Abstract
Purpose:
In vitro and animal models suggest the physiological effects of sleep apnea could contribute to cancer risk, yet epidemiologic studies have been inconsistent.
Methods:
We identified a cohort of adults diagnosed with sleep apnea between 2005–2014 using regional administrative databases. Linking this cohort to a population-based cancer registry, we identified first incident cancers diagnosed after sleep apnea diagnosis through 2015. We calculated age-sex standardized cancer incidence ratios (SIRs) to compare the observed number of cancers among those with sleep apnea with expected population estimates over a comparable period.
Results:
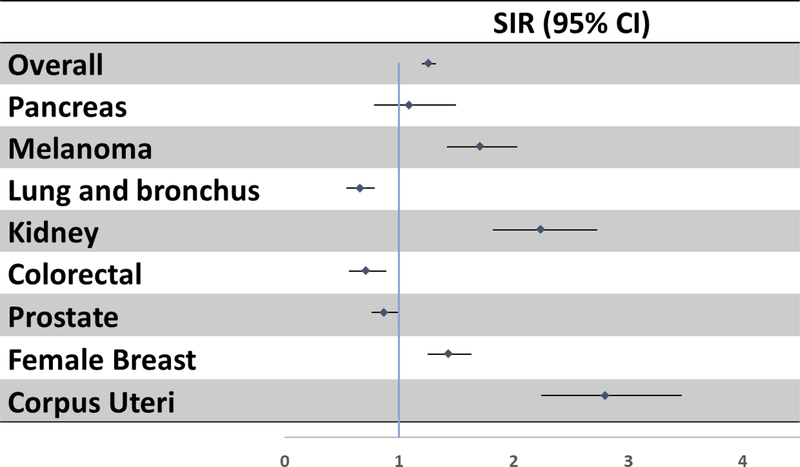
Among 34,402 individuals with sleep apnea, 1,575 first incident cancers were diagnosed during follow-up (mean±SD; 5.3±2.0 years). Compared to the general population, cancer incidence (SIR=1.26, 95% CI: 1.20–1.32) was elevated among sleep apnea patients. We observed significantly elevated incidence for kidney (SIR=2.24, 95% CI=1.82–2.72), melanoma (SIR=1.71, 95% CI=1.42–2.03), breast (SIR=1.43, 95% CI=1.76–2.00) and corpus uteri (SIR=2.80, 95% CI=2.24–2.47) while risk for lung (SIR =0.66, 95% CI = 0.54–0.79) and colorectal cancer (SIR = 0.71, 95% CI =0.56–0.89) was lower.
Conclusion:
These findings suggest an elevated cancer burden, particularly at certain sites, among individuals with diagnosed sleep apnea. Results should be interpreted with caution due to unmeasured confounders (e.g., BMI, diabetes).
Keywords: Sleep apnea, intermittent hypoxia, cancer registry, population health, medical records
Introduction:
Sleep apnea is a sleep-related breathing disorder characterized by recurrent cessations of breathing during sleep, afflicting an estimated 25 million US adults.1 These patients have increased risk for Type 2 diabetes, cardiovascular disease, depression, and motor vehicle accidents, as well as substantially elevated healthcare costs.2–8
In recent years, evidence has emerged that sleep apnea may also be a risk factor for cancer development and progression. Both animal and in-vitro cancer models show exposure to intermittent hypoxia and sleep fragmentation, two of the major hallmarks of sleep apnea, could enhance oncogenic pathways.9–24 However, studies on the sleep apnea and cancer relationship in humans is inconsistent. Four retrospective cohort studies show overall cancer incidence rates are higher among those with versus those without sleep apnea,25–28 while two more recent studies show no elevated risk.29,30 Additional studies have found a relationship between sleep apnea and increased cancer mortality.26,31,32
Most prior epidemiologic studies on this potential connection have been limited by only exploring overall malignancy rates or associations with a limited number of specific cancer types. Studies considering specific cancer sites suggest an inverse relationship between sleep apnea and incident colon, rectum, prostate and breast cancers,29 while others have reported increased risk for breast cancer,25,33 cancers of the central nervous system,34 kidney cancer,29 melanoma,29 pancreatic cancer,29 and prostate cancer25 in those with sleep apnea. To investigate gaps and to add to the current evidence regarding potential associations between sleep apnea and specific cancer types, we linked a cohort of individuals with a sleep apnea diagnosis to a population-based cancer registry in the Seattle-Puget Sound region (Western Washington State).
Methods:
Study Design
The study is a retrospective cohort leveraging the University of Washington Medicine (UWM) system and the Cancer Surveillance System (CSS) of Western Washington State; CSS is part of the NCI Surveillance, Epidemiology, and End Results (SEER) Program. The UWM system includes four regional hospitals and an extensive network of primary care neighborhood clinics. The UWM Sleep Center completes >5,000 clinic visits and performs >3,000 sleep studies (polysomnograms and home sleep apnea tests) per year.
