Abstract
Background
Quantification of the burden of overweight on the healthcare system is becoming increasingly urgent for health policy, but accurate estimates are hard to obtain.
Methods
In order to assess healthcare utilisation and expenditure of overweight and non-overweight children, we linked, on an individual basis, data on body mass index from a birth cohort study with administrative health insurance claims data. In children aged 14–15 years, we compared utilisation and expenditure on general practice care, dental care, hospital/specialist care, prescribed medication, allied healthcare and mental healthcare of overweight children (overweight at age 11 and 14, n=80) and non-overweight children (no overweight at age 11 and 14, n=1253).
Results
For overweight children, mean 1-year healthcare expenditure was €837 per child and for non-overweight children €616. This difference was mainly due to significant differences in utilisation of hospital care (49% vs 37%) and mental healthcare (14% vs 7%) and to a lesser extent to higher expenditure per user.
Conclusion
Our results indicate the potential value of linking survey data to claims data in order to obtain insight into the healthcare costs of childhood overweight. Further studies should elucidate whether the observed differences are causally related to overweight.
Keywords: obesity, child health, health services
Introduction
Overweight is increasing worldwide, and it has a high prevalence already in childhood and jeopardises health in the short and long run.1 Quantification of the burden of overweight on the healthcare system and healthcare costs is therefore becoming increasingly urgent for health policy. Assessing overweight-related costs of healthcare is a challenge, however, as few data sources contain data on individuals’ weight status as well as on their healthcare expenditure. In this study, we explore the potential of linking birth cohort data with administrative data to assess the utilisation and costs of healthcare of overweight and non-overweight children.
Methods
According to the Dutch Health Insurance Act, all citizens have a mandatory basic health insurance and children up to the age of 18 are insured for free. Health insurance claims are registered by Vektis in a national database of all Dutch healthcare insurers and can be accessed, under strict conditions, for research. The Vektis claims data contain expenditures on different healthcare services, but no data on weight, height or other personal characteristics.
For this study, we used data of participants of the Dutch Prevention and Incidence of Asthma and Mite Allergy (PIAMA) birth cohort (n=3963 at birth in 1996–1997).2 Questionnaire data, obtained when the children were aged 11 and 14 years (n=2231), were anonymised and linked to their health insurance claims by Statistics Netherlands (CBS). CBS functioned as a trusted third party, enabling the linkage between the datasets, while ensuring the privacy of the children involved, according to Dutch law (Statistics Netherlands Act 2003). Of the 2231 PIAMA participants, CBS successfully linked 98%, based on sex, date of birth, postal code and mother’s date of birth (n=2222). For 1998 of these children, complete health claims data, provided by the insurance companies, were available in 2011 when the children were aged 14–15 years. Weight and height were measured and reported by the parents when the children were aged 11 years and again when they were aged 14 years (data at 11 and/or 14 years available for n=1453 of the 1998 children with complete health claims data). Body mass index (kg/m2) was calculated and overweight (including obesity) was defined based on the International Obesity Task Force (IOTF) age-specific and sex-specific cut-off points.3
Healthcare expenditure (€/year) and utilisation (% users, defined as individuals with >0 €/year expenditure) were compared between children who were overweight at age 11 and at age 14 (n=80) and children who were not overweight at age 11 nor at age 14 (n=1253).
Results
Utilisation
All children were users of general practitioner (GP) care. (For GP care, this means they were registered with a GP, but it does not necessarily mean they had contact with the GP.) With the exception of GP care and dental care, utilisation was higher among overweight children than among non-overweight children for all healthcare services (see table 1). Utilisation of specialist/hospital care was 49% versus 37% (p=0.037) and use of prescribed medication 55% versus 45% (p=0.087). Utilisation of mental healthcare was twice as high among overweight children as among non-overweight children: 14% versus 7% (p=0.034).
Table 1.
