Introduction
Adrenal cysts and pseudocysts are a rare condition usually incidentally diagnosed by imaging methods. An “adrenal pseudocyst” is the term given to no tumoral, no parasitic cyst of the adrenal gland in which an epithelial or endothelial lining is not demonstrated. The incidence of adrenal hemorrhagic pseudocyst is very low. Less than 100 hemorrhagic pseudocysts have been reported. The diagnosis of hemorrhagic adrenal pseudocyst should be made with caution on imaging alone. It is important to distinguish adrenal malignancy from non-tumoral hemorrhage. We present a case of a giant hemorrhagic adrenal pseudocyst mimicking hydatid cyst and we discuss the clinical radiological and histopathological features.
Case
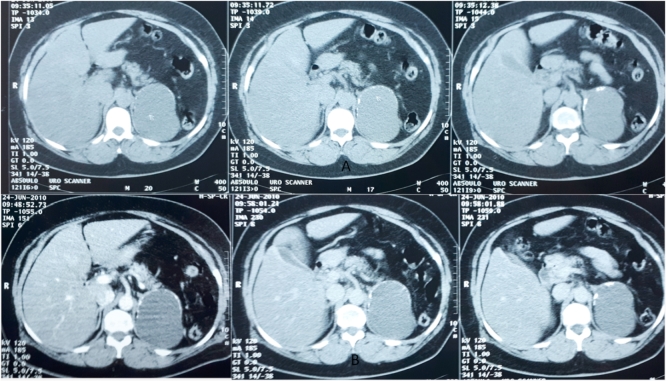
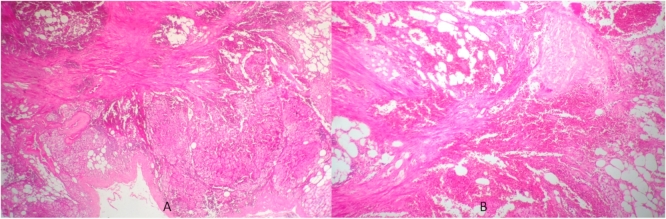
A 51-year-old woman with history of hypertension presented with a 1-year history of abdominal pain. The clinical examination didn't reveal a palpable abdominal mass or tenderness on palpation. The ultrasonographic examination of the abdominal mass showed a giant cystic mass over the left suprarenal region with internal echoes noted within the cyst. Enhanced computed tomography (CT) of the abdomen showed a well-defined lesion of the left adrenal gland with calcifications and necrotic components measuring 8 × 7 cm in the anterior-posterior and transverse diameters, with compression of the spleen, left diaphragm, and upper pole of the left kidney (Fig. 1A and B). Serum and urinary catecholamines and metanephrines were normal. Aldosterone and cortisol were also within normal limits. Based on the imaging findings and the fact that Tunisia is a country of endemic Echinococcus pathology the adrenal lesion was suspected to be a hydatid cyst despite that serology was negative. The patient underwent a left subcostal laparotomy. We carefully detached the mass from the kidney, the spleen, the left hemidiaphragm and posterior lumbar wall. We identified the left adrenal vein, which we tied and cut, and were able to remove the mass and the adrenal gland en bloc. The remaining postoperative course was uneventful and the patient was discharged home 4 days after the surgery in a good condition. The histopathological report indicated a left adrenal gland with a unilocular cystic lesion with a fibrous capsule containing amorphous eosinophilic material with calcifications and cholesterol crystals on microscopic examination (Fig. 2A and B). There was no evidence of malignancy. The final diagnosis was an adrenal hemorrhagic pseudocyst. The patient showed no recurrence during a follow-up of 5 years.
Fig. 1.
A and B: Contrast enhanced CT scan in the axial plane showing soft tissue enhancing mass with multiple calcifications.
Fig. 2.
A: Histological examination showing a fibrous hyalinized capsule containing clotted blood, residual adrenocortical tissue, and thin-walled vessels without identifiable cystic membranes. (Hematoxylin-Eosin, x 10).
B: Histological examination showing a fibrous capsule containing amorphous eosinophilic material with calcifications and cholesterol crystals. (Hematoxylin-Eosin, x 20).