Sleep Apnea Ascertainment
We extracted pertinent information from clinical and administrative databases maintained by the UWM system to identify a cohort of adults aged ≥20 years diagnosed with sleep apnea between January 2005 and December 2014 (N=34,402). This cohort included individuals with obstructive and/or central sleep apnea; however, given that obstructive sleep apnea (OSA) (alone, or in combination with elements of central sleep apnea) accounts for the vast majority of sleep apnea cases (>90%),35 our results are most reflective of associations with OSA. We identified sleep apnea diagnoses based on International Classification of Diseases, Ninth Revision, Clinical Modification codes [ICD-9-CM] (codes 327.20, 327.21, 327.23, 327.27, 327.29, 780.51, 780.53 and 780.57). For individuals with multiple sleep apnea diagnoses recorded over the study period, the first such diagnosis was selected as their index diagnosis.
Cancer case ascertainment
Records for individuals diagnosed with sleep apnea in UWM databases were linked to the CSS to ascertain incident cancer diagnoses between January 2005 and December 2015. The CSS collects data on cancer incidence among residents of the 13 counties of Western Washington State. The registry catchment area covers a population of >4 million people, with an average of 19,000 new cancer diagnoses in adults aged 20–79 years each year during our study period.36 The UWM is located within the CSS catchment area.
Linkage to cancer registry records was done via expectation maximization algorithms to compute linkage probability scores for possible record pairs ranked by importance of various personal identifiers (first name, middle name, last name, date of birth, and social security number). Individuals could link to multiple CSS records if they were diagnosed with multiple cancers during the study period; however, our primary analyses were limited to each participant’s first cancer diagnosis during the study period.
We used International Classification of Diseases for Oncology, 3rd edition (ICD-03) codes to categorize cancer sites (Table 1). We used the CSS Summary Stage 2000 coding to classify cancer stage at diagnosis,37 allowing us to group incident cancers as in situ, localized, regional stage, or metastatic disease.
Table 1:
Definition of cancer sites using ICD-0–3 site and morphology codes
| Cancer Sites | ICD-0–3 Site/Morphology |
|---|---|
| Prostate | C619 |
| Pancreas | C250-C254, C257-C259 |
| Melanoma* | C440-C449 / 8720–8790 |
| Kidney | C649 |
| Lung and Bronchus | C340-C343, C348-C349 |
| Female Breast | C500-C506, C508-C509 |
| Corpus Uteri | C540-C543,C548-C549 |
| Colorectal | C209, C180, C182-C189, C199 |
ICD-O-3: International Classification of Diseases for Oncology, 3rd edition
melanoma of the skin
Other variables
Patient characteristics pulled from UWM clinical and administrative databases included: age at sleep apnea diagnosis, sex, race (White, Black and others), Hispanic ethnicity (Hispanic, non-Hispanic) and healthcare utilization. Healthcare utilization was quantified as the total number of healthcare visits to UWM facilities and providers in the five years subsequent to sleep apnea diagnosis, including outpatient clinic visits and inpatient visits.
Statistical Methods
We tabulated the overall and site-specific counts of first incident cancers that occurred after a sleep apnea diagnosis through December 31, 2015. For each member of the sleep apnea cohort, the expected number of person-years of follow-up was computed as the total years between their first sleep apnea diagnosis and cancer diagnosis, death, or end of follow up (December 31, 2015), whichever came first. We calculated age-sex standardized cancer incidence ratios (SIR) to compare the observed number of cancer cases among those with a sleep apnea diagnosis with the number expected based on cancer incidence rates in the underlying population of the Seattle-Puget Sound region over the study period.38 To estimate the expected number of incident cases, we multiplied cancer incidence rates in sex-specific 5-year age and 10-year age categories ( for overall and cancer site-specific analyses, respectively) for the underlying CSS population by the expected person-years in the corresponding age-sex bands of the sleep apnea cohort. The person-time of follow up was distributed according to the person age with respect to each age bands, such that cohort members contributed person-time at risk to different age categories as they aged during follow-up. This allowed aging during follow-up to be accurately reflected in person-years at risk and consequently in the expected number of cancers. Cancer incidence rates for the CSS region were obtained from the SEER*Stat software38 and SIR (including their 95% confidence interval) estimates were calculated using the exact method in Stata 14.0 (College Station, Texas).39
Results:
Baseline characteristics of the UWM sleep apnea cohort are provided in Table 2, both overall (N=34,402) and for those with an incident cancer diagnosis subsequent to their sleep apnea diagnosis (N=1,575) with a total of 181,674 person-years. Overall, the mean age in the sleep apnea cohort was 52 years at the time of sleep apnea diagnosis. The majority of individuals within the cohort were male (57%) and of White race (74%). Individuals with a cancer diagnosis subsequent to sleep apnea diagnosis were slightly older at sleep apnea diagnosis, but were otherwise demographically similar to the overall cohort. The mean duration follow-up after sleep apnea diagnosis was 5.3 ± 2.0 years.
