Abstract
Background
Nakchim is a kind of neck pain syndrome that causes neck pain and stiffness without obvious trauma in East Asian traditional medicine. We aimed to summarize and critically evaluate the evidence regarding the efficacy and safety of acupressure on nakchim.
Methods
We searched eight databases for studies published up to August 29, 2017. Clinical studies evaluating the efficacy of acupressure on nakchim were included. The acupressure methods of included studies were divided into proximal acupressure performed on acupuncture points located in neck and shoulder, and distal acupressure performed on acupuncture points located in other areas. Overall clinical effective rate (CER) and immediately cured rate (ICR), which means rate of the symptom totally resolved after one treatment session, were calculated as mean percentage with 95% confidence interval. All included studies were assessed for methodological quality.
Results
Two case studies and 13 case series with 1037 participants were included, and 17 types of proximal acupuncture points and 14 types of distal acupuncture points were used. The most commonly used proximal and distal acupuncture points were GB20 and GB39, respectively. The CER in one study using both proximal and distal acupressure was 100%. The CER and ICR in studies using only proximal acupressure was 95.65% and 71.61%, respectively. The CER and ICR in studies using only distal acupressure was 99.37% and 69.08%, respectively. Eight studies performed simple acupressure technique using one acupuncture point, of which SI11, GB39, BL57, and TE3 were used. None of the studies reported adverse events.
Conclusion
This review suggests that acupressure may be effective on nakchim. However, it is not conclusive due to low methodological quality and low evidence level of included studies.
Keywords: Acupressure, Neck pain, Oriental medicine
1. Introduction
In East Asian traditional medicine (EATM), nakchim ( 枕) usually refers to a kind of cervical pain accompanied by the stiffness of the muscles around the neck. The range of neck movement is limited, and pain occurs after sleeping. The causes of this condition are wrong sleeping posture, neck muscle abnormality, and wind-cold assailing.1
枕) usually refers to a kind of cervical pain accompanied by the stiffness of the muscles around the neck. The range of neck movement is limited, and pain occurs after sleeping. The causes of this condition are wrong sleeping posture, neck muscle abnormality, and wind-cold assailing.1
This term was translated into “stiff neck” according to the World Health Organization's (WHO) International Standard Terminologies on Traditional Medicine and was defined as “acute inflammation or sprain of the soft tissue of the neck”.2 Despite this translation, the original term, nakchim, incorporates pathological information that the condition is associated with sleeping, while the translated term does not. This is why the term “stiff neck,” which can be confused with a simple symptom of stiffness that may occur in the neck, cannot accurately represent the original condition. Furthermore, in East Asia, such as Korea and China, the term nakchim is more commonly used instead of the term suggested by WHO. Therefore, in this review, we used the original term instead of the translated term.
In 2011, a Delphi consensus conducted during the development of the acupuncture clinic practice guidelines for cervical pain in Korea suggested that nakchim can be one of the formal EATM diagnoses in cervical pain.3 Although there is no standard diagnostic criterion for nakchim, in a double-blind, randomized controlled trial (RCT) of nakchim patients, it was defined as follows: the pain and restricted motion range of neck occurred within 2 weeks; either unilateral or bilateral side can be affected; there should be no history of neck trauma; and there should be no abnormalities on radiological examinations.4
Although acupuncture and acupressure share same treatment points, the so-called acupuncture points, the latter is non-invasive and relatively safe because it uses human fingers or tools to press some acupuncture points without skin penetration. Acupressure has been recognized for its effectiveness in various health problems.5, 6 Because there is no legal restriction such as medical license for treatment, it has low entry barriers. It can be performed by patients themselves or healthcare providers such as caregivers or nurses, although some technical knowledge is still required to perform acupressure.6, 7, 8 The role of caregivers and nurses is very important in patient-centered care to provide the optimal treatment environment for patients.9, 10 In this situation, acupressure is a sharable treatment among caregivers, nurses, and doctors who manage patients in the front line, and if sufficient education is given, it is also a promising treatment that patients can perform to improve their own health.6
In this review, we systematically reviewed to analyze the acupressure methods on nakchim, and to assess its therapeutic effect.
2. Methods
2.1. Search strategy
We conducted a systematic review in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.11 A systematic search was conducted on eight databases; PubMed, EMBASE, Cochrane Central Register of Controlled Trials (CENTRAL), China National Knowledge Infrastructure (CNKI), Japan Science & Technology Information Aggregator, Electronic (J-STAGE), Research Information Sharing Service (RISS), Koreanstudies Information Service System (KISS), and Oriental Medicine Advanced Searching Integrated System (OASIS). Table 1 shows the search strategies implemented in each database. All papers published until August 29, 2017 were searched.
Table 1.
Search Strategies
| DB: PubMed, CENTRAL |
| (“neck stiffness” OR “stiff neck” OR “acute fibrositis”) AND (“acupressure” [MeSH Terms] OR “acupressure”) |
| DB: EMBASE |
| #1 “neck stiffness”/exp OR “neck stiffness” OR “stiff neck”/exp OR “stiff neck” OR “acute fibrositis” |
| #2 acupressure |
| #3 #1 AND #2 |
| DB: CNKI |
| (落枕 OR 项强 OR 失枕 OR neck stiffness OR stiff neck) AND (指压 OR 按压 OR 穴位按摩 OR acupressure) |
| DB: J-STAGE |
| 落枕 OR 项强 OR 失枕 OR neck stiffness OR stiff neck |
| DB: RISS, OASIS, KISS |
낙 OR OR  OR OR  OR OR  枕 枕 |
2.2. Study selection
In this study, the inclusion criteria were set according to an existing RCT and a textbook in China as follows.4, 12 (1) Patient: Patients should be suffering from pain and restricted motion range in the neck, which occurred within 2 weeks, and have no history of physical trauma or no abnormality on radiological examination. However, even if detailed medical histories were not reported, studies reporting that patients are suffering from nakchim were also included. (2) Intervention: Patients should be treated with acupressure. Acupressure was defined as a treatment to achieve therapeutic effects by pressing acupuncture points using a finger or a non-invasive tool. (3) Comparison: There was no restriction on comparison. (4) Outcome: Study should report the treatment effect using outcome measurements such as Visual Analog Scale (VAS), Numeric Rating Scale (NRS), Neck Disability Index (NDI), or clinical effective rate (CER) based on improvement of the symptoms. (5) Design: Clinical studies including case reports, case series, before–after study, and controlled study were allowed. Two authors independently selected relevant studies, and any disagreement was solved through discussion.
