Abstract
Background
The aim of this study is to analyse the health status, the use of public healthcare services and the consumption of prescription drugs in the population of Catalonia, taking into consideration the socioeconomic level of individuals and paying special attention to vulnerable groups.
Methods
Cross-sectional study of the entire population resident in Catalonia in 2015 (7.5 million people) using administrative records. Twenty indicators are analysed related to health, the use of healthcare services and consumption of prescription drugs. Rates, frequencies and averages are obtained for the different variables stratified by age groups (under 15 years, 15–64 years and 65 years or older), gender and socioeconomic status (calculated on the basis of pharmacy copayment levels and Social Security benefits received).
Results
A socioeconomic gradient was observed in all the indicators analysed, in both sexes and in all age groups. Morbidity, use of mental healthcare centres, hospitalisation rates and probability of drug consumption among children is 3–7 times higher for those with low socioeconomic level respect to those with a higher one. In children and adults, the steepest gradient was found in the use of mental health services. Moreover, there are gender inequalities.
Conclusion
There are significant socioeconomic inequalities in health status and in the use of healthcare services in the population of Catalonia. To respond to this situation, new policies on health and other areas, such as education and employment, are required, especially those that have an impact on early years.
Keywords: health inequalities, healthcare use, socio-economic level, population data, administrative data
Introduction
The Great Recession of 2008 had a profound impact on the determinants of health in Spain as a whole and in Catalonia in particular. Among others, it has limited the public’s disposable income and affected the living, working and housing conditions of the Catalan population. More particularly, it has represented a big challenge for the Catalan health system, which has suffered an important reduction in resources. The statistics bear out this negative trend: the proportion of the population below the poverty threshold rose from 18% in 2009 to 21% in 2014; unemployment rose from 8.9% in 2008 to 20.3% in 2014, and the health budget fell by €1.44 billion between 2010 and 2014.1
Typical responses to such scenario of crisis differ greatly among countries. Big differences are found in terms of public policies on health spending and other forms of social protection.2 3 However, some effects appear to be consistent for most countries. These are the increase in suicides4 (though with qualifications5) and the impact on mental health, especially among the unemployed.6 7
Both in Catalonia and in Spain as a whole, certain indicator such as life expectancy and general mortality do not seem to have been affected by the recent economic crisis.8 9 Nonetheless, there is evidence that the crisis has modified the determinants of health and has changed lifestyles and patterns of access to healthcare services.10
As part of the continuous monitoring of the health outcomes of a general population in the long term, it is important to focus on the evolution of inequalities.11 More specifically on the most vulnerable sectors of society, which are the ones most likely to suffer the consequences of economic downturns.12
The recession of recent years has revived the interest in monitoring health inequalities.13 14 However, most of the studies of the issue conducted so far have used information coming from surveys or from small datasets and thus present important limitations. Administrative data, in contrast, provide much larger datasets, corresponding to the whole of the population that comes into contact with the public services, and there are no problems regarding data collection.
This study analyses the health status, measured with the use of public healthcare services and the consumption of prescription drugs, in the entire population of Catalonia. It controls for socioeconomic level, sex and age of individuals and pays particular attention to the most vulnerable groups.
Methods
In Catalonia, and in Spain as a whole, all residents are granted universal healthcare by law.15 This implies that the use of the health system services is free at the point of use, with the only exception of prescription of drugs. These follow a system of copayment calculated according to the individual’s income (or, if appropriate, according to the Social Security benefits received). All residents have their own healthcare ID, with which their use of the health system services (and the medication dispensed) can be easily traced. All contacts with the public healthcare system are recorded in administrative databases for quality assurance and payment purposes and can be merged using the unique healthcare ID.
We make use of this information to generate a cross-sectional database of the resident population in Catalonia in 2015. Three main kinds of outcome variables can be distinguished: variables regarding health, use of healthcare services and consumption of prescription drugs. For more details, these are listed in table 1, with their data sources and reference years. Additionally, there are controls for sex and age group (children under 15 years, 15–64 years, 55–64 years and 65 years or over).
Table 1.
Indicators analysed, data sources and reference years
| Indicator | Data source | Year |
| Mortality rate per 1000 inhabitants | Mortality registry | 2014 |
| Mortality rate due to suicide per 100 000 inhabitants | Mortality registry | 2014 |
| People with high morbidity (%)* | Databases for primary care (CMBD-AP), acute hospitals (CMBD-HA), emergencies (CMBD-URG), mental health outpatient centres (CMBD-SMA) and psychiatric hospitalisation (CMBD-SMH) | 2015 |
| People attended in primary care (%) | Database for primary care (CMBD-AP) | 2015 |
| Mean number of visits to primary care services | Database for primary care (CMBD-AP) | 2015 |
| People attended at emergency services (%) (acute hospital, primary care emergency centres or emergency medical services) | Database for emergencies (CMBD-URG) | 2015 |
| Mean number of visits to emergency care services | Database for emergencies (CMBD-URG) | 2015 |
| People attended at mental health centres (%) (excluding the under 5 years old) | Database for mental health outpatient centres (CMBD-SMA) | 2015 |
| Mean number visits to mental health centres (excluding the under 5 years) | Database for mental health outpatient centres (CMBD-SMA) | 2015 |
| Hospitalisation rate per 1000 inhabitants | Database for psychiatric hospitalisation (CMBD-SMH) | 2015 |
| Potentially preventable hospitalisation rate (complications of diabetes mellitus, heart failure, chronic obstructive pulmonary disease, asthma, angina pectoris, urinary tract infections, bacterial pneumonia, dehydration and hypertension) per 1000 inhabitants (excludes population under the age of 45)† | Database for acute hospitals (CMBD-HA) | 2015 |
| Rate of surgical hospitalisation per 1000 inhabitants | Database for acute hospitals (CMBD-HA) | 2015 |
| Rate of psychiatric hospitalisation per 1000 inhabitants (excluding the under 5 years) | Database for acute hospitals (CMBD-HA) | 2015 |
| Individuals consuming medication (%) | Pharmacy billing database | 2015 |
| Mean number of prescriptions | Pharmacy billing database | 2015 |
| People with psychoactive drugs’ prescriptions retired from the pharmacy (also known as, consumers of psychoactive drugs) (%) (anxiolytics, antidepressants or antipsychotics, excluding the under 5 years) | Pharmacy billing database | 2015 |
| Consumers of anxiolytics (%) (excluding the under 5 years) | Pharmacy billing database | 2015 |
| Consumers of antidepressants (%) (excluding the under 5 years) | Pharmacy billing database | 2015 |
| Consumers of antipsychotics (%) (excluding the under 5 years) | Pharmacy billing database | 2015 |
| Consumers of attention deficit hyperactivity disorder (ADHD) drugs (%) (population aged 6–24 years) | Pharmacy billing database | 2015 |
*Monterde D, Vela E, Clèries M; grupo colaborativo GMA. Los grupos de morbilidad ajustados: nuevo agrupador de morbilidad poblacional de utilidad en el ámbito de la atención primaria. Aten Primaria 2016;48:674–82.
