Abstract
Localized nitric oxide (NO) release from polymeric materials holds much promise for the prevention of coagulation often associated with implantable and extracorporeal blood-contacting devices. Films of polyurethane (PU) containing incorporated polyethyleneimine were thus exposed to NO gas to form diazeniumdiolates (NONOates) in situ. Donor incorporation and NO gas exposure did not affect the mechanical properties of the films. The NO release capacity increased with increasing polydimethylsiloxane (PDMS) content in the soft segment of the PU: total capacity could be more than doubled (P<0.05) from 0.093 ± 0.028 to 0.225 ± 0.004 mmol/g when the PDMS content was increased from 0 to 100%. Release kinetics were best approximated using a modified Korsemeyer-Peppas power law (R2=0.95-0.99). Despite the resultant rapid initial decrease in NO release rates, values above that observed for quiescent endothelial cells (0.83 pmol·cm−2·s−1) were maintained for extended periods of 5-10 days, while rates above that of a stimulated endothelium (2.7-6.8 pmol·cm−2·s−1) were achieved for the first 24 hours. This method of NONOate formation may be advantageous, as potential premature NO release by exposure of diazeniumdiolated donors during incorporation, processing and storage, can be avoided by in situ diazoniumdiolation closer to the time of implantation.
Keywords: In situ diazeniumdiolation, Mechanical properties, Nitric oxide, Polydimethylsiloxane, Polyurethane, Release kinetics
Introduction
The role of nitric oxide (NO) in physiology, neuroscience and immunology has been recognized to the extent that it was named by the journal Science as “Molecule of the year” in 1992 (1). In addition to its vasodilatory function, NO has also been shown to inhibit smooth muscle cell proliferation (2), inhibit platelet aggregation (3) and adhesion (4), and to attenuate leukocyte function (5). The molecule also plays an important role in angiogenesis, as it inhibits apoptosis and increases endothelial proliferation and migration (6). A review on the effects of NO in the cardiovascular system may be found in an article by Strijdom et al (7).
With all these potentially therapeutic attributes, it is not surprising that NO is used not only in clinical settings as inhaled gas for treatment of primary pulmonary hypertension, hypoxia and acute respiratory distress syndrome (8), but also increasingly in experimental medical device applications (9). Examples of devices include vascular grafts (10, 11), oxygen sensors (12, 13), extracorporeal circuits (14, 15), stents (16) and glucose sensors (17). A large number of NO donors are available (18), and many of them have been incorporated in prosthetic materials such as silicone rubber (14), polyurethane (PU) (19), polyvinyl chloride (10), polymethacrylate (20) and expanded polytetrafluoroethylene (ePTFE) (9).
Two classes of NO donors are commonly used in biomaterials, namely diazeniumdiolates (also called NONOates) and S-nitrosothiols. The S-nitrosothiols are generally formed by reaction of nitrous acid with the parent thiol, and are reported to require copper-mediated decomposition, reaction with ascorbate or cleavage by light to release NO. The former (NONOates) are synthesized by reaction of amines with NO gas to form relatively stable compounds that spontaneously release NO on contact with bodily fluids, and most of the work in the field of NO donors in biomaterials has concentrated on the use of the NONOates (9). Although primary and secondary amines may be used (21), secondary amines are more often used, as their diazeniumdiolates tend to be more stable and give greater NO yields (22, 23). A list of donors used in NOeluting materials that include a range of secondary amines is given in Table I. In order to maximize the number of secondary amines, combined with the requirement to have a nontoxic, high-molecular-mass material for incorporation into the PU polymer, linear polyethyleneimine (LPEI) was chosen as donor in the current study. The diazenium-diolization of a secondary amine, as exemplified by LPEI, is shown in Figure 1.
TABLE I.
SUMMARY OF SELECTED NITRIC OXIDE–ELUTING MATERIALS SHOWING NO ELUTION AND FLUX, WITH APPROXIMATIONS OF THE RELEASE AND FLUX PROFILES, THE MATERIALS AND DONORS USED, AS WELL AS THE TIME POINT AT WHICH THE DIAZENIUMDIOLATION OCCURRED (BEFORE OR AFTER THE INCORPORATION OF THE AMINE)
| Paper ref. | NO Elution (μmol·g−1) | NO Elution (μmol·cm−2) | Elution time (h) | Elution profile (M) | Flux max (pmol·cm−2·s−1) | Flux t (pmol·cm−2·s−1) | Flux time (hours) | Flux profile (F) | Material | Donor | NONOate formation |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (24) | – | – | – | – | 0.83 | 0.83 | – | F1 | Cultured EC | L-Arginine | – |
| (25, 26) | – | – | – | – | 2.7-6.8 | 2.7-6.8 | – | F1 | Stimulated EC | L-Arginine | – |
| Current paper | 93-225 | 2-6 | M3 | 19-48 | 1.3–0.2 | 120-800 | F3 | Elast-Eon™ PU | 4% LPEI non-cov | After | |
| (17) | – | – | – | – | 2-20 | 0-0.5 | 16 | F3/F4 | 80% BTMOS xerogels | 20% AEMP3/ AHAP3/ AEAP3 cov | After |