2.3. Data extraction
The study design, sample size, treatment method, duration and frequency of treatment, concurrent treatment, outcomes, results, and any adverse events reported were extracted from each study using a standardized extraction form. Two authors independently extracted the data and any disagreement was solved through discussion.
2.4. Data analysis
In order to distinguish the effects of physical massage on the affected muscle, the acupressure methods of included studies were divided into two categories: proximal acupressure performed on acupuncture points located in neck and shoulder, and distal acupressure performed on acupuncture points located in other areas. Overall CER of acupressure among included studies was calculated. Moreover, immediately, cured rate (ICR), which means rate of the symptom totally resolved after one treatment session, was also calculated. Overall CER and ICR were presented as mean percentage with 95% confidence interval (CI). The clinical effects of simple acupressure that used only one acupuncture point were analyzed. We also analyzed the clinical effect according to whether Dong-qi therapy was performed during the acupressure.
2.5. Methodological quality assessment
Although the methodological quality was supposed to be assessed by using different assessment tools depending on the design of the study included, the NIH's Quality Assessment of Case Series Studies was only used because all included studies were case series or case reports.13 Two authors independently assessed the methodological quality of included studies, and any disagreement was resolved through discussion.
3. Results
3.1. Study characteristics
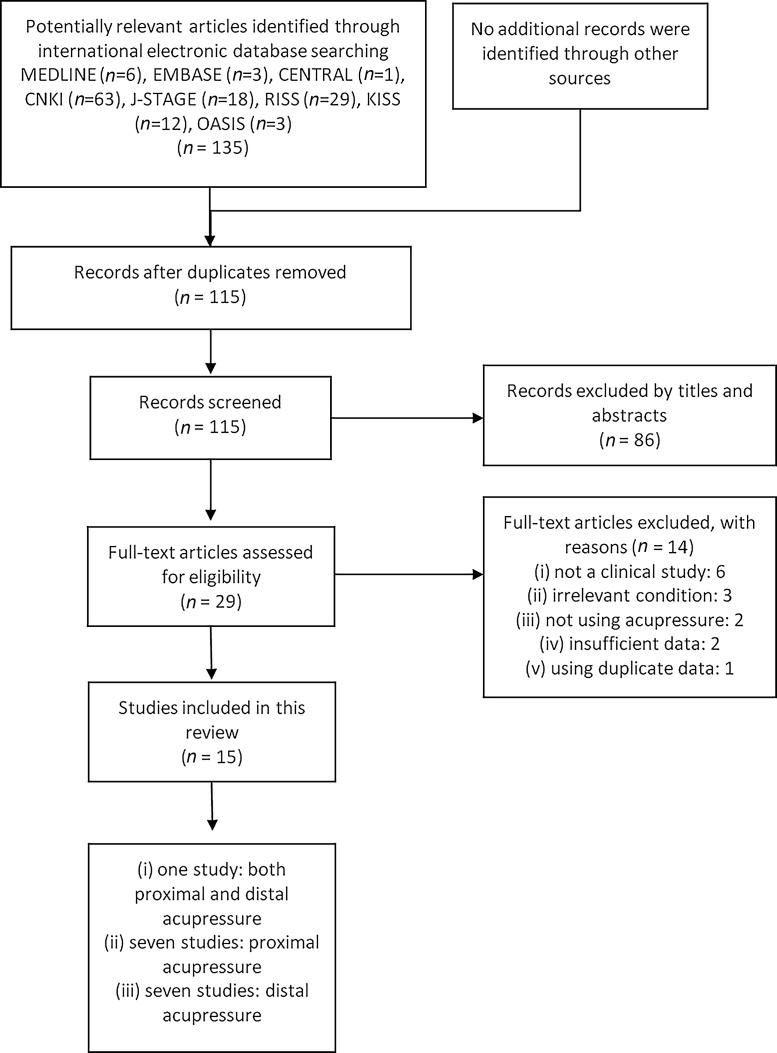
A total of 135 records were identified, and 15 studies were included in this review (Fig. 1).14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28 All studies were performed in China and were either case reports or case series, with a total of 1037 patients. One study14 performed both proximal and distal acupressure, seven studies15, 16, 17, 18, 19, 20, 21 performed only proximal acupressure, and the remaining seven studies22, 23, 24, 25, 26, 27, 28 only performed distal acupressure. All the practitioners were doctors (Table 2).
Fig. 1.
The PRISMA flow chart of the literature screening and selection process.
Table 2.
General Characteristics of Included Studies
| Study | Sample size | Treatment time per session (min) | Treatment period (day) | Treatment frequency (session per day) | Dong-qi therapy | Concurrent therapy | Results |
|---|---|---|---|---|---|---|---|
| Both proximal and distal acupressure | |||||||
| Hu (1999)14 | 9 | 2–4 | 3–5 | 1–2 | NA | Passive stretching of the strained muscle | Cured: 9 |
| Proximal acupressure | |||||||
| Wei (199915 | 39 | 6–8 | 1 | 1 | Performed | Massage on neck for 1–2 min | Cured: 32, markedly improved: 7 |
| Wang (2001)*,16 | 30 | 3–6 | 1 | 1 | Performed | NA | Cured: 15, markedly improved: 8, improved: 4, ineffective: 3 |
| Xiang (2003)17 | 112 | 1–3 | 3 | 1–2 | Performed | NA | Cured: 93 (cured through a single treatment: 54), improved: 15, ineffective: 4 |
| Huang (2003*,18 | 45 | 10 | 3 | 1 | Performed | Massage on neck and shoulder | Cured: 39, markedly improved: 6 |
| Lu (2004)19 | 50 | 2–3 | NR | NR | NA | Tuina, massage, extension therapy, etc. | Cured through a single treatment: 32, cured through two treatments: 5, cured through three treatments: 1, markedly improved through multiple treatments: 2, improved: 1, ineffective: 9 |
| Wang (2004)20 | 36 | 15–25 | NR | NR | Performed | NA | Cured through a single treatment: 32, cured through two treatments: 3, cured through six treatments: 1 |
| Li (2014)21 | 400 | 4 | NR | NR | NA | Massage on neck and shoulder, herbal medicine, hot massage, physical therapy, acupuncture, etc. | Cured: 340, markedly improved: 25, improved: 20, ineffective: 15 |
| Distal acupressure | |||||||
| Zhang (1961)*,22 | 1 | 5–7 | 1 | 1 | Performed | Massage on neck and shoulder for 10–15 min | Cured: 1 |
| Li (1984)*,23 | 1 | 2–5 | 1 | 1 | performed | NA | Cured: 1 |
| Zhang (1988)*,24 | 20 | 1–2 | NR | NR | Performed | NA | Cured through a single treatment: 17, cured through two treatments: 2, markedly improved: 1 |
| Mao (1989)25 | 24 | 3 | 1–2 | 1 | Performed | NA | Cured through a single treatment: 14, cured through two treatments: 3, markedly improved through a single treatment: 6, markedly improved through two treatments: 1 |
| Liang (1999)*,26 | 54 | 15–20 | 2 | 1 | Performed | NA | Cured: 41, improved: 11, ineffective: 2 |
| Li (2007)*,27 | 136 | 3–5 | 1–2 | 1 | Performed | NA | Cured through a single treatment: 87, cured through two treatments: 31, Improved: 18 |
| Liu (2012)*,28 | 80 | 3–5 | 1–4 | 1 | Performed | NA | Cured through a single treatment: 61, cured through two treatments: 13, cured through three to four treatments: 6 |
Abbreviations: NA, not applicable; NR, not recorded.