†AHRQ Quality Indicators. Guide to Prevention Quality Indicators: Hospital Admission for Ambulatory Care Sensitive Conditions. Rockville, MD: Agency for Healthcare Research and Quality, 2001. AHRQ Pub. No. 02-R0203. https://www.ahrq.gov/downloads/pub/ahrqqi/pqiguide.pdf.
CMBD, Conjunt mínim bàsic de dades.
Socioeconomic status was derived from the information used to calculate the levels of copayment (ie, an individual’s income or Social Security benefits received; definitions of the various allowances and benefits can be found in online supplementary annex 1) included at the Catalan government’s central registry of insured individuals as of 1 January 2015. Children were assigned to the socioeconomic level of their tutor (mother, father or legal guardian). The groups that comprise the active population, ranging from the lowest socioeconomic level to the highest, are16 17:
Individuals receiving the renda mínima d’inserció (minimum integration income or RMI) or the renda activa d’inserció (active integration income or RAI) or who no longer receive the unemployment allowance.
Individuals receiving the unemployment allowance.
Individuals who no longer receive unemployment benefit and do not qualify for unemployment allowance.
Individuals receiving unemployment benefit.
Individuals in employment earning less than €18 000 per year.
Individuals in employment earning between €18 000 and €100 000 per year or individuals affiliated to the mutual insurance system for civil servants.
Active population (in employment or not) with an income starting at €100 000 per year.
jech-2018-210817supp001.pdf (87.1KB, pdf)
Individuals receiving pensions are grouped as follows, from the lowest socioeconomic level to the highest16 17:
Individuals receiving a non-contributory pension.
Individuals receiving a contributory pension with an annual income of less than €18 000.
Individuals receiving a contributory pension with an annual income between €18 000 and €100 000.
Individuals receiving a contributory pension with an annual income of €100 000 or more.
We excluded individuals with incomes below €18 000, whose employment status was unknown and who did not receive the RMI, the RAI or a non-contributory pension, and people with toxic syndrome, some disabled groups on work integration programmes or minors on tutored programmes, given the small number of individuals in these groups.
For the analysis of mortality due to suicide, the working population was divided into three groups with regard to socioeconomic level (non-working population, people in employment earning less than €18 000 per year and people in employment earning between €18 000 and €100 000 per year) and pensioners into two groups (people receiving a non-contributory pension and people receiving a contributory pension with an annual income less than €18 000, and people receiving a contributory pension with an annual income between €18 000 and €100 000), given the low number of deaths in this population.
Rates, frequencies and averages were calculated for the different outcome variables. The results were stratified by age groups and sex and are presented for the different socioeconomic levels (online supplementary table 1). Within the same age group, the results were standardised using the population resident in Catalonia according to the registry of insured individuals on 1 January 2015 as the reference population.
jech-2018-210817supp002.pdf (204.3KB, pdf)
Results
Detailed results for each of the indicators are presented in tables 2–4 according to sex, age group and for socioeconomic level. The most relevant results for each of the indicators are described below.
Table 2.
Results of the indicators in the under-15 group, divided according to sex and socioeconomic level (Catalonia, 2015)
| Individuals under 15 years | Unemployment allowance expired, RMI/RAI | Unemployment allowance | Unemployment benefit expired | Unemployment benefit | Income <€18 000 | Income €18 000€ to €100 000 | Income >€100 000 | Max/min | ||||||||
| Girls | Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls | Boys | |
