alone or in combination with MAdCAM, RA or anti CD28 as designated, for 3 days prior to infection. Viral replication was quantified by p24 AlphaLISA (y-axis) on days 4 (purple) and 7 (red) post-infection (x-axis). The purity of CD45RO−/CD4+ T cell cultures assessed on day 0, is shown.
All four donors supported substantial levels of viral replication in cells stimulated with MAdCAM+RA or MAdCAM+anti-CD28. The inclusion of all three, MAdCAM, RA and anti-CD28, also supports high levels of viral replication. In two instances (donor 1 and 4) we observed viral replication in cultures stimulated with anti CD3+MAdCAM alone, without addition of RA or anti-CD28, despite our finding that this condition generally supports only low levels of cellular proliferation (Figure 4a–b). The capacity of anti CD3+MAdCAM to support viral replication without added cofactors likely reflects the capacity of MAdCAM to mediate cellular activation. We cannot exclude, however, that a small fraction of the viral replication we observed may stem from the purity of our starting cultures, as they did include a fraction (<3%) of CD45RO+ cells. We conclude that MAdCAM signaling through α4β7, along with an additional signal (RA or anti- CD28), promotes viral replication in recently activated naïve CD4+ T cells.
MAdCAM stimulation promotes viral replication in PBMCs from HIV-infected subjects
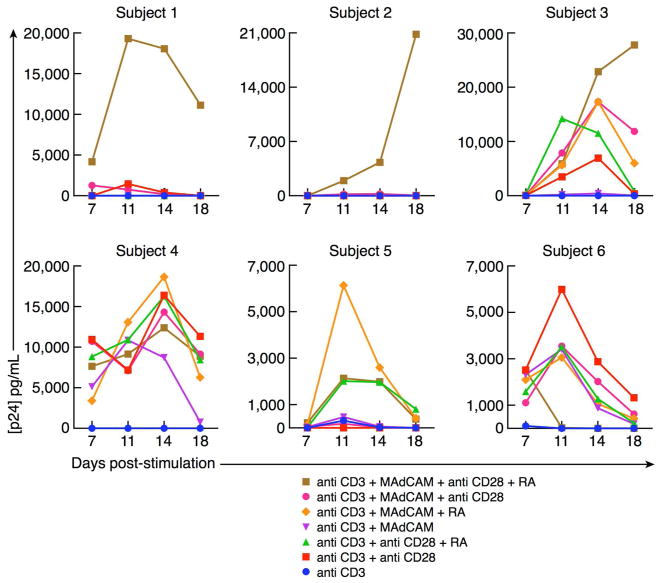
Because MAdCAM signaling through α4β7 in both the naïve and memory subsets of CD4+ T cells promotes viral replication in vitro, and upregulates the surface expression of key markers of cellular activation, we asked whether MAdCAM signaling through α4β7 could promote replication of the virus in peripheral blood mononuclear cells (PBMCs) from HIV-infected subjects. PBMCs from six antiretroviral therapy naïve subjects with viral loads ranging from 7631–54894 RNA copies/mL were evaluated. The subject cohort data are provided in Supplementary Table 1. Isolated PBMCs were CD8+ T cell depleted by positive bead selection to prevent any CD8-mediated cytolytic activity, and viral replication in the presence of our stimulatory ligands, anti-CD3, anti-CD28, MADCAM and combinations of MAdCAM with anti-CD28 and/or RA were tested. Cellular stimulation via the classical pathway with anti-CD3+anti CD28 promoted viral replication in three of the six subjects (Figure 6). In four of the subjects, anti CD3+MAdCAM+RA facilitated viral replication. In two of the subjects, anti CD3+MAdCAM alone supported viral replication. In all six subjects anti CD3+MAdCAM+anti CD28+RA supported viral replication. Although these stimuli are not as potent as non-specific stimuli that include mitogens (e.g PHA/Il2), these results suggest that in all six subjects α4β7-expressing cells were productively infected. This is consistent with previous reports that α4β7+ memory CD4+ T cells are preferential targets27,31. The fact that viral replication is induced by MAdCAM either with or without RA suggests that this is one of the mechanisms that could promote HIV replication in gut tissues.
Figure 6.
MAdCAM stimulation of PBMCs from HIV infected subjects promotes viral replication. PBMCs isolated from six HIV infected donors were CD8+ T cell depleted, and cultured over ligand coated plates. The stimulatory ligands include anti CD3, anti CD28, MAdCAM and RA in various combinations as designated. Viral p24 was measured by AlphaLISA (y-axis) from culture supernatants at day 7, 11, 14, and 18 (x- axis).
