Section 1
A 58-year-old woman presented with a 6-month history of progressive dysesthesias and weakness involving her hands as well as ambulatory dysfunction. She described a diffuse “tight band” of pain around her upper abdomen. There was no bladder dysfunction. Her history revealed systemic scleroderma diagnosed in 2001 characterized by Raynaud phenomenon, esophageal dysmotility, pulmonary involvement resulting in pulmonary hypertension, and calcinosis cutis. There was no history of trauma or intervertebral disc disease. She was on immunosuppression with methotrexate and mycophenolate. Pulmonary hypertension was treated with bosentan.
On physical examination, the patient was found to have Madonna facies, diffuse sclerodermatous skin changes, and extensive calcification of the pulp of the fingers with ulcerations. Alignment of the cervical spine was normal on clinical inspection but motility was impaired around all axes. The Spurling sign was negative. Of interest, an indurated immobile mass lesion greater than 1 inch in diameter was palpable in the mid to lower third of the neck posteriorly.
The neurologic examination showed a patient with normal cognitive skills and a known left-sided Bell palsy. Remaining cranial nerves were not impaired. On confrontational testing, muscle strength was normal in the proximal arms and in the legs. Grip and finger extension were weak (3/5) and muscle bulk diminished in the hands while the muscle tone was increased. Biceps reflexes were attenuated while all other deep tendon stretch reflexes were brisk. No pathologic reflexes were elicited. There was a fiber-length-dependent sensory deficit to thermal and vibratory stimuli but no sensory level. There were no cerebellar deficits. The gait was spastic and broad-based. Patient-Reported Outcome Measurement Information System (PROMIS) Global Physical Health 10 Score was 7/20.
Questions for consideration:
Where would you localize the patient's neurologic problem?
Outline the differential diagnosis for the patient's neurologic syndrome.
Propose the order of diagnostic procedures.
Section 2
The patient's neurologic syndrome (symmetric dysesthesias in both arms as well as the lower trunk, weakness in the forearms and hands, and spastic gait abnormality) suggested a cervical myelopathy. Based on absence of pain and the slowly progressive nature of the disease accompanied by decreased mobility, the main differential diagnostic considerations included extrinsic compression by degenerative changes such as a centrally herniated disc or an intrinsic spinal cord process such as a low-grade neoplasm or inflammatory process.
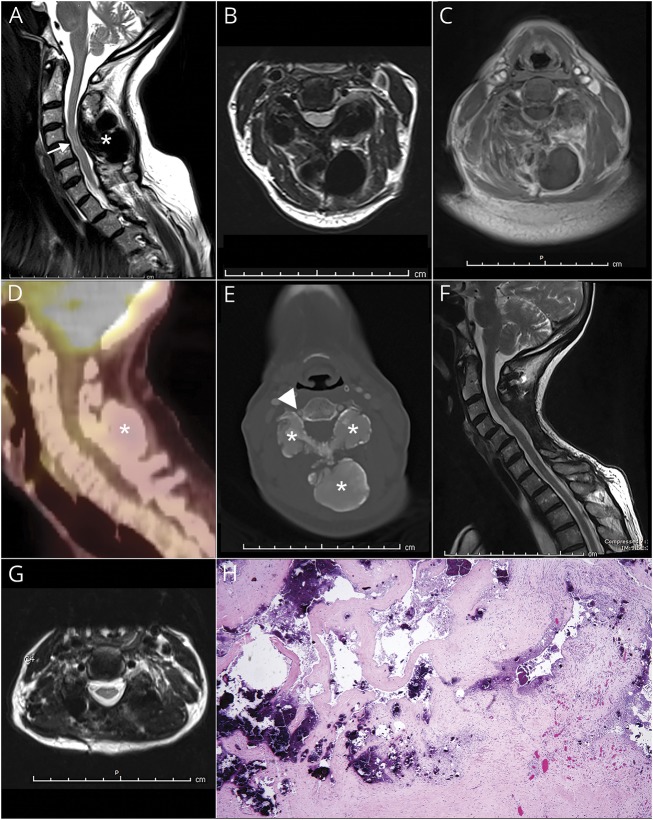
A cervical spine MRI with contrast was obtained and revealed a well-demarcated, T1- and T2-hypointense mass without enhancement. This lesion involved the soft tissues posterior to the spinal canal and was predominantly localized at C4. At this level, spinal canal stenosis with near obliteration of the CSF space as well as an intrinsic spinal cord signal abnormality was demonstrated (figure 1, A–C and E). A CT angiogram was ordered for further characterization of the mass and its relationship to the cervical vasculature. Based on CT characteristics, the cervical mass lesion was composed of a bony matrix. It involved the posterior elements of C4/5, expanded the transverse processes, laminae, and spinous processes, and encroached upon the right C4 foramen transversarium, causing mild mass effect on the vertebral artery (figure 1E). A skull to thigh 18F-FDG PET/CT failed to reveal metabolic activity within the mass (figure 1D).