| Individuals with high morbidity (%) | 0.5 | 0.6 | 0.4 | 0.4 | 0.3 | 0.3 | 0.3 | 0.4 | 0.2 | 0.3 | 0.2 | 0.2 | 0.1 | 0.2 | 4.0 | 2.8 |
| Individuals seen at primary care (%) | 86.4 | 86.6 | 87.0 | 86.8 | 66.8 | 67.7 | 82.5 | 83.3 | 86.6 | 86.7 | 78.6 | 79.3 | 55.8 | 55.2 | 1.6 | 1.6 |
| Mean primary care visits | 7.8 | 7.9 | 7.5 | 7.7 | 7.0 | 7.1 | 7.1 | 7.2 | 6.6 | 6.7 | 5.8 | 5.9 | 4.2 | 4.4 | 1.9 | 1.8 |
| Individuals seen at emergency care (%) | 37.5 | 41.0 | 37.1 | 39.8 | 26.2 | 29.4 | 33.2 | 35.5 | 34.4 | 37.2 | 28.4 | 31.4 | 17.0 | 19.3 | 2.2 | 2.1 |
| Mean emergency care visits | 2.19 | 2.2 | 2.1 | 2.1 | 1.9 | 2.1 | 2.0 | 2.0 | 1.9 | 1.9 | 1.8 | 1.8 | 1.5 | 1.7 | 1.4 | 1.3 |
| Individuals seen at mental health centres (%) | 5.9 | 11.4 | 5.9 | 10.9 | 3.7 | 7.0 | 4.7 | 8.3 | 4.6 | 8.6 | 3.0 | 5.8 | 1.3 | 2.2 | 4.4 | 5.1 |
| Mean mental health centre visits | 6.0 | 6.3 | 6.0 | 6.5 | 6.2 | 6.9 | 6.3 | 6.8 | 6.0 | 6.4 | 6.5 | 6.9 | 6.4 | 6.1 | 1.1 | 1.1 |
| Hospitalisation rate (per 1000 inhabitants) | 45.6 | 58.0 | 38.4 | 55.9 | 29.0 | 41.1 | 31.7 | 45.3 | 33.5 | 48.9 | 26.4 | 39.4 | 13.4 | 26.7 | 3.4 | 2.2 |
| Surgical hospitalisation rate (per 1000 inhabitants) | 16.7 | 25.4 | 15.6 | 23.8 | 10.1 | 17.8 | 12.1 | 21.1 | 14.5 | 23.3 | 12.0 | 18.9 | 6.1 | 11.4 | 2.8 | 2.2 |
| Psychiatric hospitalisation rate (per 1000 inhabitants) | 2.3 | 1.4 | 1.9 | 0.9 | 2.0 | 1.3 | 1.4 | 0.3 | 1.2 | 0.7 | 1.1 | 0.7 | 1.3 | 0.2 | 2.2 | 6.8 |
| Individuals consuming medication (%) | 69.9 | 70.5 | 66.4 | 66.7 | 47.4 | 48.7 | 60.2 | 61.4 | 62.2 | 63.6 | 50.6 | 52.5 | 32.3 | 33.5 | 2.2 | 2.1 |
| Mean no. of prescriptions | 6.9 | 7.7 | 5.3 | 6.0 | 5.2 | 5.8 | 5.1 | 5.6 | 4.8 | 5.4 | 4.6 | 5.2 | 4.7 | 5.1 | 1.5 | 1.5 |
| Individuals consuming psychoactive drugs (%) | 5.1 | 6.3 | 4.4 | 5.3 | 3.0 | 3.3 | 3.6 | 4.0 | 3.6 | 4.1 | 2.7 | 3.1 | 1.5 | 1.8 | 3.4 | 3.4 |
| Individuals consuming anxiolytics (%) | 4.4 | 4.3 | 3.8 | 3.7 | 2.6 | 2.3 | 3.1 | 2.9 | 3.1 | 2.9 | 2.3 | 2.2 | 1.1 | 1.2 | 4.1 | 3.4 |
| Individuals consuming antidepressants (%) | 0.4 | 0.4 | 0.4 | 0.4 | 0.4 | 0.3 | 0.4 | 0.3 | 0.4 | 0.3 | 0.3 | 0.3 | 0.3 | 0.2 | 1.6 | 2.2 |
| Individuals consuming antipsychotics (%) | 0.5 | 1.6 | 0.4 | 1.2 | 0.3 | 0.8 | 0.3 | 0.8 | 0.3 | 0.8 | 0.2 | 0.6 | 0.3 | 0.3 | 2.4 | 4.7 |
| Individuals consuming ADHD drugs (%) | 1.2 | 3.5 | 1.4 | 3.3 | 0.9 | 2.9 | 1.2 | 3.1 | 1.3 | 3.6 | 1.1 | 3.2 | 1.7 | 3.3 | 1.8 | 1.2 |
Table 3.
Results of the indicators in the 15–64 years age group, divided according to sex and socioeconomic level (Catalonia, 2015)
| Individuals aged 15–64 years | Unemployment allowance expired, RMI/RAI | Unemployment allowance | Unemployment benefit expired | Unemployment benefit | Income<18 000€ | Income 18,000€ - 100,000€ | Income>1 00 000€ | Max/Min | ||||||||
| Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | |
| Mortality rate (includes 0–64 years) (per 1000 inhabitants) | 1.1 | 2.4 | 0.5 | 1.6 | 0.6 | 1.4 | 0.3 | 1.1 | 0.4 | 0.9 | 0.4 | 0.7 | 0.6 | 0.6 | 3.7 | 3.8 |
| Mortality rate due to suicide (per 100.000 inhabitants) | 3.3 | 12.1 | 3.3 | 12.1 | 3.3 | 12.1 | 3.3 | 12.1 | 2.6 | 9.0 | 2.4 | 6.5 | 2.4 | 6.5 | 1.4 | 1.8 |
| Individuals with high morbidity (%) | 2.2 | 2.2 | 0.9 | 1.4 | 1.0 | 0.9 | 0.7 | 0.9 | 0.7 | 0.8 | 0.4 | 0.6 | 0.2 | 0.3 | 8.9 | 8.1 |
| Individuals seen at primary care (%) | 82.8 | 68.8 | 80.7 | 70.3 | 64.2 | 48.1 | 75.1 | 65.5 | 78.1 | 66.1 | 63.3 | 59.7 | 41.0 | 34.7 | 2.0 | 2.0 |
| Mean primary care visits | 8.2 | 6.8 | 6.7 | 6.0 | 6.3 | 5.3 | 6.2 | 5.5 | 6.5 | 5.5 | 5.3 | 4.9 | 3.7 | 3.3 | 2.3 | 2.0 |
| Individuals seen at emergency care (%) | 39.1 | 33.4 | 33.5 | 31.4 | 24.4 | 19.7 | 28.8 | 25.6 | 29.8 | 26.1 | 21.5 | 20.7 | 11.7 | 11 | 3.4 | 3.0 |
| Mean emergency care visits | 2.6 | 2.3 | 2.1 | 2.1 | 2.1 | 1.9 | 2.0 | 1.8 | 2.0 | 1.8 | 1.8 | 1.7 | 1.6 | 1.5 | 1.6 | 1.6 |
| Individuals seen at mental health centres (%) | 6.6 | 4.6 | 3.9 | 2.6 | 3.5 | 2.6 | 3.4 | 2.3 | 2.7 | 1.7 | 1.7 | 1.2 | 0.7 | 0.5 | 9.0 | 10.1 |
| Mean mental health centre visits | 6.6 | 7 | 5.7 | 5.9 | 6.5 | 7.6 | 5.8 | 5.8 | 5.6 | 5.7 | 6.2 | 5.6 | 8.1 | 4.8 | 1.5 | 1.6 |
