Abstract
Background
Home care workers (HCWs), which include home health aides and personal care aides, are increasingly used by heart failure (HF) patients for post-acute care and long-term assistance. Despite their growing presence, they have largely been left out of HF research and interventions. This systematic review was aimed to 1) describe utilization patterns of HCWs by adults with HF, 2) examine the effect of HCWs on HF outcomes, and 3) review HF interventions that involve HCWs.
Methods
Five electronic databases (Ovid MEDLINE, Ovid EMBASE, Cochrane Library [Wiley], CINAHL [EBSCO], and AgeLine [EBSCO]) were searched from inception through August 4, 2017. The yield was screened using prespecified inclusion and exclusion criteria. Two authors independently reviewed references and a third reviewer acted as an arbitrator when needed. Data were extracted from articles that met the inclusion criteria. The Downs and Black checklist was used for quality assessment. Due to study heterogeneity, a narrative synthesis was conducted.
Results
Of the 7,032 studies screened, 13 underwent full-text review, and six met the inclusion criteria. Two descriptive studies found that adults with HF who live alone and have functional and cognitive deficits utilize HCWs. While three retrospective cohort studies examined the association between having an HCW post-HF hospitalization and readmission rates, their findings were conflicting. One quasi-experimental study found that an HCW-delivered educational intervention improved HF patients’ self-care abilities. Overall, despite some significant findings, the studies assessed were of poor-to-fair quality (Downs and Black score range: 10–16 [28 total points]), with most lacking methodological rigor.
Conclusion
Although HCWs are quite common, the literature on these paraprofessionals in HF is limited. Given the paucity of research in this area and the low quality of studies reviewed here, additional research is warranted on the potential role of HCWs in HF self-care and on outcomes among adults with HF.
Keywords: home care workers, congestive heart failure, home health care, systematic review, health services research, quality of care, home health aides
Plain language summary
Home care workers (HCWs), which include home health aides and personal care aides, represent one of the fastest growing sectors of the health care industry and US economy and are increasingly being utilized by home-dwelling adults with heart failure (HF) for long-term assistance and post-hospitalization care. In contrast to physicians or visiting nurses who see HF patients for short periods of time, HCWs are with HF patients on a daily or near-daily basis and sometimes up to 24 hours a day. As such, they assist with many aspects of HF self-care such as meal preparation, taking vital signs, assisting with medication compliance, and accompanying patients to medical appointments. Yet, the role of HCWs in HF has not been characterized. This systematic review is the first to determine the effect of HCWs on HF patient outcomes. Five electronic databases were searched. Study quality was assessed with the Downs and Black checklist. Of the 7,032 studies screened, six met inclusion criteria. Among the six studies, five were observational and one was quasi-experimental. Studies were of poor-to-fair quality, often lacking methodological rigor. While HCWs in HF are common, the literature on them is limited. Additional research is warranted to understand their role in HF management and their effect on health outcomes.
Background
Heart failure (HF) is a complex, chronic disease that requires a high degree of self-care and frequent contact with the health care system.1,2 HF patients often have multiple chronic conditions, functional and cognitive impairments,3 and sensory deficits.4,5 As such, many rely on informal (family) and formal (paid) caregivers to help them manage their disease and navigate the health care system.6–10
Formal caregivers are increasingly being used by adults with HF. With the implementation of Medicare payment reforms, including financial penalties for 30-day readmissions, a growing number of adults hospitalized for HF are now discharged with home health care (HHC).11–13 HHC offers short-term skilled nursing, physical and occupational therapy, speech and language therapy, medical social work, and care from home care workers (HCWs).11–13
HCWs, which include home health aides (HHA) and personal care aides (PCA), are one of the fastest growing sectors of the health care industry and US economy.14–16 While their roles differ, with HHAs receiving more specialized training and having a greater scope of tasks than PCAs,17–19 both provide physical and emotional support to HF patients.17 HCWs are with patients on a daily or near-daily basis17,20 and are often involved with key aspects of HF maintenance and management including meal preparation, weight and fluid monitoring, medication compliance, and transportation to medical appointments. These interactions may affect outcomes for patients with HF, but the exact influence of HCWs in the context of HF has not been studied.
To fill this gap, we conducted a systematic review of the literature in order to 1) describe utilization patterns of HCWs by adults with HF, 2) examine the effect of HCWs on HF outcomes, and 3) review HF interventions that involve HCWs.
Methods
This systematic review is reported in line with the PRISMA guidance21 and was registered with PROSPERO (CRD42017077405).
Search strategy
A medical librarian (DD) performed comprehensive literature searches of Ovid MEDLINE (in-process and other non-indexed citations and Ovid MEDLINE from 1946 to present), Ovid EMBASE (from 1974 to present), Cochrane Library (Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials [CENTRAL], and Cochrane Methodology Register), CINAHL (EBSCO), and AgeLine (EBSCO) from inception to August 4, 2017. The first search was conducted in Ovid MEDLINE. Subject headings and key words were adapted for the other databases. No restrictions of language, publication date, or article type were applied. Additional records were identified by reviewing reference lists and employing the “Cited by” and “View references” features in Scopus of the included studies. The full search strategy for Ovid MEDLINE is available in Supplemental material S1.
Inclusion and exclusion criteria
This review was limited to observational studies, quasi-experimental studies, and randomized controlled trials (RCTs). To be included, studies must have pertained to community-dwelling adults (≥18 years of age) with HF and focused on HCWs, including HHAs, PCAs, and home health attendants. Only studies that were published in English and conducted in the United States were included (Table 1).
Table 1.
Systematic review inclusion criteria
| Inclusion criteria |
|---|
| 1. Studies of community-dwelling adults (age ≥18 years) with heart failure. |
| 2. Studies focusing on HCWsa or including HCW services as independent variables in models and analyses. |
| 3. Studies occurring in the United States. |
| 4. English articles. |
| 5. Peer-reviewed, full articles. |
| 6. RCTs, observational studies (descriptive, cross-sectional, retrospective cohort, prospective cohort), and quasi-experimental studies. |
Notes:
HCWs may be called home health aides, home health attendants, personal care aides, or home health care paraprofessionals.
Abbreviations: HCW, home care workers; RCTs, randomized control trials.
