Abstract
Epipericardial fat necrosis (EPFN) is a rare cause for acute chest. We describe the case of a previously healthy 25-year-old man who presented with sudden onset of left-sided chest pain. Laboratory values showed only mildly elevated d-dimer and electrocardiogram was normal. However, subsequent CT angiogram of the chest revealed fat necrosis in the epipericardial fat, characteristic for EPFN, for which the patient was treated with nonsteroidal anti-inflammatory drug. This case highlights the importance of radiologists to consider the prospect of EPFN in the differential diagnosis of acute chest pain as correct diagnosis allows for conservative management and avoidance of more aggressive techniques in symptomatic patients.
Keywords: Epipericardial fat necrosis, Chest pain, Dyspnea
Introduction
Fat necrosis in systemic adipose tissue can occur at various sites, commonly in the subcutaneous fat and breast following trauma, peripancreatic fat in pancreatitis, and in epiploic appendagitis. Less frequently, however, it may occur within the epipericardial fat. First described by Jackson, Clagett and McDonald in 1957, epipericardial fat necrosis (EPFN) is an uncommon benign condition but known cause for acute chest pain in an otherwise healthy person [1]. The exact prevalence of the disease is unknown as it is believed to often be unrecognized and misdiagnosed. A literature search of PubMed database with keywords “epipericardial fat necrosis” identified 45 reported cases with only 7 articles in the radiology literature.
Case
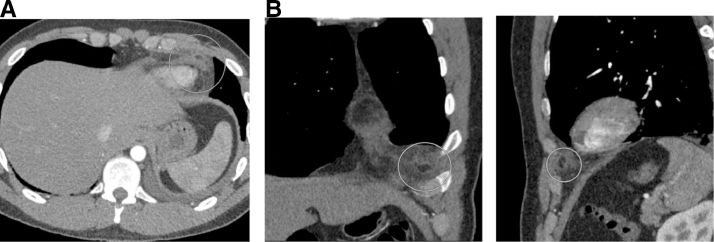
A 25-year-old man with no significant past medical history presented to the Emergency Department with 1-week intermittent left-sided, parasternal chest pain, which was nonradiating but worsened with sudden movements. He works as a consultant and travels frequently. Patient denied shortness of breath, leg pain and/or swelling, and recent hospitalization. On physical examination, the patient occasionally winced when he moved a certain way and pointed to the center of his chest. Electrocardiogram showed normal sinus rhythm. A complete metabolic panel revealed no significant abnormalities, however, d-dimer was mildly elevated. Chest radiograph (Fig. 1) and CT angiogram (Fig. 2) were obtained. The chest radiograph was unremarkable; however, the CT angiogram showed a characteristic well-encapsulated 1.3 cm fat containing lesion with adjacent fat stranding in the epipericardial fat. There were no findings suggestive for acute pulmonary embolism or pericarditis on the CTA or chest radiograph. Based on the patient's clinical history and radiologic findings, the patient was diagnosed with EPFN. He was subsequently treated and discharged with nonsteroidal anti-inflammatory drug from the Emergency Department and on the 4 week follow-up, was reported symptom free.
Fig. 1.
Posteroanterior chest radiograph showed no acute cardiopulmonary or osseous abnormality. The lungs are clear and the cardiomediastinal silhouette is within normal limits.
Fig. 2.
(A) CTA scan of the chest showed a lesion with a fat attenuation coefficient surrounded by a capsule of higher density in the epipericardial fat (circle) adjacent to the left ventricular apex. (B) Coronal and sagittal views of the oval encapsulated lesion in the left epipericardial fat (circles) are suggestive of fat necrosis.
Discussion
The pathophysiology of necrosis of the epipericardial fat is poorly understood and currently under debate. Review of EPFN case reports showed no apparent gender or age predilection. However, it has been suggested to be more common in obese individuals with a large amount of epicardial or pericardial fat tissue [2]. Additional likely predisposing factors include pre-existing structural abnormality making adipose tissue vulnerable to trauma and acute torsion of a vascular pedicle of adipose tissue triggering fat necrosis. It has also been proposed that increased capillary pressure during Valsalva maneuver may cause microvascular bleed into the adipose tissue initiating hemorrhagic fat necrosis [3].
Similar to epiploic appendagitis which presents as self-limited localized abdominal pain, the most common presentation of EPFN is acute pleuritic chest pain [4]. It is more commonly described on the left side and is self-limiting usually lasting only a few days. However, it sometimes will recur for several weeks with intermittent episodes [5]. Other associated symptoms include dyspnea, syncope, dizziness, tachycardia, and diaphoresis. Physical examination is generally unremarkable, although pericardial friction rub may occasionally be heard if there is coexisting pericarditis. Laboratory findings including cardiac enzymes typically show no abnormalities, and electrocardiogram is characteristically normal [6].