| Hospitalisation rate (per 1000 inhabitants) | 106.3 | 78.9 | 83.0 | 76.7 | 69.4 | 40.2 | 80.9 | 56.6 | 75.5 | 50.0 | 52.8 | 43.9 | 21.2 | 23.6 | 5.0 | 3.3 |
| Preventable hospitalisation rate (per 1000 inhabitants) | 5.6 | 7.5 | 2.4 | 5.3 | 2.4 | 3.1 | 2.1 | 2.7 | 2.3 | 3.3 | 1.4 | 2.0 | 0.4 | 0.5 | 13.9 | 14.7 |
| Surgical hospitalisation rate (per 1000 inhabitants) | 57.0 | 42.0 | 49.3 | 44.6 | 39.2 | 25.3 | 45.8 | 37.8 | 45.4 | 34.7 | 31.6 | 29.2 | 11.9 | 13.9 | 4.8 | 3.2 |
| Psychiatric hospitalisation rate (per 1000 inhabitants) | 6.5 | 9.7 | 2.8 | 4.6 | 3.0 | 4.1 | 2.0 | 2.9 | 1.4 | 1.7 | 1.1 | 0.9 | 1.4 | 0.8 | 5.9 | 12.6 |
| Individuals consuming medication (%) | 78.2 | 62.2 | 73.8 | 61.4 | 58.5 | 41.1 | 68.1 | 56.4 | 69.8 | 55.6 | 53.3 | 49.8 | 38.6 | 33.7 | 2.0 | 1.8 |
| Mean n° of prescriptions | 25.2 | 20.5 | 15.4 | 14.7 | 15.7 | 14.7 | 14.0 | 13.4 | 13.1 | 12.3 | 11.3 | 12.1 | 11.0 | 12.8 | 2.3 | 1.7 |
| Individuals consuming psychoactive drugs (%) | 31.1 | 18.2 | 24.7 | 13.1 | 18.8 | 10.5 | 20.8 | 11.7 | 20.2 | 10.9 | 14.2 | 9.1 | 11.6 | 6.7 | 2.7 | 2.7 |
| Individuals consuming anxiolytics (%) | 24.2 | 13.6 | 19.0 | 10.0 | 14.2 | 7.6 | 15.8 | 8.8 | 15.5 | 8.4 | 10.9 | 7 | 8.9 | 5.3 | 2.7 | 2.6 |
| Individuals consuming antidepressants (%) | 18.1 | 8.0 | 13.5 | 5.5 | 10.6 | 5.0 | 11.2 | 5.1 | 10.2 | 4.3 | 7.1 | 3.7 | 5.7 | 2.5 | 3.2 | 3.2 |
| Individuals consuming antipsychotics (%) | 4.3 | 4.6 | 2.1 | 1.9 | 1.9 | 2.1 | 1.7 | 1.5 | 1.5 | 1.3 | 1.0 | 0.9 | 0.9 | 0.5 | 4.8 | 8.6 |
ADHD, attention deficit hyperactivity disorder; RAI, active integration income; RMI, minimum integration income.
Table 4.
Results of the indicators in the over-65 year group, divided according to sex and socioeconomic level (Catalonia, 2015)
| Individuals over 65 years | Non-contributory pension | Pension <€18 000€ | Pension €18 000–€100 000 | Pension >€100 000 | Max/min | |||||
| Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | |
| Mortality rate (per 1000 inhabitants) | 33.5 | 68.7 | 29.2 | 46.4 | 21.8 | 34.4 | 19.8 | 30.9 | 1.7 | 2.2 |
| Mortality rate due to suicide (per 100.000 inhabitants) | 5.4 | 26.4 | 5.4 | 26.4 | 6.6 | 9.8 | 6.6 | 9.8 | 1.2 | 2.7 |
| Individuals with high morbidity (%) | 26.8 | 34.8 | 21.0 | 29.9 | 14.1 | 20.4 | 5.9 | 9.6 | 4.6 | 3.6 |
| Individuals seen at primary care (%) | 93.3 | 85.6 | 95.1 | 95.0 | 92.5 | 93.9 | 76.8 | 78.0 | 1.2 | 1.2 |
| Mean primary care visits | 16.0 | 14.7 | 14.0 | 14.7 | 11.4 | 11.7 | 7.5 | 7.2 | 2.1 | 2.0 |
| Individuals seen at emergency care (%) | 44.7 | 46.8 | 39.1 | 40.5 | 32.5 | 33 | 18.1 | 18.3 | 2.5 | 2.6 |
| Mean emergency care visits | 3.5 | 3.8 | 2.8 | 3.1 | 2.6 | 2.7 | 2.3 | 2.0 | 1.5 | 1.9 |
| Individuals seen at mental health centres (%) | 5.2 | 3.3 | 2.7 | 1.7 | 1.9 | 0.9 | 0.7 | 0.3 | 7.8 | 9.8 |
| Mean mental health centre visits | 5.3 | 6.2 | 4.3 | 4.4 | 4.5 | 4.0 | 4.9 | 4.1 | 1.2 | 1.6 |
| Hospitalisation rate (per 1000 inhabitants) | 299.1 | 402.6 | 258.6 | 372.9 | 188.0 | 266.9 | 82.5 | 103.6 | 3.6 | 3.9 |
| Preventable hospitalisation rate (per 1000 inhabitants) | 47.0 | 91.0 | 31.1 | 60.2 | 17.7 | 32.5 | 10 | 10.3 | 4.7 | 8.8 |
| Surgical hospitalisation rate (per 1000 inhabitants) | 131.3 | 135.5 | 135.7 | 165.4 | 105.2 | 130.9 | 39.4 | 45.2 | 3.4 | 3.7 |
| Psychiatric hospitalisation rate (per 1000 inhabitants) | 6.3 | 6.5 | 3.0 | 3.2 | 2.1 | 1.8 | 0.4 | 0.8 | 15.3 | 8.2 |
| Individuals consuming medication (%) | 94.5 | 86.9 | 95.7 | 94.8 | 93.1 | 94.0 | 77.3 | 80.1 | 1.2 | 1.2 |
| Mean no. of prescriptions | 81.0 | 73.5 | 66.7 | 65.9 | 56.8 | 57.7 | 44.3 | 50.5 | 1.8 | 1.5 |
| Individuals consuming psychoactive drugs (%) | 59.9 | 39.8 | 56.1 | 35.1 | 53.9 | 31.5 | 45.1 | 31.4 | 1.3 | 1.3 |
| Individuals consuming anxiolytics (%) | 45.9 | 29.5 | 43.9 | 26 | 42.8 | 24.3 | 37.1 | 25.7 | 1.2 | 1.2 |
| Individuals consuming antidepressants (%) | 33.2 | 15.3 | 30.3 | 14.6 | 28 | 12.1 | 21.5 | 11.4 | 1.5 | 1.3 |
| Individuals consuming antipsychotics (%) | 13.2 | 13.3 | 8.8 | 7.5 | 6.9 | 4.9 | 5.5 | 3.2 | 2.4 | 4.2 |
High morbidity
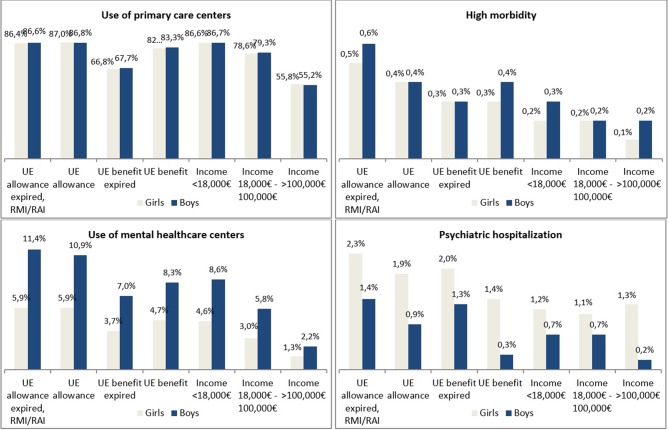
