Abstract
Background:
Itch is common and often debilitating. Itch is best assessed by self-report, often using patient-reported outcome measures (PROMs). Current PROMs for itch are limited and may not capture its full impact on quality of life (QOL).
Purpose:
We sought to develop a comprehensive conceptual model of itch to improve the understanding of itch for clinicians and to serve as a framework for development of efficient and valid PROMs of itch.
Methods:
Using mixed methods, including systematic review (n=491 manuscripts), semi-structured interviews (n=33 adults with chronic itch with multiple etiologies), and grounded theory using a constant comparative approach, we developed a conceptual model of itch.
Results:
We found the Wilson and Cleary model to be a reasonable framework for organizing our findings. It includes five primary components: biological and physiological variables, symptom status, functional status, general health perceptions, and QOL. We propose a causal relationship beginning with the biological and physiological driving factors, with direct and indirect impacts of itch and its sequelae, including pain and sleep disturbance. These can impair function, lead to task avoidance, stigma, social life and relationship problems, emotional disturbances and treatment burden. Together, these sequelae alter one’s perceptions of health, QOL and treatment response.
Conclusions:
Our conceptual model demonstrates the profound patient-burden of itch and identifies unmet needs in the evaluation and management of itch.
1. Introduction
Itch (or pruritus) is a common symptom encountered in dermatology [1], general internal medicine [2] and geriatrics [3]. Itch is a reported symptom in approximately 1% of all outpatient visits in the United States [4] and 0.6% of encounters in Australia [5]. Multiple medical disorders are associated with varying degrees of itch, such as primary sclerosing cholangitis, and renal failure [6, 7]. Itch is associated with significant impairment of patient-reported quality of life (QOL), physical and mental health, ability to carry out every day physical activities, difficulties with social activities and relationships, and higher rates of depressed mood and anhedonia [2].
Itch is a subjective symptom defined as an uncomfortable sensation on the skin that causes a desire to scratch [8]. There are no biomarkers or well-accepted diagnostic tests available to assess the severity of itch. Itch is best assessed using patient-reported outcomes (PRO). Itch is a heterogeneous symptom, analogous to pain, with varying characteristics, such as intensity, quality, frequency, duration, and interference with function [9, 10]. Commonly employed assessments of itch quantify its overall intensity or severity. However, some of these approaches have not been validated, and none capture the full spectrum of itch characteristics or the impact of itch on QOL [10]. There are PRO measures (PROMs) of itch that assess the patient experience, but they can be limited by limited evidence of validity, reliability, incomplete representation of the burden of itch, lack of demonstration of cross-cultural validity, length not easily shortened due to scoring requirements, and/or unclear instructions, scoring and interpretability [10].
As a first step in developing a valid, comprehensive itch PROM, we sought to create a conceptual model of itch. A conceptual model is a theoretical representation which defines the concepts of interest, their interfaces, and possible determinants [11]. In developing PROMs of itch, it is important that the instruments be: 1) relevant and meaningful to patients; 2) conceptually grounded in the many factors at play in the experience of itch; and 3) embedded within a specific conceptual model that indicates the relationship between itch characteristics, disability and QOL. A previous conceptual model was developed by Verhoeven for itch based on a literature review [12]. However, this model was based on a biopsychosocial model, which has a number of limitations [13], including emphasis on psychosocial aspects over the complex physiological aspects of itch. Additional frameworks to guide measuring itch have been developed based on expert consensus of international itch experts. These approaches did not include patient involvement or feedback, instead assuming that all important aspects of measuring itch were already known and/or published. However, there remain many knowledge and practice gaps in the assessment and management of itch [14]. In the present study, we used a grounded theory (GT) approach to develop a conceptual model of itch. GT uses the empirical data to generate concepts and theories, rather than starting with existing hypotheses, models, frameworks or potentially biased a priori assumptions [15]. GT employs a systematic approach to generate concepts from the empirical data. We incorporated extensive patient and expert feedback, as well as previous research and knowledge about itch via a systematic review to develop a comprehensive conceptual model of itch that would improve the understanding of itch for clinicians and serve as a framework for efficient and valid PROMs of pruritus.
2. Methods
This study was approved by the local institutional review board at Northwestern University. The conceptual framework was developed utilizing mixed research methods, with an iterative approach to data collection, synthesis, and analysis.
2.1. Expert input
We first identified key concepts closely linked to itch and its treatment. We employed a panel of eight experts to evaluate our concept elicitation process. The panel included two adult dermatologists, a pediatric dermatologist, four measurement experts with qualitative research experience, and one cross-cultural expert. The panel addressed contextual questions relating to the burden of AD, and practical questions relating to the structure of the patient interview, design of a semi-structured interview guide intended for in-person interviews, including review of interview questions and probes to enhance relevance and fit to the clinical setting of chronic itch. In October 2014, experts participated in up to 10 face-to-face and/or telephone meetings to contribute to the development of the interview guide. The expert panel discussed and refined the draft patient interview guide, and consensus was achieved by discussion. For each of the key concepts and structure of the interview guide, consensus was considered achieved if 7 of 8 on the panel were in agreement.