One-year healthcare utilisation and expenditure of overweight and non-overweight children: % users of different healthcare services and expenditures per user
| Healthcare service | Users % (n/N) | Expenditure per user (€/year)§¶ | |
| Mean (SD) | Median (IQR) | ||
| General practice | |||
| Not overweight | 99.8 (1251/1253) | 102 (42) | 89 (77 – 108) |
| Overweight | 100 (80/80) | 110 (61) | 92 (80 – 118) |
| Dental care | |||
| Not overweight | 94.9 (1189/1253) | 132 (112) | 103 (55 – 169) |
| Overweight | 91.3 (73/80) | 130 (102) | 93 (68 – 171) |
| Hospital/specialist | |||
| Not overweight | 37.1 (465/1253) | 448 (756) | 211 (97 – 495) |
| Overweight | 48.8 * (39/80) | 498 (654) | 206 (113 – 550) |
| Prescribed medication | |||
| Not overweight | 45.2 (566/1253) | 128 (436) | 40 (19 – 89) |
| Overweight | 55.0 (44/80) | 103 (152) | 54 (21 – 128) |
| Allied healthcare† | |||
| Not overweight | 18.0 (225/1253) | 258 (204) | 204 (104 – 370) |
| Overweight | 21.3 (17/80) | 337 (292) | 235 (117 – 492) |
| Mental healthcare | |||
| Not overweight | 7.3 (91/1253) | 1389 (1602) | 640 (305 – 2149) |
| Overweight | 13.8 * (11/80) | 1528 (1992) | 558 (311 – 2231) |
| Total expenditure (€/year)§ ¶ | |||
| Any healthcare‡ | |||
| Not overweight | 100 (1253/1253) | 616 (915) | 317 (192 – 638) |
| Overweight | 100 (80/80) | 837 (1213) | 379 (222 – 874) |
*P<0.05 based on χ2 test.
†Care provided by professionals like physiotherapists, speech therapists and dieticians.
‡‘Any healthcare’, and the corresponding total expenditure on healthcare, contain—in addition to the services shown in this table—a few healthcare services with low utilisation and low costs, such as patient transport and healthcare used abroad.
§The Wilcoxon-Mann-Whitney test was applied to test statistical significance of differences; no p values<0.05 were observed.
¶Expenditures are shown in 2011€. In 2017€, they would be a factor 1.09 higher.
Expenditure per user
Whereas utilisation of mental healthcare was relatively low, mean expenditure per user of mental healthcare was far higher than mean expenditure per user of any other healthcare service. Costs per user for overweight users and non-overweight users were €1528 versus €1389 per user per year for mental healthcare; €498 versus €448 for specialist/hospital care; and €337 versus €258 for ‘allied healthcare’ (care provided by professionals like physiotherapists, speech therapists, dieticians). These differences were not statistically significant (table 1).
Total expenditure
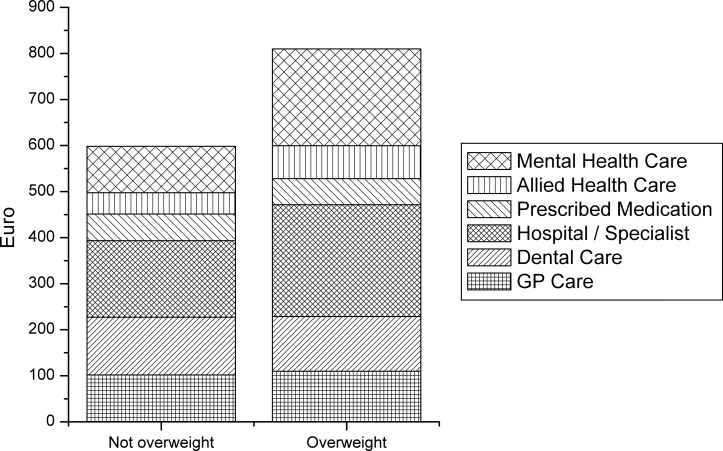
Total expenditures were on average €837 (SD €1213) for overweight children and €616 (SD €915) for non-overweight children (p=0.07) (see last row table 1). Figure 1 shows the contribution of the main types of healthcare to these total expenditures. Mental healthcare and hospital/specialist care were the largest contributors to the differences between overweight and non-overweight children in total annual healthcare expenditure. Higher utilisation contributed more than higher expenditure per user to the differences in total healthcare expenditure between overweight and non-overweight children.
Figure 1.
Total average healthcare expenditures* and expenditures per type of healthcare of overweight (n=80) and non-overweight children (n=1253).*‘Total average healthcare expenditures’ are the sum of the average expenditures on the different healthcare services shown in the figure. They are slightly lower than the mean ‘expenditures on any healthcare’ in table 1 that include a few healthcare services with low utilisation and low costs, which are not included in this figure (such as patient transport and healthcare used abroad). GP, general practitioner.
