Abstract
The invasion of the skin and subcutaneous tissue by the larvae (Maggot) is known as Maggot infestation. It was found that farmers who are working in agricultural fields are more prone to this infestation. A case of 60 year old male patient with ulceration on leg for 10 days which was initially smaller and later developed into a larger wound, due to maggot larvae. This case report illustrates the importance and method of treating this cutaneous myiasis.
Keywords: Maggot, Treatment, Infestation, Flies, Case report, Myiasis
Introduction
Maggot infestation is a condition in which the fly maggots feed off and develop in the tissues of living organisms. True myiasis results from flies deliberately laying eggs in or on the tissues. There are two forms of myiasis: obligate, in which it is necessary for the maggots to feed on living tissues and facultative, where flies opportunistically take advantage of wounds or degenerative necrotic conditions as a site in which to incubate their larvae.1 In general obligate myiasis of humans is topical in origin, whereas facultative myiasis can occur anywhere in the world. Majority of flies that are likely to cause myiasis in humans belong either to the blowfly group, family calliphoridae, or the housefly group, family muscidae. Most species causing facultative myiasis in humans are not pathogenic which is why some are used in larval therapy, while obligate parasites range from the essentially begin to the potentially lethal.
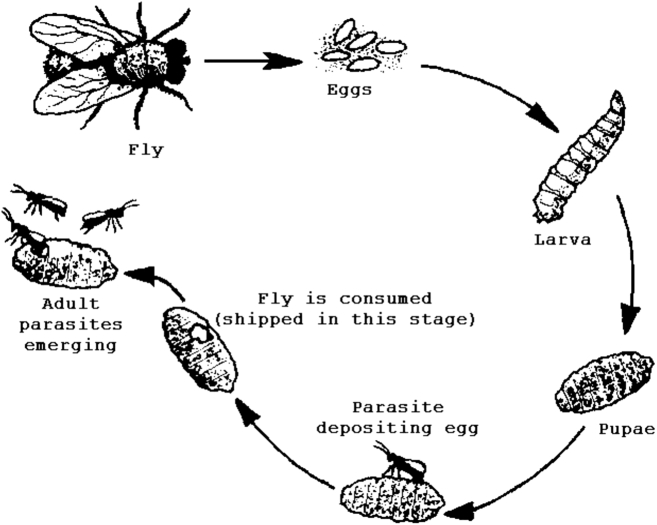
Life cycle of maggot
Female flies may visit wounds to feed or to lay eggs. They generally lay 50–300 eggs at a time and at skin temperature these hatch around 8–12 hours later. The eggs are about 1.7 mm long and the emerging larvae are about the same length but less easy to detect. Once emerged they grow rapidly, within 24 hours at human skin temperature they grows up to 7–8.5 mm long and in only 50–60 hours they attain full growth. They then stop feeding and migrate from the tissue to seek a dry crevice or soil in which to pupate (life stage in which it attains maturation). In all cases this is self-linking, determine only by the temperature and the availability of food. Insects in this group normally only take necrotic tissue and slough and it is rare to find them debriding viable tissue.2
Symptoms
The symptoms of myiasis depend on the area of the body that is infested.
Cutaneous myiasis: in which the maggot penetrates the skin and develops in the tissue under the skin, is probably the most commonly observed form of myiasis. The most common infestation sites are exposed areas such as the extremities, back, and scalp. Within 24 hours, a papule resembling an insect bite will swell into a boil-like lesion ranging anywhere from 10 to 35 mm in diameter. Often, there is a small (2–3 mm diameter) pore at the center of the boil which allows the larvae to breathe. The patient may experience pain, and some have reported feeling the larvae moving around within the tissues. This phenomenon is probably more common with D. hominis, which have relatively large larvae possessing outer layers of spikes.3
Creeping myiasis: occurs with parasitic maggots which are not able to develop in humans. Man serves as an accidental host for these flies, which include several species of Hypoderma. The primary symptom is a painful swelling that “creeps” throughout the body as the first in star larvae migrate and look for suitable sites for its development.
Wound myiasis: occurs as a result of egg deposition on decaying flesh or pus-discharging wounds. If the maggots invade rather than staying on superficial layers of exposed tissue, subcutaneous nodules can result.
Myiasis of body cavities: results from maggot infestation on the eye, nasal passages, ear canal, or mouth. It is usually caused by D. hominis and the screw worms. If the maggots penetrate into the base of the brain, meningitis and death can result. Ophthalmomyiasis is commonly a result of O. ovis infestation. In rare cases, there could be blindness due to invasion into the optic nerve.
Accidental myiasis: results from ingestion of eggs or existing maggots into the gastrointestinal tract. Local irritation, vomiting, and diarrhea are the usual symptoms. The low oxygen levels in the gut usually will kill the maggots, but some survive intact because their outer layers are resistant to digestive enzymes.4
Management therapy
The treatment of myiasis, forcible removal of larva from the host tissue is not possible because of the larva's tapered shape and many rows of spines and hooks that it uses to grip the tissue cavity. While myiasis is self-limiting and, in many cases, not dangerous to the host, several authors suggest that the psychological distress associated with maggot infestations alone is sufficient reason to treat even the most harmless cutaneous myiasis.