2.2. Semi-structured patient interviews
To refine and focus the concepts identified by our expert panel, and explore additional concepts relevant to patients, we conducted individual semi-structured interviews (interview guide presented in Supplemental materials) with adults (≥18 years) suffering from chronic itch across multiple etiologies (Table 1). Based on the principles of GT, there was no a priori hypothesis, and sample size is best determined by saturation (i.e. when no new relevant concepts are elicited) rather than a formal power analysis. Sample size consideration was based on previous research suggesting that 6-12 interviews are typically required for theoretical saturation [16-18]. We worked within that range in selection of 8 experts, but chose to oversample patients (n=33) for semi-structured interviews, to ensure adequate representation of the range of etiologies and severities of pruritic dermatologic disorders, as well as uremic pruritus, generalized idiopathic pruritus and rheumatologic disease. Patients with chronic itch were identified and recruited by medical team members from dermatology, rheumatology, nephrology, and oncology within a large Midwestern teaching hospital system.
Table 1.
Underlying etiologies of chronic itch in persons undergoing open-ended.
| Etiology | Frequency |
|---|---|
|
Open ended interviews (n=33) | |
| Atopic dermatitis / Atopic eczema | 4 |
| Prurigo nodularis – atopic variant | 1 |
| Lichen simplex chronicus | 1 |
| Contact dermatitis | 3 |
| Mycosis fungoides / cutaneous T cell lymphoma | 10 |
| Sezary syndrome | 1 |
| Chronic urticaria | 1 |
| Systemic sclerosis | 4 |
| CREST syndrome | 1 |
| Morphea | 1 |
| Lamellar ichthyosis | 3 |
| Generalized idiopathic pruritus | 1 |
| Chronic renal failure | 3 |
Two experienced interviewers conducted face-to-face individual interviews, which were audio recorded. Audio recordings of interviews were transcribed verbatim, excluding identifying information and were analyzed by three coders. The coding team convened to generate a list of themes that were expressed by interviewees or reflected in currently available literature.
The coding team convened to generate a mutually agreeable list of themes that were expressed by interviewees or reflected in currently available literature and to optimize coding. In addition, the expert panel convened after the first 5 transcripts were coded and initial development of the codebook to further refine coding and finalize the codebook. Using selective coding, constant comparative methodology [19, 20], and information from the extant literature identified in the systematic review (below), the coders identified common themes, created definitions, and developed coding rules regarding specific patient comments. After developing coding rules, thematic analysis was performed in NVivo 10 (QSR International, Burlington, MA) with an overall final concordance of coding concepts between coders of >99%.
The majority of participants were female (69.7%); most had white race/ethnicity (66.7% white, 15.2% black, 12.1% Asian, and 6.1% Hispanic). Ages ranged from 22-74 years (mean 53.7 years) and highest educational attainment included high school (45.4%), college (39.4%), and advanced degree (15.2%).
2.3. Systematic review
Once the key concepts were identified by the expert panel, we conducted a systematic literature review concurrently with the qualitative research. The goals of the systematic review were to identify and examine existing concepts related to presentation and burden of itch, and the results previously described [21]. MEDLINE, Embase and Cochrane Library were searched from start to February 1st, 2015 for a combination of‘prurit*’/‘itch*’ (*=wildcard character) and ‘quality of life’/‘QOL’/‘patient burden’/‘patient reported outcome’/‘patient report’/‘patient perspective’/‘patient centered’. Studies were excluded based on the title and/or abstract if there was no indication they investigated or discussed pruritus and/or its impact on QOL. Therapeutic trials, animal studies, and foreign language articles were excluded. Two reviewers (PD and RK), performed the title/abstract review and data extraction, and differences were resolved by discussion.
2.4. Thematic analysis and saturation
Patient interview transcripts and results of the systematic review were coded and thematic analysis was performed by at least 2 coders using NVivo 10, with resolution of disagreements by discussion and consensus. Using constant comparative logic, coding categories were continually refined by collapsing redundant categories and removing irrelevant categories. Saturation - the extent to which no new relevant information was obtained – was assessed beginning with the 12th interview. Data saturation was captured using a saturation grid, as judged by replication and redundancy [16] of themes and sub-themes. Saturation was achieved when three consecutive interviews occurred without producing a new, relevant concept.
2.5. Thematic review
Themes identified in the open-ended interviews and systematic review were reviewed by the expert panel. The panel reviewed and further organized the themes into meaningful units. These were further grouped into broader concepts, which became the foundation of the itch-specific conceptual model. The panel also reviewed the concepts for their relevance and fit to the clinical setting of chronic itch. A Microsoft Excel (Microsoft, Tacoma, WA) database was created for concept review, which yielded 12 final conceptual categories.
2.6. Drafting an itch-specific conceptual model
To organize our findings, we used the basic framework proposed by Wilson and Cleary [22], for the itch-specific conceptual model. It includes five primary components: biological and physiological variables, symptom status, functional status, general health perceptions, and HRQOL. This model was a useful foundation for our itch-specific model, because it encompassed all of the domains reflected in our qualitative findings. We modified the model to include considerations specific to chronic itch, based on the qualitative findings for patients with chronic itch, in addition to the expert panel, and systematic literature review findings.
3. Results
3.1. Expert panel
Eight distinct concepts were identified and agreed upon by our expert panel: a) how patients describe their itch; b) general impact of itch on quality of life; c); emotional impacts of itch; d) social impacts of itch; e) functional limitations; f) impact on sleep; g) side effects of treatments for itch; and h) any concerns regarding treatment for itch.