Study performing simple acupressure, which uses only one acupuncture point.
3.2. Methodological quality of clinical studies
All studies described the purpose of reporting the clinical effects of acupressure in patients with nakchim. There were only three studies17, 21, 27 that clearly described nakchim as rapid onset, neck pain with limited motion range, and no abnormalities in radiological examinations. Except for two case reports with one participant each,22, 23 the remaining studies14, 15, 16, 17, 18, 19, 20, 21, 24, 25, 26, 27, 28 did not describe whether the cases were consecutive. Except for two case reports,22, 23 five studies14, 16, 19, 24, 26 reported insufficient demographic information to analyze, and only two15, 20 of the remaining eight studies were on patients with similar age. In all of the studies, onset was within 3 days. Except for four studies19, 20, 21, 24 in which no treatment duration was specified, all of the other studies clearly described the intervention method. The results were all raw data of CER and/or ICR, and there were nine studies15, 16, 17, 18, 20, 21, 26, 27, 28 that reported clear criteria for cured, markedly improved, improved and/or not improved. Except for four studies19, 20, 21, 24 that did not report a follow-up period, the remaining studies were evaluated as appropriate with a follow-up period of 2 weeks or less. There were no studies using statistical methods. Eight studies15, 16, 17, 18, 20, 26, 27, 28 were evaluated to describe the results satisfactorily (Table 3).
Table 3.
Methodological Quality Assessment of Included Studies
| Study | NIH's Quality Assessment of Case Series Studies |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
| Both proximal and distal acupressure | |||||||||
| Hu (1999)14 | Yes | No | NR | NR | Yes | No | Yes | NA | No |
| Proximal acupressure | |||||||||
| Wei (1999)15 | Yes | No | NR | Yes | Yes | Yes | Yes | NA | Yes |
| Wang (2001)16 | Yes | No | NR | NR | Yes | Yes | Yes | NA | Yes |
| Xiang (2003)17 | Yes | Yes | NR | No | Yes | Yes | Yes | NA | Yes |
| Huang (2003)18 | Yes | No | NR | No | Yes | Yes | Yes | NA | Yes |
| Lu (200419 | Yes | No | NR | NR | No | No | NR | NA | No |
| Wang (2004)20 | Yes | No | NR | Yes | No | Yes | NR | NA | Yes |
| Li (2014)21 | Yes | Yes | NR | No | No | Yes | NR | NA | No |
| Distal acupressure | |||||||||
| Zhang (1961)22 | Yes | No | NA | NA | Yes | No | Yes | NA | No |
| Li (1984)23 | Yes | No | NA | NA | Yes | No | Yes | NA | No |
| Zhang (1988)24 | Yes | No | NR | NR | No | No | NR | NA | No |
| Mao (1989)25 | Yes | No | NR | No | Yes | No | Yes | NA | No |
| Liang (1999)26 | Yes | No | NR | NR | Yes | Yes | Yes | NA | Yes |
| Li (2007)27 | Yes | Yes | NR | No | Yes | Yes | Yes | NA | Yes |
| Liu (2012)28 | Yes | No | NR | No | Yes | Yes | Yes | NA | Yes |
Abbreviations: NA, not applicable; NR, not recorded.
NIH's Quality Assessment of Case Series Studies consists of the following questions: “1) Was the study question or objective clearly stated?; 2) Was the study population clearly and fully described, including a case definition?; 3) Were the cases consecutive?; 4) Were the subjects comparable?; 5) Was the intervention clearly described?; 6) Were the outcome measures clearly defined, valid, reliable, and implemented consistently across all study participants?; 7) Was the length of follow-up adequate?; 8) Were the statistical methods well-described?; and 9) Were the results well-described?”
3.3. Acupuncture points for acupressure on nakchim
Seventeen types of 30 proximal acupuncture points were used as basic acupuncture points. Among them, GB20 was most frequently used, that is, 4 times; GB21 was used 3 times; and SI15, ST12, BL11, TE16, LI17, SI11, BL10, and GV16 were used twice each. SI14, GV14, LI18, GB12, SI16, BL12, and GB6 were used once each. Nine types of 14 distal acupuncture points were used as basic acupuncture points. Among them, GB39 was most frequently used at 4 times, and BL57 and TE3 were used twice, respectively. BL60, EX-UE8, LI5, TE10, LI4, and SI3 were used once each. As a whole, acupuncture points on gallbladder meridian were the most commonly used (13 times), followed by acupuncture points on bladder meridian (8 times) and acupuncture points on small intestine meridian (7 times).
Three studies14, 15, 20 used A-Shi points. The number of acupuncture points used was counted except for A-Shi points. In seven studies performing proximal acupressure,15, 16, 17, 18, 19, 20, 21 an average of 2.57 acupuncture points was used, while in seven studies performing distal acupressure,22, 23, 24, 25, 26, 27, 28 an average of 1.14 acupuncture points was used (Table 4).
Table 4.