Qualitative studies, case reports, editorials, reviews, doctoral dissertations, and scientific meeting abstracts were excluded. Studies that focused on home health nurses were excluded, as were those in which HF patients resided in nursing homes, long-term care centers, and acute rehabilitation centers.
Selection of studies
Figure 1 shows the PRISMA flow diagram of reviewed and included studies (Figure 1). All studies identified following the database search were uploaded to the Web-based systematic review software package Covidence (https://www.covidence.org/). First, title and abstract review of all studies were completed independently by two authors (ALS and PBKL). Disagreements were discussed and a third reviewer helped to resolve the discrepancies (MRS). A record was kept of all the studies excluded and the reason for exclusion in Covidence. All of the studies that met the inclusion criteria (13) went through a full-text screening process by the three authors independently (ALS, PBKL, and MRS), and any disagreements on the eligibility of the studies were reviewed by a fourth author (DD).
Figure 1.
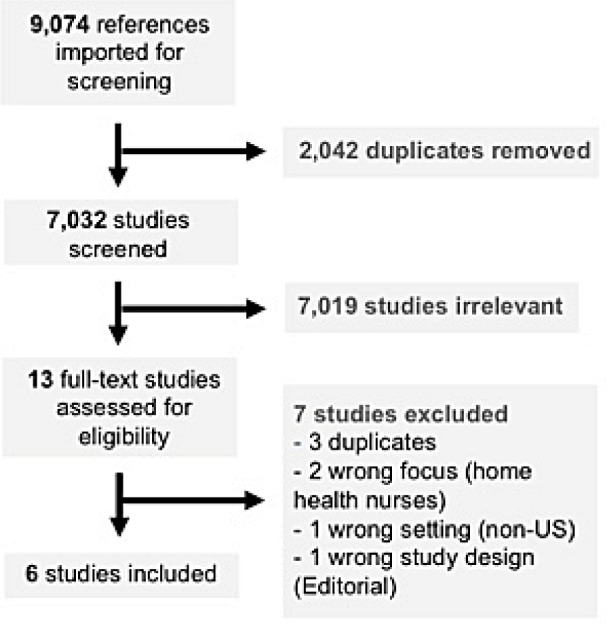
PRISMA study flow diagram.
Notes: PRISMA flow diagram of reviewed and included studies. The figure was created with web-based systematic review software package Covidence (https://www.covidence.org/).
Data extraction
Data from the included studies were extracted independently by three authors using a data extraction template. Data extracted from the studies included lead author, study title, year published, study population (design and year/duration) study type, study objective, primary outcome, intervention/control group (if applicable), main result(s), and limitations (Table 2). The review team resolved any disagreements regarding study eligibility through group discussion.
Table 2.
Characteristic of included studies
| First author/Year | Title/Journal | Study design and population | Study objective(s) | Primary outcome(s) | Main results | Limitations | Quality |
|---|---|---|---|---|---|---|---|
| Anderson et al 199827 | Home care utilization by CHF patients: a pilot study, in Public Health Nursing | Type: Descriptive study Design: Chart review of 1 year of home care patient records. Inclusion criteria: Primary diagnosis of CHF, ≥2 home visits, care reimbursed by Medicare, ≥65 years of age. Study population: Of the 80 records that met inclusion criteria, 40 were randomly selected to be included in the study. | To determine utilization patterns of CHF patients admitted and discharged from a not-for-profit HHA. | HHC utilization patterns of older adults with HF. | The majority of participants were 75–84 years old, white, female, and widowed. Men had more functional limitations and more home health aide visits than women; however, differences were not tested for statistical significance. During a HHC episode, 43% of patients were admitted to the hospital at least once. | Small sample Single center Single agency | 11 |
| Moulton et al 199828 | Utilization of HHC services by elderly patients with HF, in Home Health Care Management & Practice | Type: Descriptive study Design: Convenience sample of 104 patients admitted to a large Medicare-certified, not- for-profit HHC agency during a 1-year period. Inclusion criteria: ≥65 years of age and a diagnosis of HF. | To determine the health profile and utilization patterns of home care among older adults with HF. To identify health outcomes, following the receipt of home care serves, in this patient population. | Demographic and clinical characteristics of older adults with HF receiving home care and utilization patterns of home care services in this population. Health outcomes, following the receipt of HHC. | Participants had a mean (SD) age of 79 (7.9) years; the majority were female and widowed. Those with HHA were more functionally impaired than those without. Following home care, 72% were discharged home, 12% were rehospitalized, 5% were discharged elsewhere. | Small sample Single agency | 10 |
| Hoskins et al 199929 | Predictors of hospital readmission among the elderly with CHF, in Home Healthcare Nurse | Type: Retrospective cohort Design: Chart review of 117 randomly selected patients who were discharged from a nonprofit Medicaid/Medicare- certified home health agency to home (n=85) or readmitted to the hospital (n=32). Inclusion criteria: ≥65 years of age, insured by Medicare, HF diagnosis. | To determine differences between adults with HF who had HHC and were discharged home vs those readmitted. | Readmission to the hospital vs remaining at home, after receipt of home health services. | The majority of participants were 75–84 years old, female, and White. More than half were widowed and 42% considered themselves the primary caregiver. Seventy-three percent were discharged home and 27% were readmitted. Those discharged home had more home health aide visits compared with those who were readmitted; however, this difference was not statistically significant. | Small sample Single agency Analyses did not adjust for patients’ severity of illness or caregiving needs. Models were not included in the paper. | 12 |
| Russell et al 201130 | Implementing a transitional care program for high-risk HF patients: findings from a community-based partnership between a certified home health care agency and regional hospital, in Journal of Healthcare Quality | Type: Retrospective cohort Design/Inclusion: Chart review of 447 high-risk HF patients who received home care services post discharge from a nonprofit hospital. Two hundred twenty-three patients who received a transitional care program were compared to 224 patients who received usual home care from the same HHC agency. | To compare the odds of 30-day readmission for transitional care program recipients to similar patients receiving usual home care during the year prior to the pilot program. | 30-day readmission, from the beginning of the HHC episode. | Participants had a mean age of 79.9 (10.7) years, 56% were female, 57% were white, and 30.2% received HHA services. Twenty-eight percent were rehospitalized within 30 days of starting home services. The adjusted odds ratio for 30-day readmitted among those in the intervention group was 0.57 (P<0.01). HHA use was not associated with readmission. | Readmitted patients had more chronic conditions, making it difficult to draw conclusions about the effect of HHAs on readmission. | 15 |