3.2. Patient interviews
We conducted semi-structured interviews with 33 adults suffering from chronic itch across multiple etiologies (Table 1). We hypothesized there are differences in the characteristics and QOL impact associated with different etiologies of itch. Therefore, we interviewed patients with a range of etiologies to ensure comprehensive capture of itch experiences and concepts. Saturation was achieved at 31 interviews. Patient descriptions of itch are detailed below.
3.3. Systematic review
The systematic literature search yielded 1889 articles, of which 491 contained at least one concept related to itch, including 24 original research studies (n=24) and multiple prior models and frameworks of itch. A full list of relevant articles is available in the Supplemental Results section. Original articles and review articles produced 366 and 1,669 distinct nested concepts, respectively.
We identified 10 general concepts, most with multiple nested concepts: emotional effects (23 nested concepts), functional limitations (10 nested concepts), relationship-social effects, sleep impairment, physical manifestations of itch (15 nested concepts), exacerbating factors (10 nested concepts), self-consciousness and embarrassment, temporal aspects (11 nested concepts), treatment-related concerns (8 nested concepts), and other miscellaneous concerns related to itch. After completion of coding all interview transcripts and manuscripts from the systematic review, themes identified were reviewed and further organized by the expert panel.
3.4. Itch-specific conceptual model
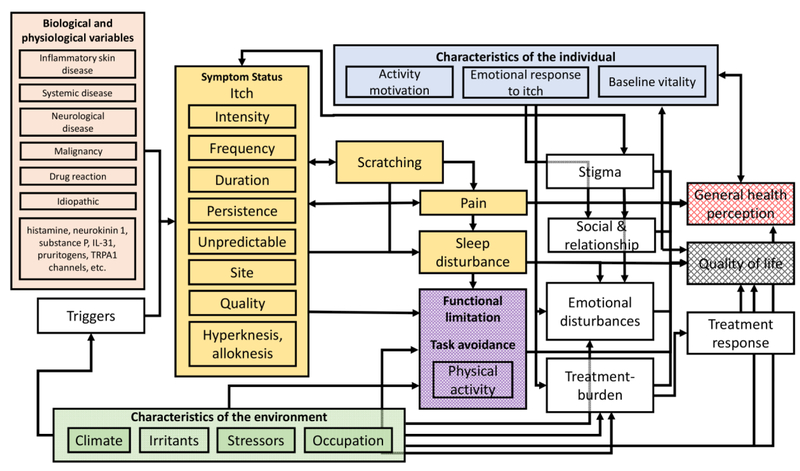
The expert input, patient interviews, and literature review informed development of the conceptual model. Our itch-specific conceptual model is modified from the model proposed by Wilson and Cleary [22] and hypothesizes a causal relationship beginning with biological and physiological variables, with direct and indirect impacts of itch and its sequelae, including pain and sleep disturbance. These in turn impair function, lead to task avoidance, stigma, social life and relationship impacts, emotional disturbances, and treatment burden. All of these may directly and/or indirectly impact one’s perceptions of health, HRQOL, and treatment response (Figure 1). The conceptual model is described in detail below.
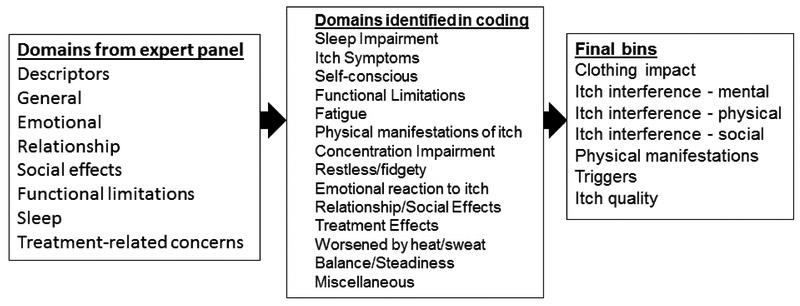
Figure 1.
Itch-related domains identified by the expert panel, selective coding and constant comparative methods, and final bins.
3.5. Biological and physiological variables
The “biological and physiological variables” component of the model, includes the various etiologies and triggers of chronic itch, including inflammatory skin disease (e.g. atopic dermatitis; psoriasis), systemic disease (e.g. liver and renal disorders), neurological disorders (e.g. brachioradial pruritus), medication induced itch (e.g. opioids and adverse events with other medications), itch associated with burns, and idiopathic itch. Many different peripheral and central mechanisms of itch have been implicated across various etiologies [23]. There is a complex interplay of these mechanisms that predisposes to itch and increases susceptibility to exogenous stimuli. These etiologies are relevant in the clinical evaluation and management of patients with chronic itch. However, the mechanisms underlying itch in these disorders are not well understood. Therefore, this component of the conceptual model was not a major focus of this work.