Discussion
Adrenal gland cysts are uncommon entities and 4 pathological subtypes have been described: cystic degeneration of adrenal neoplasms, true cysts, pseudocysts and infectious cysts.1
Most of these cystic lesions are clinically silent and are therefore often diagnosed incidentally. Large cysts generally present as nonspecific abdominal pain. Since up to 7% of adrenal cysts are malignant, a careful preoperative hormonal and morphofunctional evaluation is mandatory.2 Malignancy may be suspected in the presence of symptoms caused by functioning neoplasms such as Cushing's syndrome, hyperadrenalism, hirsutism in women, and hypertension.2
On CT scan, adrenal pseudocysts typically appear as well-demarcated uni- or multilocular cystic lesions with the density of fluid, but unlike simple cysts can contain solid components, including septa, blood, and calcifications.3 The differential diagnosis of adrenal pseudocysts includes epithelial cysts, endothelial cysts, and parasitic cysts.3 The definitive preoperative diagnosis of adrenal pseudocyst can be difficult to make when there is acute intracystic hemorrhage, as in the present case, as this results in contrast enhancement on imaging. Certain features raise the suspicion of malignancy within a cystic adrenal lesion, including a heterogeneous appearance on imaging and the presence of necrosis in the center of the mass accompanied by calcification, and the size of the adrenal mass.3 In our case we suspect a hydatid cyst of adrenal gland.
Surgical excision is indicated in the presence of symptoms, suspicion of malignancy, an increase in size and detection of a functioning adrenal cyst.4
Laparoscopic treatment is indicated for small tumors. Cysts larger than 6 cm should be approached using an open procedure because of concerns about potential malignancy.4
Histopathology of the excised specimen gives confirmatory diagnosis showing unique microscopic features, as they are composed of a fibrous hyalinized capsule containing clotted blood, residual adrenocortical tissue, and thin-walled vessels without identifiable cystic membranes. This lack of epithelial layer characterizes it as a pseudocyst.5 The actual etiology of adrenal pseudocysts is unknown and hypotheses include the cystic degeneration of an adrenal neoplasm, ectasia of preexisting vessels, cystic degeneration of hematomas, or malformation of adrenal veins or intra-adrenal hemorrhage caused by trauma.5 Another theory holds that the degeneration of a true cyst that has lost its cellular lining due to inflammation or bleeding inside the cyst can lead to a pseudocyst.5
Conclusion
A hemorrhagic adrenal pseudocyst is an uncommon clinical finding. In most cases of hemorrhagic adrenal pseudocysts, no identifiable cause of hemorrhage can be determined. Clinical and radiological features of the tumor are nonspecific and histopathological examination is essential to establish definitive diagnosis.
Conflicts of interest
None for all authors.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Diolombi Mairo L., Khani Francesca, Epstein Jonathan I. Diagnostic dilemmas in enlarged and diffusely hemorrhagic adrenal glands. Hum Pathol. 2016 doi: 10.1016/j.humpath.2016.02.017. [DOI] [PubMed] [Google Scholar]
- 2.Simon D.R., Palese M.A. Clinical update on the management of adrenal hemorrhage. Curr Urol Rep. 2009;10(1):78–83. doi: 10.1007/s11934-009-0014-y. [DOI] [PubMed] [Google Scholar]
- 3.Yip L., Tublin M.E., Falcone J.A. The adrenal mass: correlation of histopathology with imaging. Ann Surg Oncol. 2010;17:846–852. doi: 10.1245/s10434-009-0829-2. [DOI] [PubMed] [Google Scholar]
- 4.Amarillo H.A., Bruzoni M., Loto M., Castagneto G.H., Mihura M.E. Hemorrhagic adrenal pseudocyst: laparoscopic treatment. Surg Endosc. 2004;18:1539. doi: 10.1007/s00464-003-4547-8. [DOI] [PubMed] [Google Scholar]
- 5.Medeiros L.J., Lewandrowski K.B., Vickery A.L. Adrenal pseudocyst: a clinical and pathological study of eight cases. Hum Pathol. 1989;20:660–665. doi: 10.1016/0046-8177(89)90153-6. [DOI] [PubMed] [Google Scholar]