Table 2:
Selected characteristics of sleep apnea cohort from University of Washington Medicine and linked cancer cases, January 1 2005 to December 31 2014
| Characteristics | Total (N=34,402) | Cancer group (n =1575) | ||
|---|---|---|---|---|
| N | % | N | % | |
| Age at sleep apnea diagnosis (years) | ||||
| mean(SD) | 51.6 (13.0) | 58.6 (11.0) | ||
| age group | ||||
| 20–29 | 1,883 | 5.5 | 16 | 1.0 |
| 30–39 | 4,803 | 14.0 | 72 | 4.6 |
| 40–49 | 8,651 | 25.2 | 247 | 15.7 |
| 50–59 | 9,047 | 26.3 | 451 | 28.6 |
| 60–69 | 7,082 | 20.6 | 531 | 33.7 |
| 70–79 | 2,936 | 8.5 | 258 | 16.4 |
| Gender | ||||
| Female | 14,662 | 42.6 | 692 | 43.9 |
| Male | 19,740 | 57.4 | 883 | 56.1 |
| Race | ||||
| White | 25,198 | 73.3 | 1,230 | 78.1 |
| African American/ Black | 2,979 | 8.7 | 131 | 8.3 |
| Asian | 1,686 | 4.9 | 59 | 3.8 |
| Other | 1,349 | 3.9 | 29 | 1.8 |
| Missing | 3,190 | 9.3 | 126 | 8.0 |
| Ethnicity | ||||
| Hispanic | 1,208 | 3.5 | 24 | 1.5 |
| Non-Hispanic | 18,786 | 54.6 | 874 | 55.5 |
| Missing | 14,408 | 41.9 | 677 | 43.0 |
| Clinic Visits in 5 years | ||||
| <=5 visits | 11,279 | 32.79 | 369 | 23.4 |
| 6+ visits | 23,123 | 67.21 | 1,206 | 76.6 |
Selected characteristics of incident cancers in the sleep apnea cohort are reported in Table 3. The median interval between sleep apnea and cancer diagnosis ranged from 1.3 years for kidney cancer to almost 3 years for breast cancer. The most common cancer sites were breast (15%), prostate (13%), melanoma (8%), lung (7%), kidney (6%), colorectal (5%), corpus uteri (5%) and pancreas (3%). With the exception of sex-specific cancers (i.e., breast, corpus uteri, prostate) and melanoma, the distribution of common cancer sites was similar in men and women within the study cohort. Among those diagnosed with cancer after sleep apnea diagnosis, 61% were diagnosed with as early stage disease (In situ/ Localized) versus 50% in the underlying CSS population.
Table 3:
Selected characteristics of incident cancers diagnosed in the University of Washington Medicine sleep apnea cohort, 2005–2014
| Total | Men | Women | |||||
|---|---|---|---|---|---|---|---|
| Median years at risk | Cancers (N=1575) | Cancers (N=883) | Cancers (N=692) | ||||
| n | %* | n | %* | n | %* | ||
| Common cancer sites | |||||||
| Prostate | 2.08 | 207 | 13.1 | 207 | 23.4 | NA | NA |
| Pancreas | 2.64 | 39 | 2.5 | 24 | 2.7 | 15 | 2.2 |
| Melanoma | 2.21 | 129 | 8.2 | 87 | 9.9 | 42 | 6.1 |
| Lung and bronchus | 2.54 | 115 | 7.3 | 60 | 6.8 | 55 | 8.0 |
| Kidney | 1.34 | 100 | 6.4 | 67 | 7.6 | 33 | 4.8 |
| Female breast | 2.88 | 227 | 14.5 | NA | NA | 227 | 32.8 |
| Corpus uteri | 1.40 | 84 | 5.3 | NA | NA | 84 | 12.1 |
| Colorectal | 2.47 | 78 | 5.0 | 46 | 5.2 | 32 | 4.6 |
| Cancer stage | |||||||
| In Situ | 2.28 | 178 | 11.3 | 86 | 9.8 | 92 | 13.3 |
| Localized | 2.06 | 788 | 51.0 | 451 | 51.1 | 337 | 48.6 |
| regional | 2.01 | 265 | 16.8 | 134 | 15.2 | 131 | 18.9 |
| Metastatic | 2.28 | 292 | 18.5 | 179 | 20.3 | 113 | 16.3 |
Percent’s for cancer site do not sum to 100% because less commonly diagnosed cancer sites are not listed or missing stage information
Overall, the incidence of cancer following sleep apnea diagnosis was higher than would be expected based on the general CSS population (SIR=1.26, 95% CI=1.06, 1.21). Cancer incidence was elevated in both men (SIR=1.13, 95% CI=1.06, 1.21) and women (SIR=1.41, 95% CI=1.31, 1.52) with sleep apnea. Of the specific cancer sites evaluated, significantly elevated cancer incidence was noted for kidney cancer (n=100, SIR=2.24, 95% CI=1.82, 2.73) and melanoma (n=129, SIR=1.71, 95% CI=1.42, 2.03). Incidence of these two specific cancer types was similarly elevated in men and in women (Table 4). Conversely, reduced incidence was reported for lung cancer (n=115, SIR = 0.66, 95% CI= 0.65, 0.79) and colorectal cancer (n=78, SIR=0.71, 95% CI=0.56, 0.89) (Table 4), with similar patterns in each gender. In sex-specific analyses, women with a prior sleep apnea diagnosis also experienced strongly elevated incidence for cancers of the corpus uteri (n=84, SIR=2.80, 95% CI=2.24, 3.47) and breast (n=227, SIR=1.43, 95% CI=1.25, 1.63).