3.6. Symptom status
3.6.1. Multiple dimensions of itch
The “symptom status” component of the model, includes the patient experience of itch. The symptom “itch” is characterized by an urge to scratch. Like pain, its experience and effects can be quite varied. Intensity of itch was a primary concern. Patients were also concerned by itch characteristics. Prolonged duration and persistence of the itch were particularly concerning, as patients described “relentless”, “I am afraid that I am going to deal with this for a long time”, “I don’t want it to affect me 24/7”, “it just doesn’t stop itching”, and “I'm concerned that things are going to get worse before it gets better, this is my concern all the time”. Unpredictable flares and recurrences were also a major concern as described by “I am just so upset that this has come back”, “you never know when it’s going to hit you”. Body site of itch was also important, as itch of the genitals and axillae were especially embarrassing to scratch, and itch on the hands and feet led to more functional limitations.
Various combinations of these dimensions of itch had different sequelae. For example, one patient revealed that persistent, moderate-intensity, generalized itch had a more harmful impact than a short-lived intense localized itch by describing, “I used to be able to deal with the really bad itch when it happened some of the time, but now I got a low-grade itch all day and all night and I can’t do anything.” Another patient reported, “it pretty much just affected everything every day because it didn’t matter what time, at some point throughout the day I had to scratch because I was itchy.”
3.6.2. Itch quality and pain
Our qualitative analyses and systematic review revealed that there are different qualities of itch. Twenty seven of 33 subjects described their itch with additional descriptors (Table 2). Multiple patients endorsed that their itch was not superficial. For example, “felt like the itch came from the inside” and “it goes further than just skin deep, it is not just like on the surface.”
Table 2.
Common descriptors and triggers of itch.
| Domain | Sample patient statements |
|---|---|
| Descriptors of itch. | • My skin was painful • The itch was pulsating • My skin felt like it was throbbing • It feels like something is biting my skin • It feels bee-sting like • My skin felt hot • My skin feels tight • I get burning sensations on my fingers • It goes from itching to burning, back and forth • It feels like a shooting pain • I get a shooting sensation • My skin is very sensitive • It feels like crawling things on my skin • It feels like something is crawling on my skin • It feels like red ants on my skin |
| Triggers of itch. | • I get itchy when I'm hot • I get irritable when I'm hot • My itch is set off by sweat • I don’t cook because it worsens my itch • I can’t go somewhere warm because of my itch • Tight clothing aggravates my itch • Fragrances aggravate my itch • I itch when I am bored • Talking about itch makes me itch • Stress triggers my itch • My itch worsens when the weather changes • My itch is worse in the winter • My itch is worse in the summer • My itch is worse in extreme humidity • My itch is worse when the air is dry |
Our qualitative analyses revealed that many patients with chronic itch also experienced pain. For some, the pain only occurred after traumatizing the skin with scratching, rubbing and/or picking the skin in order to alleviate the itch. For others, the pain occurred concomitantly with the itch, even if they did not manipulate the skin.
Some patients with chronic itch may have associated hyperknesis (prolonged and stronger itch to punctate mechanical stimulus) and alloknesis (itch evoked by light touch that is not typically pruritic). This latter symptom may particularly predispose patients to worsening of itch from exogenous and mechanical stimuli in contact with the skin. Patients in our sample reported multiple stimuli that worsened their itch (Table 2).
3.6.3. Scratching
Our qualitative research found that the scratching per se was problematic in all 33 subjects. That is, substantial numbers of patients reported having to stop everything to scratch (n=8) and being unable to stop scratching (n=9), which was embarrassing (n=16) and had direct effects on functional status and HRQOL (n=7). In some patients, concerns related to scratching were even greater than the effects of the itch per se. Of note, while patients reported that scratching provided short-term relief of itch, chronic scratching and rubbing of the skin has been shown to cause a vicious itch-scratch cycle and increase itch long-term [24]. The arrows in the proposed conceptual model depict these relationships (Figure 2).
Figure 2.
Conceptual model of itch. The five primary components of the Wilson and Cleary model are color coded: 1) biological and physiological variables  , 2) symptom status including itch, scratch, pain and sleep disturbance
, 2) symptom status including itch, scratch, pain and sleep disturbance  , 3) functional status including functional limitations and task avoidance
, 3) functional status including functional limitations and task avoidance  , 4) general health perceptions
, 4) general health perceptions  , and 5) health related quality of life
, and 5) health related quality of life  . Additional itch-specific modifications of the model include stigma, social life and relationship problems, emotional disturbances, treatment burden and treatment response. Each of these steps in the model are potentially modified characteristics of the individual including activity motivation, emotional response to itch and baseline vitality
. Additional itch-specific modifications of the model include stigma, social life and relationship problems, emotional disturbances, treatment burden and treatment response. Each of these steps in the model are potentially modified characteristics of the individual including activity motivation, emotional response to itch and baseline vitality  and characteristics of the environment including climate, irritants, stressors and occupation
and characteristics of the environment including climate, irritants, stressors and occupation  .
.
3.6.4. Sleep disturbance
The itch, pain and uncontrollable scratching contribute to sleep disturbance, including inability to fall asleep or stay asleep, frequent and prolonged nighttime awakenings, restless sleep, and difficulty getting up in the morning. These were accompanied by increased day time fatigue and functional impairment.
3.7. Functional status
Functional status includes the myriad effects of chronic itch on physical activities, function and task avoidance. Task avoidance refers to ceasing engagement in certain activities to manage itch onset or worsening. The capacity to tolerate discomfort and personal motivation for a given that activity varies across individuals and will accordingly influence one’s rating of functional capability or limitation. If one’s tolerance threshold is exceeded, he/she may report avoiding activities because of itch.