| Madigan et al 201231 | Re-hospitalization in a national population of HHC patients with HF, in Health Services Research | Type: Retrospective cohort Design: Analysis of a national sample of 74,580 home health care patients from 2005. Inclusion: Primary diagnosis of HF, HHC paid by Medicare. | To determine if patient, HHC agency, and geographic factors were associated with 30-day readmission and time to readmission. | 30-day readmission. | Twenty-six percent of the study participants were readmitted within 30 days. Receiving any HHA visit (OR: 1.07 [1.02, 1.12]) was associated with higher odds of readmission in multivariable analyses. Receiving any HHA visit (HR: 1.32 [1.09, 1.28]) was associated with shorter times to readmission. Patient factors influenced readmission more than geographic or agency factors. | Not all analyses were shown in the Results section. Models did not adjust for basic demographic factors. | 16 |
| Russell et al 201732 | Preparing HHA to serve as health coaches for home care patients with chronic illness: findings and lessons learned from a mixed-method evaluation of two pilot programs, in Home Health Care Management & Practice | Type: Quasi-experimental (pre–post) Design: HHAs delivered an education and support-based intervention to 32 HF patients recently discharged from a large hospital in 2014 via weekly home visits/telephone follow-up. Data were collected pre- and post intervention. Inclusion criteria: HF patients, ≥65 years of age, receiving HHC services within 30 days of discharge. | To compare patient- reported measures of self-care maintenance and QoL before and after receiving the HHA- delivered intervention. | Health-related QoL (clinically meaningful change in score on validated survey instrument ([EuroQoL 5D-5L and EuroQoL Visual Analog Scale]) Self-care maintenance (clinically meaningful change in score on validated survey instrument [Self- Care of Heart Failure Index]). | The participants had a mean age of 76.6 (13.7) years, 56.3% were female, 62.5% were non-Hispanic white, 89.5% spoke English, 46.9% lived alone, and on average, patients had limitations in 6.1 (1.1) activities of daily living. QoL scores were not significantly different after the HHA-delivered intervention. Self-care maintenance scores improved significantly after the HHA-delivered intervention (74.4 [7.1] vs 66.2 [12.1]; P=0.01) | Single hospital Single agency. Convenience sample. Poor survey response rate (high dropout rate) Lacking external control group. | 13 |
Abbreviations: CHF, congestive heart failure; HF, heart failure; HHA, home health agency; QoL, quality of life; HHC, home health care; HHA, home health aides.
Assessment of quality
The studies included in this systematic review were evaluated using a quality index proposed by Downs and Black (DB), which examines five subscales that measure reporting, external validity, internal validity (two subscales on bias and confounding), and power.22 The DB scale is a 27-item checklist that was developed to assess quality in clinical trials and was modified, based on previous systematic reviews, to accommodate the characteristics of observational studies (Table S1).23–25 The checklist has a good interrater (r=0.75) and test–retest (r=0.88) reliability, as well as high internal consistency (KR-20=0.89).22 The maximum score for the modified checklist was 28 since all individual items were rated as yes (=1), no (=0), or unable to determine (=0), with the exception of Item 5, where one could receive a maximum of 2 points. The ranges of scores were grouped into four categories: excellent (26–28 points), good (20–25), fair (15–19), and poor (≤14).24,26
Data synthesis
Following data extraction and quality assessment, consideration was given to the appropriateness of conducting a meta-analysis. As the studies were too heterogeneous to combine statistically, the data were synthesized qualitatively.
Results
Study selection
The PRISMA flowchart is presented in Figure 1. The literature search yielded 9,074 articles, from which 2,042 duplicates were removed, leaving 7,032 articles for review. Of these, 7,019 were excluded based on title and abstract review. Among the 13 full-text articles reviewed, 7 were excluded for various reasons (duplicates [n=3], study population [n=2], study location [n=1], and study design [n=1]). Overall, the study reports on six articles.
Description of included studies
Characteristics of the six included studies are detailed in Table 2. The studies were published from 1998 to 2017 in journals that focused on home care and management, nursing, and health services research. The majority (n=5) of the included studies were observational,27–31 of which two were descriptive in nature27,28 and three used retrospective cohort designs.29–31 One study was a quasi-experimental study with pre- and post-intervention design.32 There were no RCTs. The majority of patients in these studies were ≥65 years of age and were non-Hispanic white. All six studies focused on HHAs without mention of PCAs or other types of paid HCWs.
Risk of bias
Overall, the quality of the studies was fair to poor, with DB quality scores ranging from 10 to 16 and with a mean score of 12.8 (SD 2.3); four studies27–29,32 were of poor quality and two30,31 were of fair quality (Table S2). The majority (n=5) of studies27–30,32 utilized small samples from one home care agency or one hospital, and thus their results lacked external validity. One study was missing outcome data32 and several were missing demographic and clinical information on study participants. Two studies27,28 found interesting trends but did not perform statistical analyses to discern whether these trends were statistically significant. Finally, reverse causality limited the validity and generalizability of the three studies that examined the effect of HCWs on readmission rates, since they did not attempt to adjust for HF patients’ severity of disease or their caregiving needs.
Utilization patterns of HCW by adults with HF
Two studies (Anderson et al27 and Moulton et al28) characterized the utilization of HHC services, including HHAs, among adults with HF. Both were descriptive in design, collected data via chart review, derived study samples from single home care agencies, and included HF patients who were ≥65 years of age and insured by Medicare. Data from both studies suggested that HF patients who utilized HHAs were older adults with functional limitations, lived alone, or had an unmet caregiving needs. Notably, Anderson et a.27 found that men had more functional limitations and used HHAs more often than women, although this difference was not tested for statistical significance.
HCW and hospital readmission in HF
Three studies evaluated the effect of having an HHA on the risk of hospital readmission among adults with HF.29–31 All used retrospective cohort designs, although the sample size varied greatly among the three studies.