Details of Acupressure on Nakchim
| Study | Sample size | Acupuncture points | Treatment side | Cured after one treatment session | ICR | Improved | CER |
|---|---|---|---|---|---|---|---|
| Both proximal and distal acupressure | |||||||
| Hu (1999)14 | 9 | 1) SCM: LI17, LI18, TE16, SI16, LI4, LI5, TE3, TE10, and A-Shi points 2) DM: GB20, SI15, GB21, GV14, BL11, SI14, BL10, GB39, SI3, and A-Shi points 3) PCM: GV16, BL10, SI15, GV14, SI16, BL11, BL60, SI3, and A-Shi points |
NR | NA | NA | 9 | 100% |
| Proximal acupressure | |||||||
| Wei (1999)15 | 39 | GB20, TE16, GB21, SI15, and A-Shi points | NR | 32 | 82.05% | 39 | 100% |
| Wang (2001)*,16 | 30 | SI11 | Affected or bilateral side | 15 | 50.00% | 27 | 90.00% |
| Xiang (2003)17 | 112 | GB6 and GB20 | Affected side | NA | NA | 108 | 96.40% |
| Huang (2003)*,18 | 45 | SI11 | Bilateral side | NA | NA | 45 | 100% |
| Lu (200419 | 50 | ST12 and Li17 | Affected side | 32 | 64.00% | 41 | 82.00% |
| Wang (2004)20 | 36 | GB20, BL10, BL11, BL12, and A-Shi points | Affected side | 32 | 88.89% | 36 | 100% |
| Li (2014)21 | 400 | GB20, GB12, ST12, and GB21 | Affected side | NA | NA | 385 | 96.25% |
| Subtotal | 712 | 111 | 71.61% (95% CI, 64.51–78.71) 111/155 |
681 | 95.65% (95% CI, 94.15–97.15) 681/712 |
||
| Distal acupressure | |||||||
| Zhang (1961)*,22 | 1 | GB39 | NR | 1 | 100% | 1 | 100% |
| Li (1984)*,23 | 1 | BL57 | Unaffected side | 1 | 100% | 1 | 100% |
| Zhang (1988)*,24 | 20 | TE3 | Affected side | 17 | 85.00% | 20 | 100% |
| Mao (1989)25 | 24 | GB39 and EX-UE8 | Affected side | 14 | 58.33% | 24 | 100% |
| Liang (1999)*,26 | 54 | BL57 | Bilateral side | NA | NA | 52 | 96.30% |
| Li (2007)*27 | 136 | GB39 | bilateral side | 87 | 63.97% | 136 | 100% |
| Liu (2012)*,28 | 80 | TE3 | Bilateral side | 61 | 76.25% | 80 | 100% |
| Subtotal | 316 | 181 | 69.08% (95% CI, 63.49–74.68) 181/262 |
314 | 99.37% (95% CI, 98.49–100.24) 314/316 |
||
Abbreviations: CER, clinical effective rate; CI, confidence interval; DM, deltoid muscle; ICR, immediately cured rate; NA, not applicable; NR, not recorded; PCM, posterior cervical muscle; SCM, sternocleidomastoid muscle.
Study performing simple acupressure, which uses only one acupuncture point.
3.4. The effects of both proximal and distal acupressure
Hu14 classified the affected muscle of nakchim of nine patients into sternocleidomastoid muscle, deltoid muscle, and posterior cervical muscle, and performed both proximal and distal acupressure for 2–4 minutes per each treatment session, with 1–2 sessions daily for 3–5 days. In the case of sternocleidomastoid muscle, LI17, LI18, TE16, SI16, LI4, LI5, TE3, TE10, and A-Shi points were used; in deltoid muscle, GB20, SI15, GB21, GV14, BL11, SI14, BL10, GB39, SI3, and A-Shi points were used; and in posterior cervical muscle, GV16, BL10, SI15, GV14, SI16, BL11, BL60, SI3, and A-Shi points were used. Passive stretching of strained muscle was performed after the acupressure. As a result, the symptoms of all nine patients were cured. The CER was 100%.
3.5. The effects of proximal acupressure
A total of 712 patients were included in the seven studies of proximal acupressure.15, 16, 17, 18, 19, 20, 21 Of these, as 681 patients showed improvement in symptoms, the overall CER was 95.65% (95% CI, 94.15–97.15). In four studies involving 155 patients,15, 16, 19, 20 ICR was reported, ranging from 50% to 89%. As the number of patients whose symptoms were cured after one treatment session was 111, the overall ICR was 71.61% (95% CI, 64.51–78.71).
Wei15 performed one treatment session of proximal acupressure for 6–8 minutes on 39 patients, and GB20, TE16, GB21, SI15, and A-Shi points were used. Massage on neck for 1–2 minutes was performed after the acupressure. As a result, 32 patients were cured, and 7 were markedly improved. The CER was 100%. Wang16 performed one treatment session of proximal acupressure for 3–6 minutes on 30 patients, and SI11 was used. As a result, 15 patients were cured, 8 were markedly improved, 4 were improved, and 3 were not improved. The CER was 90.00%. Xiang et al17 performed 1–3 minutes of proximal acupressure per each treatment session, with 1–2 sessions daily for 3–5 days on 112 patients, and GB6 and GB20 were used as basic acupuncture points. If the symptoms were severe, GB21, SI14, and GV14 were added. As a result, 93 patients were cured, 15 were improved, and 4 were not improved. The CER was 96.40%. Huang18 performed one treatment session of proximal acupressure for 10 minutes daily for 3 days on 45 patients, and SI11 was used. Massage on neck and shoulder was performed after the acupressure. As a result, 39 patients were cured, and 6 were markedly improved. The CER was 100%. Lu19 performed treatment sessions of proximal acupressure for 2–3 minutes on 50 patients, and ST12 and Li17 were used. If the symptoms were severe, GB20 and EX-UE8 were added. If periarthritis of the shoulder was presented, LI15 and SI11 were added. Tuina, massage, and extension therapy were performed after the acupressure. As a result, 38 patients were cured, 2 were markedly improved, 1 was improved, and 9 were not improved. The CER was 82.00%. Wang20 performed treatment sessions of proximal acupressure for 15–25 minutes on 36 patients, and GB20, BL10, BL11, BL12, and A-Shi points were used. As a result, all of them were cured. The CER was 100%. Li21 performed treatment sessions of proximal acupressure for 4 minutes on 400 patients, and GB20, GB12, ST12, and GB21 were used. Concurrent treatments including massage on neck and shoulder, herbal medicine, hot massage, physical therapy, and acupuncture were performed. As a result, 340 patients were cured, 24 were markedly improved, 20 were improved, and 15 were not improved. The CER was 96.25%.