| (27) | 8-20 | M3 | 80-170 | 8-30 | 17 | F4 | PVC/DOS | 4-8% DIB non-cov | Before | ||
| (19) | 0.05 | M2 | 0.125§ | 0.002§ | 48-1300 | – | PU | SGKKKKGGS cov | Before and after | ||
| (28) | 125 11/25 2.2 | – | – | M3* | – | PU/DOS PU/DOS PVC/DOS | 4% DIM non-cov 6-12% LPEI non-cov 50% PVC-Piperazine cov | In solution | |||
| (10) | – | – | – | – | 120 | 30-5 | 168-504 | F3 | PVC | DIB | Before |
| (29) | – | 0.04§ | M3 | – | PU-PEG-YIGSR | SGKKKKGGS cov | In solution | ||||
| (30) | – | – | – | – | 300 | 300-0 | 0-70 | F3/F4 | Aminosilane xerogels | 40% AHAP3 cov | After |
| (31) | – | – | – | – | 3.3-100 | 0.8-7.2 | 48 | F1/F3/F4 | Carbosil PU±NH2 | DIB non-cov | Before |
| (32) | – | – | – | – | 18-60 | 10-30 | 4.5 | F3/F4 | BTMOS xerogels | AHAP3 cov | After |
| (14) | – | 1.2-3.8 | 5-480 | M3 | 13-41 | 8-17 | 5 | F4 | SR | DACA cov | After |
| (33) | – | – | – | – | 12-18 | 1 | 21 | F3 | PU (Pellethane) | DETA etc cov | After |
| (34) | – | – | – | – | 2-7 | 1.6-4 | 12 | F1/F3/F4 | Pursil 20 PU | DIB non-cov | Before |
| (35) | – | 0.001 | 3 | – | PU | Cysteine cov | After | ||||
| (36) | – | 0.2 | – | 3 | 0.4 | 30 | F3 | PU | S Nitroso cov. | Before | |
| (37) | 2.5-25 | – | 1700 | E1 | 17-36 | 2 | 17-22 | F4 | PU | =NH (MOM) | Before |
| (38) | – | – | – | – | 63-73 | – | – | – | PU | NCON-cyclen/Cu(II) | N/A |
AEAP3 = N-(6-aminoethyl)-3-aminopropyltrimethoxysilane; AEMP3 = (aminoethylaminomethyl)phenethyltrimethoxysilane); AHAP3 = N-(6-aminohexyl)aminopropyltrimethoxysilane; BTMOS = Isobutyltrimethoxysilane; DACA = diamino-alkyltrimethoxysilane; DET3 = N-[3-(Trimethoxysilyl)propyl]diethylenetriamine; DIB/DIM = N, N′-dibutyl-1,6-hexanediamine/N, N′-dimethyl-1,6-hexanediamine; DOS/LPEI = Dioctyl sebacte/linear polyethylenimine; MAHMA/MOM = (Z)-1(N-methyl-N-[6(N-methylammoniohexyl)amino])/methoxymethyl; PEI/PTFE/PU = polyethylenimine/polytetrafluoroethylene/Polyurethane; PVP/SR = poly(vinylpyrrolidone)/Silicone rubber; cov/non-cov = covalent/noncovalent incorporation of donor; */§ = Not Higuchi ([NO] α t1/2) or First order (ln[NO] α t)/calculated from given data; Illustrative profiles for Elution (M: Column 5) and Flux (F: column 9) are given below: 
Fig. 1.
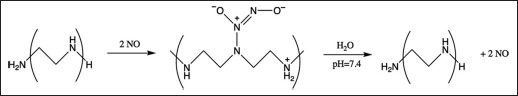
Reaction of nitric oxide (NO) with linear polyethyleneimine to form the diazeniumdiolate, and the subsequent release of the NO when encountering physiological conditions.
NO donors may be non-covalently incorporated (by dispersion) into the polymer matrix or coating (28). More recently, more lipophilic donors have been developed (27), or the donors were covalently coupled to the polymer backbones (19, 27, 33). When the donors are incorporated into the polymers, there is also a choice between diazeniumdiolation of the donor before incorporation (28), or incorporating the donor and then exposing the polymer to NO gas to NONOates it in situ (14). In the latter case, the diffusion of the NO gas through the base polymer is of importance, and this method holds the advantage over pre-exposure in that the device may be processed into its final shape and then exposed to NO before use. On the other hand, pre-exposure of the donors would require careful handling of the diazeniumdiolate and doped polymer during processing and storage, as NONOates can have very short half-lives (9).
The current study thus describes the incorporation of LPEI in PU films containing different amounts of polydimethylsiloxane (PDMS) in their soft segments and subsequent NONOation by NO gas exposure to determine whether long-term NO elution can be achieved. In addition, the hypothesis that the higher diffusivity of diatomic gasses through PDMS over PU (39, 40) would result in increased NO release with increased PDMS content (e.g., N2 has a larger diffusion constant in PDMS than in PU). Finally, the effect of LPEI doping and elution on the mechanical properties of the PU was determined, mainly to ensure that the loading with LPEI and NO did not have an unacceptable adverse effect on these properties.
Materials and Methods
PU film fabrication
Elast-Eon™ (donated by Aortech, Australia) comprising 60% soft segments (PDMS and/or poly(hexamethylene oxide) [PHMO]) and 40% hard segment (4,4′-methylene-diphenyl diisocyanate [MDI] and 1,4-butanediol [BDO]) was used in this study. Films of this polymer, containing 0, 20%, 40%, 60%, 80% and 100% PDMS in their soft segments, and further containing 4 mass% (nominally) of linear polyethylene imine (LPEI50: molecular masses of 22,000; Polychemistry, Tucson Arizona), were made by (i) adding 9.2 mL of a 12.5 mg/mL solution of LPEI (in MeOH) to a 10 mass% solution of the PU (in THF), (ii) casting 15 mL of the resultant mixture in 70-mm diameter dishes, (iii) slow evaporation of the solvents in air (48 hours) and (iv) drying under vacuum (100 kPa absolute pressure; 48 hours). The concentration of 4% LPEI was chosen based on literature values and qualitative trials in which higher concentrations led to brittle materials. Control films were made in an identical manner but without addition of entrapped LPEI.
