Abstract
Background:
Biodentine is comparatively a new biomaterial claimed to have properties comparable to mineral trioxide aggregate (MTA). Biodentine and MTA are effectively used for direct pulp capping (DPC), and they are capable of regenerating relatively damaged pulp and formation of hard dentine bridge.
Objectives:
The aim of this systematic review was to test the null hypothesis of no difference between Biodentine and MTA as DPC materials for human permanent mature teeth, against the alternative hypothesis of a difference.
Data Sources:
Clinical trials were identified by electronic databases searches of Midline, CENTRAL Cochrane Library, Latin American and Caribbean Health Sciences Literature, Scopus, Scientific Electronic Library Online, evidence-based endodontics literature, KoreaMed, and Google Scholar. The literature search was performed from January 2010 to February 2018. Hand searches were also performed for relevant abstracts, books, and reference lists. Titles and abstracts of studies identified using the above-described protocol were independently screened by two authors. Full texts of studies judged by title and abstracts to be relevant were independently evaluated by two authors for stated eligibility criteria.
Study Eligibility Criteria:
The eligibility criteria included randomized clinical trials (RCTs) and non-RCTs.
Participants:
Patients with permanent mature molars indicated for surgical extraction or molars that have symptomless exposure of vital pulp tissue by caries or trauma. In both cases, the molars were subjected to DPC.
Interventions:
The pulp exposures were directly treated by Biodentine or MTA.
Study Appraisal:
To assess article quality, two authors independently used the risk of bias in nonrandomized studies – of interventions.
Methods:
Qualitative metasynthesis was used to analyze data across qualitative studies.
Results:
The initial search identified 8725 unique references through the search process. No additional studies were identified through handsearching. After filtering, 915 references were recorded and screened. After the eligibility criteria were applied, seven unduplicated prospective and retrospective cohort studies were included in the qualitative metasynthesis.
Limitations:
Further RCTs with much larger sample size and proper methodology with longer observational time are still in need to adequately address the questions of the present systematic review.
Conclusion and Implications of Key Findings:
Within the limitations of this review, it may be concluded that Biodentine had a similar effect on dentin bridge formation likely to MTA. However, this conclusion is based on only very few well-conducted prospective and retrospective cohort studies.
Systematic Review Registration Number:
The review had been registered with PROSPERO (registration number CRD42018089302).
Keywords: Biodentine, dentin bridge formation, direct pulp capping, mineral trioxide aggregate, permanent molars
INTRODUCTION
Pulp exposure can be due to trauma, mechanical reasons, or caries. Direct pulp capping (DPC) may be required as one of the treatment options to prevent the dental pulp from necrosis.[1] Ideal pulp capping material should maintain pulpal vitality and stimulate reparative dentin formation.[2] These materials should possess certain properties such as radiopacity, insolubility, dimensional stability, biocompatibility, bioactivity, and adequate adhesive ability to both the dentin and to the restorative materials.[3] It should also release fluoride, provide bacterial seal, prevent secondary caries, should have bactericidal or bacteriostatic activity against the causative pathogens, and promote the formation of mineralized tissue.[4]
Till date, calcium hydroxide (CH), mineral trioxide aggregate (MTA), and tricalcium silicate cement (Biodentine) are the materials of choice which have been most commonly used in clinics.[5] Although CH has been considered as the gold standard for pulp capping, it still has several drawbacks, namely, insufficient adherence to dentin, multiple tunnel defects in the dentin bridges, and dissolution over time.[6] The two main components of MTA are calcium oxide and silicon dioxide. When these raw materials are blended, they produce tricalcium silicate, dicalcium silicate, tricalcium aluminate, tetracalcium aluminoferrite, and other mineral oxides. Bismuth oxide was added so that the material can be detected on radiographs. On addition of water, the cement hydrates, form silicate hydrate gel.[7] Gray MTA was the original formulation to be introduced, and white MTA was developed later as this version improved esthetics.[8]