Children from lower socioeconomic level families were more likely to present high morbidity respect to children from higher socioeconomic level families (four times more in the case of girls, and 2.8 times more in the case of boys) (table 3, figure 1). In the 15–64 year age group, high morbidity was more than eight times more frequent in both lower socioeconomic level women and men, with respect to their higher socioeconomic level counterparts. For the 65 years and older age group, high morbidity was 4.6 times more likely in women and 3.6 times more likely in men of lower socioeconomic level, with respect to their higher socioeconomic level counter-parts.
Figure 1.
Result of selected indicators in the under-15 group, by sex and socioeconomic level (Catalonia, 2016).
Mortality
For the under 65 years age group, men of lower socioeconomic level had a mortality rate almost four times greater than those with incomes above €100 000 (2.4 vs 0.6 per 1000 inhabitants, respectively) (table 2). For the 65 years and older age group, the mortality rate for women of the lower socioeconomic level group was 1.5 times higher than for the group of higher socioeconomic level (33.5 vs 19.8 per 1000 inhabitants); for men, the rate was twice as high. For the 55–64 years age group, individuals in employment had similar values to the under 65 years age group, while pensioners had values more similar to those in the 65 years and older age group.
In relation to mortality due to suicide, in the under 65 years age group, men who did not work had rates twice as large as those with an annual income of more than €18 000. In the 65 years and older age group, men with an income of less than €18 000 were 2.7 times more likely to commit suicide than those with incomes above €18 000 (table 2).
Primary care
Children from lower socioeconomic level families were 1.6 times more likely to attend primary care than those from higher socioeconomic level families (mean number of visits 7.8 vs 4.2 for girls, and 7.9 vs 4.4 for boys) (table 3, figure 1). In the 15–64 years age group, lower socioeconomic level women and men were twice more likely to attend primary care than their higher socioeconomic level counterparts. They also made twice as many visits (table 2).
Emergency care
For all age groups, a higher proportion of lower socioeconomic level individuals visited the emergency department with respect to their higher socioeconomic level counterparts. The number of visits was also higher for the lower socioeconomic level individuals: for example, in the 65 years and older age group, 44.7% of women and 46.8% of men of a lower socioeconomic level used the emergency care services (with means of 3.5 and 3.8 visits per year, respectively), while among people with a higher socioeconomic level, 18.1% of women and 18.3% of men used emergency care (with means of 2.3 and 2.0 visits per year, respectively) (table 4).
Mental healthcare centres
Children from lower socioeconomic level families attended mental health centres much more frequently than those of higher socioeconomic level families: 4.4 times more for girls, and 5.1 for boys (figure 1). For the 15–64 years age group, these values rose by 9.0 times for women and 10.1 for men, and for the 65 years and older age group by 7.8 and 9.8 times, respectively (table 2). The differences with regard to the number of visits for both sexes and all age groups were small.
Individuals of the 55–64 years age group with a non-contributory pension or a pension below €18 000 made more visits for mental health centres than the active population (online supplementary table 2).
At all socioeconomic levels, and especially at the lowest, women made more visits to mental health centres than men.
Hospitalisation
Children hospitalisation rate was 3.4 times higher for girls of lower socioeconomic level families with respect to the rate of girls of higher socioeconomic level families. This ratio was 2.2 times higher for boys (table 2). The values were very similar to the rate of surgical hospitalisation. For the other categories, both rates were higher for men respect to women, except for the 15–64 years age group (table 2).