A study by Hoskins et al29 included 117 patients who received HHC from one large, nonprofit, Medicare/Medicaid-certified home care agency following an HF hospitalization.29 Overall, 27% of the sample were readmitted. Those who remained at home had more HHA visits (mean[SD] 19[17.5]) compared with those who were readmitted (14[11.9]), but this difference was not statistically significant. Instead, patients’ number of prior hospitalizations and their medication burden were significantly associated with greater readmission risk.
Russell et al30 examined the effect of a transitional care program on readmission risk among patients discharged home with home care services following an HF hospitalization from a nonprofit medical/surgical hospital.30 A total of 223 patients received the transitional care program (n=223) while 224 medically similar patients received usual home care services. Overall, 28% of patients were readmitted to the hospital within 30 days. Patients who received the program were 43% less likely to be readmitted to a hospital compared with those who received usual home care services, after adjusting for demographic, clinical, and home care characteristics (adjusted OR 0.57 [95% CI 0.38, 0.87]). Notably, there were no differences in readmission by HHA use.
Madigan et al31 used a national sample of 74,580 HHC patients with HF who received home care services in order to identify which patient, geographic, and home care agency factors were associated with 30-day readmissions.31 Overall, the 30-day readmission rate was 26%. Patient-level factors influenced readmission risk the most, when compared with geographic and home care agency factors. Receiving any HHA visit was independently associated with higher likelihood of readmission (OR 1.07 [1.02, 1.12]) and shorter time to readmission (HR 1.32[1.09, 1.28]) in multivariable analyses.
HF interventions involving HCWs
A quasi-experimental study by Russell et al32 determined the effect of an HHA-delivered coaching intervention on HF patients’ self-care maintenance and quality of life (QoL).32 Participants who received home health services post discharge served as their own controls pre and post intervention. HHAs provided weekly support and HF self-care information to patients during home visits and telephone calls. Health-related QoL and HF self-care were assessed with validated instruments.33–35 While QoL scores did not differ significantly, participants’ HF self-care maintenance scores, as measured by the Self-Care of Heart Failure Index,35 improved significantly (74.4 [7.1] vs 66.2 [12.1], P=0.01) after HHA coaching.
Discussion
Although HCWs frequently care for community-dwelling adults with HF in the United States, our findings demonstrate a paucity of literature that explicitly investigates HCWs in the context of HF self-care and outcomes. A few studies examined the effect of HCWs on the risk of readmission; however, the results were conflicting. Remarkably, only one study incorporated HCWs into an HF intervention. Neither of the studies mentioned PCAs, who comprise 50% of agency-employed HCWs, nor did any of the studies mention non-agency-employed HCWs, of which there are currently 8,00,000 in the United States.19,20
Because we reviewed observational and quasi-experimental studies (without RCT-level evidence) which were of fair to poor quality, our findings must be interpreted with caution. The studies that examined HCW utilization patterns utilized small and homogeneous patient populations and were conducted two decades ago. The studies that examined the effect of HCWs on hospital readmission used larger, more diverse patient samples, but were methodologically limited.36 That is, HF patients who receive HCWs at discharge are often sicker and have more caregiving needs than those who do not. Thus, without accounting for this, the association between HCWs and readmission risk cannot be carefully isolated. One study used a quasi-experimental approach to determine the effect of HCW-delivered intervention on HF patients’ self-care abilities and QoL; however, there was no control group, the sample was small, and dropout rates were high. Overall, our findings call for additional high-quality observational and experimental research to examine the role and effect of HCWs in HF.
To our knowledge, our systematic review is the first to evaluate the peer-reviewed literature on HCWs in HF. Prior reviews have examined the role and impact of other health care professionals on HF patients’ outcomes, particularly in the post-discharge period. A systematic review and meta-analysis by van Spall et al37 evaluated RCTs that examined the effect of home-based, nurse-led visits during the post-discharge period on HF patients’ health outcomes.37 Compared with usual care, nurse-led interventions offered the greatest reduction in mortality (RR 0.81 [95% CI 0.63, 1.03]) and readmission (RR 0.65 [95% CI 0.49, 0.86]). This finding is similar to reviews by Feltner et al, Philips et al, and Slyer et al, which also found post-discharge nurse-led visits in HF patients’ homes to be effective.38,39,45 Beyond the benefits of single health care professionals, studies have found that multidisciplinary team-based interventions in HF patients’ homes reduce hospitalization and readmission rates.40,41 The team members cited in these studies include nurses, advanced HF nurses, pharmacists,42,43 dieticians, physical therapists,44 social workers, primary care providers, and cardiologists.44 Notably absent from this list are HCWs, who, apart from family caregivers, spend the most amount of time with HF patients in the home.
Strengths and limitations
The strengths of our study include the rigorous literature search across several databases, using predefined search terms and strict inclusion and exclusion criteria. Additionally, quality was assessed with the DB checklist, a well-validated tool.22 Some limitations should also be noted. Given that so few quantitative studies exist in this area, our exclusion of qualitative studies may have limited our understanding of the role of HCWs in HF. Additionally, due to the heterogeneous nature of the studies, a meta-analysis was unable to be conducted.
Conclusion
We conducted this systematic review in order to describe utilization patterns of HCWs by adults with HF, examine the effect of HCWs on HF patients’ health outcomes, and review HF interventions that involve HCWs. Our findings suggest that despite their widespread use among community-dwelling adults with HF, the literature on HCWs in HF is limited. Due to the paucity of research in this area and the lack of high-quality studies reviewed here, additional and more rigorous research is warranted on the potential role of HCWs in improving QoL and decreasing avoidable health services utilization in HF.
Data sharing statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study. We have, however, provided our search strategy as this may be helpful to reviewers and readers who wish to reproduce our results (Supplemental material S1).
Supplementary materials
Supplemental material S1 Search strategy Ovid MEDLINE(R) Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R) 1946 to Present Search ran on August 4, 2017
Home Health Aides/
Home Care Services/
House Calls/
(home adj3 (aide* or care or nurse* or nursing or service* or visit* or worker* or attendant* or agencies or program or programme)).mp.