EPFN may be clinically mistaken for other severe etiologies of pleuritic chest pain and dyspnea, most notably acute myocardial infarction and pulmonary thromboembolism [7]. However, laboratory values and electrocardiogram in EPFN are usually normal in an otherwise healthy patient, which can help guide clinicians to the correct diagnosis in the appropriate clinical setting. In addition, imaging tests are essential to elucidate the diagnosis. Chest radiographs are often normal during the first few days but usually will progress revealing an ill-defined round mass overlying the ipsilateral cardiophrenic angle on the same side of the chest pain. CT can further provide characterization of the nonspecific paracardiac mass such as exact location and density measurements to determine if the mass contains fat. The typical CT findings for EPFN are an encapsulated, round fat-containing lesion with adjacent fat stranding occurring within epicardial or pericardial fat. There may sometimes be associated pericardial thickening and ipsilateral pleural effusion as well [2], [8].
The unique clinicoradiologic findings coupled with CT's ability to demonstrate fat density within the chest mass should allow physicians to diagnose EPFN once other causes of acute chest pain has been ruled out. However, when diagnostic question remains, the definitive diagnosis is attained by histopathological analysis from surgical resection. This has fallen in disuse because of the high accuracy of radiologic characteristics and benign self-limiting nature of the condition [7]. When performed, however, the pathologic features closely resemble epiploic appendagitis with a central focus of necrotic adipose cells encompassed by macrophages and neutrophils. Specimens obtained later in the clinical course will show fibrosis as the lesion has resolved into a scar tissue [3], [9].
It is important for clinicians to be familiar of this disease process in order to manage it properly in the acute clinical setting. Due to the benign, self-limited nature, nonsteroidal anti-inflammatory drugs is indicated with surgical resection rarely performed for indeterminate cases [7]. Clinical follow-up and chest CT in 4 weeks may also be recommended to document resolution of symptoms and radiographic findings [5].
Conclusion
Although EPFN is an uncommon condition, radiologists need to be aware of its characteristics because the imaging and clinical features often lead to its diagnosis, preventing otherwise more aggressive testing. The difficulty in attaining the diagnosis lies in the nonspecific presenting symptom as well as unremarkable laboratory values and normal electrocardiogram. Definitive diagnosis is obtained by histopathological analysis, however, EPFN has been increasingly diagnosed by radiologic findings associated with suggestive clinical context, for which conservative management is recommended.
Consent
Informed consent was obtained from the patient.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: Neither I nor my co-authors received grant funding or financial support during the creation of the work. We have no financial relationship with a commercial organization that may have a direct or indirect interest in the content.
Contributor Information
Don N. Nguyen, Email: don.nguyen@ahn.org.
Cassie D. Tran, Email: cassie.tran@ahn.org.
Scott M. Rudkin, Email: scott.rudkin@ahn.org.
Jeffrey S. Mueller, Email: jeffrey.mueller@ahn.org.
Matthew S. Hartman, Email: matthew.hartman@ahn.org.
References
- 1.Fred HL. Pericardial fat necrosis: a review and update. Texas Heart Inst J. 2010;37(1):82–84. [PMC free article] [PubMed] [Google Scholar]
- 2.Pineda V, Cáceres J, Andreu J, Vilar J, Domingo ML. Epipericardial fat necrosis: radiologic diagnosis and follow-up. AJR. 2005;185(5):1234–1236. doi: 10.2214/AJR.04.1310. [DOI] [PubMed] [Google Scholar]
- 3.Giassi de S K, Costa AN, Apanavicius A, Bachion GH, Musolino RS, Kairalla RA. Epipericardial fat necrosis: an unusual cause of chest pain. J Bras Pneumol. 2013;39(5):627–629. doi: 10.1590/S1806-37132013000500014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Runge T, Greganti MA. Epipericardial fat necrosis–a rare cause of pleuritic chest pain: case report and review of the literature. Arch Med Sci. 2011;7(2):337–341. doi: 10.5114/aoms.2011.22088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lacasse MC, Prenovault J, Lavoie A, Chartrand-Lefebvre C. Pericardial fat necrosis presenting as acute pleuritic chest pain. J Emerg Med. 2013;44(2):e269–e271. doi: 10.1016/j.jemermed.2012.05.032. [DOI] [PubMed] [Google Scholar]
- 6.Baig A, Campbell B, Russell M, Singh J, Borra S. Epipericardial fat necrosis: an uncommon etiology of chest pain. Cardiol J. 2012;19(4):424–428. doi: 10.5603/cj.2012.0076. [DOI] [PubMed] [Google Scholar]
- 7.Carvalho N, Silva N, Pereira P, Morganti A, Silva S, Rodrigues A. Epipericardial fat necrosis. An important differential diagnosis of chest pain. Int J Cardiovasc Sci. 2017 [Google Scholar]
- 8.van den Heuvel DAF, van Es HW, Cirkel GA, Bos WJ. Acute chest pain caused by pericardial fat necrosis. Thorax. 2010;65:188. doi: 10.1136/thx.2009.114637. [DOI] [PubMed] [Google Scholar]
- 9.Lee BY, Song KS. Calcified chronic pericardial fat necrosis in localized lipomatosis of pericardium. AJR. 2007;188(1):W21–W24. doi: 10.2214/AJR.04.1989. [DOI] [PubMed] [Google Scholar]