NONOate formation
For the formation of diazeniumdiolates (NONOates), LPEI-doped (and non-doped control) Elast-Eon™ films were exposed to NO in a custom-built stainless-steel chamber (Fig. 2). After loading the films into the chamber and flushing the system 6 times with Ar gas (2 atm. gauge pressure followed by release to atmospheric pressure), the chamber was filled to 5 atmospheres (gauge) with NO gas (Kinox 900, >90%; Airliquid, SA) and maintained for 96 hours, after which the system was again flushed 6 times with Ar to remove the excess NO, and the samples removed for further analysis. During the pressurization with NO gas, the concentration of this gas was 83.3% (with the remainder mostly Ar). The subsequent 6 flushes with Ar removed all but a small amount (0.12%) of NO gas before the vessel was opened.
Fig. 2.
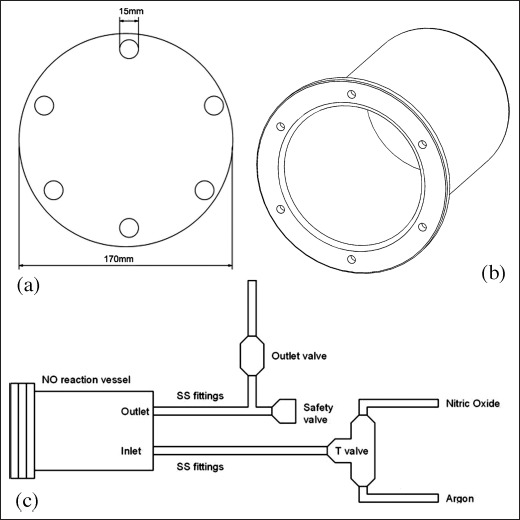
Front, dimetric and side views of the stainless steel reaction chamber and fittings used for the formation of NONOates from the linear polyethyleneimine (LPEI) in the polyurethane films.
A notation was made where the first 2-3 digits (00 to 100) represent the percentage of PDMS in the PU, the sign and number “50” indicate the presence (+50) or absence (-50) of the LPEI50, and +NO or –NO indicate whether the samples were exposed or not (respectively) to NO gas. For example, 100+50+NO designated a sample with 100% PDMS in the soft segment, which contained LPEI50, and was exposed to NO gas as described.
Mechanical Testing
Specimens (n=2) were cut from film samples (with and without LPEI incorporation, and with and without NO exposure) using an ASTM D638 (Type V) cutter and extended to failure at 200 mm/min on a model 5544 Instron tensile tester to derive tensile stress and strain at break, as well as the Young's modulus. To determine the effect of LPEI leaching on the mechanical properties, samples of Elast-Eon™ containing 80% PDMS (with and without LPEI incorporation) were tested before and after 15 days of incubation in phosphate-buffered saline (PBS) at pH 7.4 (PBS: Na2HPO4·12H2O, 2.89 g, 8.1 mmol; KH2PO4, 0.20 g, 1.5 mmol; KCl, 0.20 g, 2.7 mmol and NaCl, 8.0 g, 136.9 mmol).
NO Elution
NO-treated LPEI-containing film disks (18-mm diameter, n=2) were incubated in 5 mL of PBS buffer (37°C) with regular PBS replacement. As released NO reacts with oxygen and water to form nitrite, the NO release was quantified using the Griess nitrite assay (41), which is regularly used for determining NO release from similar polymeric samples (19, 28, 29). Briefly, 100 μL of Griess reagent (Sigma-Aldrich, St. Louis, MO, USA) was added to 50 μL of each sample (in triplicate) in a 96-well plate, and the resulting chromophore quantified against a standard curve (NaNO2) at 540 nm using a spectrophotometer (Typical standard curve A540 vs. [Nitrite] (μM): A540 = 0.0048 ± 0.0001 [Nitrite] + 0.0547 ± 0.0004; R2=0.9999 ± 0.0001). Results are presented as moles of NO per unit mass of film over time. Power curves of the form M=k'tn were used to fit the elution data, and values for k′, n and R2 (coefficient of determination) are also given. The release rates were determined by calculating the derivatives of the power curves: Flux = dM/dt=k'ntn-1.
Statistical analysis
For quantitative data, Student's t-test (2-tailed, assuming equal variance) was used to assess differences between groups, with P<0.05 considered significant.
Results
Mechanical properties
It is evident that there was a trend toward increased modulus and decreases in both ultimate stress and strain with increased PDMS content in the soft segment (control sheets: PU-50-NO), with statistically significant differences between the 20-50-NO and 40-50-NO as well as between 60-50-NO and 80-50-NO samples, as indicated (Fig. 3).
Fig. 3.
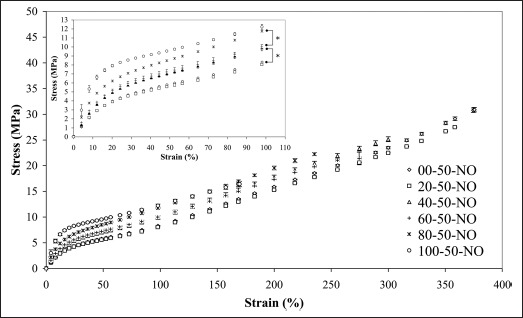
Stress-strain characteristics of pure Elast-Eon™ polymer films containing 0 to 100% polydimethylsiloxane (PDMS) in their soft segments. Insert: First 100% strain with tie bars showing statistically significant differences in stress values at 100% strain.