Disadvantages of MTA are that it is highly soluble and has a prolonged setting more than 2 h.[9] Meanwhile, Biodentine is a two components material; the powder component consists of tricalcium silicate, dicalcium silicate as a second core material, calcium carbonate, oxide as filler, iron oxide shade, and zirconium oxide as a radioopacifier. The liquid, on the other hand, contains calcium chloride as a setting accelerator and a water reducing agent.[10] There is ample evidence for positive effects of Biodentine on vital pulp cells, for stimulating tertiary dentin formation, and early formation of reparative dentin.[11]
The gold standard of experimental design is the randomized clinical trials (RCTs), in which participants are divided by chance into separate groups.[12] The British physician Archie Cochrane contributed greatly to the development of epidemiology as a science, and he was concerned about the efficacy of health care. Cochrane emphasized the necessity of performing strict systematic review with high scientific evidence from well-designed and well-conducted RCTs of medical studies to acquire a true and reliable conclusion.[13] The Oxford Centre for Evidence-based Medicine considers systematic reviews of RCTs as Level 1 according to the levels of evidence (LoE) corresponding to study design.[14]
The rationale for conducting this systematic review arose from the fact that a reliable biomaterial for DPC may be considered as an alternative to pulpectomy, especially if the pulp status is favorable. Biodentine has been recently introduced on the market to overcome the limitations of MTA as long setting time, poor handling properties, cost, and the potential discoloration of teeth and soft tissue. Accordingly, this systematic review will provide decision-making process based on scientific evidence for the clinician and health-care provider to select the material of choice as a DPC. The aim of this study was to conduct a systematic review on the efficacy of Biodentine versus MTA as DPC materials for human permanent teeth. This objective was based on a research question; is there is a difference between Biodentine and MTA as DPC materials for permanent mature teeth.
METHODS
Protocol and registration
The methodology of this systematic review was done on the basis of the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-analyses checklist.[15] The review had been registered with international prospective register of systematic reviews (PROSPERO) (registration number CRD42018089302). The clinical question was formulated and organized using the PICO strategy for the research question construction.
Eligibility criteria
The inclusion criteria included were as follows: (1) studies are RCTs or non-RCTs; (2) all selected teeth were permanent molars with symptomless exposure of vital pulp tissue by caries or trauma; (3) the pulp exposures were treated by Biodentine or MTA; (4) all selected teeth had a 1-month follow-up time at least; and (5) the outcome was evaluated by clinical symptoms and/or radiographic evidence. The exclusion criteria were (1) immature teeth, (2) primary teeth, (3) studies assessed mechanical or physical properties of the materials, (4) negative control group which does not have a capping material, (5) indirect pulp capping, pulpotomy, and pulpectomy, and (6) animal and laboratory-based studies, qualitative and/or quantitative reviews, commentaries, case reports/case series, and letters to the editor.
Information sources and search strategy
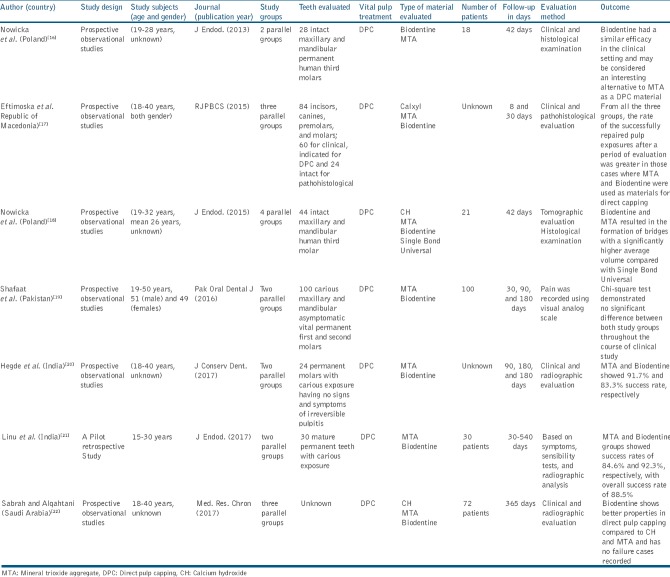
The PROSPERO and the Cochrane Database of Systematic Reviews were searched in February 2018 and presented no existing reviews that were found comparing the effect of these two materials as a DPC for permanent teeth. To identify published clinical trials relevant to the focused question, all searches were conducted independently by two authors (MG and SE). A literature search was conducted based on multiple electronic databases (PubMed [Midline], CENTRAL Cochrane Library, Latin American and Caribbean Health Sciences Literature, Scopus, Scientific Electronic Library Online, evidence-based endodontics literature, KoreaMed records [KoreaMed], and Google Scholar). The literature search was performed from January 2010 to February 2018, based on a predetermined PICOS statement. The population was adult patients; the intervention was tricalcium silicate cement/Biodentine; the comparator was MTA; the outcome was the efficacy of these two materials as a DPC; and the study designs were clinical trials. Medical subject headings terms, “dental pulp capping” and “pulp capping and pulpectomy agents,” were used in our search. Other search words or terms were used in search strategy [Table 1]. The search strategy used in PubMed was adjusted for use in the other databases. These keywords were used with Boolean operators AND, OR, and NOT. References of the identified studies were handsearched to identify further potentially relevant studies, relevant conference proceedings, and relevant abstracts; books as well as searching gray literatures were performed. Any disagreements in the study selection were resolved through discussion with a third author (SM).