Our qualitative research found a complex relationship between itch, functional disturbances and task avoidance. Patients reported avoidance of many different tasks that can exacerbate the itch, including physical activity ranging from light to vigorous intensity (n=12), spending time outdoors in warmer weather (n=12), turning on the heat when indoors (n=3), going on vacation (n=3), reading a book (n=6), watching television (n=2), driving (n=2), or other tasks requiring prolonged concentration (n=21), and wearing certain types of clothing (wool or harsh materials, tight fitting, revealing of scratches, occlusive shoes, etc.) (n=16).
For example, many patients reported limiting exercise and other forms of moderate and vigorous physical activity in order to minimize excessive heat and sweating (n=8), which are common triggers of itch [25, 26]. Patients’ clothing choices were impacted in three different ways. First, they avoid clothing that is tight fitting or made of wool or occlusive footwear that can trigger the underlying itch. Second, some patients reported embarrassment from wearing clothing or footwear that reveals the physical manifestations of their scratching the skin, e.g. erosions or prurigo nodules. Third, oozing and bleeding secondary to erosions from intense scratching ruined clothing and linens.
Difficulty concentrating secondary to itch, fatigue, sleep disturbance, and adverse-effects from sedating anti-itch treatments, all contribute to difficulty performing activities of daily living, including difficulty driving a car, shopping, dealing with finances, and even performing simple tasks. These limitations impact patients with itch in all settings. Patients in our sample commonly described impacts in the home, school and work settings.
3.8. Stigma
The “stigma” component, includes the impact of stigmatization related to itch, scratching behavior and the physical manifestations of itch. Our qualitative research revealed that many patients had friends, family members, coworkers and other persons that did not understand them and perceived them as being sick, contagious, dirty, neurotic, crazy, abnormal, etc. For example, some patients described “to be always scratching, you know…people look at you like you have some type of disease or something that is contagious” and “I didn’t want to have anyone judge me because people are quick to think you have something or that you are responsible for whatever you have or that you have some kind of disease.” Patients describing stigma reported lowered self-esteem, increased emotional disturbances, impaired social life and relationships. For example, “I have not gone to church for fear that people might think I have something.”
3.9. Social life and relationships
Many patients reported embarrassment (n=19), self-consciousness (n=29) and stigma (n=4) secondary to scratching behavior and its physical sequelae. That is, patients found the urge to scratch to be so intense that they could not avoid scratching even in a public setting. This then leads to embarrassment when others see them scratching. Patients were frustrated by others, including friends and family, telling them to stop scratching. In addition, patients were embarrassed by the visually apparent physical signs of scratching. Patients had anxiety over the unpredictability of their itch and whether they may develop intense itching during social interactions. Together, all of these concerns led to profound emotional disturbances, a sense of social isolation, avoidance of and strained social interactions with friends, family and coworkers, and avoidance of travel and vacation.
3.10. Emotional disturbances
Almost all patients reported some degree of emotional disturbance (n=30), including sadness, depression, anxiety, agitation, despair, guilt, hopelessness, fear, and panic. Most patients with emotional disturbances reported that these correlated directly with the severity of itch. That is, severe itch (e.g. high intensity; extensive; persistent) was associated with more profound emotional disturbances than milder itch. These emotional disturbances were reported to almost entirely disappear when the itch was well-controlled. For example, “when your skin is broken out and itchy and you’re feeling kind of down and then you put the creams on and everything starts to improve, your mood improves along with that.”
3.11. Treatment related concerns
Our qualitative research identified a substantial burden from treating their itch and other treatment-related concerns. These included stinging and burning from application of topical treatments (n=3), sedation and multiple other adverse-events (e.g. dry mouth, dizziness, gastrointestinal discomfort, headaches, etc.) from oral anti-itch treatments (n=4). Patients were bothered by the inconvenience, lack of feasibility and large amount of time devoted to their skin care regimen (n=12). In addition, patients reported that the greasiness of topical treatments ruined their clothing, pajamas and linens, and was often highly visible and unsightly (n=5). Morning application of topical anti-pruritics, emollients or treatments of the underlying etiology of itch was associated with difficulties getting to school and/or work on time (n=3).
Most patients reported frustration regarding the lack of anti-itch treatments that are immediately effective at reducing itch (n=24). Scratching and rubbing of itchy skin was the most commonly used method for short-term relief of itch. However, some patients reported that the itch was “internal” and that scratching was therefore not effective. Some patients found that local application of ice packs, cold water compresses and/or other cold items within reach was effective at reducing their itch. Beyond these simple approaches, most patients reported that currently available over-the-counter and prescription anti-pruritics were ineffective.
Patients were frustrated by the lack of long-term efficacy of their anti-itch treatments (n=4). For example, patients considered oral corticosteroids to be a “temporary fix” and “it comes back with a vengeance” after discontinuation. Patients considered that the most effective approach for long-term control of itch was to successfully treat the underlying disorder where possible (n=10). However, they were frustrated by the lack of consistently effective treatments targeting the symptom of itch, particularly while awaiting improvement of the underlying etiology of itch and when they had chronic refractory disease.