Discussion
During AI, GALT is a principal site of viral replication. Two features distinguish GALT from most other lymphoid tissues. First, trafficking of lymphocytes into these tissues is mediated by MAdCAM, and second, within GALT inductive sites, dendritic cells convert vitamin A to RA. We find that MAdCAM alone, or in combination with RA promotes high levels of HIV replication. P24 values in MAdCAM stimulated culture supernatants 6-days post stimulation, in most cases, exceeded 100 ng/ml. Of note, the anti-α4β7 mAb, which we previously demonstrated reduces mucosal transmission of SIV by 50 percent in a macaque model24, is able to inhibit this replication.
Naïve CD4+ T cells traffick continuously through PPs and MLNs via a MAdCAM dependent pathway. In this regard, we asked whether MAdCAM costimulation could prime naïve CD4+ T cells for productive infection. In bulk cultures that included both CD45RO+ and CD45RO− CD4+ T cells, MAdCAM costimulation appeared to drive the activation of both subsets. CD45RO− naïve cells were rapidly activated as evidenced by the up-regulation of CD69 and the shedding of L-selectin. Both of these effects were inhibited by the addition of anti-α4β7. However, we were surprised to find that CD45RO−/CD4+ T cells, when costimulated with MAdCAM, failed to proliferate in a significant way. RA, which is generated in PPs and MLNs, exerts potent effects on lymphocytes, including upregulation of expression of α4β7 and CCR540,41. It has also been reported that RA can acts as latency reversing agent42. This prompted us to ask whether its inclusion might enhance MAdCAM costimulation and hence permissiveness for HIV replication. This is noteworthy insofar as RA is often considered an “anti-infective” agent that enhances immunity against foreign microbes. Our observations are consistent with the above mentioned studies and the finding that, while vitamin A supplementation promotes resistance to other infectious agents, it paradoxically enhances HIV infection43. RA was unable to facilitate anti-CD28 mediated costimulation (Figure 4). However, when we combined anti-CD28 with MAdCAM, anti-CD28 effectively substituted for RA. We conclude that MAdCAM primes naïve CD4+ T cells for proliferation, but such cells require an additional stimulus.
The apparent synergy between MAdCAM and RA is likely to influence the manner in which antigen–specific immune responses evolve within GALT. Naïve CD4+ T cells uniformly express intermediate levels of α4β7, unlike α4β7+ memory cells, which express high levels of α4β7. This lower level deters naïve lymphocytes from accessing the LP16. In the course of MAdCAM/RA costimulation, α4β7 was up-regulated on proliferating cells. Such increased expression would facilitate the eventual trafficking of these cells to gut effector sites including LP. In contrast, MAdCAM/CD28 costimulation promoted similar levels of proliferation, but without α4β7 up-regulation, reducing in a relative way the potential of such cells to migrate to gut effector sites. Thus, these two types of costimulation likely lead to differential trafficking of lymphocytes. In this regard, the three principal subsets of CD4+ T cells that express α4β7 are TH17, Treg 29,38,39,44, and Tfh cells (Supplementary Figure 6). Determining whether MAdCAM/RA helps drive cells toward one or more of these functional CD4+ T cell subsets is the subject of ongoing studies. Finally, recognizing that in the PPs and MLNs, DCs are the source of both RA and CD80/86 signaling45, it is quite possible that in the context of an antigen specific response MAdCAM primed naïve CD4+ T cells are stimulated by both RA and CD80/86. In this regard MAdCAM/α4β7 costimulation is distinct from classical costimulation through CD28 in ways that suggest it may act in some manner as a 2nd costimulatory signal. To our knowledge this is the first demonstration of RA as a factor that can enhance cellular proliferation. Of note, the combination of MAdCAM, anti-CD28 and RA was consistent in promoting replication of HIV in PBMCs of HIV infected subjects (Figure 6).
In addition to promoting proliferation, MAdCAM/RA treatment of CD4+ T cells also up- regulates CCR5 (Supplementary Figure 3d). Because CCR5 functions as an entry receptor for most isolates of HIV, including those isolates that establish infection following mucosal transmission, its upregulation provides another way in which MAdCAM costimulation provides a conducive environment for the high levels of viral replication in GALT during AI. We note that RA-mediated increases in CCR5 expression (Supplementary Figure 3d) coincided with increases in the surface expression of α4β7. There appears to be an interesting, but not well-understood, relationship between these two cell surface receptors.
The anti-α4β7 mAb employed in our studies is a “primatized” analogue of vedolizumab, a therapeutic mAb used in the treatment of inflammatory bowel disease (IBD)46. Vedolizumab interferes with lymphocyte trafficking to the gut, which is believed to be the basis for its anti-inflammatory activity. However, MAdCAM-mediated lymphocyte trafficking and costimulation of lymphocytes through α4β7 are likely to be closely linked. Likewise, the capacity of anti-α4β7 mAb to block trafficking and signal transduction through α4β7 cannot be easily separated. In this regard it is reasonable to consider whether the efficacy of vedolizumab in the treatment of IBD involves not simply alterations in trafficking, but also a reduction of MAdCAM driven costimulation of α4β7+/CD4+ T cells.