The numerical values for the moduli, ultimate stress and ultimate strain of the base polymer, with and without the incorporation of LPEI, and with and without exposure to NO gas are graphically summarized in Figure 4. The general increase in stiffness with increased PDMS content was confirmed for the pure PU polymer samples, where an increase from 0.250 ± 0.003 to 0.603 ± 0.030 occurred from 00-50-NO to 100-50-NO (138%) (Fig. 4a). This trend (increased modulus with increased PDMS content) was generally maintained after exposure of the control samples to NO gas (PU-50+NO), and the effect of this gas exposure (PU-50-NO to PU-50+NO) not significant. The effect of LPEI addition to the control samples on the moduli was also not significant (without gassing, i.e., PU-50-NO to PU+50-NO; apart from the 60-50-NO modulus decreasing by 13% when LPEI is added [60+50-NO]). Both the effects of NO exposure of the PLEI loaded films, and the overall effect of LPEI addition and NO exposure were not generally statistically discernable.
Fig. 4.

a) Young's modulus, b) ultimate tensile stress and c) ultimate tensile strain of polymer films with and without linear polyethyleneimine (LPEI) incorporation and with and without exposure to NO gas. Asterisks (*) indicate that the value is statistically discernable from that of the 0% polydimethylsiloxane (PDMS) sample in the same treatment group. Additional significant differences are indicated by the tie bars.
In conjunction with the increase in modulus with increased PDMS content in the soft segment, both the ultimate tensile stress (Fig. 4b) and strain (Fig. 4c) showed significant decreases from 0 to 100% PDMS (51% and 57%, respectively). Apart from the 2 instances where the exposure of the control samples to NO gas resulted in decreased ultimate stress (40% and 80% PDMS samples) and one where the addition of LPEI resulted in a discernable decrease (80% PDMS), neither the exposure to the gas nor inclusion of the polyamine had deleterious effects on the ultimate stress of the remaining samples. Overall, the addition of both amine and NO affected the ultimate stress of only the sample containing no PDMS. The ultimate strain values followed a similar pattern, with decreases observed with increasing PDMS content, and apart from a few exceptions, little overall effect of addition of LPEI and/or NO.
The effect of PBS exposure on the mechanical properties (for samples containing 80% PDMS in their soft segment) is shown in Figure 5. Although the addition of LPEI to the control samples did result in changes in ultimate stress and strain (as described above), the exposure to the buffer (for 16 days) did not result in significant differences in modulus, ultimate stress or ultimate strain of the control or LPEI-doped films.
Fig. 5.
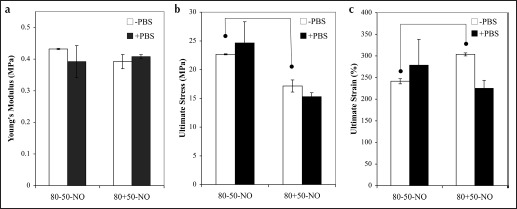
a) Young's modulus, b) ultimate tensile stress and c) ultimate tensile strain of polymer films (80% polydimethylsiloxane [PDMS]), with and without nitric oxide (NO) exposure, after the incubation in phosphate-buffered saline (PBS) for 15 days.
NO Elution
The NO release from the polymer films generally, although not strictly, increased with increasing PDMS content in the polymer's soft segment; the sample of which the soft segment comprised only PDMS (100%, i.e., sample 100+50+NO) released the highest amount (0.225 ± 0.004 mmol NO per gram of polymer film), much of which was released within the first 48 hours (Fig. 6). The total amount was significantly higher than that released by either 80+50+NO or 60+50+NO (0.176 ± 0.032 and 0.185 ± 0.009 mmol/g, respectively), while the 60+50+NO in turn released more NO than the 20+50+NO samples (0.149 ± 0.015 mmol/g), which in turn was higher than the amount released by the samples that contained no PDMS (00+50+NO, 0.093 ± 0.028 mmol/g). The 00+50+NO and 100+50+NO values were equivalent to 2.14 ± 0.54 and 6.12 ± 0.03 μmol/cm2; although normalization to mass is preferred in this paper to account for varying film thickness and thus total amount of polymer/donor/NO, the area normalizations are given to allow for comparison with published data.
Fig. 6.
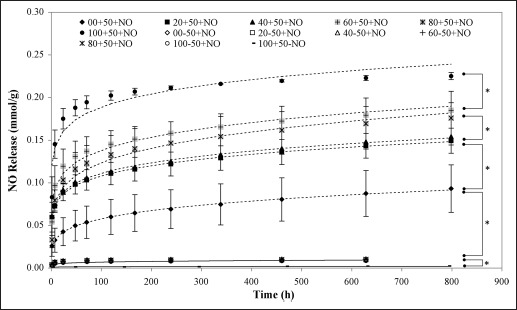
Release of nitric oxide (NO) from diazeniumdiolated linear polyethyleneimine (LPEI)-loaded Elast-Eon™ polyurethane samples incubated in phosphate-buffered saline (PBS), as determined by nitrate quantification using the Griess assay. Dashed lines represent curve fitting according to a simple power M=k'tn function. Asterisk-marked tie bars show statistically significant differences between the series indicated.
Control films (containing LPEI but without NO exposure – i.e., 100+50-NO) showed extremely low (baseline) levels (0.002 mmol/g), while films without LPEI incorporation (but with NO exposure) released levels significantly higher than the control baseline level (0.008 to 0.010 mmol/g). The latter levels were, however, less than a tenth of that released by the NONOated LPEI-containing sample with the lowest release (00+50+NO) (all indicated differences P<0.05).
The release rates similarly initially seem to follow the PDMS content of the soft segments, with the highest rates observed with 100+50+NO (48.4 ± 5.0 μmol·cm−2·s−1), as opposed to the lowest for the 00+50+NO sample (18.8±6.4 μmol·cm−2·s−1) (Fig. 7). At 120 hours, there was still between 0.8-1.3 nmol·cm−2·s−1 NO released, while the rates at the longest investigated time point (800 hours) were between 0.18 and 0.24 nmol·cm−2·s−1.