3.12. Characteristics of the individual
The “characteristics of the individual” component, includes emotional response to itch, baseline vitality and personal preferences for task exertion. Our qualitative research indicated that these characteristics influence the perception of itch, impact on social life, relationships and functional limitation, task avoidance, emotional disturbances, treatment related concerns, and ultimately general health perception and/or QOL. We hypothesized that individual characteristics and differences play an important role in the conceptual model.
In particular, individual differences in motivation were found to influence functional limitation and task avoidance. These differences also influenced patients’ emotional reactions to itch, including anxiety and depression. The baseline activity motivation includes whether a person has a preference toward particular activities, such as going to the gym, clothing decisions, and occupational tasks. For example, we hypothesize that patients who are more sedentary may not be as bothered by their inability to participate in vigorous physical activities. Further, patients with better coping skills and social support may not have as much of a negative impact from itch on their relationships, social life, and may have fewer emotional disturbances.
3.13. Characteristics of the environment
The “characteristics of the environment” component, includes influences of climate, irritants, stress and occupational exposures on itch. Environmental factors often trigger itch, and can have a direct effect upon itch experience and sequelae. Extreme low or high humidity, excess heat, exposure to allergens, irritants and pruritogens from personal care products, home and occupational environment, and/or psychosocial stressors, were described in terms of their impact upon itch characteristics, functional limitations, emotional disturbances, task avoidance, treatment burden, and ultimately treatment response and overall QOL.
3.14. Outcomes
Finally, “general health perceptions”, “quality of life” and “treatment response” were the final outcomes of our conceptual model. These concepts were ultimately driven by all the intermediate steps. General health perceptions that emerged from our qualitative findings included feelings of worry regarding itch as a symptom of worsening or uncontrolled medical disease and as a sign of poor overall health.
4. Discussion
Our conceptual model of itch, guided by the Wilson and Cleary framework, was supported by extensive qualitative input from patients and experts, as well as the scientific literature. The model organizes our understanding of patient-burden, and the QOL impact of itch. Further, the information we gathered identifies multiple unmet needs in the evaluation and management of itch, including proper assessment of itch characteristics and triggers, and QOL impairment secondary to itch.
Our qualitative findings revealed that multiple characteristics of itch were important to patients, including intensity, frequency, duration, persistence, site, quality, and related sensitivity to external stimuli. These characteristics affected other aspects of the model. The multiple descriptors of itch identified in semi-structured interviews are consistent with previous reports [27, 28]. Moreover, an important component of the patient-burden of itch stems from concomitant physical and mental health symptoms that are highly correlated with itch severity, including pain, sleep and emotional disturbances. These related symptoms should routinely be assessed in clinical practice and therapeutic trials for itch, though currently may not be adequately assessed.
Our findings revealed there are myriad endogenous and exogenous exacerbating influences on itch. However, most patients reported only being affected by a small number of triggers, i.e. not all possible triggers are relevant in all patients. It is essential that a patient-centered approach be taken for the evaluation of itch triggers, in order to develop customized and optimized educational strategies to mitigate itch.
Our conceptual model highlights the extensive patient-burden of itch, including functional limitations, task avoidance, social and relationship effects, emotional disturbances and treatment-related concerns. Some concepts elicited in our qualitative analysis have not been elucidated or previously captured in existing PROMs. These results highlight the need for a more comprehensive PROM of itch.
This study has a number of strengths, including use of a GT approach that incorporated extensive input from patients and experts and myriad concepts elicited from a comprehensive literature review, including previous qualitative research studies, existing pruritus assessments, and multiple models and frameworks of itch. There were still multiple new empirical concepts elicited from the semi-structured interviews. The semi-structured interviews included subjects with a broad representation of age, race/ethnicity, gender, and educational level. However, there are some potential limitations. All patients in the semi-structured patient interviews were recruited from a single quaternary care center, though patients resided in 4 different Midwestern states. The sample size of the concept elicitation interviews was consistent with previous qualitative research [17, 18], and we achieved saturation at interview 31. Nevertheless, larger studies are underway to determine whether novel concepts in our model of itch are generalizable to all patients with itch. However, we conducted a systematic review of the literature to reflect the extensive research of itch previously performed. Thus, our conceptual model is both comprehensive and generalizable to the broader itch population.
5. Conclusions
There are currently no biomarkers or diagnostic tests for assessing itch severity. Given the subjective and multidimensional nature of itch, a patient-centered approach is essential to evaluating the symptom-burden and treatment-related concerns. The qualitative input from patients and experts fits well into a new itch-specific conceptual model, which lends itself to future applications in the design of a conceptual framework and PROM. This model represents the relationship between itch and potential critical clinical trial components, such as different etiologies of itch, concomitant pain, sleep and emotional disturbance, functional limitations, stigma, social and relationship effects, and general health perceptions and overall QOL. Our next step is to develop novel instruments, using the PROMIS methodology {PROMIS Network Staff. PROMIS Instrument Development and Validation Scientific Standards (version 2.0). 2013 updated May 2013 [cited; Available from: http://www.healthmeasures.net/images/PROMIS/PROMISStandards_Vers2.0_Final.pdf}, to measure the PRO components of the conceptual model, including the development and testing of large pools (item banks) of questions to measure the characteristics, triggers and QOL impairment secondary to itch, which could be incorporated in clinical trials and practice.