(domestic health care or domiciliary care).mp.
house call*.mp.
or/1-6
exp Heart Failure/
(heart failure or asystole or asystolia or asystoly or Cardiac asthma or cardiac arrest or cardiac backward failure or cardiac decompensation or Cardiac Edema* or Cardiac Failure or cardiac incompetence or cardiac insufficiency or cardiac stand still or Cardio Renal Syndrome* or cardiorenal syndrome* or cardiogenic shock or cardiopulmonary insufficiency or cardiorespiratory arrest or cardiorespiratory collaps or cardiorespiratory failure or cardiovascular shock or chronic heart insufficiency or circulation arrest or circulatory arrest or decompensatio cordis or diastolic dysfunction or diastolic overload or forward failure or heart arrest or heart backward failure or heart decompensation or heart incompetence or heart insufficiency or heart left ventricle outflow tract obstruction or heart right ventricle outflow tract obstruction or heart outflow tract obstruction or heart overload or heart shock or heart standstill or heart ventricle failure or high cardiac output failure or high heart output failure or high output cardiac failure or high output failure or high output heart failure or nsufficientia cardis or insufficientia ventriculi or insufficientia ventriculi cordis or low cardiac output or low heart output or myocardial failure or myocardial insufficiency or Paroxysmal Dyspnea* or PRIS or propofol infusion syndrome* or propofol related infusion syndrome* or Renocardiac Syndrome* or Reno-Cardiac Syndrome* or Reno Cardiac Syndrome* or systolic dysfunction or systolic overload or ventricular insufficiency or ventricular overload or ventricle insufficiency or ventricle overload).mp.
or 9
and 10
Table S1.
Downs and Black 27-item Checklist
| Checklist question | Scoring | |
|---|---|---|
| Reporting | 1) Is the hypothesis/aim/objective of the study clearly described? | Yes = 1; No = 0 |
| 2) Are the main outcomes to be measured clearly described in the introduction or methods section? | Yes = 1; No = 0 | |
| 3) Are the characteristics of the patients included in the study clearly described? | Yes = 1; No = 0 | |
| 4) Are the interventions of interest clearly described? | Yes = 1; No = 0 | |
| 5) Are the distributions of principal confounders in each group of patients to be compared clearly described? | Yes = 2; Partially = 1; No = 0 | |
| 6) Are the main findings of the study clearly described? | Yes = 1; No = 0 | |
| 7) Does the study provide estimates of the random variability in the data for the main outcomes? | Yes = 1; No = 0 | |
| 8) Have all important adverse events that may be a consequence of the intervention been reported? | Yes = 1; No = 0 | |
| 9) Have the characteristics of patients lost to follow-up been described? | Yes = 1; No = 0 | |
| 10) Have actual probability values been reported (eg, 0.035 rather than <0.05) for the main outcomes, except where the probability value is <0.001? | Yes = 1; No = 0 | |
| External validity | 11) Were the subjects asked to participate in the study representative of the entire population from which they were recruited? | Yes = 1; No = 0; Unable to determine = 0 |
| 12) Were those subjects who were prepared to participate representative of the entire population from which they were recruited? | Yes = 1; No = 0; Unable to determine = 0 | |
| 13) Were the staff, places, and facilities where the patients were treated representative of the treatment the majority of patients receive? | Yes = 1; No = 0; Unable to determine = 0 | |
| Internal validity – bias | 14) Was an attempt made to blind study subjects to the intervention they have received? | Yes = 1; No = 0; Unable to determine = 0 |
| 15) Was an attempt made to blind those measuring the main outcomes of the intervention? | Yes = 1; No = 0; Unable to determine = 0 | |
| 16) If any of the results of the study were based on “data dredging,” was this made clear? | Yes = 1; No = 0; Unable to determine = 0 | |
| 17) In trials and cohort studies, do the analyses adjust for different lengths of follow- up of patients, or in case–control studies, is the time period between the intervention and outcome the same for cases and controls? | Yes = 1; No = 0; Unable to determine = 0 | |
| 18) Were the statistical tests used to assess the main outcomes appropriate? | Yes = 1; No = 0; Unable to determine = 0 | |
| 19) Was compliance with the intervention(s) reliable? | Yes = 1; No = 0; Unable to determine = 0 | |
| 20) Were the main outcome measures used accurate (valid and reliable)? | Yes = 1; No = 0; Unable to determine = 0 | |
| Internal validity – confounding (selection bias) | 21) Were the patients in different intervention groups (trials and cohort studies) or were the cases and controls (case–control studies) recruited from the same population? | Yes = 1; No = 0; Unable to determine = 0 |
| 22) Were study subjects in different intervention groups (trials and cohort studies) or were the cases and controls (case–control studies) recruited over the same period of time? | Yes = 1; No = 0; Unable to determine = 0 | |
| 23) Were study subjects randomized to intervention groups? | Yes = 1; No = 0; Unable to determine = 0 | |
| 24) Was the randomized intervention assignment concealed from both patients and health care staff until recruitment was complete and irrevocable? | Yes = 1; No = 0; Unable to determine = 0 | |
| 25) Was there adequate adjustment for confounding in the analyses from which the main findings were drawn? | Yes = 1; No = 0; Unable to determine = 0 | |
| 26) Were losses of patients to follow-up taken into account? | Yes = 1; No = 0; Unable to determine = 0 | |
| Power | 27) Did the study have sufficient power to detect a clinically important effect where the probability value for a difference being due to chance is less than 5%? | Yes = 1; No = 0; Unable to determine = 0 |
Notes: The Downs and Black Checklist is a 27-item methodological quality assessment tool of randomized and nonrandomized studies of health care interventions. The maximum score is 28 since all individual items were rated as yes (=1), no (=0), or unable to determine (=0), with the exception of Item 5, where a maximum of 2 points could be received. Scores are grouped into four categories: excellent (26–28 points); good (20–25); fair (15–19); and poor (≤14).
Table S2.