Fig. 7.
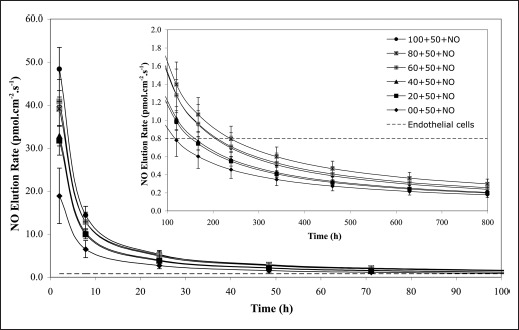
Rate of nitric oxide (NO) release from diazeniumdiolated linear polyethyleneimine (LPEI)-loaded films over the first 100-hour observation period, with an inset showing the time frame from 50 through 800 hours.
Discussion
The current paper discusses the effect of soft-segment composition on the mechanical and NO release properties of PDMS-based PUs. Specifically: (i) the PUs (without LPEI) showed increased modulus, decreased ultimate stress and decreased ultimate strain with increased PDMS content, (ii) PU films doped with LPEI could be cast from solution and exposed to NO gas at elevated pressure to form NO donors in situ, (iii) the inclusion of LPEI and exposure to NO gas had little or no effect on the mechanical properties of the films, (iv) the total amount of NO released in vitro generally increased with increased PDMS content of the PU, (v) the release of NO occurred over an extended time period after an initial burst release within the first 48 hours and (vi) the release rate of NO from the films exceeded that reported for endothelial cells for up to 120-240 hours depending on the polymer formulation.
The decreases in ultimate tensile stress and strain with increased PDMS content of the PU soft segments were similar to those observed by Gunatillake et al (42). The stiffness (Young's moduli) of the materials also showed similar increases with increased PHMO content, which can be ascribed to the compatibilizing effect of the PHMO in the soft segments, as there is a large difference in the solubility parameters between PDMS and the other reagents constituting the PU. The overall lack of significant differences between the mechanical properties of the control (PU-50-NO) and NO gas exposed (PU-50+NO) samples (without LPEI incorporation) shows that the gas itself did not cause damage to the polymer that was sufficient to discern at this level. The inclusion of LPEI in the polymers similarly did not dramatically influence the mechanical properties: apart from one instance of decreased modulus, 2 samples actually showed small increases in ultimate tensile strength that may be attributed to a reinforcing effect of the added polymer, as well as variation in sample properties often observed with tensile specimens. As the further exposure of the LPEI-loaded films to NO gas also had mostly a small and nonsignificant effect on all 3 of the mechanical parameters investigated, the overall effect of donor incorporation and in situ diazeniumdiolation of the donor on the mechanical properties of the films was concluded to be small and deemed acceptable. The lack of significant differences in mechanical properties of samples before and after exposure to PBS also indicates that the mechanical integrity of the materials is not compromised by exposure to the eluant in the short term, and is not expected to be compromised by in vivo exposure, as these polymers were shown to exhibit good biostability, especially the formulation with 80% PDMS in the soft segment (43).
The choice of LPEI as donor was based on a number of factors: it (i) is relatively nontoxic (especially compared with small dialkyl diamines; e.g., N, N′-dibutyl-1,6-hexanediamine [DIB] has an LC50 of 220 mg/m3), (ii) has a high secondary amine content and (iii) has a high molecular mass that should slow elution rate from the matrix. Trials with N, N′-dimethyl-1,6-hexanediamine (DIM) and DIB as secondary amines were abandoned after blooming of the former to the surface, while the latter was essentially fully eluted from the polymer films within 12 hours. In comparison, semiquantitative determination of LPEI release showed that only approximately 25% of the loaded amount eluted after 100 hours (data not shown).
The formation of the diazenium diolate was not shown directly, but their formation and the subsequent release of NO is indirectly shown by the highly elevated values measured for NO release in when LPEI was present in the PU polymer; PU samples containing no LPEI showed release of less than a tenth of those amounts. The latter can be explained by the absorption of the NO gas in the PU material itself. Although the decomposition of diazeniumdiolate NO donors have been shown to be pseudo-first order (27), the release profile of NO from the films was not consistent with first order (lnMt α t) (44) kinetics (R2 <0.95-0.86 for 00+50+NO through 100+50+NO). The release also did not follow the Higuchi release model based on Fickian diffusion (Mt α t1/2) (45) (R2 <0.89-0.59 for 00+50+NO through 100+50+NO), as NO release is dependent not only on the decomposition of the NONOate and diffusion of the released NO from the polymer, but also on the rate of ingress of the eluant. The data did, however, give very good least square fits over the entire 800-hour period using a modified Korsmeyer-Peppas power model (Mt α tn) (46), with R2 values ranging from 0.951 to 0.999 (Tab. II), while even better fits (0.987 to 0.999) could be achieved for the 60%-100% PDMS samples when an x-shifted power law (Mt = k′ (t-a)n) was applied, where the x-shift could account for the loss of NO in these samples while being transferred into the elution medium. Despite this good fit to the power curve, the diffusional exponent (n) did not correspond to the values (0.5<n<<1) for thin films obtained by Ritger and Peppas for anomalous non-Fickian transport (46). The short half-life of NONOates in the presence of water, and the high diffusion rates of the NO in the polymer (due to its small size) are offered as a possible explanation for the low value of the exponent in this case, while the increase in NO release with increased PDMS content can be ascribed to the increased diffusivity of PDMS toward diatomic gases, although the gas transport of NO was not specifically tested.
TABLE II.