Table 4:
Total and sex-specific cancer Standardized Incidence Rate (SIRs) in University of Washington Medicine sleep apnea cohort, overall and by cancer sites, 2005–2014
| Total | Males | Females | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Observed | Expected | SIR (95% CI) | Observed | Expected | SIR (95% CI) | Observed | Expected | SIR (95% CI) | |
| Cancer site | |||||||||
| All sites | 1575 | 1253 | 1.26 (1.20, 1.32) | 883 | 779 | 1.13 (1.06, 1.21) | 692 | 490 | 1.41 (1.31, 1.52) |
| Female Breast | 227 | 159 | 1.43 (1.25, 1.63) | NA | 227 | 159 | 1.43 (1.25, 1.63) | ||
| Prostate | 207 | 238 | 0.87 (0.76, 1.00) | 207 | 238 | 0.87 (0.76, 1.00) | NA | ||
| melanoma | 129 | 76 | 1.71 (1.42, 2.03) | 87 | 50 | 1.76 (1.41, 2.16) | 42 | 28 | 1.52 (1.09, 2.05) |
| Lung and Bronchus | 115 | 175 | 0.66 (0.54,0.79) | 60 | 111 | 0.54 (0.41, 0.69) | 55 | 66 | 0.83 (0.62, 1.08) |
| Kidney | 100 | 45 | 2.24 (1.82, 2.73) | 67 | 34 | 1.96 (1.52, 2.49) | 33 | 13 | 2.61 (1.79, 3.66) |
| Corpus Uteri | 84 | 30 | 2.80 (2.24, 3.47) | NA | 84 | 30 | 2.80 (2.24, 3.47) | ||
| Colorectal | 78 | 110 | 0.71 (0.56, 0.89) | 46 | 70 | 0.66 (0.48, 0.87) | 32 | 41 | 0.78 (0.53, 1.10) |
| Pancreas | 39 | 36 | 1.09 (0.78, 1.50) | 24 | 23 | 1.05 (0.67, 1.56) | 15 | 14 | 1.12 (0.63, 1.85) |
NA: gender specific
When stratified by age, cancer incidence was most elevated among older adults with sleep apnea (age ≥60 years), with evidence of elevated incidence across all evaluated cancer sites (Table 5). Among individuals with sleep apnea aged <60 years, cancer incidence for several sites was lower than expected; however, cancer incidence overall, and the incidence of melanoma, uterine and kidney cancers remained elevated in this younger age group.
Table 5:
Age specific cancer Standardized Incidence Rate (SIRs) in University of Washington Medicine sleep apnea cohort, overall and by cancer sites, 2005–2014
| Age at sleep apnea diagnosis | ||||||
|---|---|---|---|---|---|---|
| <60 y | 60+ y | |||||
| Observed | Expected | SIR (95% CI) | Observed | Expected | SIR (95% CI) | |
| Cancer site | ||||||
| All sites | 786 | 927.9 | 0.85 (0.79, 0.91) | 789 | 325 | 2.43 (2.26, 2.60) |
| Female Breast | 120 | 105.9 | 1.13 (0.94, 1.35) | 107 | 22.1 | 4.85 (3.97, 5.86) |
| Prostate | 74 | 151.4 | 0.49 (0.38, 0.61) | 133 | 51.4 | 2.59 (2.17, 3.07) |
| melanoma | 60 | 48.2 | 1.25 (0.95, 1.61) | 69 | 10.52 | 6.56 (5.10, 8.30) |
| Lung and Bronchus | 39 | 97.6 | 0.40 (0.29, 0.55) | 76 | 38.8 | 1.96 (1.55, 2.45) |
| Kidney | 63 | 27.6 | 2.29 (1.76, 2.93) | 37 | 7.73 | 4.79 (3.37, 6.60) |
| Corpus Uteri | 51 | 20.3 | 2.51 (1.87, 3.30) | 33 | 4.36 | 7.57 (5.21, 1000) |
| Colorectal | 43 | 61.3 | 0.70 (0.51, 0.94) | 35 | 20.6 | 1.70 (1.19, 2.37) |
| Pancreas | 21 | 27.6 | 1.12 (0.69, 1.71) | 18 | 7.7 | 2.34 (1.39, 3.70) |
In addition, the risk of in situ (SIR=5.52, 95% CI =4.74, 6.39), localized (SIR=1.40, 95% CI =1.30, 1.50), regional stage (SIR=1.08, 95% CI =0.96, 1.22) and metastatic (SIR=1.20, 95% CI =1.07, 1.35) cancers were consistently elevated.