Downs and Black quality assessment of the included studies
| Author, year of publication | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anderson et al 19981 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 0 |
| Moulton et al 19982 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |
| Hoskins et al 19993 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 |
| Russell et al 20114 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 |
| Madigan et al 20125 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 |
| Russell et al 20176 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |
References
- 1.Anderson MA, Pena RA, Helms LB. Home care utilization by congestive heart failure patients: a pilot study. Public Health Nurs. 1998;15(2):146–62. doi: 10.1111/j.1525-1446.1998.tb00333.x. [DOI] [PubMed] [Google Scholar]
- 2.Moulton PJ, McGrane AM, Beck TL, Holland NL, Christopher MA. Utilization of home health care services by elderly patients with heart failure. Home Health Care Manage Pract. 1998;10(4):66–73. [Google Scholar]
- 3.Hoskins LM, Walton-Moss B, Clark HM, Schroeder MA, Thiel L. Predictors of hospital readmission among the elderly with congestive heart failure. Home Healthc Nurse. 1999;17(6):373–381. doi: 10.1097/00004045-199906000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Russell D, Rosati RJ, Sobolewski S, Marren J, Rosenfeld P. Implementing a transitional care program for high-risk heart failure patients: findings from a community-based partnership between a certified home healthcare agency and regional hospital. J Healthc Qual. 2011;33(6):17–24. doi: 10.1111/j.1945-1474.2011.00167.x. [DOI] [PubMed] [Google Scholar]
- 5.Madigan EA, Gordon NH, Fortinsky RH, Koroukian SM, Piña I, Riggs JS. Rehospitalization in a national population of home health care patients with heart failure. Health Serv Res. 2012;47(6):2316–2338. doi: 10.1111/j.1475-6773.2012.01416.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Russell D, Mola A, Onorato N, et al. Preparing home health aides to serve as health coaches for home care patients with chronic illness: findings and lessons learned from a mixed-method evaluation of two pilot programs. Home Health Care Manag Pract. 2017;29(3):191–198. [Google Scholar]
Acknowledgments
This study was presented at the Society of General Internal Medicine Annual Meeting in Denver, CO, on April 21, 2018.
Footnotes
Author contributions
MRS contributed to the development of the study protocol, oversaw data collection, extracted data from included papers, synthesized the results, drafted the manuscript, edited the tables and figures, and revised the manuscript. ALS and PBKL screened titles and abstracts, extracted data from included papers, participated in the synthesis of results, helped to draft the tables and figures of the manuscript, and revised the final draft. MMS contributed to the development of the study protocol, the drafting of the manuscript, and revised the draft. CDJ and EKT contributed to the development of the study protocol, the drafting of the manuscript, and revised the final draft. DD contributed to the development of the study protocol, conducted the analysis, oversaw data synthesis, and revised the final draft. All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
Dr Sterling was supported by the T32HS000066 from the Agency for Healthcare Research and Quality for the duration of this study. She also received the 2018 Founder’s Grant from the Society of General Internal Medicine to support her research on home care workers in heart failure. Dr Safford receives salary support for Amgen, unrelated to this work. Dr Jones was supported by K08HS024569 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality. The authors report no other conflicts of interest in this work.
References
- 1.Annema C, Luttik ML, Jaarsma T. Reasons for readmission in heart failure: perspectives of patients, caregivers, cardiologists, and heart failure nurses. Heart Lung. 2009;38(5):427–434. doi: 10.1016/j.hrtlng.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 2.Riegel B, Lee CS, Dickson VV, Medscape Self care in patients with chronic heart failure. Nat Rev Cardiol. 2011;8(11):644–654. doi: 10.1038/nrcardio.2011.95. [DOI] [PubMed] [Google Scholar]
- 3.Bennett SJ, Sauvé MJ. Cognitive deficits in patients with heart failure: a review of the literature. J Cardiovasc Nurs. 2003;18(3):219–242. doi: 10.1097/00005082-200307000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Sterling MR, Lin FR, Jannat-Khah DP, Goman AM, Echeverria SE, Safford MM. Hearing loss among older adults with heart failure in the United States: data from the National Health and Nutrition Examination Survey. JAMA Otolaryngol Head Neck Surg. 2018;144(3):273–275. doi: 10.1001/jamaoto.2017.2979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sterling MR, Jannat-Khah D, Vitale S, Safford MM. Can your patients with heart failure see? The prevalence of visual impairment among adults with heart failure. J Gen Intern Med. 2018;33(5):605–607. doi: 10.1007/s11606-018-4366-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burke RE, Jones J, Ho PM, Bekelman DB. Caregivers’ perceived roles in caring for patients with heart failure: what do clinicians need to know? J Card Fail. 2014;20(10):731–738. doi: 10.1016/j.cardfail.2014.07.011. [DOI] [PubMed] [Google Scholar]
- 7.Jones CD, Bowles KH, Richard A, Boxer RS, Masoudi FA. High-value home health care for patients with heart failure: an opportunity to optimize transitions from hospital to home. Circ Cardiovasc Qual Outcomes. 2017;10(5):e003676. doi: 10.1161/CIRCOUTCOMES.117.003676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nicholas Dionne-Odom J, Hooker SA, Bekelman D, et al. Family caregiving for persons with heart failure at the intersection of heart failure and palliative care: a state-of-the-science review. Heart Fail Rev. 2017;22(5):543–557. doi: 10.1007/s10741-017-9597-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Retrum JH, Nowels CT, Bekelman DB. Patient and caregiver congruence: the importance of dyads in heart failure care. J Cardiovasc Nurs. 2013;28(2):129–136. doi: 10.1097/JCN.0b013e3182435f27. [DOI] [PubMed] [Google Scholar]
- 10.Strachan PH, Currie K, Harkness K, Spaling M, Clark AM. Context matters in heart failure self-care: a qualitative systematic review. J Card Fail. 2014;20(6):448–455. doi: 10.1016/j.cardfail.2014.03.010. [DOI] [PubMed] [Google Scholar]
- 11.Bueno H, Ross JS, Wang Y, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993-2006. JAMA. 2010;303(21):2141–2147. doi: 10.1001/jama.2010.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jones CD, Ginde AA, Burke RE, Wald HL, Masoudi FA, Boxer RS. Increasing home healthcare referrals upon discharge from U.S. hospitals: 2001-2012. J Am Geriatr Soc. 2015;63(6):1265–1266. doi: 10.1111/jgs.13467. [DOI] [PubMed] [Google Scholar]
- 13.Jones CD, Wald HL, Boxer RS, et al. Characteristics associated with home health care referrals at hospital discharge: results from the 2012 national inpatient sample. Health Serv Res. 2017;52(2):879–894. doi: 10.1111/1475-6773.12504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Craig E. The jobs Americans do. The New York Times Magazine. 2017 [Google Scholar]
- 15.Bercovitz A, Moss A, Sengupta M, Park-Lee EY, Jones A, Harris-Kojetin LD. An overview of home health aides: United States, 2007. Natl Health Stat Report. 2011;34(34):1–31. [PubMed] [Google Scholar]
- 16.PHI US home care workers: key facts. 2016. [Accessed September 26, 2017]. Available from: https://phinational.org/sites/phinational.org/files/phi-home-care-workers-key-facts.pdf.