Although MAdCAM expression is generally limited to the gut in healthy adults, other infectious agents, that elicit inflammatory responses induce MAdCAM expression outside of the gut. MAdCAM is expressed in the liver of hepatitis C infected individuals47, the female genital tract of chlamydia-infected women48, and the vaginal mucosa of HSV-2 infected macaques45,49. MAdCAM is also widely expressed in peripheral lymph nodes of newborns50. Whether, during the course of AI, HIV and SIV infection results in expression of MAdCAM outside of GALT remains to be determined; however, if that is the case, such expression could potentially contribute to the dissemination of virus subsequent to the seeding of PPs and MLNs at the outset of acute infection.
We speculate two possible scenarios in which α4β7+/CD4+ T cells encounter MAdCAM in a way that might facilitate viral replication in vivo. The first involves the direct interaction of these cells with HEVs proximal to GALT (see schematic in Supplementary Figure 7). In this context α4β7 binds to MAdCAM as part of diapedesis, a multi-step adhesion cascade that immediately precedes extravasation of migrating lymphocytes into the PPs, MLNs and LP15. The second scenario stems from reports that follicular dendritic cells (fDCs) in the germinal centers can express MAdCAM 51 while both Tfh CD4+ T cells and germinal center B cells express α4β7 52,53 (see schematic in Supplementary Figure 7d). Thus, there exists the potential for MAdCAM on fDCs to activate Tfh cells via interaction with α4β7. It is well established that fDCs trap HIV virions and transfer virus to anatomically secluded Tfh CD4+ T cells54,55. This trapping and transfer of virions is thought to contribute to the formation of viral reservoirs, and to viral persistence. We recently reported that a primatized analog of vedolizumab facilitated control of SIV rebound in ART-treated macaques following analytical treatment interruption56. Although the mechanism of control in these macaques remains to be identified, it is possible that the anti-α4β7 mAb interferes, in some manner, with α4β7 signalling in germinal centers in a way that contributes at least in part to that control. Of note, we observed qualitatively distinct anti gp120 antibody responses that persisted in animals receiving the anti-α4β7 mAb.
Viral replication in, and destruction of GALT is a defining feature of AI and a central event in HIV pathogenesis. In this report we have shown that MAdCAM, a surface receptor whose expression is largely restricted to GALT, promotes viral replication in α4β7+/CD4+ cells. The role of RA together with MAdCAM in promoting infection of recently activated CD4+ T cells provides a plausible explanation for the central role that GALT play in AI. This capacity of MAdCAM to signal through α4β7 in gut tissues may contribute in a significant way to the gut-tropic nature of HIV. That the anti-α4β7 mAb blocks this activity and inhibits viral replication suggests a novel intervention strategy that could potentially protect GALT during AI and delay the eventual progression of HIV disease.
Methods
Human blood and tissue samples
All primary CD4+ T cells utilized in these studies were isolated from PBMCs, collected from healthy donors through a NIH Department of Transfusion Medicine protocol that was approved by the Institutional Review Board of the National Institute of Allergy and Infectious Diseases (NIAID), National Institutes of Health. Informed consent was written and was provided by study participants and/or their legal guardians. Studies on HIV infected subjects were approved by the NIAID Institutional Review Board. PBMCs were isolated from these subjects by leukapheresis. HIV infection was determined by HIV-1/2 immunoassay (Abbott Laboratories, Abbott Park, IL) and Cambridge Biotech HIV-1 Western blot (Maxim Biomedical, Inc., Rockville, MD). All subjects acquired HIV infection in the USA and, therefore, are likely infected with clade B viruses, with no history of ART and no history of opportunistic diseases.
Primary cells and tissue culture reagents
Primary CD4+ T cells utilized in these studies were freshly isolated from healthy donor PBMCs and separated by Lymphocyte separation medium (MP Biomedicals, Santa Clara, CA). Purified CD4+ T cells, were obtained by negative selection (Stem Cell Technologies, Vancouver, Canada) to > 95% purity, as determined by flow cytometry. CD4+ T cells were cultured in complete RPMI 1640 medium with 2% L-glutamine-penicillin-streptomycin (Gibco Laboratories, Gaithersburg, MD) and 10% FBS (Gibco Laboratories, Gaithersburg, MD). Where designated, naïve CD45RO−/CD4+ T cell cultures were generated by CD45RO positive selection of bulk CD4+ T cells with Macs beads (Miltenyi Biotec, San Diego, CA) resulting in CD45RO−/CD4+ T cells at >96% purity. Purity of CD45RO−/CD4+ T cell cultures was validated in control experiments that included anti CD3 and retinoic acid and no cellular proliferation was observed (Supplementary Figure 8) indicating the contamination by antigen presenting cells did not contribute to proliferative responses. CD8+ T cells were depleted in a similar manner, by positive bead selection (Stem Cell Technologies, Vancouver, Canada) to 97% purity.