Discussion:
In this study, we found overall cancer incidence was about 26% higher in those with a diagnosis of sleep apnea than expected in the general population. More specifically, we observed elevated incidences of kidney, melanoma, uterine, and breast cancers among those with sleep apnea, particularly among older individuals. In contrast, inverse associations were noted with respect to lung and colorectal cancers. These results suggest that sleep apnea may contribute to overall cancer risk, with a more pronounced association on select cancer sites.
Our findings are consistent with prior animal studies and in vitro models demonstrating the carcinogenic potential of intermittent hypoxia and sleep fragmentation, two hallmarks of sleep apnea. Intermittent hypoxia, defined as a temporary deprivation of adequate oxygen, promotes tumor growth and metastasis in melanoma-injected mice12, and has been associated with resistance to radiation in cancer cell lines.18,19,41 Among the suggested mechanisms underlying these effects, chronic intermittent hypoxia has been shown to contribute to the generation of excessive reactive oxygen species (leading to oxidative stress induced DNA damage)10,40,42, sustained activation of inflammatory pathways13,43, alterations in the miRNA cargo of circulating exosomes,10,44 and overexpression of the transcriptional regulator hypoxia-inducible factor-1alpha (HIF-1α).18,45,46 Overexpression of HIF-1α up-regulates proangiogenic mediators, such as Vascular Endothelial Growth Factor (VEGF), thereby stimulating tumor growth, whereas chronic activation of Nuclear factor κB (NFκB) promotes tumorigenesis.18,45–49 In particular, over-expression of HIF-1α enhances angiogenesis in clear cell renal cell carcinoma.50 Persistent sleep fragmentation is also associated with accelerated tumor growth and progression via similar pathways to those recruited by intermittent hypoxia.10,11,13 Therefore, these sleep apnea induced physiologic changes may plausibly contribute to cancer initiation through the creation of a pro-inflammatory and immunosuppressive microenvironment.11,13,16
A number of human studies are consistent with our findings. A 2012 study utilizing the Wisconsin Sleep Cohort noted a 4.8-fold elevation in cancer mortality among individuals with severe OSA relative to those without sleep-disordered breathing.31 Two years later, two other studies using a community-based and clinic-based cohort respectively, reported an elevated cancer mortality in those diagnosed with sleep apnea.26,32 Subsequently, three studies found a significant association between sleep apnea and cancer incidence with risk ratios ranging from 1.7–2.5.25–27 However, more recent studies are inconsistent with these earlier findings. Kendzerska et al., found no significant association with cancer incidence when comparing OSA patients to the general population (HR:1.02; 95% CI 0.80 – 1.31).30 A meta-analysis of the 4 studies including 86,460 participants found no association between overall cancer incidence and sleep apnea (HR 1.04; 95% CI 0.92, 1.16).51 Another meta-analysis including one additional study on breast cancer,33 found an overall elevated risk.52 Both studies noted cautionary interpretation of the results due to possibility of confounding by cancer risk factors, heterogeneity between studies, and the possibility of publication bias.51,52 These prior studies are also summarized in a recent study.53 Additionally, in the largest study to date, Gozal et al., found no association between OSA and overall cancer risk (HR 0.98; 95% CI 0.90–1.00).29
The fact that some prior studies have observed no significant association between sleep apnea and cancer overall may reflect heterogeneity in the relationship of sleep apnea with risk of specific types of cancer. That is, investigations of associations with overall cancer incidence may obscure cancer site-specific associations. Specifically, our study found increased incidence of breast, melanoma, corpus uteri and kidney cancers in patients with sleep apnea. However, we found reduced incidence with respect to lung and colorectal cancer. At least two prior studies also found an increased risk for breast cancer associated with sleep apnea.25,33 In their recent study, Gozal et al., reported no such association with breast cancer; however, they did report elevated incidence of melanoma and kidney cancers and reduced incidence of colorectal cancer among individuals with sleep apnea,29 consistent with our findings.
Furthermore, the sleep apnea and cancer incidence association was stronger in women than in men. However, given that our statistical approach using SIR estimates for men and women involves a different set of weights for each sex, we are unable to assess any potential statistical inference on this gender difference. Additionally, with respect to age, older adults seemed to have higher burden of cancer incidence in this sleep apnea cohort, a finding that has been recently corroborated in a prospective cohort.54 This might imply there are other important risk factors such as genetic susceptibility driving the cancer burden in the younger cohort, whereas sleep apnea remains an important risk factor for the older cohort. However, in a murine model of sleep apnea and lung cancer, old age was protective rather than deleterious, suggesting that type of cancer and age may be interactively implicated along with sleep apnea to modify their epidemiological characteristics.55 Other reasons might be due to differential misclassification of sleep apnea in younger adults, since it is not only generally under-diagnosed in the population, but it is perceived as being more commonly present in older adults, thereby leading to higher proportion of younger subjects remaining undetected. However, incidence of kidney and corpus uteri cancers and melanoma remained elevated in both age groups, which is consistent with the overall estimates.
Lastly, our findings should be interpreted in the context of study limitations. In particular, we lacked data on several potential confounders of the association between sleep apnea and cancer, such as body mass index (BMI), smoking history and socioeconomic status (SES). For instance, being overweight or obese is an established risk factor for kidney, endometrial and breast cancer,56–58 as well as sleep apnea.59 We retrieved BMI information for a random sample of the sleep apnea cohort and observed a high prevalence of obesity (42%) as compared to county-level estimates of adult obesity (22%) for the county in which UWM is located (i.e,. King County). Therefore, it would be expected that the elevated incidence observed for these cancers could be lower if adjusted for BMI. However, based on the fact that other studies adjusting for BMI have also noted increased risk for these cancers associated with sleep apnea,25,29,33 and given that melanoma incidence (also elevated in our study) has not been consistently linked with BMI,60 lack of adjustment for BMI is unlikely to account for the entirety of our results. However, unadjusted BMI, could explain some the association observed with sleep apnea for certain cancer sites such as uterine cancer.61,62 Diabetes, a comorbidity linked with both sleep apnea and cancer, could similarly contribute as an unmeasured confounder.63 Although we posited smoking as another unmeasured confounder, the smoking prevalence (12%) reported in a random sample of the sleep cohort was consistent with rates reported in King County, the largest population of the CSS catchment area64. We also relied on administrative codes for identifying individuals with a sleep apnea diagnosis. It is possible that these codes were entered into medical records as part of a medical history rather than reflecting a primary diagnosis; however, we counted follow-up time from the time of the first recorded sleep apnea code during the study period. Our approach to identifying sleep apnea patients precluded us from distinguishing between mild and severe sleep apnea, potentially limiting the study sensitivity to detect significant associations with overall and specific cancer sites.
There are also some limitations implicit in our estimation of person time at risk. Firstly, although we restricted our investigation to cancers diagnosed after sleep apnea, both sleep apnea and cancer are diseases with latency periods that can span several years or decades prior to diagnosis; thus, we cannot be certain that sleep apnea was present before the initiation of a cancer. However, sensitivity analyses excluding the first year of follow-up after a sleep apnea diagnosis yielded an attenuated (but still significantly elevated) SIR of 1.07 (1.01, 1.14) for cancer overall as well as a consistent direction but attenuated risk for cancer sites.
Lastly, our ascertainment of cancer diagnoses was limited to the 13-county catchment area of the CSS cancer registry. As such, we could have missed other cancers diagnosed if or when individuals with sleep apnea moved outside the 13-county region. In addition, we had a relatively short follow up period (mean =5.3 years); however, other studies with a longer duration of follow-up (>10 years)31,34 have similarly found a putative link between sleep apnea and incidence of a specific cancer or cancer mortality. Furthermore, lumping OSA and CSA into one “sleep apnea” cohort might yield different results if looked at separately due to the pathophysiological differences between these two respiratory sleep disorders. However, given that the majority of our cohort are OSA patients, this is unlikely as also shown by the similar overall cancer incidence estimate when CSA cases are dropped in a sensitivity analysis (SIR: 1.25 vs 1.26).
A strength of our study compared to prior work is our relatively large sample size, which allowed us to evaluate associations with several specific cancer sites.53 We also had the ability to link sleep apnea cases with a population-based cancer registry, allowing for more comprehensive identification of cancer cases in our cohort.
In conclusion, our study suggests that sleep apnea is a potential risk factor for cancer, and that this association likely differs across cancer sites. Given the widespread and highly treatable nature of sleep apnea, these findings may suggest potential opportunities for reducing population cancer burden if these associations were causal.
Figure 1:
Standardized Incidence Ratio (and 95% CI bounds) in sleep apnea cohort relative to the Seattle-Puget Sound region (Cancer Surveillance System).
Acknowledgments
Funding: This work was supported by grant number P30CA015704.
Footnotes
Conflict of Interest: NONE
References
- 1.Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006–1014. doi: 10.1093/aje/kws342 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Acker J, Richter K, Piehl A, Herold J, Ficker J, Niklewski G. Obstructive sleep apnea (OSA) and clinical depression—prevalence in a sleep center. Sleep and Breathing. 2016:1–8. [DOI] [PubMed] [Google Scholar]
- 3.Barger LK, Rajaratnam S, Wang W, OBrien CS, Sullivan JP, Quadri S. Common sleep disorders increase risk of motor vehicle crashes and adverse health outcomes in firefighters. J Clin Sleep Med. 2015;11(3):233–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clark AJ, Salo P, Lange T, et al. Onset of impaired sleep and cardiovascular disease risk factors: A longitudinal study. 2016. [DOI] [PMC free article] [PubMed]
- 5.Covassin N, Somers VK. Sleep apnea, hypertension, and hemorrhagic stroke—déjà vu all over again. Journal of the American Society of Hypertension. 2016;10(3):197–200. [DOI] [PubMed] [Google Scholar]
- 6.Kendzerska T, Gershon AS, Hawker G, Tomlinson G, Leung RS. Obstructive sleep apnea and incident diabetes. A historical cohort study. American journal of respiratory and critical care medicine. 2014;190(2):218–225. [DOI] [PubMed] [Google Scholar]
- 7.Tarasiuk A, Reuveni H. The economic impact of obstructive sleep apnea. Curr Opin Pulm Med. 2013;19(6):639–644. doi: 10.1097/MCP.0b013e3283659e1e [doi]. [DOI] [PubMed] [Google Scholar]
- 8.Kao L, Lee H, Lin H, Tsai M, Chung S. Healthcare service utilization by patients with obstructive sleep apnea: A population-based study. PloS one. 2015;10(9):e0137459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Almendros I, Montserrat JM, Torres M, et al. Intermittent hypoxia increases melanoma metastasis to the lung in a mouse model of sleep apnea. Respiratory physiology & neurobiology. 2013;186(3):303–307. [DOI] [PubMed] [Google Scholar]
- 10.Khalyfa A, Almendros I, Gileles-Hillel A, et al. Circulating exosomes potentiate tumor malignant properties in a mouse model of chronic sleep fragmentation. Oncotarget. 2016. doi: 10.18632/oncotarget.10578 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zheng J, Almendros I, Wang Y, et al. Reduced NADPH oxidase type 2 activity mediates sleep fragmentation-induced effects on TC1 tumors in mice. OncoImmunology. 2015;4(2):e976057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gozal D, Farré R, Nieto FJ. Putative links between sleep apnea and cancer: From hypotheses to evolving evidence. CHEST Journal. 2015;148(5):1140–1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hakim F, Wang Y, Zhang SX, et al. Fragmented sleep accelerates tumor growth and progression through recruitment of tumor-associated macrophages and TLR4 signaling. Cancer Res. 2014;74(5):1329–1337. doi: 10.1158/0008-5472.CAN-13-3014 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nanduri J, Prabhakar NR. Intermittent hypoxia: Mechanistic pathways influencing cancer In: Impact of sleep and sleep disturbances on obesity and cancer. Springer; 2014:103–119. [Google Scholar]
- 15.Miao Z, Zhao T, Wang Z, et al. Influence of different hypoxia models on metastatic potential of SGC-7901 gastric cancer cells. Tumor Biol. 2014;35(7):6801–6808. [DOI] [PubMed] [Google Scholar]
- 16.Zhang J, Guo X, Shi Y, Ma J, Wang G. Intermittent hypoxia with or without hypercapnia is associated with tumorigenesis by decreasing the expression of brain derived neurotrophic factor and miR-34a in rats. Chin Med J (Engl). 2014;127(1):43–47. [PubMed] [Google Scholar]
- 17.Almendros I, Montserrat JM, Ramirez J, et al. Intermittent hypoxia enhances cancer progression in a mouse model of sleep apnoea. Eur Respir J. 2012;39(1):215–217. doi: 10.1183/09031936.00185110 [doi]. [DOI] [PubMed] [Google Scholar]
- 18.Wan J, Chai H, Yu Z, et al. HIF-1α effects on angiogenic potential in human small cell lung carcinoma. Journal of Experimental & Clinical Cancer Research. 2011;30(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu Y, Song X, Wang X, et al. Effect of chronic intermittent hypoxia on biological behavior and hypoxia‐associated gene expression in lung cancer cells. J Cell Biochem. 2010;111(3):554–563. [DOI] [PubMed] [Google Scholar]
- 20.Rofstad EK, Gaustad J, Egeland TA, Mathiesen B, Galappathi K. Tumors exposed to acute cyclic hypoxic stress show enhanced angiogenesis, perfusion and metastatic dissemination. International journal of cancer. 2010;127(7):1535–1546. [DOI] [PubMed] [Google Scholar]
- 21.Toffoli S, Michiels C. Intermittent hypoxia is a key regulator of cancer cell and endothelial cell interplay in tumours. FEBS journal. 2008;275(12):2991–3002. [DOI] [PubMed] [Google Scholar]
- 22.Carmeliet P, Dor Y, Herbert J, et al. Role of HIF-1α in hypoxia-mediated apoptosis, cell proliferation and tumour angiogenesis. Nature. 1998;394(6692):485–490. [DOI] [PubMed] [Google Scholar]
- 23.Shweiki D, Itin A, Soffer D, Keshet E. Vascular endothelial growth factor induced by hypoxia may mediate hypoxia-initiated angiogenesis. Nature. 1992;359(6398):843–845. doi: 10.1038/359843a0 [doi]. [DOI] [PubMed] [Google Scholar]