- 17.Hewko SJ, Cooper SL, Huynh H, et al. Invisible no more: a scoping review of the health care aide workforce literature. BMC Nurs. 2015;14:38. doi: 10.1186/s12912-015-0090-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McClement S, Wowchuk S, Klaasen K. “Caring as if it were my family”: health care aides’ perspectives about expert care of the dying resident in a personal care home. Palliat Support Care. 2009;7(4):449–457. doi: 10.1017/S1478951509990459. [DOI] [PubMed] [Google Scholar]
- 19.Stone R, Sutton JP, Bryant N, Adams A, Squillace M. The home health workforce: a distinction between worker categories. Home Health Care Serv Q. 2013;32(4):218–233. doi: 10.1080/01621424.2013.851049. [DOI] [PubMed] [Google Scholar]
- 20.Stone RI. The direct care worker: the third rail of home care policy. Annu Rev Public Health. 2004;25:521–537. doi: 10.1146/annurev.publhealth.25.102802.124343. [DOI] [PubMed] [Google Scholar]
- 21.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151(4):W65–W94. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]
- 22.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nguyen HL, Saczynski JS, Gore JM, Goldberg RJ. Age and sex differences in duration of prehospital delay in patients with acute myocardial infarction: a systematic review. Circ Cardiovasc Qual Outcomes. 2010;3(1):82–92. doi: 10.1161/CIRCOUTCOMES.109.884361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Samoocha D, Bruinvels DJ, Elbers NA, Anema JR, van der Beek AJ. Effectiveness of web-based interventions on patient empowerment: a systematic review and meta-analysis. J Med Internet Res. 2010;12(2):e23. doi: 10.2196/jmir.1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reichert FF, Baptista Menezes AM, Wells JC, Carvalho Dumith S, Hallal PC. Physical activity as a predictor of adolescent body fatness: a systematic review. Sports Med. 2009;39(4):279–294. doi: 10.2165/00007256-200939040-00002. [DOI] [PubMed] [Google Scholar]
- 26.Tan L, Wang MJ, Modini M, et al. Preventing the development of depression at work: a systematic review and meta-analysis of universal interventions in the workplace. BMC Med. 2014;12:74. doi: 10.1186/1741-7015-12-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anderson MA, Pena RA, Helms LB. Home care utilization by congestive heart failure patients: a pilot study. Public Health Nurs. 1998;15(2):146–162. doi: 10.1111/j.1525-1446.1998.tb00333.x. [DOI] [PubMed] [Google Scholar]
- 28.Moulton PJ, McGrane AM, Beck TL, Holland NL, Christopher MA. Utilization of home health care services by elderly patients with heart failure. Home Health Care Manag Pract. 1998;10(4):66–73. [Google Scholar]
- 29.Hoskins LM, Walton-Moss B, Clark HM, Schroeder MA, Thiel L. Predictors of hospital readmission among the elderly with congestive heart failure. Home Healthc Nurse. 1999;17(6):373–381. doi: 10.1097/00004045-199906000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Russell D, Rosati RJ, Sobolewski S, Marren J, Rosenfeld P. Implementing a transitional care program for high-risk heart failure patients: findings from a community-based partnership between a certified home healthcare agency and regional hospital. J Healthc Qual. 2011;33(6):17–24. doi: 10.1111/j.1945-1474.2011.00167.x. [DOI] [PubMed] [Google Scholar]
- 31.Madigan EA, Gordon NH, Fortinsky RH, Koroukian SM, Piña I, Riggs JS. Rehospitalization in a national population of home health care patients with heart failure. Health Serv Res. 2012;47(6):2316–2338. doi: 10.1111/j.1475-6773.2012.01416.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Russell D, Mola A, Onorato N, et al. Preparing home health aides to serve as health coaches for home care patients with chronic illness: findings and lessons learned from a mixed-method evaluation of two pilot programs. Home Health Care Manag Pract. 2017;29(3):191–198. [Google Scholar]
- 33.Balestroni G, Bertolotti G. EuroQol-5D (EQ-5D): an instrument for measuring quality of life. Monaldi Arch Chest Dis. 2012;78(3):155–159. doi: 10.4081/monaldi.2012.121. [DOI] [PubMed] [Google Scholar]
- 34.Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001;33(5):337–343. doi: 10.3109/07853890109002087. [DOI] [PubMed] [Google Scholar]
- 35.Riegel B, Carlson B, Moser DK, Sebern M, Hicks FD, Roland V. Psychometric testing of the self-care of heart failure index. J Card Fail. 2004;10(4):350–360. doi: 10.1016/j.cardfail.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 36.Sattar N, Preiss D. Reverse causality in cardiovascular epidemiological research: more common than imagined? Circulation. 2017;135(24):2369–2372. doi: 10.1161/CIRCULATIONAHA.117.028307. [DOI] [PubMed] [Google Scholar]
- 37.van Spall HGC, Rahman T, Mytton O, et al. Comparative effectiveness of transitional care services in patients discharged from the hospital with heart failure: a systematic review and network meta-analysis. Eur J Heart Fail. 2017;19(11):1427–1443. doi: 10.1002/ejhf.765. [DOI] [PubMed] [Google Scholar]
- 38.Phillips CO, Wright SM, Kern DE, Singa RM, Shepperd S, Rubin HR. Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure: a meta-analysis. JAMA. 2004;291(11):1358–1367. doi: 10.1001/jama.291.11.1358. [DOI] [PubMed] [Google Scholar]
- 39.Feltner C, Jones CD, Cené CW, et al. Transitional care interventions to prevent readmissions for persons with heart failure: a systematic review and meta-analysis. Ann Intern Med. 2014;160(11):774–784. doi: 10.7326/M14-0083. [DOI] [PubMed] [Google Scholar]
- 40.Fergenbaum J, Bermingham S, Krahn M, Alter D, Demers C. Care in the home for the management of chronic heart failure: systematic review and cost-effectiveness analysis. J Cardiovasc Nurs. 2015;30(4 Suppl 1):S44–S51. doi: 10.1097/JCN.0000000000000235. [DOI] [PubMed] [Google Scholar]
- 41.Holland R, Battersby J, Harvey I, Lenaghan E, Smith J, Hay L. Systematic review of multidisciplinary interventions in heart failure. Heart. 2005;91(7):899–906. doi: 10.1136/hrt.2004.048389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Koshman SL, Charrois TL, Simpson SH, McAlister FA, Tsuyuki RT. Pharmacist care of patients with heart failure: a systematic review of randomized trials. Arch Intern Med. 2008;168(7):687–694. doi: 10.1001/archinte.168.7.687. [DOI] [PubMed] [Google Scholar]
- 43.Ponniah A, Anderson B, Shakib S, Doecke CJ, Angley M. Pharmacists’ role in the post-discharge management of patients with heart failure: a literature review. J Clin Pharm Ther. 2007;32(4):343–352. doi: 10.1111/j.1365-2710.2007.00827.x. [DOI] [PubMed] [Google Scholar]
- 44.Jaarsma T. Health care professionals in a heart failure team. Eur J Heart Fail. 2005;7(3):343–349. doi: 10.1016/j.ejheart.2005.01.009. [DOI] [PubMed] [Google Scholar]
- 45.Slyer JT, Concert CM, Eusebio AM, Rogers ME, Singleton J. A systematic review of the effectiveness of nurse coordinated transitioning of care on readmission rates for patients with heart failure. JBI Libr Syst Rev. 2011;9(15):464–490. doi: 10.11124/01938924-201109150-00001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1.