Discussion
Higher healthcare utilisation and costs among overweight than among non-overweight children have been observed previously, but studies from Europe are scarce and have mostly relied on questionnaire reported use of healthcare services in order to estimate costs.4–7 The majority of cost-of-childhood-overweight studies have been conducted in the USA, based on linkage of data from the Medical Expenditure Panel Survey8 with information from healthcare providers.9–14 Linkage of survey to claims data, as we did in our study, has been applied in Australia15 16 and Canada,17 but, to our knowledge, not in Europe. Our results indicate the potential value of this approach and suggest that linking survey data to claims data could also provide insight into healthcare utilisation and expenditure related to other lifestyle factors and conditions.
Although exploring the linkage of individual survey data to registered health insurance claims showed promising results, a number of limitations of our study have to be considered. We used a fairly strict definition of overweight (being overweight at age 11 and at age 14) to avoid including children in the overweight category who happened to have ‘crossed the overweight cut-off’ at just one occasion. This resulted in low numbers of overweight users for some types of healthcare and consequently limited statistical power to assess differences in expenditure between these children and their non-overweight counterparts. We were unable to conduct separate analyses on obese children. In the Netherlands, the prevalence of obesity in this age group is <2%18 and in our study population <1% of the children were obese at both the age of 11 and of 14 years. Also, we were unable to conduct more detailed analyses, such as analyses stratified for family socioeconomic status. Furthermore, we had no information on the health problems underlying the insurance claims so that causality cannot be established from this study.
In conclusion, our study indicates that already in childhood healthcare utilisation is higher among overweight than among non-overweight individuals and it suggests that linking survey data to administrative data offers promising opportunities for future cost-of-childhood-overweight studies. Further studies are needed to provide insight into the specific health problems of overweight children that underlie the excess use of hospital and mental healthcare observed in this study.
What is already known on this subject.
The burden of childhood overweight on the healthcare system continues to increase, but is difficult to quantify.
What this study adds.
Linking, on an individual basis, data on body mass index from a birth cohort study with registered health insurance claims data, we used an innovative approach to compare healthcare utilisation and expenditure of overweight and non-overweight children.
In our general population sample of children aged 14–15 years, we observed excess utilisation by overweight children compared with non-overweight children of hospital care (49% vs 37%) and mental healthcare (14% vs 7%).
Acknowledgments
The authors thank Vektis for providing access to the health claims data and for sharing their comprehensive knowledge on health claims data.
Footnotes
Contributors: AHW contributed to the design of the PIAMA birth cohort and supervised data collection and management. AHW, SMM and EU conceived the design of this study. AHW and EU collaborated with Statistics Netherlands to establish the data linkage. SMM analysed the data. AHW wrote the first draft of the paper. All authors critically reviewed the manuscript, were involved in finalising the paper and had final approval of the submitted version.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: Ethics approval for the PIAMA study was obtained from the Ethics Committees of the participating Institutes: Rotterdam, MEC (Medisch Ethische Commisie Erasmus Universiteit Rotterdam/Academische Ziekenhuizen Rotterdam) 132.636/1994/39, 13 June 1994 and 137.326/1994/130, 16 February 1995. Groningen, MEC (Medisch Ethische Commisie Academisch ziekenhuis Groningen) 94/08/92, 26 August 1994. Utrecht/Bilthoven, MEC-TNO (Medisch Ethische Commisie-Toegepast Natuurwetenschappelijk Onderzoek) 95/50, 28 February 1996 (METC_TNO_UtrechtBilthoven_95_50.pdf).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data from the PIAMA birth cohort study are available on request. Requests can be submitted to the PIAMA Principal Investigators. Their names and email addresses are listed on the PIAMA website (http://piama.iras.uu.nl/index-en.php#collaboration). The PIAMA data are not freely accessible in the public domain because this would be in conflict with the agreement between the PIAMA study team and the PIAMA participants. The information participants received at the start of the study (in 1996–1997) included the statement ’the information that we receive from you will only be used for the PIAMA project' and participants gave written informed consent based on this information.