3.6. The effects of distal acupressure
A total of 316 patients were included in the seven studies on distal acupressure.22, 23, 24, 25, 26, 27, 28 Of these, as 314 patients showed improvement of symptoms, the overall CER was 99.37% (95% CI, 98.49–100.24). In six studies involving 262 patients,22, 23, 24, 25, 27, 28 ICR was reported, ranging from 96.30% to 100%. As the number of patients whose symptoms were cured after one treatment session was 181, the overall ICR was 69.08% (95% CI, 63.49–74.68).
Zhang22 performed one treatment session of distal acupressure for 5–7 minutes on one patient, and GB39 was used. Massage on neck and shoulder for 10–15 minutes was performed after the acupressure. As a result, the patient was cured. Li et al23 performed one treatment session of distal acupressure for 2–5 minutes on one patient, and BL57 was used. As a result, the patient was cured. Zhang et al24 performed treatment sessions of distal acupressure for 1–2 minutes on 20 patients, and TE3 was used. As a result, 19 patients were cured, and 1 was markedly improved. The CER was 100%. Mao25 performed each treatment session of distal acupressure for 3 minutes, 1 session daily for 1–2 days on 24 patients, and GB39 and EX-UE8 were used. As a result, 17 patients were cured, and 7 were markedly improved. The CER was 100%. Liang26 performed each treatment session of distal acupressure for 15–20 minutes, 1 session daily for 2 days on 54 patients, and BL57 was used. As a result, 41 patients were cured, 11 were markedly improved, and 2 were not improved. The CER was 96.30%. Li27 performed each treatment session of distal acupressure for 3–5 minutes, 1 session daily for 1–2 days on 136 patients, and GB39 was used. As a result, 118 patients were cured, and 18 were improved. The CER was 100%. Liu28 performed each treatment session of distal acupressure for 3–5 minutes, 1 session daily for 1–2 days on 80 patients, and TE3 was used. As a result, all of the patients were cured. The CER was 100%.
3.7. The effects of simple acupressure
Simple acupressure using one acupuncture point was performed in eight studies: two studies16, 18 performed proximal acupressure, and the remaining six studies22, 23, 24, 26, 27, 28 performed distal acupressure.
Two studies involving 75 patients16, 18 performed simple proximal acupressure on SI11. As 72 patients showed improvement of symptoms, the overall CER was 96.00% (95% CI, 91.57–100.44). In the one study involving 30 patients,16 the number of patients whose symptoms were cured after one treatment session was reported as 15. Therefore, the ICR was 50.00% (95% CI, 32.11–67.89).
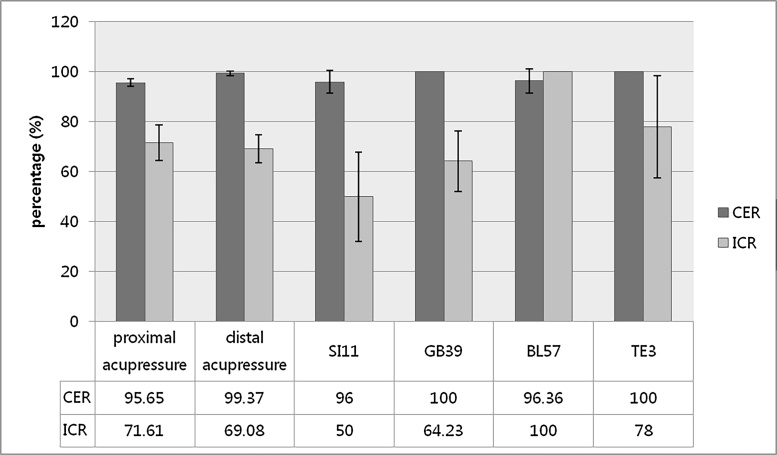
Six studies involving 292 patients22, 23, 24, 26, 27, 28 performed simple distal acupressure, and GB39,22, 27 BL57,23, 26 and TE324, 28 each were used in two studies, respectively. As 290 patients showed improvement of symptoms, the overall CER was 99.32% (95% CI, 98.37–100.26). In the five studies involving 238 patients,22, 23, 24, 27, 28 the number of patients whose symptoms were cured after one treatment session was reported as 167. Therefore, the overall ICR was 70.17% (95% CI, 64.36–75.98). The number of patients with improvement of symptoms after acupressing GB39, BL57, and TE3 was 137 out of 137, 53 out of 55, and 100 out of 100, respectively. Therefore, the overall CERs for each acupuncture point were 100%, 96.36% (95% CI, 91.42–101.31), and 100%, respectively. The number of patients whose symptoms were cured after one treatment session of GB39, BL57, and TE3 was 88 out of 137, 1 out of 1, and 78 out of 100, respectively. Therefore, the overall ICRs for each acupuncture point were 64.23% (95% CI, 52.11–76.35), 100%, and 78.00% (95% CI, 57.45–98.55), respectively (Table 5) (Fig. 2).
Table 5.
The Effects of Simple Acupressure in Included Studies
| Acupuncture point | Cured after one treatment session | ICR | Improved | CER |
|---|---|---|---|---|
| SI11 | 15 (out of 30) | 70.17% (95% CI, 64.36–75.98) |
72 (out of 75) | 50.00% (95% CI, 32.11–767.89) |
| GB39 | 88 (out of 137) | 64.23% (95% CI, 52.11–776.35) |
137 (out of 137) | 100% |
| BL57 | 1 (out of 1) | 100% | 53 (out of 55) | 96.36% (95% CI, 91.42–7101.31) |
| TE3 | 78 (out of 100) | 78.00% (95% CI, 57.45–798.55) |
100 (out of 100) | 100% |
| Total | 181 | 69.08% (95% CI, 63.49–774.68) 181/262 |
314 | 99.37% (95% CI, 98.49–7100.24) 314/316 |
Abbreviations: CER, clinical effective rate; CI, confidence interval; ICR, immediately cured rate.