POWER LAW CURVE FIT DATA TO THE CUMULATIVE NO RELEASE FROM PU+50+NO SAMPLES: y=k'xn (M=k'tn)
| Sample | k′ | S.E. (k) | n | S.E. (n) | R2 | S.E. (R2) |
|---|---|---|---|---|---|---|
| 00+50+NO | 0.021 | 0.009 | 0.222 | 0.026 | 0.999 | 0.001 |
| 20+50+NO | 0.053 | 0.005 | 0.152 | 0.012 | 0.999 | 0.001 |
| 40+50+NO | 0.055 | 0.002 | 0.153 | 0.005 | 0.999 | 0.000 |
| 60+50+NO | 0.068 | 0.019 | 0.153 | 0.054 | 0.979 | 0.003 |
| 80+50+NO | 0.052 | 0.007 | 0.186 | 0.034 | 0.970 | 0.002 |
| 100+50+NO | 0.111 | 0.022 | 0.114 | 0.031 | 0.951 | 0.001 |
NO = nitric oxide; PU = polyurethane.
Direct comparison with historical NO release values found in the literature for similar systems is hampered by the lack of consistency of units and often the lack of normalization of released amounts to unit mass or area. Table I has thus been compiled to, wherever possible, normalize the data presented in the literature and present the data in comparable units, as well as give an indication of the release profiles achieved. Thus, the current release of 93-225 μmol/g of film compares favorably with others in the field (see Tab. I). For example, Mowery et al achieved 11 and 125 μmol/g NO elution from PU material loaded with LPEI and DIM respectively (28), where the diazeniumdiolates were prepared in solution before incorporation, while 2.5 to 25 μmol/g could be achieved by incorporating diazeniumdiolated secondary amine-containing chain extenders covalently into the PU backbone (37). In terms of elution per unit area, the 2-6 μmol/cm2 also compares well with values of 0.001 and 0.02 μmol/cm2 for PUs containing S-nitrosothiol donors (35, 36) and even with the 8-20 μmol/cm2 achieved from PVC materials using 4%-8% noncovalently incorporated DIB (27). NO fluxes are even harder to compare as they were determined at different times during the elution process, but the fact that relatively high fluxes in the order of 1 pmol·cm−2·s−1 could be achieved in the current experiment over such a long timeframe (120-800 hours), compared with the double digit time points reported in most prior cases (Tab. I: Flux at time t [flux t] and time point of flux measurement [flux time], is encouraging.
The increase in NO release capacity with increased PDMS content may be ascribed to the increased diffusivity of the PDMS soft segment, as the non-LPEI-loaded samples did not show significant differences in NO storage/release capacity.
Although the total release capacity of the device may be of importance, the rate at which the release is maintained and the period for which it is maintained are probably the more important measure. Resting endothelial cells are reported to release NO at a rate (Flux: F) of 0.83 pmol·cm−2·s−1, while that of a stimulated endothelium is in the 2.7-6.8 pmol·cm−2·s−1 range (24), and release rates of synthetic devices are often compared with these benchmarks. In the current study, the release rate was above that of the stimulated endothelium for at least the first 24 hours, while levels above base value were maintained for 120-240 hours. It is known that high release rates (10-20 pmol·cm−2·s−1) can decrease bacterial adhesion to surfaces (17, 32), and that even at levels well below (0.002 pmol·cm−2·s−1) that of the endothelium, platelet and smooth muscle cell adhesion are decreased, and endothelial cell adhesion increased (19). The current films maintained initial rates greater than that shown to be required for bacterial resistance (in the initial stages when this will be most required in an implant), and maintained values above those shown to be sufficient for the other advantageous cellular attachment effects for the full investigation period of more than 33 days.
The encouraging in vivo results by Fleser et al (10), namely that of increased thrombus free area and patency when using NO-releasing PVC coatings on Dacron vascular grafts in a sheep arteriovenous shunt model, shows the potential of this technology. It thus seems only a question of time for the fulfilment of the promise of NO-releasing materials becoming the “artificial endothelium” (24) and of being used in the vascular grafts of the future (47).
Conclusions
Increased PDMS content in the segmented PU Elast-Eon™ resulted in increased NO release when the LPEI donor was incorporated into the PU and subsequently exposed to NO gas. LPEI and NO incorporation did not result in significant losses in mechanical properties. Extended release rates above that of the cultured endothelium could be achieved for extended periods using this system, which holds much promise for use in vascular graft and other applications where thrombogenicity requires suppression.
Acknowledgements
The authors would like to thank Dr. Ajay Padsalgikar, technical director, Aortech, for the generous donation of the Elast-Eon™, and Prof Jeff Hubbell, EPFL, for helpful discussions.
Footnotes
Financial support: Funding was received from the National Research Foundation and Medical Research Council of South Africa.
Conflict of interest: None.