Antibodies and flow cytometry
The following antibodies were used for flow cytometry: anti Integrin β7 PE (clone FIB504), anti CD45RO APC and anti CD45RO BV421 (clone UCHL1), anti CD62L PE (clone DREG-56), anti CD69 PE (clone FN50), anti CCR5 APC (clone 2D7) and anti Ki-67 FITC (clone MOPC-21) (BD Pharmingen, San Diego, CA). For intracellular Ki-67 staining, BD Perm Wash Kit and company protocol were utilized (BD Pharmingen, San Diego, CA). The anti-α4β7 mAb heterodimer (clone Act-1) was gifted by Dr. Aftab Ansari. The Synagis antibody was gifted from Dr. Barton Haynes and used as a control in several experiments where designated. Data were collected on a FACSCanto II (BD Biosciences, San Diego, CA) and were analyzed using FlowJo and GraphPad Prism software.
Viral Replication Assay
96-well flat bottom cell culture treated plates were coated overnight at 4°C with either 200ng of anti CD3 (clone OKT3, eBioscience, San Diego, CA), 200ng of anti CD28 (CD28.2, eBioscience, San Diego, CA), 200ng of recombinant human MAdCAM-1 Fc Chimera (R&D Biosystems, Minneapolis, MN) or combinations of these ligands in 100ul HBS (1x). In certain wells, 2ug of anti-α4β7 mAb or a control mAb Synagis were added to test specificity. The following day, plates were washed in PBS solution and primary CD4+ T cells were added over each well of the ligand-coated plates at a concentration of 2 × 106 cells/mL. Plates were subsequently cultured at 37°C, 5% CO2 for three days in the presence of ligand. Following stimulation, cells were infected with 2uL of HIV-containing infectious cell supernatant (viral concentration of 0.16 ng/uL, p24-based ELISA). After 12-hours of incubation, plates were washed in PBS to remove excess virus, resuspended in RPMI (10%FBS) and cultured, whereby cell supernatants were collected days 4, 6 and 7 post-infection. The virus utilized for the in vitro experiments was prepared by cloning the full-length gp160 from the SF162 viral isolate (accession number EU123924) into the NL4.3 viral backbone. In one experiment the full length NL4.3 (accession number AF324493) was utilized, as designated. Viral stocks were produced by transient transfection of 293T cells and then passaged for one round through PBMCs. Experiments conducted on cells from HIV infected human subjects were performed in a similar manner, such that ligands were coated overnight in a 48-well flat bottom plate. In order to avoid CD8 suppressor activity57,58 PBMCs from HIV infected subjects were CD8+ T cell depleted by positive bead selection, and CD8-depleted PBMCs were cultured over the ligand coated wells at a concentration of 2 × 106 cells/mL. In both the in vitro HIV infection assays and viral replication assays utilizing PBMCs from infected donors, retinoic acid (Sigma Aldrich, St. Louis, MO) was added to specific test wells at a concentration of 10nM. Culture supernatants were collected at various time points post-infection and virus replication was detected by measuring the concentration of p24 GAG antigen by ELISA (PerkinElmer, Santa Clara, CA) or p24 GAG AlphaLISA (PerkinElmer, Santa Clara, CA).
Cellular Proliferation Assay
96-well flat bottom cell culture-treated plates were coated overnight at 4°C with either 200ng of anti CD3, 200ng of anti CD28, 200ng of MAdCAM-Fc Chimera or combinations of these ligands. In certain wells, anti-α4β7 mAb or a control mAb Synagis were added to test specificity. The following day, primary CD4+ T cells were CFSE labeled using the CellTrace CFSE Cell Proliferation Kit per manufacturer’s instructions (Invitrogen, Grand Island, NY). CD4+ T cells were washed twice in PBS, resuspended in PBS containing 5-(and-6-) carboxyfluorescein diacetate succinimidyl ester (CFSE) at a final concentration of 0.5μM, and incubated at room temperature for 10 min. Labeled cells were washed three times with RPMI 10% FBS and 2 × 105 cells were added over each ligand coated well. In certain wells, retinoic acid (Sigma Aldrich, St. Louis, MO) was also added at a concentration of 10nM. Cells were incubated over ligands at 37°C, 5% CO2 for a minimum of 4 days in RPMI (10% FBS). After 5 days, cells were doubly stained with anti CD45RO APC and anti Integrin-β7 PE. CFSE dilution was measured by flow cytometry. The division index for cells in each treatment group was calculated using FlowJo software.
Cell Cycle Analysis
96-well flat bottom cell culture-treated plates were coated overnight at 4°C with either 200ng of anti CD3, 200ng of anti CD28, 200ng of MAdCAM-Fc Chimera or combinations of these ligands as in the cellular proliferation assay. The following day, purified naïve CD45RO−/CD4+ T cells were added to the ligand coated wells. In certain wells, retinoic acid was also added at a concentration of 10nM. Cells were incubated over ligands at 37°C, 5% CO2 for a minimum of 4 days in RPMI (10% FBS). After 3 days, cells were stained with 50ug/mL propidium iodide (PI) in buffer containing 4mM sodium citrate and 0.3% Triton X-100 (Sigma Aldrich, St. Louis, MO). PI staining was measured by flow cytometry and data was analyzed using FlowJo software.
Animal Lymphocyte Staining
All animals were housed in compliance with regulations under the Animal Welfare Act, the Guide for the Care and Use of Laboratory Animals, at Tulane National Primate Research Center TNPRC; Covington LA. Inguinal lymph nodes were collected from adult, female Rhesus macaques at necropsy, cut in small pieces and passed through a 40 μm cell strainer. Cells were washed and stained with live-dead fixable Aqua (Invitrogen, Grand Island, NY) and monoclonal antibodies against CD3 (clone SP34) and CD4 (clone L200) from BD Pharmingen (San Diego, CA), PD1 (clone eBioJ105) from eBioscience (San Diego, CA) and CXCR5 (clone 710D82.1) and integrin-α4β7 (clone Act1) from Mass Biologics (Mattapan, MA).
Statistical Analysis
Parametric, paired two-tailed T tests for normally distributed data were calculated by GraphPad Prism and p values < 0.05 were reported.
Supplementary Material
Table 1.
Subject cohort. Subject baseline viral loads, CD4/CD8 T cell counts and basic demographics are shown.
| Subject | Viral Load (copies/mL) | CD4 Count (cells/mm3) | CD8 Count (cells/mm3) | Age(Yr) | sex | Race | Diagnosis | Risk factor |
|---|---|---|---|---|---|---|---|---|
| 1 | 17345 | 514 | 780 | 61 | M | Caucasian | 1985 | MSM |
| 2 | 7631 | 455 | 1037 | 58 | M | AA | 1985 | MSM |
| 3 | 14446 | 955 | 1002 | 64 | F | AA | 1985 | Heterosexual |
| 4 | 54894 | 428 | 1283 | 65 | M | Caucasian | 2001 | MSM |
| 5 | 24224 | 575 | 932 | 56 | M | AA | 1993 | MSM |
| 6 | 15875 | 460 | 719 | 70 | M | Caucasian | 1984 | MSM |
Acknowledgments
Financial Support
This work was supported by the Intramural Research Program of the US National Institutes of Health (National Institute of Allergy and Infectious Diseases).
This work was supported by the Intramural Research Program of the US National Institutes of Health (National Institute of Allergy and Infectious Diseases). Livia Ramos Goes was supported by a scholarship from National Council for Scientific and Technological Development (CNPq) – Brazil. The antibody used for staining of α4β7 (anti-α4β7 mAb) was obtained from Dr. Aftab Ansari but originates from the NIH Nonhuman Primate Reagents Resource supported by AI126683 and OD010976. We thank Dr. Keith Reimann and Mr. Adam Busby for their preparation of the recombinant Rhesus macaque α4β7 monoclonal antibody, and Dr. Barton Haynes for the Synagis antibody. We also thank J. Weddle and A. Weddle for assistance with preparation of figures.
Footnotes
Author contributions
JA, CC, ASF, FN, LRG, JCR and RO conceived and designed the study; FN, LRG, JCR, RO, IP, JH, DVR, DW, MW, and KJ optimized all reagents and performed cell stimulation and viral replication assays, and carried out all cellular phenotyping; DW performed virus stock production and quantification; EM performed biopsies and staining of Tfh cells from the macaque lymph node; MC and SAM collected clinical samples and provided cohort data for HIV infected subjects; AAA, FV and EM provided expert advice on experimental planning and data interpretation; JA, CC, FN and LRG wrote the manuscript; ASF, AAA, FV, EM, SAM and JCR read and commented on the manuscript.
Disclosure
The authors have no conflict of interest to declare.
Conflict of Interest
The authors have no conflicts of interest to declare.