Table 1.
Databases involved and the search terms used with the number of references obtained after filtering and applying the eligibility criteria
Study selection and data collection
Two authors (AZ and MZ) screened all the titles and abstracts and selected only studies related to DPC materials in accordance with the eligibility criteria. They independently tabulated the data of interest. From the studies included, the following data were tabulated: authors and their country, study design, journal (year of publication), age and gender of study individuals, study groups, vital pulp treatment, type of material evaluated, follow-up in days, and the type of teeth evaluated. Authors of the studies included were contacted through electronic mail in case data were missing or additional information regarding their studies was required. Fields for which information could not be found in a publication or online abstract were entered as “unknown” and were either excluded in the subsequent meta-analysis or included as “unknown [Table 2].”
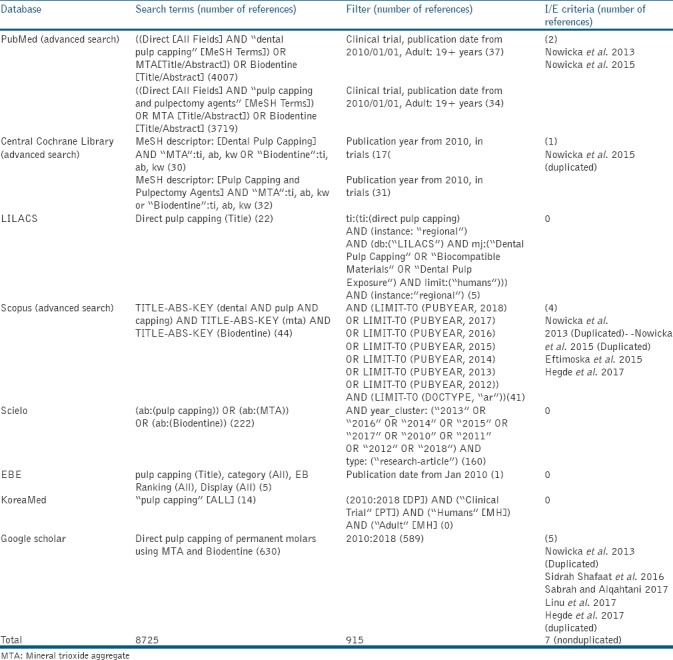
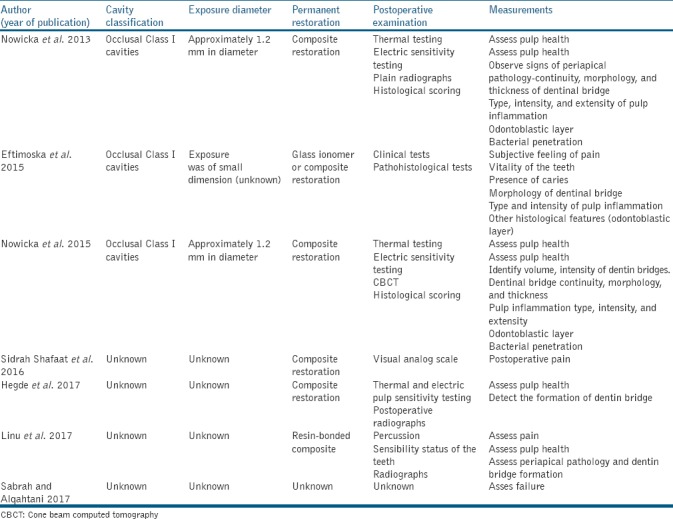
Table 2.