Supplementary Material
Table 3.
Sample concepts elicited from the qualitative interviews.
| Domain | Sample patient statements |
|---|---|
| Effects of itch on emotions. | • Thinking about my itch makes me anxious • I feel panicky when I need to scratch all over • I get nervous that others will see me itching • I get angry because of the itch • Itching makes me feel miserable • I get sad when I am itching • I am depressed all the time because of my itching • Itch makes me upset • I am tired of everybody asking questions about my itching |
| Effects of itch on social life? | • My itch caused me to stay home from church • I talk to my friends about itching • I sit in the back of class to avoid comments • People comment to me about my itch • People stare at me because of my itch • My itch makes other people itch • Itch makes me antisocial • I stay home most of the time because of itch • My itch has made me introverted • People tell me to stop scratching |
| Effects of itch on physical activity? | • I scratch during walking • I will not do any physical activity that causes me to sweat a • I mostly sit • I do as little as possible physically because of my itch • I am not as mobile as I would like because of itch • My itch makes it extremely hard to move around • My itch makes it hard to do even simple tasks • I try to not let the itch stop me from doing what I want to do |
| Effects of itch on sleep? | • I have to catch up on my sleep • I need to take naps because itch disrupts my sleep • I scratch in my sleep • My sleep is not restful because of itch • It takes several hours for me to fall asleep • I toss and turn in bed because of itch • I wish I could sleep longer • I have to get up in the middle of the night to apply lotion |
| Concerns and adverse-effects from treatment of itch? | • Topical medications prevented me from using my hands • The treatment for my itch is inconvenient • The treatment for my itch is frustrating • The treatment for my itch is not effective • I am concerned about side-effects from the treatment of my • The treatment for my itch caused side-effects • I am concerned about the cost of treating my itch • I am annoyed because of the medications to treat my itch • My skin is sticky from applying creams and ointments • The lotions and creams for my skin ruin my clothes • The lotions and creams make my skin greasy • I don’t like being covered in creams |
Key Points.
-
-
A comprehensive conceptual model of itch can provide a framework to improve the understanding of itch for clinicians and the development of improved assessments of itch.
-
-
Using mixed methods, we developed a conceptual model of itch that included biological and physiological variables, symptom status, functional status, general health perceptions, and quality of life.
-
-
Our conceptual model demonstrates the profound patient-burden of itch and identifies unmet needs in the evaluation and management of itch.
Acknowledgments
Funding Support:
This publication was made possible with support from the Agency for Healthcare Research and Quality (AHRQ), grant number K12HS023011, and the Dermatology Foundation.
Abbreviations used:
- PRO
patient reported outcome
- HRQOL
health related quality of life
Footnotes
JI Silverberg had full access to all the data in the study and takes responsibility for the integrity of the data and accuracy of the data analysis.
Study concept and design: JI Silverberg and D Cella
Acquisition of Data: JI Silverberg, C Hickey, P Dalal and R Kantor
Analysis and interpretation of data: JI Silverberg, C Hickey, P Dalal, K Kaiser, JS Lai, R Kantor, S Shaunfield, D Cella
Drafting of the manuscript: JI Silverberg, JS Lai, D Cella
Critical revision of the manuscript for important intellectual content: JI Silverberg, JS Lai, R
Kantor, S Shaunfield, D Cella, K Kaiser, C Hickey, P Dalal
Statistical analysis: JI Silverberg
Obtained funding: JI Silverberg and D Cella
Administrative technical or material support: None
Study supervision: None
Financial disclosures: None
Design and conduct of the study? No
Collection, management, analysis and interpretation of data? No
Preparation, review, or approval of the manuscript? No
Decision to submit the manuscript for publication? No
Conflicts of interest: JI Silverberg, JS Lai, RW Kantor, S Shaunfield, Kaiser K, D Cella, C Hickey, P Dalal have no relevant conflicts of interest to declare.