Figure. Calcified cervical mass lesion (asterisks).
(A–C) Sagittal, axial T2- weighted, and T1-weighted gadolinium-enhanced cervical spine MRI show an intrinsic spinal cord abnormality (arrow in A) related to compression by a large mass involving the C4 vertebral body. (D) The bulky lesion is demonstrated as photopenic by means of 18FDG-PET. (E) Axial neck CT angiogram identifies a bony matrix within the lesion resulting in segmental narrowing of the right vertebral artery at C4 (arrowhead). (F, G) Sagittal and axial T2-weighted postoperative MRI shows the effects of resection of the mass and nearly complete resolution of intrinsic cord signal abnormality. (H) Hematoxylin & eosin stain of the biopsy specimen shows dense regular fibroconnective tissue with reactive fibrovascular proliferation and multiple deposits of calcium hydroxyapatite (original magnification × 40).
Questions for consideration:
How do the imaging studies help you narrow your differential diagnosis?
What are the next steps in management of this case?
Section 3
Lack of metabolic activity as demonstrated on PET/CT narrowed the differential diagnosis to fibrous dysplasia or a benign primary osteogenic tumor such as osteoblastoma.1 Given the patient's history of systemic scleroderma, diffuse calcinosis of the neck was also considered. Fine-needle aspiration cytology revealed necrotic tissue with calcifications. Subsequently, the patient was taken to the operating room for C4-6 laminectomy, tumor removal, and C2-T1 fusion. The excised tumor was composed of dense regular fibroconnective tissue with focal necrosis and multiple deposits of calcium hydroxyapatite consistent with calcinosis (figure 1H). The patient was seen for follow-up 6 months after surgery with no evidence of residual or recurrent mass on a surveillance MRI of the cervical spine (figure 1, F and G). Neurologic examination revealed persistent acral dysesthesias in the fingertips and weakness of intrinsic hand muscles while pain sensation improved markedly. The band-like tightening over the patient’s upper abdomen resolved and may be interpreted as what has been described as a false localizing sign of her cervical myelopathy. PROMIS Global Physical Health 10 score had improved and was 13/20. The patient was scheduled for clinical reevaluation in 1 year.
Question for consideration:
What is your final diagnosis?
Discussion
Our diagnosis was cervical myelopathy related to spinal stenosis caused by calcinosis in the setting of systemic scleroderma (SSC). SSC is an immune-mediated rheumatic disorder characterized by dysfunction in the repair of connective tissue. Gastroesophageal reflux and Raynaud phenomenon are the most common primary manifestations. Diagnostic criteria established by the American College of Rheumatology and the European League against Rheumatism include fibrosis of the skin and internal organs, production of autoantibodies, and vasculopathy.2 The disease is most prevalent in middle-aged women. Overall incidence is 20 per million adults per year in the United States.3 The prognosis of SSC is determined primarily by the involvement of internal organs. Subcutaneous calcinosis typically occurs at localized sites of recurrent microtrauma such as elbows. Infrequently, SSC may affect the spinal column through dystrophic calcinosis. Neurologic complications are rare and often result from compression or entrapment of peripheral or cranial nerves.4 We identified reports of 9 patients with soft tissue calcinosis involving the cervical spinal cord resulting in radiculopathy or myelopathy published in the last 20 years.5–7 A single fatal case due to ectopic calcinosis compromising the cervical cord has been reported.7 Diagnosis rests upon CT and MRI of the spine. 18F-FDG PET/CT and SPECT can assist in the distinction from malignant processes. Treatment of SSC focuses on the reduction of symptoms. For management of the common skin-associated complications, various randomized trials revealed the benefit of immune-modulating therapies, namely methotrexate and mycophenolate mofetil. Moreover, endothelin receptor blockers, which are typically used for treatment of pulmonary hypertension, also reduce the number of digital ulcers in patients with SSC.8 Less certain is the effect of immunomodulatory therapy on soft tissue calcinosis and overall survival.9 At this point it is generally recommended to excise symptomatic calcinosis while asymptomatic lesions are followed expectantly. For patients with poor prognosis due to extensive organ manifestations, intensive immunosuppression or stem cell transplantation may be beneficial.10
Our case represents an unusual neurologic complication of SSC. Soft tissue calcinosis can result in profound neurologic morbidity even in patients on immunosuppressive therapy. Modern neuroimaging facilitates timely localization and diagnosis, which serves as the basis for surgical management and restoration of neurologic function.