Characteristics of the studies included
Risk of bias in individual studies
To assess article quality, two authors (SM and SE) independently used the “risk of bias (RoB) in nonrandomized studies – of interventions.”[23] It is concerned with evaluating the RoB in the results of nonrandomized studies of the effects of interventions that compare the health effects of two or more interventions. Each criterion was rated as “Yes,” “Probably yes,” “Probably no,” “No,” and “No information [Table 3].” For consistency, any disagreements in the assessment were resolved through discussion with a third author (MG).
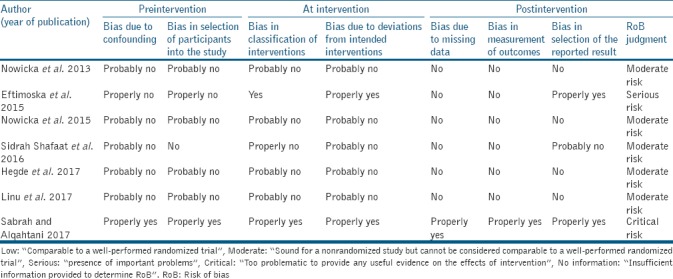
Table 3.
Quality assessment of included studies
Statistical analysis
Degree of chance – adjusted agreement (kappa coefficient value) was used to determine the inter-reviewer reliability.
RESULTS
Study selection
The initial search identified 8725 unique references through the search process. No additional studies were identified through handsearching. After filtering, 915 references were recorded and screened. After the eligibility criteria were applied, seven unduplicated prospective and retrospective cohort studies were obtained and were included in the present review [Table 1 and Figure 1]. The kappa value for interexaminer's agreements was 0.79.
Figure 1.
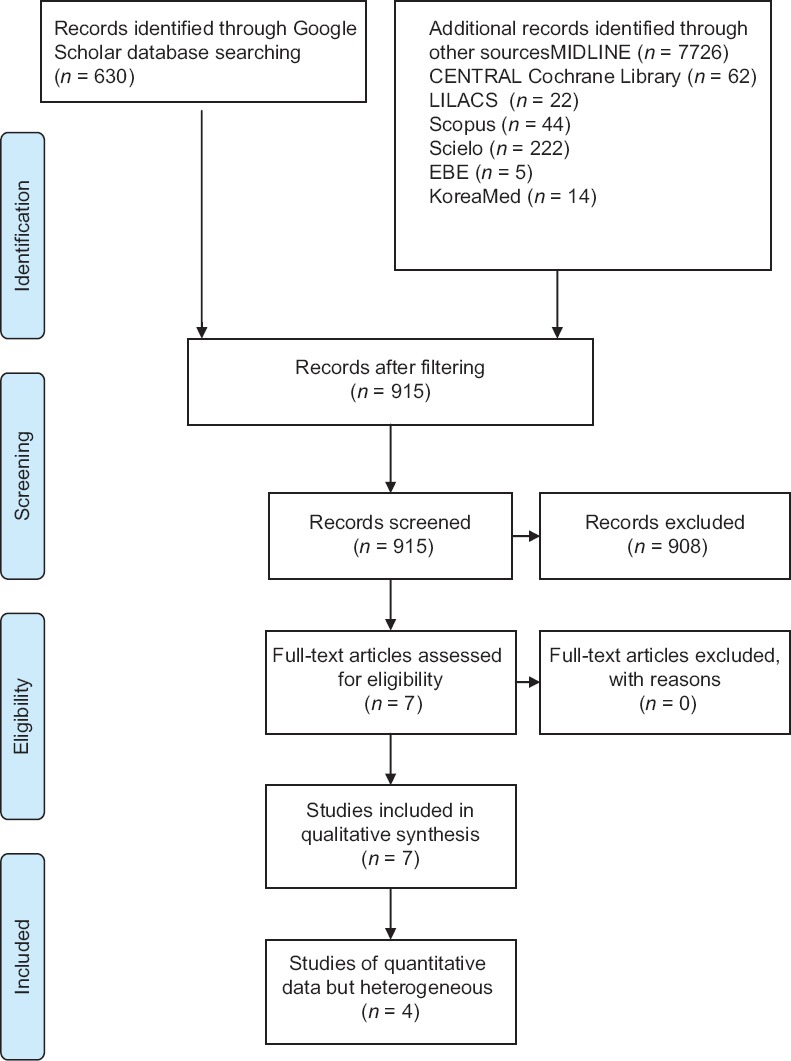
Flowchart for article selection according to preferred reporting items for systematic reviews and meta-analyses guidelines
Study characteristics
One study was performed in 2013 (Poland), two at 2015 (Poland and Republic of Macedonia), one in 2016 (Pakistan), and three in 2017 (India and Saudi Arabia). Six of them were prospective observational studies while the remaining one was pilot retrospective study. Two studies were done by Nowicka et al.[16,18] evaluating the clinical and histological response of human dental pulp capped with Biodentine or MTA. Clinical examination was done through thermal and electric testing, and in addition, plain radiographs and tomographic evaluation using CBCT imaging were performed. Histologically, they evaluated continuity, morphology and thickness of hard tissue formation, type, intensity and extension of pulp inflammation, and other histologic features. Moreover, one study[17] carried their trial on two levels, clinical testing and pathohistological one. The pathohistological evaluation was for dentin bridge morphology, type and intensity of pulp inflammation, and other histological features [Table 4]. The clinical and radiological evaluations were performed after 8 and 30 days for the vitality of teeth, subjective symptoms, and amount of reparative dentin formation. The other four studies recorded the postoperative pain of patients included using visual