Surgical debridement
Surgical incision and extraction of the larva is usually done under local anesthesia. Care must be taken to prevent laceration of the larva; any portion of the larva remaining in the tissue cavity will produce an undesirable inflammatory response, a bacterial infection, or the formation of a granuloma. Surgery may be unnecessary except in cases in which the larva has died inside the lesion.
The surgical treatment is accompanied by systemic administration of antimicrobials to control secondary infection.
Innovative alternative treatment strategies
An alternative to both surgical and suffocation techniques is the injection of lidocaine at the base of the tissue cavity in which the larva inhibits. The local swelling forces the larva to the surface, where it is easily grasped and removed. This technique may be of limited use in cases involving multiple larvae, as necessary doses lidocaine or other anesthetic could prove toxic.5
Case report
A 60 years old, Indian male farmer, came to the hospital with a history of ulceration over right leg for 10 days which was initially small in size and later developed into increased size (6 × 5 cm) with pain and itching on the wound site. On general examination the patient was regular, conscious, oriented and tongue coated. Patient was anemic and pedal edema was also present. Pale granulation tissue was present on the wound site. After examination it was found myiasis on the right leg (parasitic infestation of a live mammal by fly larvae maggots) that had grown inside the host by feeding on its tissue, some of the visible larvae were removed and then treated with Inj. Taximax 1.5 g IV twice a day, Tab. Albendazole 400 mg Stat, Tab. Livogen (Ferrous fumarate plus folic acid) to treat anemia. The wound was cleaned and dressed every alternate day. The patient was discharged after 5 days of IV antibiotic treatment and asked to review in outpatient department for dressing. The wound was later healed completely.
Discussion
Myasis has been defined as an infestation on humans and vertebrate animals by larvae of insects, which feeds themselves, for certain time, on living or dead tissue from the host or on fluid substances.6 Most of the cases occur in developing and under developed countries where sanitation is a public health problem. The most common cases occur during summer and in tropical climate due to the fact that the larvae need warm temperature to incubate.7 Myiasis from some types of larvae can be useful to the host because they help on necrotic tissue extraction. That is why larvae were used for therapeutic removal of wounds.8
Current treatment for wound myiasis requires debridement with irrigation to eliminate the larvae from the wound or surgical removal. Application of chloroform, chloroform in light vegetable oil, or ether, with removal of the larvae under local anesthesia, has been advocated for wound myiasis.9 Followed by treatment with a broad spectrum antibiotics. Surgical removal is not required unless requested by the patient, as the larvae are naturally sloughed within 5–7 weeks.10
Conclusion
Health education is a paramount to the prevention of myiasis. The incidence of myiasis can be reduced by wearing safety coverings on legs while working in agricultural fields. Treating this type of patients with antibiotics and anthelmintics is quite sufficient, further the eradication of maggot eggs from the infected site is mandatory to prevent further remission of the infection. Probably due to under reporting many clinicians and clinical pharmacist still have inadequate knowledge about clinical implications of human myiasis. Health care professionals should be aware of identification and also to initiate appropriate supportive treatment wherever necessary to minimize morbidity.
References
- 1.Franza R., Leo L., Minerva T., Sanapo F. Myiasis of the tracheostomy wound: case report. Acta Otorhinolaryngol Ital. 2006;26(4):222–224. [PMC free article] [PubMed] [Google Scholar]
- 2.Spradbery J.P. Screw-worm fly: a tale of two species. Agric Zool Rev. 1994;6:1–62. [Google Scholar]
- 3.Amendt J., Goff M.L., Compobasso C.P., Gherardi M. Springer; 2010. Forensic Implications of Myiasis, Current Concepts of Forensic Entomology. Chapter 14. [Google Scholar]
- 4.Arora S., Sharma J.K., Pippal S.K., Sethi Y., Yadav A. Clinical etiology of myiasis in ENT: a reterograde period—interval study. Braz J Otorhinolaryngol. 2009;75(3):356–361. doi: 10.1016/S1808-8694(15)30651-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.http://web.stanford.edu/group/parasites/ParaSites2004/Myiasis/symptoms.htm.
- 6.Zumpt F. first ed. Butterworths; London, UK: 1965. Myiasis in Man and Animals in the Old World. [Google Scholar]
- 7.Sutherst R.W., Spradbery J.P., Maywald G.F. The potential geographical distribution of the old world screw-worm fly, chrysomya bezziana. Med Vet Entomol. 1989;3(3):273–280. doi: 10.1111/j.1365-2915.1989.tb00228.x. [DOI] [PubMed] [Google Scholar]
- 8.Sonikpreet Sonikpreet, Gulshan Oberoi, and Sarwan Kumar. Case report: maggots' infestation as a predisposing condition for heparininduced thrombocytopenia, a newest entity. December, 6, 2014: 124(21).
- 9.Vitavasiri M.D.A., Charoenchasri M.D.P., Kaewmanee M.S.S., Bhaibulaya M.D.M. Subdermal myiasis caused by maggots of chrysomyia bezziana. Siriraj Hospital Gazzetee. 1995;47(5):419–422. [Google Scholar]
- 10.Lebwohl M.G., Heymann W.R., Berth-Jones J., Coulson I. second ed. Elesevier-Mosby; 2006. Myiasis. Treatment of Skin Diseases. Comprehensive Therapeutic Strategies; pp. 420–421. [Google Scholar]