Potentially preventable hospitalisations
For the 15–64 years age group, the potentially preventable hospitalisation rate was far higher for individuals of a lower socioeconomic level with respect to their higher socioeconomic level counterparts: 13.9 times higher for women and 14.7 times higher for men (table 2). Pensioners aged 55–64 years of both sexes had a much higher rate of potentially preventable hospitalisations than the active population of the same age group (online supplementary table 2 and supplementary table 3). For the 65 years and older age group, notable differences were recorded between sexes and between socioeconomic levels.
Psychiatric hospitalisation
Regarding children, the rate of psychiatric hospitalisation for girls of low socioeconomic level families was 6.8 times higher than for girls of higher socioeconomic level families (figure 1). For the 15–64 years age group of low socioeconomic level, the rate was 5.9 times higher for women and 12.6 times higher for men (table 2) with respect to their higher socioeconomic level counterparts. For the 65 years and older age group, the rate was 15.3 times higher for women and 8.2 times higher for men (table 4).
Consumption of prescription drugs
For children and the 15–64 years age group, twice as many people of lower socioeconomic level had been prescribed drugs.
Psychoactive drug use
Children of lower socioeconomic level families were three times as likely to consume psychoactive drugs respect to their higher socioeconomic level counterparts. Girls were more than four times as likely to consume anxiolytics, and boys were more than four times as likely to consume antipsychotics. Children of a lower socioeconomic level families had a higher consumption of attention deficit hyperactivity disorder (ADHD) medication than those of the highest socioeconomic level families. Boys consumed more than twice as many ADHD drugs with respect to girls (table 3).
For the 15–64 years age group and among the 65 years and older age group, the consumption of psychoactive drugs in both sexes was the greatest for the lower socioeconomic status individuals (table 2).
Discussion
A socioeconomic gradient was observed in almost all the variables analysed in both sexes and in all age groups: that is, in health status and also in the use of healthcare services and consumption of prescription drugs. The gradient was small (though present) in primary and emergency care, moderate in consumption of prescription drugs, higher in hospitalisations and much higher in mental health and preventable hospitalisations. In general, the gradient was noticeable from childhood onwards, reaching its peak for the 15–64 years age group, and then falling again for those aged 65 years and older.
With regard to gender, males had higher rates of mortality, mortality due to suicide, more complex morbidity, more hospitalisations and increased use of ADHD medication. In contrast, females attended mental health centres more frequently and consumed more psychoactive drugs, with the exception of psychiatric hospitalisations and antipsychotic consumption. Males and females made similar use of primary and emergency care. The socioeconomic gradient for the different age groups was quite similar for both.
Since the publication of the Black Report in 1980, social inequality in health has established itself as a major issue in all European national health systems, and reducing this inequality is seen as a matter of equity and social justice.13 However, Organisation for Economic Co-operation and Development countries continue to present large disparities in health, including, for example, significant differences in life expectancy between people with the highest and lowest levels of education.18 To reduce the steepness of this social gradient, action must be taken at a scale and intensity proportionate to the level of disadvantage (‘proportionate universalism’, to use the term coined in the Marmot review13). Measures to reduce health inequalities will benefit society in many ways, since these inequalities cause losses in productivity, reduce tax revenue, increase welfare payments and raise treatment costs.13 19
Gender-based studies of inequalities in healthcare have traditionally been conducted in parallel to socioeconomic studies, but it is very important to bear in mind that these two factors of inequality act simultaneously.20 In Spain, there are major gender inequalities in working conditions and in occupational health, which are influenced by people’s socioeconomic level21; thus, in the current socioeconomic context, women represent a particularly vulnerable group.
The impact of the economic crisis on the mental health of the paediatric population in Catalonia is reflected in an increase in the number of children and adolescents making use of mental health services and an increase in serious diagnoses.22
Indeed, the most striking results of the paper refer to children: their health status is deeply affected by the socioeconomic level of their parents. There is increasing scientific evidence, both from biology and from the social sciences, of the importance of the first years of life (including in utero exposure) in the formation of the capacities that promote well-being throughout the life cycle.23 Childhood is also a structural transmitter of inequalities,24 25 in terms of both health and socioeconomic level26; naturally, children are affected by their socioeconomic environment,27 and disadvantages in this area are particularly hard to overcome.28 This paper adds empirical data supporting this evidence.
The greater use of healthcare services among the more disadvantaged shows that the public health system is responding to the differences in the general public’s state of health. Nevertheless, there are two important points to make here. First, since it is not possible to adjust the analysis according to the needs of each individual, we cannot determine whether the gradient observed in the use of services should be greater, since there is evidence pointing out that people with lower socioeconomic levels have more access difficulties, for example, quite clearly, to preventive services.29
Second, we cannot be sure that the gradient observed in the public healthcare services is maintained throughout the health system as a whole, since little is known about the use of private healthcare services.30 31 Actually, some studies have shown that specialised outpatient care is used more frequently by the better-off classes.30 31
When interpreting the data, we should bear in mind the differences in the numbers of individuals referred to in each of the indicators and the age and sex groups analysed. It should also be noted that in the case of children from 0 to 4 years, only 55% of the population was included, while for the other age groups the proportion was between 70% and 95% (online supplementary table 1).
For many variables in this study, the gradient between the different socioeconomic levels was not linear. This point has been noted in previous research, in which inequalities were more noticeable up to an income of approximately €30 000 per year, after which point the effect began to fall off.32 In the current study, membership of the group with an income of €18 000 or more entailed a significant improvement in health indicators.
Like all studies, this appraisal is not without its limitations. Apart from the ones mentioned above, we should also stress that individuals are assigned to a particular medication copayment group on the basis of the income stated in individual income tax declarations. In the case of individuals who make joint tax declarations or individuals in the same family unit with different incomes, this assessment procedure may introduce a bias; however, no better information is available.
On the positive side, this paper analyses individual information from almost the entire population of Catalonia and is an example of the strength of the reuse of administrative data for research purposes.