References
- 1.Haase AT. Perils at mucosal front lines for HIV and SIV and their hosts. Nat Rev Immunol. 2005;5:783–792. doi: 10.1038/nri1706. [DOI] [PubMed] [Google Scholar]
- 2.Zhang Z, et al. Sexual transmission and propagation of SIV and HIV in resting and activated CD4+ T cells. Science. 1999;286:1353–1357. doi: 10.1126/science.286.5443.1353. [DOI] [PubMed] [Google Scholar]
- 3.Zhang ZQ, et al. Roles of substrate availability and infection of resting and activated CD4+ T cells in transmission and acute simian immunodeficiency virus infection. Proc Natl Acad Sci U S A. 2004;101:5640–5645. doi: 10.1073/pnas.0308425101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mehandru S, et al. Primary HIV-1 Infection Is Associated with Preferential Depletion of CD4+ T Lymphocytes from Effector Sites in the Gastrointestinal Tract. The Journal of Experimental Medicine. 2004;200:761–770. doi: 10.1084/jem.20041196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Habtezion A, Nguyen LP, Hadeiba H, Butcher EC. Leukocyte Trafficking to the Small Intestine and Colon. Gastroenterology. 2016;150:340–354. doi: 10.1053/j.gastro.2015.10.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Santangelo PJ, et al. Early treatment of SIV+ macaques with an alpha4beta7 mAb alters virus distribution and preserves CD4(+) T cells in later stages of infection. Mucosal Immunol. 2017 doi: 10.1038/mi.2017.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shale M, Schiering C, Powrie F. CD4(+) T-cell subsets in intestinal inflammation. Immunol Rev. 2013;252:164–182. doi: 10.1111/imr.12039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brenchley JM, Douek DC. The mucosal barrier and immune activation in HIV pathogenesis. Curr Opin HIV AIDS. 2008;3:356–361. doi: 10.1097/COH.0b013e3282f9ae9c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brenchley JM, et al. CD4+ T cell depletion during all stages of HIV disease occurs predominantly in the gastrointestinal tract. The Journal of experimental medicine. 2004;200:749–759. doi: 10.1084/jem.20040874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mehandru S, et al. Mechanisms of gastrointestinal CD4+ T-cell depletion during acute and early human immunodeficiency virus type 1 infection. J Virol. 2007;81:599–612. doi: 10.1128/JVI.01739-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guadalupe M, et al. Severe CD4+ T-cell depletion in gut lymphoid tissue during primary human immunodeficiency virus type 1 infection and substantial delay in restoration following highly active antiretroviral therapy. J Virol. 2003;77:11708–11717. doi: 10.1128/JVI.77.21.11708-11717.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mattapallil JJ, et al. Massive infection and loss of memory CD4+ T cells in multiple tissues during acute SIV infection. Nature. 2005;434:1093–1097. doi: 10.1038/nature03501. [DOI] [PubMed] [Google Scholar]
- 13.Veazey RS, et al. Gastrointestinal tract as a major site of CD4+ T cell depletion and viral replication in SIV infection. Science. 1998;280:427–431. doi: 10.1126/science.280.5362.427. [DOI] [PubMed] [Google Scholar]
- 14.Hamann A, Andrew DP, Jablonski-Westrich D, Holzmann B, Butcher EC. Role of alpha 4-integrins in lymphocyte homing to mucosal tissues in vivo. J Immunol. 1994;152:3282–3293. [PubMed] [Google Scholar]
- 15.Bargatze Rf JMABEC, Bargatze RF, Jutila MA, Butcher EC. Distinct roles of L-selectin and integrins alpha 4 beta 7 and LFA-1 in lymphocyte homing to Peyer’s patch-HEV in situ: the multistep model confirmed and refined. Immunity. 1995;3:99–108. doi: 10.1016/1074-7613(95)90162-0. [DOI] [PubMed] [Google Scholar]
- 16.Berlin C, et al. Alpha 4 beta 7 integrin mediates lymphocyte binding to the mucosal vascular addressin MAdCAM-1. Cell. 1993;74:185–195. doi: 10.1016/0092-8674(93)90305-a. [DOI] [PubMed] [Google Scholar]
- 17.Erle DJ, et al. Expression and function of the MAdCAM-1 receptor, integrin alpha 4 beta 7, on human leukocytes. Journal of immunology (Baltimore, Md: 1950) 1994;153:517–528. [PubMed] [Google Scholar]
- 18.Lehnert K, Print CG, Yang Y, Krissansen GW. MAdCAM-1 costimulates T cell proliferation exclusively through integrin alpha4beta7, whereas VCAM-1 and CS-1 peptide use alpha4beta1: evidence for “remote” costimulation and induction of hyperresponsiveness to B7 molecules. Eur J Immunol. 1998;28:3605–3615. doi: 10.1002/(SICI)1521-4141(199811)28:11<3605::AID-IMMU3605>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 19.Shimizu Y, van Seventer GA, Horgan KJ, Shaw S. Costimulation of proliferative responses of resting CD4+ T cells by the interaction of VLA-4 and VLA-5 with fibronectin or VLA-6 with laminin. J Immunol. 1990;145:59–67. [PubMed] [Google Scholar]