analog scale after 7 days, 1 month, 3 months, and 6 months. In addition, postoperative radiographs were taken on 3-month and 6-month recall visits to detect any apical radiolucency,[19] assessed the pulpal health after 3 weeks, 3 months, 6 months, and 1 year using thermal and electrical pulp sensitivity testing, and in addition, 6-month follow-up radiographs were taken,[20] analyzed the clinical and radiographic recall data at intervals of 1, 3, 6, 12, and 18 months. The data were comprised pain, sensibility status of the teeth, radiographic signs of periapical pathology, and dentin bridge formation[21] and were performed clinical and radiological examination after 1-year recall.[22]
Table 4.
Heterogeneity assessment of included studies
Risk of bias within studies
Heterogeneity was found between the previous studies.[16,17,18,19,20,21,22] as they used different methods of evaluation (histological, clinical, and radiological), and in addition, different scores for the amount of dentin bridge formation were used in histological and radiological assessments. Pulp vitality was assessed with different parameters; moreover, dichotomous data were sometimes used, and in other instances, continuous data were the main outcome. Common study limitations included inadequate randomization and allocation concealment, nonreporting of study withdrawals and participants lost to follow-up, lack of blinding of outcome assessor, contamination, and failure to perform an intention to treat analysis. Four studies had moderate RoB, two had serious RoB, and one had critical RoB.
DISCUSSION
A systematic review, by virtue of the method used to collect information, provides a solid base for clinical decision-making, due to its high LoE. It is a systematic assessment of the available literature for the effects of health-care interventions and is an assessment that is intended to help professionals in choosing the appropriate treatment.[24]
The main findings of the included studies were dentin bridge formation, inflammatory cell infiltration, amount of pulp necrosis, and pulp vitality. With regard to dentin bridge formation, it was found that Biodentine and MTA are likely to promote the formation of reparative dentin, and they have positive results on odontoblasts when used in DPC. Biodentine and MTA are used in pulp capping due to their involvement in mineralized tissue bridge formation, the preservation of pulpal vitality, and promotion of odontoblast layer integrity.[25] For health-care provider and clinicians, Biodentine is new bioactive cement that is similar to the widely used MTA. It has dentin-like mechanical properties, which may be considered a suitable material for clinical indications of dentin-pulp complex regeneration such as DPC.