References
- 1.Culotta E., Koshland D.E. Jr.. NO news is good news. Science. 1992; 258(5090): 1862–1865. [DOI] [PubMed] [Google Scholar]
- 2.Zuckerbraun B.S., Stoyanovsky D.A., Sengupta R. et al. Nitric oxide-induced inhibition of smooth muscle cell proliferation involves S-nitrosation and inactivation of RhoA. Am J Physiol Cell Physiol. 2007; 292(2): C824–C831. [DOI] [PubMed] [Google Scholar]
- 3.Radomski M.W., Palmer R.M., Moncada S. Endogenous nitric oxide inhibits human platelet adhesion to vascular endothelium. Lancet. 1987; 2(8567): 1057–1058. [DOI] [PubMed] [Google Scholar]
- 4.de Graaf J.C., Banga J.D., Moncada S., Palmer R.M., de Groot P.G., Sixma J.J. Nitric oxide functions as an inhibitor of platelet adhesion under flow conditions. Circulation. 1992; 85(6): 2284–2290. [DOI] [PubMed] [Google Scholar]
- 5.Lefer A.M. Nitric oxide: nature's naturally occurring leukocyte inhibitor. Circulation. 1997; 95(3): 553–554. [DOI] [PubMed] [Google Scholar]
- 6.Cooke J.P., Losordo D.W. Nitric oxide and angiogenesis. Circulation. 2002; 105(18): 2133–2135. [DOI] [PubMed] [Google Scholar]
- 7.Strijdom H., Chamane N., Lochner A. Nitric oxide in the cardiovascular system: a simple molecule with complex actions. Cardiovasc J Afr. 2009; 20(5): 303–310. [PMC free article] [PubMed] [Google Scholar]
- 8.Gianetti J., Bevilacqua S., De Caterina R. Inhaled nitric oxide: more than a selective pulmonary vasodilator. Eur J Clin Invest. 2002; 32(8): 628–635. [DOI] [PubMed] [Google Scholar]
- 9.Varu V.N., Tsihlis N.D., Kibbe M.R. Basic science review: nitric oxide–releasing prosthetic materials. Vasc Endovascular Surg. 2009; 43(2): 121–131. [DOI] [PubMed] [Google Scholar]
- 10.Fleser P.S., Nuthakki V.K., Malinzak L.E. et al. Nitric oxide-releasing biopolymers inhibit thrombus formation in a sheep model of arteriovenous bridge grafts. J Vasc Surg. 2004; 40(4): 803–811. [DOI] [PubMed] [Google Scholar]
- 11.Smith D.J., Chakravarthy D., Pulfer S. et al. Nitric oxide-releasing polymers containing the [N(O)NO]- group. J Med Chem. 1996; 39(5): 1148–1156. [DOI] [PubMed] [Google Scholar]
- 12.Schoenfisch M.H., Mowery K.A., Rader M.V., Baliga N., Wahr J.A., Meyerhoff M.E. Improving the thromboresistivity of chemical sensors via nitric oxide release: fabrication and in vivo evaluation of NO-releasing oxygen-sensing catheters. Anal Chem. 2000; 72(6): 1119–1126. [DOI] [PubMed] [Google Scholar]
- 13.Marxer S.M., Robbins M.E., Schoenfisch M.H. Sol-gel derived nitric oxide-releasing oxygen sensors. Analyst (Lond). 2005; 130(2): 206–212. [DOI] [PubMed] [Google Scholar]
- 14.Zhang H., Annich G.M., Miskulin J. et al. Nitric oxide releasing silicone rubbers with improved blood compatibility: preparation, characterization, and in vivo evaluation. Biomaterials. 2002; 23(6): 1485–1494. [DOI] [PubMed] [Google Scholar]
- 15.Annich G.M., Meinhardt J.P., Mowery K.A. et al. Reduced platelet activation and thrombosis in extracorporeal circuits coated with nitric oxide release polymers. Crit Care Med. 2000; 28(4): 915–920. [DOI] [PubMed] [Google Scholar]
- 16.Yoon J.H., Wu C.J., Homme J. et al. Local delivery of nitric oxide from an eluting stent to inhibit neointimal thickening in a porcine coronary injury model. Yonsei Med J. 2002; 43(2): 242–251. [DOI] [PubMed] [Google Scholar]
- 17.Schoenfisch M.H., Rothrock A.R., Shin J.H., Polizzi M.A., Brinkley M.F., Dobmeier K.P. Poly(vinylpyrrolidone)-doped nitric oxide-releasing xerogels as glucose biosensor membranes. Biosens Bioelectron. 2006; 22(2): 306–312. [DOI] [PubMed] [Google Scholar]
- 18.Ignarro L.J., Napoli C., Loscalzo J. Nitric oxide donors and cardiovascular agents modulating the bioactivity of nitric oxide: an overview. Circ Res. 2002; 90(1): 21–28. [DOI] [PubMed] [Google Scholar]
- 19.Jun H.W., Taite L.J., West J.L. Nitric oxide-producing polyurethanes. Biomacromolecules. 2005; 6(2): 838–844. [DOI] [PubMed] [Google Scholar]
- 20.Zhou Z., Meyerhoff M.E. Polymethacrylate-based nitric oxide donors with pendant N-diazeniumdiolated alkyldiamine moieties: synthesis, characterization, and preparation of nitric oxide releasing polymeric coatings. Biomacromolecules. 2005; 6(2): 780–789. [DOI] [PubMed] [Google Scholar]
- 21.Miranda K.M., Katori T., Torres de Holding C.L. et al. Comparison of the NO and HNO donating properties of diazeniumdiolates: primary amine adducts release HNO in vivo. J Med Chem. 2005; 48(26): 8220–8228. [DOI] [PubMed] [Google Scholar]
- 22.Drago R., Karstetter B. The reaction of nitrogen(II) oxide with various primary and secondary amines. J Am Chem Soc. 1961; 83(3): 1819–1822. [Google Scholar]
- 23.Keefer LK; From laboratory curiosity to broad-spectrum biomedical advances: fifty years of diazeniumdiolate research. From laboratory curiosity to broad-spectrum biomedical advances. ACS Chem Biol. 2011; 6(11): 1147–1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reynolds M.M., Annich G.M. The artificial endothelium. Organogenesis. 2011; 7(1): 42–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vaughn M.W., Kuo L., Liao J.C. Estimation of nitric oxide production and reaction rates in tissue by use of a mathematical model. Am J Physiol. 1998; 274(6 Pt 2): H2163–H2176. [DOI] [PubMed] [Google Scholar]