Given the multiple impacts of the crisis, the attempts to design public policies for mitigating its effects must be intersectorial33 and must act on the determinants of health. Educational levels of individuals are crucial for their employment, earnings and health status, for social and health mobility across generations, and also for protecting them against the economic and social risks brought on by the crisis.34 35 In addition, it is important to design policies for the most vulnerable sectors of the population such as children, women and groups that already presented greater inequalities prior to the crisis. Gender policies and integration policies are clear examples. As an example of the different actions that are currently taking place in Catalonia, the second edition of the PINSAP (Health in All Policies Intersectorial Plan, according to the Catalan acronym), 2017–2020, will implement the planned actions in all the territory through territorial councils, with the collaboration of all Government departments, local entities, healthcare providers, academia, professional colleges and other associations, as well as the third sector.36
What is already known on this subject.
The economic crisis of recent years has revived the interest in monitoring health inequalities.
What this study adds?
This paper analyses inequalities in health status, examining the use of public healthcare services and consumption of prescription drugs in the entire population of Catalonia using individual data of 7.5 million residents.
A socioeconomic gradient was observed in almost all the variables analysed in both sexes and in all age groups. However, the most striking results refer to children: their health status is deeply affected by the socioeconomic level of their parents.
Policy implications.
To address this situation, new policies on health and other areas (ie, education, employment, gender equality and integration) are required, especially those that have an impact on early years.
Acknowledgments
We are grateful to Marisol Rodríguez (University of Barcelona) and Lluis Bohigas for their comments on this paper. We also thank Marc Boher (AQuAS), Isabel Garcia Hernández (Department of Employment, Social Affairs and Families), Carles Vicenç Pérez (CatSalut), Joan MV Pons (AQuAS), Emili Vela (CatSalut) and the staff in charge of maintaining the central register of insured persons and the Citizen Service Management (CatSalut).
Footnotes
Contributors: AG-A generated the idea for the paper, and DR-M and CC prepared an analytical plan with DR-M, CC, MM and NMB conducting all data analyses. All the authors contributed to the interpretation of the results. AG-A and DR-M prepared the first draft of the manuscript on which all coauthors commented.
Funding: This work was not supported by any body other than the authors’ employer.
Competing interests: None declared.
Patient consent: Not required.
Provenance and peer review: Commissioned; externally peer reviewed.
Data sharing statement: Data cannot be made publicly available. Requests for data should be sent to AG-A.
References
- 1.Observatori del Sistema de Salut de Catalunya. Efectes de la crisi econòmica en la salut de la població de Catalunya. Anàlisi territorial. Barcelona: Agència de Qualitat i Avaluació Sanitàries de Catalunya. Departament de Salut. Generalitat de Catalunya. 2015. http://observatorisalut.gencat.cat/web/.content/minisite/observatorisalut/ossc_crisi_salut/Fitxers_crisi/Salut_crisi_informe_2015.pdf (accessed 21 Mar 2018).
- 2.Thomson S, Figueras J, Evetovits T, et al. Economic crisis, health systems and health in Europe. Impact and implications for policy. Copenhagen: European Observatory on Health Systems and Policies. WHO Regional Office for Europe, 2014. [PubMed] [Google Scholar]
- 3.Rivadeneyra-Sicilia A, Minué Lorenzo S, Artundo Purroy C, et al. Lecciones desde fuera. Otros países en ésta y otras crisis anteriores. Informe SESPAS 2014. Gac Sanit 2014;28(Supl 1):12–17. 10.1016/j.gaceta.2014.03.006 [DOI] [PubMed] [Google Scholar]
- 4.Lopez Bernal JA, Gasparrini A, Artundo CM, et al. The effect of the late 2000s financial crisis on suicides in Spain: an interrupted time-series analysis. Eur J Public Health 2013;23:732–6. 10.1093/eurpub/ckt083 [DOI] [PubMed] [Google Scholar]
- 5.Librero J, Segura A, Beatriz LV. Suicides, hurricanes and economic crisis. Eur J Public Health 2014;24:183 10.1093/eurpub/ckt167 [DOI] [PubMed] [Google Scholar]
- 6.Bartoll X, Palència L, Malmusi D, et al. The evolution of mental health in Spain during the economic crisis. Eur J Public Health 2014;24:415–8. 10.1093/eurpub/ckt208 [DOI] [PubMed] [Google Scholar]
- 7.Novoa AM, Ward J, Malmusi D, et al. How substandard dwellings and housing affordability problems are associated with poor health in a vulnerable population during the economic recession of the late 2000s. Int J Equity Health 2015;14:120 10.1186/s12939-015-0238-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jiménez-Martín S, Viola A. El sistema de salud en España en perspectiva comparada. Primer Informe Observatorio de Sanidad Fedea. Madrid: Observatorio de la Sanidad Fedea, 2014. [Google Scholar]
- 9.La salut a Barcelona. Barcelona: Agència de Salut Pública de Barcelona, 2014:2015. [Google Scholar]
- 10.Cortès-Franch I, González López-Valcárcel B. Crisis económico-financiera y salud en España. Evidencia y perspectivas. Informe SESPAS 2014. Gac Sanit 2014;28(Supl 1):1–6. 10.1016/j.gaceta.2014.03.011 [DOI] [PubMed] [Google Scholar]
- 11.Dávila-Quintana CD, Lopez-Valcarcel BG. Secuelas a largo plazo de la crisis económica y desigualdades sociales en salud. Revista Española de Salud Pública 2014;88:187–90. 10.4321/S1135-57272014000200002 [DOI] [PubMed] [Google Scholar]
- 12.The impact of the economic downturn and policy changes on Health inequailites in London. London: UCL Institute of Health Equity, 2012. [Google Scholar]
- 13.Fair Society, Healthy Lives. The marmot review. strategic review of health inequalities in England post-2010. London: UCL Institute of Health Equity, 2010. [Google Scholar]
- 14.Goldblatt PO. Moving forward monitoring of the social determinants of health in a country: lessons from England 5 years after the Marmot Review. Glob Health Action 2016;9:29627 10.3402/gha.v9.29627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.García-Armesto S, Begoña Abadía-Taira M, Durán A, et al. Spain: Health system review. Health Syst Transit 2010;12:1–295. [PubMed] [Google Scholar]
- 16.Prestaciones por desempleo. Subsidios por desempleo. Madrid: Servicio Público de Empleo Estatal (SEPE). Ministerio de Empleo y Seguridad Social. Gobierno de España. 2017. https://www.sepe.es/contenidos/que_es_el_sepe/publicaciones/pdf/pdf_prestaciones/cuadr_subsidio.pdf (accessed 21 Mar 2018).