The main appeal of the RCT in health care comes from its potential to reduce selection bias. In the present systematic review, all the included studies were parallel groups without randomization and this can be attributed to the little number of participant involved in each study. Studies with small sample sizes have a tendency to be less reliable and are more probably inconclusive due to inadequate statistical power.[26] In addition, the study designs were based in some studies on using sound molar teeth, and in others, they depend on carious teeth. From the biological point of view, the pulp will respond differentially in both situations even at the basis of the molecular level with differential molecular interactions that potentially affect the final outcome. The major causes of postoperative inflammation and pulp necrosis are nonsterile procedures and bacterial micro-infiltration of the pulp through dentin tubules.[27]
Among the drawbacks of the included studies were the short time follow-up evaluation periods. Dentin formation usually starts within 30 days of the pulp capping (there can be a delay in onset of dentin formation if the odontoblasts of the pulp are injured during cavity removal) and is largely completed by 130 days.[28] Moreover, the size of the pulp exposure is not considerably consistent in the included studies. The success of the pulp capping procedure greatly depends on the circumstances under which it is performed, and the prognosis depends on the age, type, site, and size of pulp exposure.[29]
The outcomes of the present systematic review should be taken with caution due to the presence of uncontrolled confounding factors in the included clinical trials. Within the limitations of the existing clinical trials, the results of the present study suggest that the Biodentine had a similar effect on dentin bridge formation likely to MTA. However, this conclusion is based on only very few well-conducted prospective and retrospective cohort studies.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Aguilar P, Linsuwanont P. Vital pulp therapy in vital permanent teeth with cariously exposed pulp: A systematic review. J Endod. 2011;37:581–7. doi: 10.1016/j.joen.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 2.Qureshi A, ES, Nandakumar, Pratapkumar, Sambashivarao Recent advances in pulp capping materials: An overview. J Clin Diagn Res. 2014;8:316–21. doi: 10.7860/JCDR/2014/7719.3980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaur M, Singh H, Dhillon JS, Batra M, Saini M. MTA versus biodentine: Review of literature with a comparative analysis. J Clin Diagn Res. 2017;11:ZG01–ZG05. doi: 10.7860/JCDR/2017/25840.10374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Araújo LB, Cosme-Silva L, Fernandes AP, Oliveira TM, Cavalcanti BD, Gomes Filho JE, et al. Effects of mineral trioxide aggregate, biodentineTM and calcium hydroxide on viability, proliferation, migration and differentiation of stem cells from human exfoliated deciduous teeth. J Appl Oral Sci. 2018;26:e20160629. doi: 10.1590/1678-7757-2016-0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akhlaghi N, Khademi A. Outcomes of vital pulp therapy in permanent teeth with different medicaments based on review of the literature. Dent Res J (Isfahan) 2015;12:406–17. doi: 10.4103/1735-3327.166187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hilton TJ. Keys to clinical success with pulp capping: A review of the literature. Oper Dent. 2009;34:615–25. doi: 10.2341/09-132-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kang JY, Lee BN, Son HJ, Koh JT, Kang SS, Son HH, et al. Biocompatibility of mineral trioxide aggregate mixed with hydration accelerators. J Endod. 2013;39:497–500. doi: 10.1016/j.joen.2012.11.037. [DOI] [PubMed] [Google Scholar]
- 8.Storm B, Eichmiller FC, Tordik PA, Goodell GG. Setting expansion of gray and white mineral trioxide aggregate and Portland cement. J Endod. 2008;34:80–2. doi: 10.1016/j.joen.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 9.Islam I, Chng HK, Yap AU. Comparison of the physical and mechanical properties of MTA and portland cement. J Endod. 2006;32:193–7. doi: 10.1016/j.joen.2005.10.043. [DOI] [PubMed] [Google Scholar]