References
- 1.Afshin A, Forouzanfar MH, Reitsma MB, et al. . Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med 2017;377:13–27. 10.1056/NEJMoa1614362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wijga AH, Kerkhof M, Gehring U, et al. . Cohort profile: the prevention and incidence of asthma and mite allergy (PIAMA) birth cohort. Int J Epidemiol 2014;43:527–35. 10.1093/ije/dys231 [DOI] [PubMed] [Google Scholar]
- 3.Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes 2012;7:284–94. 10.1111/j.2047-6310.2012.00064.x [DOI] [PubMed] [Google Scholar]
- 4.Wenig CM. The impact of BMI on direct costs in children and adolescents: empirical findings for the German Healthcare System based on the KiGGS-study. Eur J Health Econ 2012;13:39–50. 10.1007/s10198-010-0278-7 [DOI] [PubMed] [Google Scholar]
- 5.Batscheider A, Rzehak P, Teuner CM, et al. . Development of BMI values of German children and their healthcare costs. Econ Hum Biol 2014;12:56–66. 10.1016/j.ehb.2013.05.007 [DOI] [PubMed] [Google Scholar]
- 6.Breitfelder A, Wenig CM, Wolfenstetter SB, et al. . Relative weight-related costs of healthcare use by children--results from the two German birth cohorts, GINI-plus and LISA-plus. Econ Hum Biol 2011;9:302–15. 10.1016/j.ehb.2011.02.001 [DOI] [PubMed] [Google Scholar]
- 7.Doherty E, Queally M, Cullinan J, et al. . The impact of childhood overweight and obesity on healthcare utilisation. Econ Hum Biol 2017;27:84–92. 10.1016/j.ehb.2017.05.002 [DOI] [PubMed] [Google Scholar]
- 8.U.S. Department Of Health & Human Services, Agency for Healthcare Research and Quality. Medical expenditure panel survey [WWW document]. 2017. https://meps.ahrq.gov/mepsweb/survey_comp/survey.jsp
- 9.Janicke DM, Harman JS, Jamoom EW, et al. . The relationship among child weight status, psychosocial functioning, and pediatric health care expenditures in a medicaid population. J Pediatr Psychol 2010;35:883–91. 10.1093/jpepsy/jsp122 [DOI] [PubMed] [Google Scholar]
- 10.Trasande L, Chatterjee S. The impact of obesity on health service utilization and costs in childhood. Obesity 2009;17:1749–54. 10.1038/oby.2009.67 [DOI] [PubMed] [Google Scholar]
- 11.Finkelstein EA, Trogdon JG. Public health interventions for addressing childhood overweight: analysis of the business case. Am J Public Health 2008;98:411–5. 10.2105/AJPH.2007.114991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Skinner AC, Mayer ML, Flower K, et al. . Health status and health care expenditures in a nationally representative sample: how do overweight and healthy-weight children compare? Pediatrics 2008;121:e269–e277. 10.1542/peds.2007-0874 [DOI] [PubMed] [Google Scholar]
- 13.Monheit AC, Vistnes JP, Rogowski JA. Overweight in adolescents: implications for health expenditures. Econ Hum Biol 2009;7:55–63. 10.1016/j.ehb.2008.07.007 [DOI] [PubMed] [Google Scholar]
- 14.Bell JF, Zimmerman FJ, Arterburn DE, et al. . Health-care expenditures of overweight and obese males and females in the medical expenditures panel survey by age cohort. Obesity 2011;19:228–32. 10.1038/oby.2010.104 [DOI] [PubMed] [Google Scholar]
- 15.Hayes A, Chevalier A, D’Souza M, et al. . Early childhood obesity: association with healthcare expenditure in Australia. Obesity 2016;24:1752–8. 10.1002/oby.21544 [DOI] [PubMed] [Google Scholar]
- 16.Au N. The health care cost implications of overweight and obesity during childhood. Health Serv Res 2012;47:655–76. 10.1111/j.1475-6773.2011.01326.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Janssen I, Lam M, Katzmarzyk PT. Influence of overweight and obesity on physician costs in adolescents and adults in Ontario, Canada. Obes Rev 2009;10:51–7. 10.1111/j.1467-789X.2008.00514.x [DOI] [PubMed] [Google Scholar]
- 18.Schönbeck Y, Talma H, van Dommelen P, et al. . Increase in prevalence of overweight in Dutch children and adolescents: a comparison of nationwide growth studies in 1980, 1997 and 2009. PLoS One 2011;6:e27608 10.1371/journal.pone.0027608 [DOI] [PMC free article] [PubMed] [Google Scholar]