References
- 1.Verhoeven EW, Kraaimaat FW, van de Kerkhof PC, van Weel C, Duller P, van der Valk PG, et al. Prevalence of physical symptoms of itch, pain and fatigue in patients with skin diseases in general practice. The British journal of dermatology. 2007. June;156(6):1346–9. [DOI] [PubMed] [Google Scholar]
- 2.Silverberg JI, Hinami K, Trick WE, Cella D. Itch in the General Internal Medicine Setting: A Cross-Sectional Study of Prevalence and Quality-of-Life Effects. American journal of clinical dermatology. 2016. December;17(6):681–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Valdes-Rodriguez R, Mollanazar NK, Gonzalez-Muro J, Nattkemper L, Torres-Alvarez B, Lopez-Esqueda FJ, et al. Itch Prevalence and Characteristics in a Hispanic Geriatric Population: A Comprehensive Study Using a Standardized Itch Questionnaire. Acta dermato-venereologica. 2014. September 9. [DOI] [PubMed] [Google Scholar]
- 4.Shive M, Linos E, Berger T, Wehner M, Chren MM. Itch as a patient-reported symptom in ambulatory care visits in the United States. Journal of the American Academy of Dermatology. 2013. October;69(4):550–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Britt H, Pan Y, Miller GC, Valenti L, Charles J, Knox S, et al. Presentations of 'itch' in Australian general practice. Australian family physician. 2004. July;33(7):488. [PubMed] [Google Scholar]
- 6.Gotthardt DN, Rupp C, Bruhin M, Schellberg D, Weiss KH, Stefan R, et al. Pruritus is associated with severely impaired quality of life in patients with primary sclerosing cholangitis. European journal of gastroenterology & hepatology. 2014. December;26(12):1374–9. [DOI] [PubMed] [Google Scholar]
- 7.Susel J, Batycka-Baran A, Reich A, Szepietowski JC. Uraemic pruritus markedly affects the quality of life and depressive symptoms in haemodialysis patients with end-stage renal disease. Acta dermato-venereologica. 2014. May;94(3):276–81. [DOI] [PubMed] [Google Scholar]
- 8.Waite M, Soanes C. Pocket Oxford English dictionary. Eleventh edition ed. Oxford: Oxford: University Press; 2013. [Google Scholar]
- 9.Elman S, Hynan LS, Gabriel V, Mayo MJ. The 5-D itch scale: a new measure of pruritus. The British journal of dermatology. 2010. March;162(3):587–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schoch D, Sommer R, Augustin M, Stander S, Blome C. Patient-Reported Outcome Measures in Pruritus: A Systematic Review of Measurement Properties. The Journal of investigative dermatology. 2017. October;137(10):2069–77. [DOI] [PubMed] [Google Scholar]
- 11.Earp JA, Ennett ST. Conceptual models for health education research and practice. Health Educ Res 1991. June;6(2):163–71. [DOI] [PubMed] [Google Scholar]
- 12.Verhoeven EW, de Klerk S, Kraaimaat FW, van de Kerkhof PC, de Jong EM, Evers AW. Biopsychosocial mechanisms of chronic itch in patients with skin diseases: a review. Acta dermato-venereologica. 2008;88(3):211–8. [DOI] [PubMed] [Google Scholar]
- 13.Benning TB. Limitations of the biopsychosocial model in psychiatry. Adv Med Educ Pract 2015;6:347–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Silverberg JI. Practice Gaps in Pruritus. Dermatol Clin. 2016. July;34(3):257–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Glaser BG. Theoretical sensitivity : advances in the methodology of grounded theory. Mill Valley, Calif: Sociology Press; 1978. [Google Scholar]
- 16.Bowen GA. Naturalistic inquiry and the saturation concept: a research note. Qualitative Research. 2008;8(1):137–52. [Google Scholar]
- 17.Lamoureux RE, Shields A, Stokes J, Yaworsky A, Galipeau N. How many subjects are enough for symptom-focused concept elicitation studies? A retrospective analysis of saturation across twenty-six studies. Value in Health. 2015;18(3):A33. [Google Scholar]
- 18.Guest G, Bunce A, Johnson L. How Many Interviews Are Enough?: An Experiment with Data Saturation and Variability. Field Methods. 2006. 2006/02/01;18(1):59–82. [Google Scholar]
- 19.Basch CE, DeCicco IM, Malfetti JL. A focus group study on decision processes of young drivers: reasons that may support a decision to drink and drive. Health Educ Q. 1989. Fall;16(3):389–96. [DOI] [PubMed] [Google Scholar]
- 20.Basch CE. Focus group interview: an underutilized research technique for improving theory and practice in health education. Health Educ Q. 1987. Winter;14(4):411–48. [DOI] [PubMed] [Google Scholar]
- 21.Kantor R, Dalal P, Cella D, Silverberg JI. Research letter: Impact of pruritus on quality of life-A systematic review. Journal of the American Academy of Dermatology. 2016. November;75(5):885–6 e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA : the journal of the American Medical Association. 1995. January 04;273(1):59–65. [PubMed] [Google Scholar]
- 23.Dhaka A, Viswanath V, Patapoutian A. Trp ion channels and temperature sensation. Annu Rev Neurosci. 2006;29:135–61. [DOI] [PubMed] [Google Scholar]
- 24.Stander S, Steinhoff M, Schmelz M, Weisshaar E, Metze D, Luger T. Neurophysiology of pruritus: cutaneous elicitation of itch. Archives of dermatology. 2003. November;139(11):1463–70. [DOI] [PubMed] [Google Scholar]
- 25.Chrostowska-Plak D, Salomon J, Reich A, Szepietowski JC. Clinical aspects of itch in adult atopic dermatitis patients. Acta dermato-venereologica. 2009;89(4):379–83. [DOI] [PubMed] [Google Scholar]
- 26.Williams JR, Burr ML, Williams HC. Factors influencing atopic dermatitis-a questionnaire survey of schoolchildren's perceptions. The British journal of dermatology. 2004. June;150(6):1154–61. [DOI] [PubMed] [Google Scholar]
- 27.Majeski CJ, Johnson JA, Davison SN, Lauzon CJ. Itch Severity Scale: a self-report instrument for the measurement of pruritus severity. The British journal of dermatology. 2007. April;156(4):667–73. [DOI] [PubMed] [Google Scholar]
- 28.Darsow U, Scharein E, Simon D, Walter G, Bromm B, Ring J. New aspects of itch pathophysiology: component analysis of atopic itch using the 'Eppendorf Itch Questionnaire'. International archives of allergy and immunology. 2001. Jan-Mar;124(1–3):326–31. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.