Downs and Black 27-item Checklist
| Checklist question | Scoring | |
|---|---|---|
| Reporting | 1) Is the hypothesis/aim/objective of the study clearly described? | Yes = 1; No = 0 |
| 2) Are the main outcomes to be measured clearly described in the introduction or methods section? | Yes = 1; No = 0 | |
| 3) Are the characteristics of the patients included in the study clearly described? | Yes = 1; No = 0 | |
| 4) Are the interventions of interest clearly described? | Yes = 1; No = 0 | |
| 5) Are the distributions of principal confounders in each group of patients to be compared clearly described? | Yes = 2; Partially = 1; No = 0 | |
| 6) Are the main findings of the study clearly described? | Yes = 1; No = 0 | |
| 7) Does the study provide estimates of the random variability in the data for the main outcomes? | Yes = 1; No = 0 | |
| 8) Have all important adverse events that may be a consequence of the intervention been reported? | Yes = 1; No = 0 | |
| 9) Have the characteristics of patients lost to follow-up been described? | Yes = 1; No = 0 | |
| 10) Have actual probability values been reported (eg, 0.035 rather than <0.05) for the main outcomes, except where the probability value is <0.001? | Yes = 1; No = 0 | |
| External validity | 11) Were the subjects asked to participate in the study representative of the entire population from which they were recruited? | Yes = 1; No = 0; Unable to determine = 0 |
| 12) Were those subjects who were prepared to participate representative of the entire population from which they were recruited? | Yes = 1; No = 0; Unable to determine = 0 | |
| 13) Were the staff, places, and facilities where the patients were treated representative of the treatment the majority of patients receive? | Yes = 1; No = 0; Unable to determine = 0 | |
| Internal validity – bias | 14) Was an attempt made to blind study subjects to the intervention they have received? | Yes = 1; No = 0; Unable to determine = 0 |
| 15) Was an attempt made to blind those measuring the main outcomes of the intervention? | Yes = 1; No = 0; Unable to determine = 0 | |
| 16) If any of the results of the study were based on “data dredging,” was this made clear? | Yes = 1; No = 0; Unable to determine = 0 | |
| 17) In trials and cohort studies, do the analyses adjust for different lengths of follow- up of patients, or in case–control studies, is the time period between the intervention and outcome the same for cases and controls? | Yes = 1; No = 0; Unable to determine = 0 | |
| 18) Were the statistical tests used to assess the main outcomes appropriate? | Yes = 1; No = 0; Unable to determine = 0 | |
| 19) Was compliance with the intervention(s) reliable? | Yes = 1; No = 0; Unable to determine = 0 | |
| 20) Were the main outcome measures used accurate (valid and reliable)? | Yes = 1; No = 0; Unable to determine = 0 | |
| Internal validity – confounding (selection bias) | 21) Were the patients in different intervention groups (trials and cohort studies) or were the cases and controls (case–control studies) recruited from the same population? | Yes = 1; No = 0; Unable to determine = 0 |
| 22) Were study subjects in different intervention groups (trials and cohort studies) or were the cases and controls (case–control studies) recruited over the same period of time? | Yes = 1; No = 0; Unable to determine = 0 | |
| 23) Were study subjects randomized to intervention groups? | Yes = 1; No = 0; Unable to determine = 0 | |
| 24) Was the randomized intervention assignment concealed from both patients and health care staff until recruitment was complete and irrevocable? | Yes = 1; No = 0; Unable to determine = 0 | |
| 25) Was there adequate adjustment for confounding in the analyses from which the main findings were drawn? | Yes = 1; No = 0; Unable to determine = 0 | |
| 26) Were losses of patients to follow-up taken into account? | Yes = 1; No = 0; Unable to determine = 0 | |
| Power | 27) Did the study have sufficient power to detect a clinically important effect where the probability value for a difference being due to chance is less than 5%? | Yes = 1; No = 0; Unable to determine = 0 |
Notes: The Downs and Black Checklist is a 27-item methodological quality assessment tool of randomized and nonrandomized studies of health care interventions. The maximum score is 28 since all individual items were rated as yes (=1), no (=0), or unable to determine (=0), with the exception of Item 5, where a maximum of 2 points could be received. Scores are grouped into four categories: excellent (26–28 points); good (20–25); fair (15–19); and poor (≤14).
Table S2.
Downs and Black quality assessment of the included studies
| Author, year of publication | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anderson et al 19981 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 0 |
| Moulton et al 19982 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |
| Hoskins et al 19993 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 |
| Russell et al 20114 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 |
| Madigan et al 20125 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 |
| Russell et al 20176 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |


