To the Editor—There is substantial overlap in symptoms, including fatigue, muscle and joint pain, and cognitive and memory deficits, between post-treatment Lyme disease syndrome (PTLDS) and myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) [1]. Increasing evidence suggests a role for immunologic and inflammatory pathways in both PTLDS and ME/CFS [2–4]. However, in part owing to their etiologic complexity and the lack of established biomarkers, our understanding of the pathways involved and potential mechanistic differences between the 2 conditions is very limited.
In a 2016 study published in Clinical Infectious Diseases, Uhde et al [5] examined the concentrations of acute-phase response proteins, including C-reactive protein (CRP), in individuals with PTLDS. CRP is a highly sensitive marker of infection and inflammation that binds a variety of ligands present on the surface of pathogens or exposed during autologous cell stress or death, exerting its effect through opsonin deposition and activation of the complement pathway, in addition to direct interaction with phagocytic cells [6]. We found that the circulating levels of CRP, as well as the frequency of concentrations >3 mg/mL (generally considered to represent some degree of inflammation [7]) to be significantly higher in the PTLDS cohort than in a control group of subjects who had a history of Lyme disease but without persistent symptoms (both P < .001). The data provided evidence for increased expression of an objective marker of inflammation in PTLDS but suggested a mechanism of activation distinct from that in active infection, as previously discussed [5].
Using the same methods [5] in a new study, we screened plasma samples from 131 patients with ME/CFS (89 female; mean age [standard deviation], 50.0 [11.4] years; mean body mass index (BMI), 26.0 [5.5]) and 86 healthy controls (68 female; mean age, 50.0 [12.8] years; mean BMI, 26.5 [6.8]), provided by the SolveCFS BioBank [8]. Patients with ME/CFS met the criteria of Fukuda et al [9] and the Canadian criteria [10] for this condition [9, 10]. Screening questionnaires were used to evaluate the general health of the unaffected controls and to confirm that they did not meet ME/CFS case definition criteria. The ME/CFS and control sample sizes provided >95% power, with an α value <.05, to detect the same increase in CRP response as in the patients with PTLDS [5]. Group differences were assessed by the analysis of covariance, using the general linear model, to account for the potential confounding effect of age, sex, and BMI. This study was approved by the Institutional Review Board of Columbia University. In contrast to data from patients with PTLDS [5], we did not find a statistically significant difference in the circulating levels of CRP (Figure 1) or the frequency of CRP levels >3 mg/L (33 of 131 [25.2%] vs 22 of 86 [25.6%], respectively) between patients with ME/CFS and controls.
Figure 1.
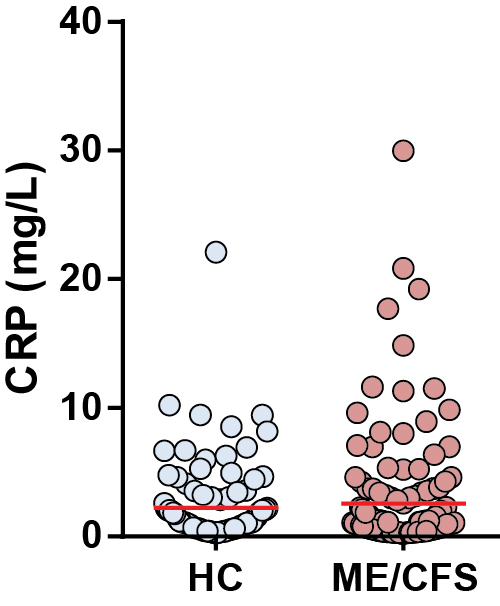
C-reactive protein (CRP) concentrations in the cohorts of patients with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and healthy controls (HCs). The difference between the 2 groups was not statistically significant (P = .55). Horizontal red bars represent the mean for each group.
These data provide evidence for the likely existence of distinct inflammatory mechanisms in ME/CFS versus PTLDS, which may be driven in part by the potentially more heterogeneous etiology of ME/CFS symptoms in comparison with PTLDS. The absence of a significantly enhanced CRP response in ME/CFS, despite published data suggesting activation of various inflammatory pathways, warrants further examination.
Notes
Disclaimer. The funding organizations had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Financial support. This work was supported by the National Institute of Allergy and Infectious Diseases, National Institutes of Health (grant R21AI121996 to A. A.) and the Global Lyme Alliance (A. A.).
Potential conflicts of interest. G. P. W. reports receiving research grants from Immunetics, the Institute for Systems Biology, Rarecyte, and Quidel Corporation. He owns equity in Abbott/AbbVie, has been an expert witness in malpractice cases involving Lyme disease and babesiosis, and is an unpaid board member of the American Lyme Disease Foundation. A. R. M. is a coinventor on a US patent using the Luciferase Immunoprecipitation Systems assay for profiling antibody responses to a panel of Borrelia burgdorferi proteins. A. A. reports receiving grants from the National Institutes of Health, the Global Lyme Alliance, and the Solve ME/CFS Initiative for research related to ME/CFS and Lyme disease. All other authors report no potential conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Gaudino EA, Coyle PK, Krupp LB. Post-Lyme syndrome and chronic fatigue syndrome: neuropsychiatric similarities and differences. Arch Neurol 1997; 54:1372–6. [DOI] [PubMed] [Google Scholar]
- 2. Lorusso L, Mikhaylova SV, Capelli E, Ferrari D, Ngonga GK, Ricevuti G. Immunological aspects of chronic fatigue syndrome. Autoimmun Rev 2009; 8:287–91. [DOI] [PubMed] [Google Scholar]
- 3. Jacek E, Fallon BA, Chandra A, Crow MK, Wormser GP, Alaedini A. Increased IFNα activity and differential antibody response in patients with a history of Lyme disease and persistent cognitive deficits. J Neuroimmunol 2013; 255:85–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Strle K, Stupica D, Drouin EE, Steere AC, Strle F. Elevated levels of IL-23 in a subset of patients with post–Lyme disease symptoms following erythema migrans. Clin Infect Dis 2014; 58:372–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Uhde M, Ajamian M, Li X, Wormser GP, Marques A, Alaedini A. Expression of C-reactive protein and serum amyloid A in early to late manifestations of Lyme disease. Clin Infect Dis 2016; 63:1399–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pepys MB, Hirschfield GM. C-reactive protein: a critical update. J Clin Invest 2003; 111:1805–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kushner I, Rzewnicki D, Samols D. What does minor elevation of C-reactive protein signify?Am J Med 2006; 119:166 e17–28. [DOI] [PubMed] [Google Scholar]
- 8. Irlbeck DM, Vernon SD, McCleary KK, et al. No association found between the detection of either xenotropic murine leukemia virus-related virus or polytropic murine leukemia virus and chronic fatigue syndrome in a blinded, multi-site, prospective study by the establishment and use of the SolveCFS BioBank. BMC Res Notes 2014; 7:461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A. The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group. Ann Intern Med 1994; 121:953–9. [DOI] [PubMed] [Google Scholar]
- 10. Carruthers BM. Definitions and aetiology of myalgic encephalomyelitis: how the Canadian consensus clinical definition of myalgic encephalomyelitis works. J Clin Pathol 2007; 60:117–9. [DOI] [PMC free article] [PubMed] [Google Scholar]