- 20.Teague TK, Lazarovits aI, McIntyre BW. Integrin alpha 4 beta 7 co-stimulation of human peripheral blood T cell proliferation. Cell adhesion and communication. 1994;2:539–547. doi: 10.3109/15419069409014217. [DOI] [PubMed] [Google Scholar]
- 21.Van Seventer GA, Shimizu Y, Horgan KJ, Shaw S. The LFA-1 ligand ICAM-1 provides an important costimulatory signal for T cell receptor-mediated activation of resting T cells. J Immunol. 1990;144:4579–4586. [PubMed] [Google Scholar]
- 22.Bernard A, Lamy &, Alberti I. The two-signal model of T-cell activation after 30 years. Transplantation. 2002;73:S31–35. doi: 10.1097/00007890-200201151-00011. [DOI] [PubMed] [Google Scholar]
- 23.Van Seventer GA, et al. Remote T cell co-stimulation via LFA-1/ICAM-1 and CD2/LFA-3: demonstration with immobilized ligand/mAb and implication in monocyte-mediated co-stimulation. Eur J Immunol. 1991;21:1711–1718. doi: 10.1002/eji.1830210719. [DOI] [PubMed] [Google Scholar]
- 24.Byrareddy SN, et al. Targeting alpha4beta7 integrin reduces mucosal transmission of simian immunodeficiency virus and protects gut-associated lymphoid tissue from infection. Nat Med. 2014;20:1397–1400. doi: 10.1038/nm.3715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cicala C, Arthos J, Fauci AS. HIV-1 envelope, integrins and co-receptor use in mucosal transmission of HIV. Journal of Translational Medicine. 2011;9 doi: 10.1186/1479-5876-9-S1-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martinelli E, et al. The frequency of alpha(4)beta(7)(high) memory CD4(+) T cells correlates with susceptibility to rectal simian immunodeficiency virus infection. J Acquir Immune Defic Syndr. 2013;64:325–331. doi: 10.1097/QAI.0b013e31829f6e1a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sivro A, et al. Integrin alpha4beta7 expression on peripheral blood CD4(+) T cells predicts HIV acquisition and disease progression outcomes. Sci Transl Med. 2018;10 doi: 10.1126/scitranslmed.aam6354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vaccari M, et al. Adjuvant-dependent innate and adaptive immune signatures of risk of SIV acquisition. Nature Medicine. 2016;22:762–770. doi: 10.1038/nm.4105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McKinnon LR, et al. Characterization of a human cervical CD4+ T cell subset coexpressing multiple markers of HIV susceptibility. J Immunol. 2011;187:6032–6042. doi: 10.4049/jimmunol.1101836. [DOI] [PubMed] [Google Scholar]
- 30.Kelley CF, et al. Differences in expression of gut-homing receptors on CD4+ T cells in black and white HIV-negative men who have sex with men. AIDS. 2016;30 doi: 10.1097/QAD.0000000000001062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kader M, et al. Alpha4(+)beta7(hi)CD4(+) memory T cells harbor most Th-17 cells and are preferentially infected during acute SIV infection. Mucosal Immunol. 2009;2 doi: 10.1038/mi.2009.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang X, et al. Monitoring alpha4beta7 integrin expression on circulating CD4+ T cells as a surrogate marker for tracking intestinal CD4+ T-cell loss in SIV infection. Mucosal Immunol. 2009;2:518–526. doi: 10.1038/mi.2009.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Krzysiek R, et al. Preferential and persistent depletion of CCR5+ T-helper lymphocytes with nonlymphoid homing potential despite early treatment of primary HIV infection. Blood. 2001;98:3169–3171. doi: 10.1182/blood.v98.10.3169. [DOI] [PubMed] [Google Scholar]
- 34.Landegren U, Andersson J, Wigzell H. Mechanism of T lymphocyte activation by OKT3 antibodies. A general model for T cell induction. European Journal of Immunology. 1984;14:325–328. doi: 10.1002/eji.1830140409. [DOI] [PubMed] [Google Scholar]
- 35.Chen a, Engel P, Tedder TF. Structural requirements regulate endoproteolytic release of the L-selectin (CD62L) adhesion receptor from the cell surface of leukocytes. The Journal of experimental medicine. 1995;182:519–530. doi: 10.1084/jem.182.2.519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kahn J, Ingraham RH, Shirley F, Migaki GI, Kishimoto TK. Membrane proximal cleavage of L-selectin: Identification of the cleavage site and a 6-kD transmembrane peptide fragment of L-selectin. Journal of Cell Biology. 1994;125:461–470. doi: 10.1083/jcb.125.2.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Iwata M, et al. Retinoic acid imprints gut-homing specificity on T cells. Immunity. 2004;21:527–538. doi: 10.1016/j.immuni.2004.08.011. [DOI] [PubMed] [Google Scholar]
- 38.Lu X, et al. Preferential loss of gut-homing alpha4beta7 CD4(+) T cells and their circulating functional subsets in acute HIV-1 infection. Cell Mol Immunol. 2016;13:776–784. doi: 10.1038/cmi.2015.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stassen M, et al. Human CD25 + regulatory T cells : two subsets defined by the integrins a4b7 or a4b1 confer distinct suppressive properties upon CD4 + T helper cells. Eur J Immunol. 2004;34:1303–1311. doi: 10.1002/eji.200324656. [DOI] [PubMed] [Google Scholar]