- 17.Prestaciones por desempleo. Prestación por desempleo de nivel contributivo. Protección por desempleo. Madrid: Servicio Público de Empleo Estatal (SEPE). Ministerio de Empleo y Seguridad Social. Gobierno de España. 2017. https://www.sepe.es/contenidos/que_es_el_sepe/publicaciones/pdf/pdf_prestaciones/folleto_pres_desemp.pdf (accessed 21 Mar 2017).
- 18.OECD. Health at a Glance 2015: OECD Indicators. Paris: OECD Publishing, 2015. [Google Scholar]
- 19.Cookson R. Justice and the NICE approach. J Med Ethics 2015;41:99–102. 10.1136/medethics-2014-102386 [DOI] [PubMed] [Google Scholar]
- 20.Borrell C, García-Calvente MdelM, Martí-Boscà JV. La salud pública desde la perspectiva de género y clase social. Gac Sanit 2004;18:2–6. 10.1157/13062243 [DOI] [PubMed] [Google Scholar]
- 21.Campos-Serna J, Ronda-Pérez E, Artazcoz L, et al. Desigualdades de género en salud laboral en España. Gac Sanit 2012;26:343–51. 10.1016/j.gaceta.2011.09.025 [DOI] [PubMed] [Google Scholar]
- 22.Quiroga V, Guasch C. L’afectació de salut mental en la població infantil i adolescent en situació de risc a Catalunya. Educació Social. Revista d’Intervenció Socioeducativa 2014;57:135–53. [Google Scholar]
- 23.Heckman JJ. The developmental origins of health. Health Econ 2012;21:24–9. 10.1002/hec.1802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Desheredados. Desigualdad infantil, igualdad de oportunidades y políticas públicas en España. Save the Children. 2017. https://www.savethechildren.es/publicaciones/desheredados (accessed 21 Mar 2018).
- 25.Goldblatt P, Siegrist J, Lundberg O, et al. Improving health equity through action across the life course: Summary of evidence and recommendations from the DRIVERS project. (Report produced as part of the ‘DRIVERS for Health Equity’ project). Brussels: EuroHealthNet, 2015. [Google Scholar]
- 26.Flores M, García-Gómez P, Zunzunegui M-V. Crisis económica, pobreza e infancia. ¿Qué podemos esperar en el corto y largo plazo para los “niños y niñas de la crisis”? Informe SESPAS 2014. Gac Sanit 2014;28:132–6. 10.1016/j.gaceta.2014.02.021 [DOI] [PubMed] [Google Scholar]
- 27.Flores R. La transmisión intergeneracional de la pobreza: factores, procesos y propuestas para la intervención. Madrid: Fundación Foessa, 2016. [Google Scholar]
- 28.García-Altés A, Ortún V. Funcionamiento del ascensor social en España y posibles mejoras. Informe SESPAS 2014. Gac Sanit 2014;28:31–6. 10.1016/j.gaceta.2014.03.010 [DOI] [PubMed] [Google Scholar]
- 29.Urbanos-Garrido R. La desigualdad en el acceso a las prestaciones sanitarias. Propuestas para lograr la equidad. Gac Sanit 2016;30(Suppl 1):25–30. 10.1016/j.gaceta.2016.01.012 [DOI] [PubMed] [Google Scholar]
- 30.Rodríguez M, Stoyanova A. The effect of private insurance access on the choice of GP/specialist and public/private provider in Spain. Health Econ 2004;13:689–703. 10.1002/hec.832 [DOI] [PubMed] [Google Scholar]
- 31.Fjær EL, Balaj M, Stornes P, et al. Exploring the differences in general practitioner and health care specialist utilization according to education, occupation, income and social networks across Europe: findings from the European social survey (2014) special module on the social determinants of health. Eur J Public Health 2017;27:73–81. 10.1093/eurpub/ckw255 [DOI] [PubMed] [Google Scholar]
- 32.Costa-Font J, Hernandez-Quevedo C, Sato A. A Health ’Kuznets' Curve'? Cross-Sectional and Longitudinal Evidence on Concentration Indices'. Soc Indic Res 2018;136:439–52. 10.1007/s11205-017-1558-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pla Interdepartamental de Salut Pública (PINSAP). Barcelona: Agència de Salut Pública de Catalunya. Generalitat de Catalunya. http://salutpublica.gencat.cat/ca/sobre_lagencia/pinsap/ (accessed 21 Mar 2018).
- 34.Stringhini S, Carmeli C, Jokela M, et al. LIFEPATH consortium. Socioeconomic status and the 25×25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1·7 million men and women. Lancet 2017;389:1229–37. 10.1016/S0140-6736(16)32380-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hidalgo-Hidalgo M, Iturbe-Ormaetxe I. Long-run effects of public expenditure on poverty. The Journal of Economic Inequality 2018;16:1–22. 10.1007/s10888-017-9360-z [DOI] [Google Scholar]
- 36.Pla Interdepartamental i Intersectorial de Salut Pública. PINSAP 2017-2020. Barcelona: Agència de Salut Pública de Catalunya. Generalitat de Catalunya. http://salutpublica.gencat.cat/web/.content/minisite/aspcat/sobre_lagencia/pinsap/01Els_Plans/PINSAP_2017-2020/PINSAP_2017-2020-Complet.pdf (accessed 21 Mar 2018).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jech-2018-210817supp001.pdf (87.1KB, pdf)
jech-2018-210817supp002.pdf (204.3KB, pdf)