- 10.Gandolfi MG, Ciapetti G, Taddei P, Perut F, Tinti A, Cardoso MV, et al. Apatite formation on bioactive calcium-silicate cements for dentistry affects surface topography and human marrow stromal cells proliferation. Dent Mater. 2010;26:974–92. doi: 10.1016/j.dental.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 11.Zanini M, Sautier JM, Berdal A, Simon S. Biodentine induces immortalized murine pulp cell differentiation into odontoblast-like cells and stimulates biomineralization. J Endod. 2012;38:1220–6. doi: 10.1016/j.joen.2012.04.018. [DOI] [PubMed] [Google Scholar]
- 12.Coward DD. Partial randomization design in a support group intervention study. West J Nurs Res. 2002;24:406–21. doi: 10.1177/01945902024004008. [DOI] [PubMed] [Google Scholar]
- 13.Kavale KA, Glass GV. Meta-analysis and the integration of research in special education. J Learn Disabil. 1981;14:531–8. doi: 10.1177/002221948101400909. [DOI] [PubMed] [Google Scholar]
- 14.Burns PB, Rohrich RJ, Chung KC. The levels of evidence and their role in evidence-based medicine. Plast Reconstr Surg. 2011;128:305–10. doi: 10.1097/PRS.0b013e318219c171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: Checklist and explanations. Ann Intern Med. 2015;162:777–84. doi: 10.7326/M14-2385. [DOI] [PubMed] [Google Scholar]
- 16.Nowicka A, Lipski M, Parafiniuk M, Sporniak-Tutak K, Lichota D, Kosierkiewicz A, et al. Response of human dental pulp capped with biodentine and mineral trioxide aggregate. J Endod. 2013;39:743–7. doi: 10.1016/j.joen.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 17.Eftimoska M, Apostolska S, Rendzhova V, Gjorgievska E, Stevanovic M, Ivanovski K, et al. Clinical and histological analyzes of the response of the pulp after its direct capping with Calxyl, MTA and biodentine. RJPBCS. 2015;6:1097–111. [Google Scholar]
- 18.Nowicka A, Wilk G, Lipski M, Kołecki J, Buczkowska-Radlińska J. Tomographic evaluation of reparative dentin formation after direct pulp capping with ca(OH) 2, MTA, biodentine, and dentin bonding system in human teeth. J Endod. 2015;41:1234–40. doi: 10.1016/j.joen.2015.03.017. [DOI] [PubMed] [Google Scholar]
- 19.Shafaat OS, Jamil AR, Shazia AS, Maryam M. A comparison of the human pulpal pain response to biodentine and mineral trioxide aggregate as pulp capping agent. Pak Oral Dent J. 2016;36:464–7. [Google Scholar]
- 20.Hegde S, Sowmya B, Mathew S, Bhandi SH, Nagaraja S, Dinesh K, et al. Clinical evaluation of mineral trioxide aggregate and biodentine as direct pulp capping agents in carious teeth. J Conserv Dent. 2017;20:91–5. doi: 10.4103/0972-0707.212243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Linu S, Lekshmi MS, Varunkumar VS, Sam Joseph VG. Treatment outcome following direct pulp capping using bioceramic materials in mature permanent teeth with carious exposure: A pilot retrospective study. J Endod. 2017;43:1635–9. doi: 10.1016/j.joen.2017.06.017. [DOI] [PubMed] [Google Scholar]
- 22.Sabrah SA, Alqahtani MT. Outcomes of direct pulp capping done by different materials in permanent teeth after 1 year recall. Med Res Chron. 2017;4:591–2. [Google Scholar]
- 23.Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Newman MG, Caton JG, Gunsolley JC. The use of the evidence-based approach in a periodontal therapy contemporary science workshop. Ann Periodontol. 2003;8:1–1. doi: 10.1902/annals.2003.8.1.1. [DOI] [PubMed] [Google Scholar]
- 25.De Rossi A, Silva LA, Gatón-Hernández P, Sousa-Neto MD, Nelson-Filho P, Silva RA, et al. Comparison of pulpal responses to pulpotomy and pulp capping with biodentine and mineral trioxide aggregate in dogs. J Endod. 2014;40:1362–9. doi: 10.1016/j.joen.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 26.Halpern SD, Karlawish JH, Berlin JA. The continuing unethical conduct of underpowered clinical trials. JAMA. 2002;288:358–62. doi: 10.1001/jama.288.3.358. [DOI] [PubMed] [Google Scholar]
- 27.Stockton LW. Vital pulp capping: A worthwhile procedure. J Can Dent Assoc. 1999;65:328–31. [PubMed] [Google Scholar]
- 28.Hargreaves K. Cohen's Pathways of the Pulp (Tenth Edition ed) St. Louis, Missouri: Mosby Elsevier; 2011. [Google Scholar]
- 29.Cohen BD, Combe EC. Development of new adhesive pulp capping materials. Dent Update. 1994;21:57–62. [PubMed] [Google Scholar]