Note. “SI11 located in the scapular region, in the depression between the upper one-third and lower two-thirds of the line connecting the midpoint of the spine of the scapula with the inferior angle of the scapula. GB39 located on the fibular aspect of the leg, anterior to the fibula, and 3 B-cun proximal to the prominence of the lateral malleolus. BL57 located on the posterior aspect of the leg, at the connecting point of the calcaneal tendon with the two muscle bellies of the gastrocnemius muscle. TE3 located on the dorsum of the hand, between the 4th and 5th metacarpal bones, in the depression proximal to the 4th metacarpophalangeal joint.” (Korean Medicine Convergence Research Information Center. KMCRIC standard acupuncture point database. KMCRIC Website. http://www.kmcric.com/knowledge/acupoint. Published 2008. Accessed September 19, 2017.)
Fig. 2.
The clinical effect of Acupressure on Nakchim.
Abbreviations: CER, clinical effective rate; ICR, immediately cured rate.
3.8. Dong-qi therapy
Twelve studies15, 16, 17, 18, 20, 22, 23, 24, 25, 26, 27, 28 involving 578 patients performed Dong-qi therapy. The Dong-qi therapy on nakchim was performed by slowly moving the affected area simultaneously with acupressure. As 569 patients showed improvement of symptoms, the overall CER was 98.44% (95% CI, 95.37–101.51). The number of patients whose symptoms were cured after one treatment session was 260 out of 367; therefore, the overall ICR was 70.84% (95% CI, 54.33–87.36).
Three studies involving 459 patients14, 19, 21 did not perform Dong-qi therapy. As 435 patients showed improvement of symptoms, the overall CER was 94.77% (95% CI, 86.50–103.04). The number of patients whose symptoms were cured after one treatment session was 32 out of 50; therefore, the overall ICR was 64.00% (95% CI, 3.18–124.82).
3.9. Safety
None of the studies reported adverse events.
4. Discussion
This review was conducted to assess the efficacy of acupressure on nakchim. Fifteen case studies or case series were included, and 17 types of proximal acupuncture points and 14 types of distal acupuncture points were used. The most commonly used proximal and distal acupuncture points were GB20 and GB39, respectively. In seven studies performing proximal acupressure,15, 16, 17, 18, 19, 20, 21 an average of 2.57 acupuncture points was used, while in seven studies performing distal acupressure,22, 23, 24, 25, 26, 27, 28 an average of 1.14 acupuncture points were used. Therefore, the number of acupuncture points used can be interpreted as being relatively smaller in studies performing distal acupressure. In fact, all but one study performing distal acupressure22, 23, 24, 26, 27, 28 used only one acupuncture point.
Acupuncture points on gallbladder meridian were most common, followed by acupuncture points on bladder meridian. In the EATM pathology, the areas where the nakchim occurs are mainly the posterior and lateral sides of the neck, so it can be interpreted that the acupuncture points on the meridians that pass through the affected area were used.
The CER in one study using both proximal and distal acupressure14 was 100%. The overall CER in seven studies using proximal acupressure15, 16, 17, 18, 19, 20, 21 was 95.65% (95% CI, 94.15–97.15), and four of these studies15, 16, 19, 20 yielded the overall ICR of 71.61% (95% CI, 64.51–78.71). The overall CER in seven studies using distal acupressure22, 23, 24, 25, 26, 27, 28 was 99.37% (95% CI, 98.49–100.24), and six of these studies22, 23, 24, 25, 27, 28 yielded the overall ICR of 69.08% (95% CI, 63.49–74.68). Although direct comparison was not possible, the proximal acupressure and distal acupressure did not overlap 95% CI in the overall CER, not like overall ICR. This suggests that there may be a possibility that the efficacy rate of distal acupressure is superior to that of proximal acupressure.
We analyzed eight studies performing simple acupressure technique using one acupuncture point.16, 18, 22, 23, 24, 26, 27, 28 In two studies performing simple proximal acupressure on SI11,16, 18 the overall CER was 96.00% (95% CI, 91.57–100.44), and one study16 yielded the ICR of 50.00% (95% CI, 32.11–67.89). In six studies performing simple distal acupressure,22, 23, 24, 26, 27, 28 GB39, BL57, and TE3 were used and the overall C.
ER was 99.32% (95% CI, 98.37–100.26). Five studies22, 23, 24, 27, 28 yielded the overall ICR of 70.17% (95% CI, 64.36–75.98). The CERs of SI11, GB39, BL57, and TE3 were 96.00% (95% CI, 91.57–100.44), 100%, 96.36% (95% CI, 91.42–101.31), and 100%, respectively. The ICRs of the acupuncture points were 50.00% (95% CI, 32.11–67.89), 64.23% (95% CI, 52.11–76.35), 100%, and 78.00% (95% CI, 57.45–98.55), respectively. However, in case of the ICR of BL57, the analyzed sample size was only 1. Therefore, the effect may be exaggerated. In this view, the most efficient simple acupressure on nackchim, which is the most effective and works fastest according to current evidences, may be the acupressure of TE3.
Dong-qi therapy is performed simultaneously with acupuncture or acupressure, and is used to increase the therapeutic effect. Twelve studies15, 16, 17, 18, 20, 22, 23, 24, 25, 26, 27, 28 used Dong-qi therapy and overall CER and ICR were 98.44% (95% CI, 95.37–101.51) and 70.84% (95% CI, 54.33–87.36), respectively. Three studies14, 19, 21 did not use Dong-qi therapy, and overall CER and ICR were 94.77% (95% CI, 86.50–103.04) and 64.00% (95% CI, 3.18–124.82), respectively. All the 95% CIs were overlapped, suggesting the possibility that the treatment effect may not change depending on the presence or absence of Dong-qi therapy.
Symptoms of nakchim include neck stiffness, but in general, the term nakchim refers to not only a stiff feeling but also a limited range of motion of the neck. A random population-based study of Australians reported that about 18% and 17% experienced waking cervical pain and waking cervical stiffness, respectively.29 Cervical stiffness does not include limitation in the range of motion of the joint, so the prevalence may be overestimated than that of nakchim.