Author contributions
P. Karschnia: study concept and design, analysis and interpretation of data, drafting and revising of manuscript. R.K. Fulbright: analysis and interpretation of data, revising of manuscript. M.S. Laurans: analysis and interpretation of data, revising of manuscript. A.J. Huttner: analysis and interpretation of data, revising of manuscript. J.M. Baehring: study concept and design, analysis and interpretation of data, drafting and revising of manuscript.
Study funding
No targeted funding reported.
Disclosure
The authors report no disclosures relevant to the manuscript. Go to Neurology.org/N for full disclosures.
References
- 1.Rodallec MH, Feydy A, Larousserie F, et al. Diagnostic imaging of solitary tumors of the spine: what to do and say. Radiographics 2008;28:1019–1041. [DOI] [PubMed] [Google Scholar]
- 2.van den Hoogen F, Khanna D, Fransen J, et al. 2013 classification criteria for systemic sclerosis: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum 2013;65:2737–2747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mayes MD, Lacey JV Jr, Beebe-Dimmer J, et al. Prevalence, incidence, survival, and disease characteristics of systemic sclerosis in a large US population. Arthritis Rheum 2003;48:2246–2255. [DOI] [PubMed] [Google Scholar]
- 4.Amaral TN, Peres FA, Lapa AT, Marques-Neto JF, Appenzeller S. Neurologic involvement in scleroderma: a systematic review. Semin Arthritis Rheum 2013;43:335–347. [DOI] [PubMed] [Google Scholar]
- 5.Nguyen HS, Sharma A, Doan N, Gelsomino M, Shabani S, Maiman D. Central cord syndrome in a patient with systemic sclerosis and cervical calcinosis: case report and review of literature. Spinal Cord Ser Cases 2016;2:15029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Furuta M, Furuta N, Makioka K, et al. Tumoral ectopic calcinosis causing cervical spine compression in a patient with systemic sclerosis. Neurol Clin Neurosci 2017;5:73. [Google Scholar]
- 7.Lima IV, Galrão LA, Maia TS, Santiago MB. Spinal cord compression by ectopic calcinosis in scleroderma. Clin Exp Rheumatol 2005;23:704–706. [PubMed] [Google Scholar]
- 8.Korn JH, Mayes M, Matucci Cerinic M, et al. Digital ulcers in systemic sclerosis: prevention by treatment with bosentan, an oral endothelin receptor antagonist. Arthritis Rheum 2004;50:3985–3993. [DOI] [PubMed] [Google Scholar]
- 9.Volkmann E, Sim M, Tashkin D, et al. OP0124 Treatment with cyclophosphamide for systemic sclerosis-related interstitial lung disease does not improve survival after 12 years of follow up. Ann Rheum Dis 2017;76:104. [Google Scholar]
- 10.Del Papa N, Onida F, Zaccara E, et al. Autologous hematopoietic stem cell transplantation has better outcomes than conventional therapies in patients with rapidly progressive systemic sclerosis. Bone Marrow Transpl 2017;52:53–58. [DOI] [PubMed] [Google Scholar]