- 26.Radomski M.W., Palmer R.M., Moncada S. The role of nitric oxide and cGMP in platelet adhesion to vascular endothelium. Biochem Biophys Res Commun. 1987; 148(3): 1482–1489. [DOI] [PubMed] [Google Scholar]
- 27.Batchelor M.M., Reoma S.L., Fleser P.S. et al. More lipophilic dialkyldiamine-based diazeniumdiolates: synthesis, characterization, and application in preparing thromboresistant nitric oxide release polymeric coatings. J Med Chem. 2003; 46(24): 5153–5161. [DOI] [PubMed] [Google Scholar]
- 28.Mowery K.A., Schoenfisch M.H., Saavedra J.E., Keefer L.K., Meyerhoff M.E. Preparation and characterization of hydrophobic polymeric films that are thromboresistant via nitric oxide release. Biomaterials. 2000; 21(1): 9–21. [DOI] [PubMed] [Google Scholar]
- 29.Taite L.J., Yang P., Jun H.W., West J.L. Nitric oxide-releasing polyurethane-PEG copolymer containing the YIGSR peptide promotes endothelialization with decreased platelet adhesion. J Biomed Mater Res B Appl Biomater. 2008; 84(1): 108–116. [DOI] [PubMed] [Google Scholar]
- 30.Nablo B.J., Prichard H.L., Butler R.D., Klitzman B., Schoenfisch M.H. Inhibition of implant-associated infections via nitric oxide release. Biomaterials. 2005; 26(34): 6984–6990. [DOI] [PubMed] [Google Scholar]
- 31.Zhou Z., Meyerhoff M.E. Preparation and characterization of polymeric coatings with combined nitric oxide release and immobilized active heparin. Biomaterials. 2005; 26(33): 6506–6517. [DOI] [PubMed] [Google Scholar]
- 32.Charville G.W., Hetrick E.M., Geer C.B., Schoenfisch M.H. Reduced bacterial adhesion to fibrinogen-coated substrates via nitric oxide release. Biomaterials. 2008; 29(30): 4039–4044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Reynolds M.M., Hrabie J.A., Oh B.K. et al. Nitric oxide releasing polyurethanes with covalently linked diazeniumdiolated secondary amines. Biomacromolecules. 2006; 7(3): 987–994. [DOI] [PubMed] [Google Scholar]
- 34.Wu B., Gerlitz B., Grinnell B.W., Meyerhoff M.E. Polymeric coatings that mimic the endothelium: combining nitric oxide release with surface-bound active thrombomodulin and heparin. Biomaterials. 2007; 28(28): 4047–4055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhao J., Tu M., Zeng R., Geng J., Cha Z., Zhou C. Study on preparation and properties of nitric oxide releasing polyurethane. 2009; 610-613(2): 1237–1243. [Google Scholar]
- 36.Coneski P.N., Schoenfisch M.H. Synthesis of nitric oxide-releasing polyurethanes with S-nitrosothiol-containing hard and soft segments. Polmer Chemistry. 2011; 2: 906–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Reynolds M.M., Saavedra J.E., Showalter B.M. et al. Tailored synthesis of nitric oxide-releasing polyurethanes using O-protected diazeniumdiolated chain extenders. J Mater Chem. 2010; 20(15): 3107–2114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Puiu S.C., Zhou Z., White C.C. et al. Metal ion-mediated nitric oxide generation from polyurethanes via covalently linked copper(II)-cyclen moieties. J Biomed Mater Res B Appl Biomater. 2009; 91(1): 203–212. [DOI] [PubMed] [Google Scholar]
- 39.Merkel T.C., Bondar V.I., Nagai K., Freeman B.D., Pinnau I. Gas sorption, diffusion and permeation in poly(dimethylsiloxane). J Polym Sci B: Polym Sci. 1991; 38(3): 415–424. [Google Scholar]
- 40.Pauly S. Permeability and diffusion data. 4th ed. New York: Wiley; 1999. [Google Scholar]
- 41.Tsikas D. Analysis of nitrite and nitrate in biological fluids by assays based on the Griess reaction: appraisal of the Griess reaction in the L-arginine/nitric oxide area of research. J Chromatogr B Analyt Technol Biomed Life Sci. 2007; 851(1-2): 51–70. [DOI] [PubMed] [Google Scholar]
- 42.Gunatillake P.A., Meijs G.F., McCarthy S.J., Adhikari R. Poly(dimethylsiloxane)/poly(hexamethylene oxide) mixed macrodiol based polyurethane elastomers. I. Synthesis and properties. J Appl Polym Sci. 2000; 76(14): 2026–2040. [Google Scholar]
- 43.Martin D.J., Warren L.A., Gunatillake P.A., McCarthy S.J., Meijs G.F., Schindhelm K. Polydimethylsiloxane/polyether-mixed macrodiol-based polyurethane elastomers: biostability. Biomaterials. 2000; 21(10): 1021–1029. [DOI] [PubMed] [Google Scholar]
- 44.Hahn A., Brandes G., Wagener P., Barcikowski S. Metal ion release kinetics from nanoparticle silicone composites. J Control Release. 2011; 154(2): 164–170. [DOI] [PubMed] [Google Scholar]
- 45.Higuchi T. Mechanism of sustained-action medication: theoretical analysis of rate of release of solid drugs dispersed in solid matrices. J Pharm Sci. 1963; 52(12): 1145–1149. [DOI] [PubMed] [Google Scholar]
- 46.Ritger P.L., Peppas N.A. A simple equation for description of solute release: I. Fickian and non-fickian release from nonswellable devices in the form of slabs, spheres, cylinders or discs. J Control Release. 1987; 5(1): 23–36. [PubMed] [Google Scholar]
- 47.Verma S., Marsden P.A. Nitric oxide-eluting polyurethanes: vascular grafts of the future? N Engl J Med. 2005; 353(7): 730–731. [DOI] [PubMed] [Google Scholar]