Among the clinical studies included in this review, only three17, 21, 27 clearly described nakchim as rapid onset, neck pain with limited motion range, and no abnormalities in radiological examinations. Although nakchim has not been defined in modern medicine, with reference to the features of the previously described nakchim, the pathological condition can be defined as tissue damage and/or inflammation that is limited to the muscles, ligaments, or peripheral nerves of neck and shoulders without a history of trauma. If a patient visits with a morning stiff neck, or if an inpatient complains it one day, it is necessary to check for a history of the trauma at first. Additionally, it is necessary to distinguish red flags associated with neck stiffness: “If fatigue, diffuse joint pain, and abnormal laboratory test results are associated with the limited neck mobility, it may suggest rheumatoid arthritis; If it is accompanied by neuropathic symptoms such as sensory deficits or motor neuron signs, it may suggest spondyloarthropathy; If weight loss, anorexia, family or personal history of cancer are present, it may suggest metastasis; If fever and elevated white blood cell count are present, it may be indicative of infectious symptoms such as meningitis.”30
At this moment, clinicians will be able to use Cervicalgia (code M54.2) or Torticollis (code M43.6) as disease codes for nakchim patients in the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10). All these codes refer to simple symptoms; however, nakchim needs to be considered as a syndrome with pain and neck stiffness. These patients are common in the clinic, and often do not have clear external trauma, radiological abnormalities, or underlying diseases. In this case, a differential diagnosis could be used to make a diagnosis with nakchim. To do this, it is necessary to precede the creation of standards through expert consensus based on the existing inclusion criteria in clinical studies of nakchim patients and textbooks.4, 12
In the studies included in this review, it was common that acupressure effectively improved the symptoms of nakchim, and the therapeutic effect was immediately apparent. Acupressure applied to the distal acupuncture point was also effective. This is consistent with the results that both distal acupressure and proximal acupressure of the females with chronic neck pain showed significant pain relief.31 Recently, a RCT have also shown that acupressure is effective in improving acute ankle sprain injuries.32
The underlying mechanisms of acupressure are still unclear. However, there are some hypotheses that can explain the effect of acupressure on nakchim. First, proximal acupressure may have relieved local muscle tensions by physically massaging the affected muscle, and may have resulted in analgesic effects through Gate Control theory.33 Second, acupressure may have modulated sympathetic nervous system activity and hypothalamic–pituitary–adrenocortical axis to reduce the overproduction of cortisol, resulting in a systematic relaxation response, which can relax stiff neck and shoulder muscles.34, 35, 36 Third, acupressure, particularly proximal acupressure, may have induced analgesic effects by physically stimulating peripheral nerves with pathological problems.37 Fourth, acupressure may have induced analgesic effects through endogenous release of opioids.38 Fifth, cognitive shift in perception of pain may be caused by Dong-qi therapy performed with acupressure.39 Finally, acupressure may be involved in the recovery from disease by controlling the energy flow, so-called Qi, in the meridians.
EATM treatments for nakchim may include acupuncture, herbal medicine, and tuina.40, 41, 42 However, acupressure is not only a cost-effective, safe, and non-invasive treatment, but also a treatment that can be shared among caregivers, nurses, and doctors. Moreover, acupressure is a simple treatment that can be performed by patient himself/herself. In terms of public health, this potentially reduces medical costs, and patients can improve their confidence in own health.
In our knowledge, this is the first systematic review assessing the effects of acupressure on nakchim. Especially, this review separately analyzed simple acupressure using one acupuncture point, and these results can be applied to clinical practice, patient education, and study design.
However, this study has the following limitations. Because all of the included studies are case report or case series, the evidence level of the results is considered to be very low. Additionally, the methodological quality of the included studies was generally poor, which can affect the reliability of the results. Moreover, among the included studies, standardized assessment tools such as VAS, NRS, and NDI were not used. The fact that specific definition and golden diagnostic criteria of nakchim are not established yet may be an obstacle to future research, though there is an existing RCT of nakchim.4
Therefore, in future studies, definition and diagnostic criteria of nakchim should be established through expert consensus, and acupressure should be considered as a main intervention, considering its clinical and cost effectiveness. In order to find the optimal therapeutic effect, it is also necessary to compare the therapeutic effect by using different acupuncture points for each affected area according to EATM theory. Additional well-designed, placebo-controlled studies using standardized acupressure methods should be performed to confirm the effects of acupressure on nakchim.
Conflicts of interest
The authors declare no conflict of interest.
References
- 1.Korean Acupuncture, Moxibustion Medicine Society . Hanmi Medicinal Publishing Co.; Seoul: 2016. Acupuncture medicine; pp. 485–488. [Google Scholar]
- 2.World Health Organization . Word Health Organization; 2007. WHO international standard terminologies on traditional medicine in the western pacific region. Available at: http://www.wpro.who.int/publications/who_istrm_file.pdf?ua=1. [Google Scholar]
- 3.Song I., Lee G.M., Hong K.E. Research on oriental medicine diagnosis and classification system by using neck pain questionnaire. Acupuncture. 2011;28:85–100. [Google Scholar]
- 4.Lee K.H., Youn H.M., Ko W.S., Song C.H., Jang K.J., Ahn C.B. Comparison of treatment effects and allergic responses to stiff neck between sweet bee venom and bee venom pharmacopuncture. J Pharmacopunct. 2008;11:39–48. [Google Scholar]
- 5.Lee E.J., Frazier S.K. The efficacy of acupressure for symptom management: a systematic review. J Pain Symptom Manage. 2011;42:589–603. doi: 10.1016/j.jpainsymman.2011.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Song H.J., Seo H.J., Lee H., Son H., Choi S.M., Lee S. Effect of self-acupressure for symptom management: a systematic review. Complem Ther Med. 2015;23:68–78. doi: 10.1016/j.ctim.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 7.Yue S., Jiang X., Wong T. Effects of a nurse-led acupressure programme for stroke patients in China. J Clin Nurs. 2013;22:1182–1188. doi: 10.1111/j.1365-2702.2012.04127.x. [DOI] [PubMed] [Google Scholar]
- 8.Tiwari A., Lao L., Wang A.X., Cheung D.S., So M.K., Yu D.S. Self-administered acupressure for symptom management among Chinese family caregivers with caregiver stress: a randomized, wait-list controlled trial. BMC Complem Altern Med. 2016;16:424. doi: 10.1186/s12906-016-1409-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gillick M.R. The critical role of caregivers in achieving patient-centered care. JAMA. 2013;310:575–576. doi: 10.1001/jama.2013.7310. [DOI] [PubMed] [Google Scholar]
- 10.Salmond S.W., Echevarria M. Healthcare transformation and changing roles for nursing. Orthop Nurs. 2017;36:12–25. doi: 10.1097/NOR.0000000000000308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 12.State Administration of Traditional Chinese Medicine . Nanjing University Press; Nanjing: 1994. Criteria of diagnosis and therapeutic effects of diseases and syndromes in traditional Chinese medicine; p. 65. [Google Scholar]
- 13.National Institutes of Health Quality assessment tool for case series studies. NIH website. https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/case_series. Published 2014. Accessed September 8, 2017.