- 40.Monteiro P, et al. Memory CCR6+CD4+ T cells are preferential targets for productive HIV type 1 infection regardless of their expression of integrin beta7. J Immunol. 2011;186:4618–4630. doi: 10.4049/jimmunol.1004151. [DOI] [PubMed] [Google Scholar]
- 41.Planas D, et al. HIV-1 selectively targets gut-homing CCR6+CD4+ T cells via mTOR-dependent mechanisms. JCI Insight. 2017;2 doi: 10.1172/jci.insight.93230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li P, et al. Stimulating the RIG-I pathway to kill cells in the latent HIV reservoir following viral reactivation. Nat Med. 2016;22:807–811. doi: 10.1038/nm.4124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.MacDonald KS, et al. Vitamin A and risk of HIV-1 seroconversion among Kenyan men with genital ulcers. AIDS. 2001;15:635–639. doi: 10.1097/00002030-200103300-00014. [DOI] [PubMed] [Google Scholar]
- 44.Engelhardt BG, JEC Homing in on Acute Graft vs Host Disease: Tissue-specific T Regulatory and Th17 cells. Curr Top Microbiol Immunol. 2010;341:121–146. doi: 10.1007/82_2010_24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Martinelli E, et al. HSV-2 infection of dendritic cells amplifies a highly susceptible HIV-1 cell target. PLoS Pathogens. 2011;7:2–3. doi: 10.1371/journal.ppat.1002109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jovani M, Danese S. Vedolizumab for the treatment of IBD: a selective therapeutic approach targeting pathogenic a4b7 cells. Current Drug Targets. 2013;14:1433–1443. doi: 10.2174/13894501113146660206. [DOI] [PubMed] [Google Scholar]
- 47.Grant AJ, Lalor PF, Hübscher SG, Briskin M, Adams DH. MAdCAM-1 expressed in chronic inflammatory liver disease supports mucosal lymphocyte adhesion to hepatic endothelium (MAdCAM-1 in chronic inflammatory liver disease) Hepatology. 2001;33:1065–1072. doi: 10.1053/jhep.2001.24231. [DOI] [PubMed] [Google Scholar]
- 48.Kelly KA, Rank RG. Identification of homing receptors that mediate the recruitment of CD4 T cells to the genital tract following intravaginal infection with Chlamydia trachomatis. Infect Immun. 1997;65:5198–5208. doi: 10.1128/iai.65.12.5198-5208.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Goode D, et al. HSV-2-driven increase in the expression of alpha4beta7 correlates with increased susceptibility to vaginal SHIV(SF162P3) infection. PLoS Pathog. 2014 Dec;10 doi: 10.1371/journal.ppat.1004567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Salmi M, et al. Immune cell trafficking in uterus and early life is dominated by the mucosal addressin MAdCAM-1 in humans. Gastroenterology. 2001;121:853–864. doi: 10.1053/gast.2001.27968. [DOI] [PubMed] [Google Scholar]
- 51.Szabo MC, Butcher EC, McEvoy LM. Specialization of Mucosal Follicular Dendritic Cells Revealed by Mucosal Addressin-Cell Adhesion Molecule-1 Display. Journal of Immunology. 1997:5584–5588. [PubMed] [Google Scholar]
- 52.Jelicic K, et al. The HIV-1 envelope protein gp120 impairs B cell proliferation by inducing TGF-beta1 production and FcRL4 expression. Nat Immunol. 2013;14:1256–1265. doi: 10.1038/ni.2746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Velu V, et al. Induction of Th1-Biased T Follicular Helper (Tfh) Cells in Lymphoid Tissues during Chronic Simian Immunodeficiency Virus Infection Defines Functionally Distinct Germinal Center Tfh Cells. J Immunol. 2016;197:1832–1842. doi: 10.4049/jimmunol.1600143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Perreau M, et al. Follicular helper T cells serve as the major CD4 T cell compartment for HIV-1 infection, replication, and production. The Journal of experimental medicine. 2013;210:143–156. doi: 10.1084/jem.20121932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Thornhill JP, Fidler S, Klenerman P, Frater J, Phetsouphanh C. The Role of CD4+ T Follicular Helper Cells in HIV Infection: From the Germinal Center to the Periphery. Frontiers in Immunology. 2017;8:46–46. doi: 10.3389/fimmu.2017.00046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Byrareddy SN, et al. Sustained virologic control in SIV+ macaques after antiretroviral and α4β7 antibody therapy. Science. 2016;354:197–LP-202. doi: 10.1126/science.aag1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Migueles SA, et al. Lytic granule loading of CD8+ T cells is required for HIV-infected cell elimination associated with immune control. Immunity. 2008;29:1009–1021. doi: 10.1016/j.immuni.2008.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Migueles SA, et al. Defective human immunodeficiency virus-specific CD8+ T-cell polyfunctionality, proliferation, and cytotoxicity are not restored by antiretroviral therapy. J Virol. 2009;83:11876–11889. doi: 10.1128/JVI.01153-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.