- 14.Hu L.C. Clinical realization in points massage treatment of Luozhen disease. Natural Sci J Hainan Teachers Coll. 1999;12:113–115. [Google Scholar]
- 15.Wei J.C. Clinical observation of 39 cases of Nakchim treated by acupuncture point massage. Chin Manipul Qi Gong Ther. 1999;15:25. [Google Scholar]
- 16.Wang L. Acupressure in Tianzong points in 30 cases of Nakchim. Fujian J TCM. 2001;32:27. [Google Scholar]
- 17.Xiang Y.C., Liu J.P., Guo J.G., Zhang P. Acupressure in Xuanli points in 112 cases of Nakchim. People's Milit Surg. 2003;46:618. [Google Scholar]
- 18.Huang J.B. Acupressure in Tianzong points in 45 cases of Nakchim. Chin Manipul Qi Gong Ther. 2003;19:25. [Google Scholar]
- 19.Lu D.C. Acupressure in Quepen, Tianding points in treatment of Nakchim, frozen shoulder. J Guangxi Commer Coll. 2004;21:115–116. [Google Scholar]
- 20.Wang X.M. Efficacy observation in 36 cases of Nakchim treated with hand acupuncture point massage therapy. Mod J Integr Tradit Chin West Med. 2014;13:232. [Google Scholar]
- 21.Li K.F. Manipulation of acupuncture-based treatment in 400 cases of Nakchim. Nei Mongol J Tradit Chin Med. 2014;12:91. [Google Scholar]
- 22.Zhang P. Massage treatment of Nakchim. Jiangsu J Tradit Chin Med. 1961;1:41. [Google Scholar]
- 23.Li A.Y., Zhang S.Y. Acupressure in Chengshan points in treatment of Nakchim. J New Chin Med. 1984;6:33. [Google Scholar]
- 24.Zhang J.G., Wang W.C. Acupressure in Zhongzhu points in treatment of Nakchim. J Sichuan Trad Chin Med. 1988;11:59. [Google Scholar]
- 25.Mao W.Y. Acupressure in Xuanzhong and Luozhen points in treatment of Nakchim. Milit Med J South China. 1989;1:91–92. [Google Scholar]
- 26.Liang Z.S. Acupressure in Chengshan points in treatment of Nakchim. J Agric. 1999;1:42. [Google Scholar]
- 27.Li K. Acupressure in Xuanzhong points in treatment of 136 cases of Nakchim. Med J Natl Defend Forces Southwest China. 2007;1:36. [Google Scholar]
- 28.Liu H.F. Acupressure in Zhongzhu points in treatment of 80 cases of Nakchim. Zhejiang J Trad Chin Med. 2012;1:23. [Google Scholar]
- 29.Gordon S.J., Trott P., Grimmer K.A. Waking cervical pain and stiffness, headache, scapular or arm pain: gender and age effects. Aust J Physiother. 2002;48:9–15. doi: 10.1016/s0004-9514(14)60277-4. [DOI] [PubMed] [Google Scholar]
- 30.Cohen S.P. Epidemiology, diagnosis, and treatment of neck pain. Mayo Clin Proc. 2015;90:284–299. doi: 10.1016/j.mayocp.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 31.Matsubara T., Arai Y.C., Shiro Y., Shimo K., Nishihara M., Sato J. Comparative effects of acupressure at local and distal acupuncture points on pain conditions and autonomic function in females with chronic neck pain. Evid Based Complem Alternat Med 2011. 2011 doi: 10.1155/2011/543291. pii:543291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhao M., Gao W., Zhang L., Huang W., Zheng S., Wang G. Acupressure therapy for acute ankle sprains: a randomized clinical trial. PM&R. 2017:1–9. doi: 10.1016/j.pmrj.2017.06.009. [DOI] [PubMed] [Google Scholar]
- 33.Melzak R., Wall P. Pain mechanism: a new theory. Sciences. 1965;150:971–979. doi: 10.1126/science.150.3699.971. [DOI] [PubMed] [Google Scholar]
- 34.Arai Y.C., Ushida T., Osuga T., Matsubara T., Oshima K., Kawaguchi K. The effect of acupressure at the extra 1 point on subjective and autonomic responses to needle insertion. Anesth Analg. 2008;107:661–664. doi: 10.1213/ane.0b013e31817b8495. [DOI] [PubMed] [Google Scholar]
- 35.Remington T. Calming music and hand massage with agitated elderly. Nurs Res. 2002;51:317–323. doi: 10.1097/00006199-200209000-00008. [DOI] [PubMed] [Google Scholar]
- 36.McFadden K.L., Hernández T.D. Cardiovascular benefits of acupressure (Jin Shin) following stroke. Complem Ther Med. 2010;18:42–48. doi: 10.1016/j.ctim.2010.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang W., Tan W., Luo D., Lin J., Yu Y., Wang Q. Acute pressure on the sciatic nerve results in rapid inhibition of the wide dynamic range neuronal response. BMC Neurosci. 2012;13:147. doi: 10.1186/1471-2202-13-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Trentini J.F., Thompson B., Erlichman J.S. The antinociceptive effect of acupressure in rats. Am J Chin Med. 2005;33:143–150. doi: 10.1142/S0192415X05002746. [DOI] [PubMed] [Google Scholar]
- 39.Shin J.S., Ha I.H., Lee J., Choi Y., Kim M.R., Park B.Y. Effects of motion style acupuncture treatment in acute low back pain patients with severe disability: a multicenter, randomized, controlled, comparative effectiveness trial. Pain. 2013;154:1030–1037. doi: 10.1016/j.pain.2013.03.013. [DOI] [PubMed] [Google Scholar]
- 40.Yu X., Li H.B., Wen S.Y. Progress of clinical research on acupuncture treatment of stiff neck. J Liaoning Univ TCM. 2013;15:270–272. [Google Scholar]
- 41.Ou L., Zeng X.H., Zhao P. Observation on the therapeutic effect of Mahuangjiazhutang combined with cupping in treatment of Nakchim. J Pract Tradit Chin Med. 2009;25:790–791. [Google Scholar]
- 42.Chen W., Wu Y.C. The clinical evaluation of manuipulation with fumigation on stiff neck. Chin J Trad Med Traum Orthop. 2009;17:16–17. [Google Scholar]