- 24.Li L, Ren F, Cao J, Chen B. Relevant mechanism of intermittent hypoxia-induced melanoma lung metastases in a murine model of sleep apnea. CHEST Journal. 2016;149(4_S):A556–A556. [Google Scholar]
- 25.Fang H, Miao N, Chen C, Sithole T, Chung M. Risk of cancer in patients with insomnia, parasomnia, and obstructive sleep apnea: A nationwide nested case-control study. Journal of Cancer. 2015;6(11):1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marshall NS, Wong K, Cullen S, Knuiman MW, Grunstein RR. Sleep apnea and 20-year follow-up for all-cause mortality, stroke, and cancer incidence and mortality in the busselton health study cohort. J Clin Sleep Med. 2014;10(4):355–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Campos-Rodriguez F, Martinez-Garcia MA, Martinez M, et al. Association between obstructive sleep apnea and cancer incidence in a large multicenter spanish cohort. American journal of respiratory and critical care medicine. 2013;187(1):99–105. [DOI] [PubMed] [Google Scholar]
- 28.Christensen AS, Clark A, Salo P, et al. Symptoms of sleep disordered breathing and risk of cancer: A prospective cohort study. Sleep. 2013;36(10):1429–1435. doi: 10.5665/sleep.3030 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gozal D, Ham SA, Mokhlesi B. Sleep apnea and cancer: Analysis of a nationwide population sample. Sleep. 2016;39(8):1493–1500. doi: 10.5665/sleep.6004 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kendzerska T, Leung RS, Hawker G, Tomlinson G, Gershon AS. Obstructive sleep apnea and the prevalence and incidence of cancer. CMAJ. 2014;186(13):985–992. doi: 10.1503/cmaj.140238 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nieto FJ, Peppard PE, Young T, Finn L, Hla KM, Farré R. Sleep-disordered breathing and cancer mortality: Results from the wisconsin sleep cohort study. American journal of respiratory and critical care medicine. 2012;186(2):190–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Martinez-Garcia MA, Campos-Rodriguez F, Duran-Cantolla J, et al. Obstructive sleep apnea is associated with cancer mortality in younger patients. Sleep Med. 2014;15(7):742–748. doi: 10.1016/j.sleep.2014.01.020 [doi]. [DOI] [PubMed] [Google Scholar]
- 33.Chang W, Liu M, Chang W, et al. Sleep apnea and the subsequent risk of breast cancer in women: A nationwide population-based cohort study. Sleep Med. 2014;15(9):1016–1020. [DOI] [PubMed] [Google Scholar]
- 34.Chen J, Hwang J. Sleep apnea increased incidence of primary central nervous system cancers: A nationwide cohort study. Sleep Med. 2014;15(7):749–754. [DOI] [PubMed] [Google Scholar]
- 35.Foldvary-Schaefer NR, Waters TE. Sleep-disordered breathing. Continuum (Minneap Minn). 2017;23(4, Sleep Neurology):1093–1116. doi: 10.1212/01.CON.0000522245.13784.f6 [doi]. [DOI] [PubMed] [Google Scholar]
- 36.Surveillance, epidemiology, and end results program (SEER) seattle-puget sound registry https://Seer.cancer.gov/registries/sps.html accessed 5.23.2017.
- 37.Fritz AG, RHIT C, Hurlbut AA, et al. SEER summary staging manual-2000 codes and coding instructions. 2001.
- 38.Surveillance research program, national cancer institute SEER*Stat software (www.seer.cancer.gov/seerstat) version 8.3.4.
- 39.StataCorp. stata statistical software: Release 14 college station, TX: StataCorp LP; 2015. [Google Scholar]
- 40.Almendros I, Gileles-Hillel A, Khalyfa A, et al. Adipose tissue macrophage polarization by intermittent hypoxia in a mouse model of OSA: Effect of tumor microenvironment. Cancer Lett. 2015;361(2):233–239. [DOI] [PubMed] [Google Scholar]
- 41.Akbarpour M, Khalyfa A, Qiao Z, et al. Altered CD8+ T-cell lymphocyte function and TC1 cell stemness contribute to enhanced malignant tumor properties in murine models of sleep apnea. Sleep. 2016. doi: sp-00426-16 [pii]. [DOI] [PubMed] [Google Scholar]
- 42.Reuter S, Gupta SC, Chaturvedi MM, Aggarwal BB. Oxidative stress, inflammation, and cancer: How are they linked? Free Radical Biology and Medicine. 2010;49(11):1603–1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hatfield SM, Kjaergaard J, Lukashev D, et al. Immunological mechanisms of the antitumor effects of supplemental oxygenation. Sci Transl Med. 2015;7(277):277ra30. doi: 10.1126/scitranslmed.aaa1260 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gharib SA, Seiger AN, Hayes AL, Mehra R, Patel SR. Treatment of obstructive sleep apnea alters cancer-associated transcriptional signatures in circulating leukocytes. Sleep. 2014;37(4):709–14, 714A-714T. doi: 10.5665/sleep.3574 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ryan HE, Poloni M, McNulty W, et al. Hypoxia-inducible factor-1alpha is a positive factor in solid tumor growth. Cancer Res. 2000;60(15):4010–4015. [PubMed] [Google Scholar]
- 46.Dewhirst MW. Intermittent hypoxia furthers the rationale for hypoxia-inducible factor-1 targeting. Cancer Res. 2007;67(3):854–855. doi: 67/3/854 [pii]. [DOI] [PubMed] [Google Scholar]
- 47.Wang JQ, Jeelall YS, Ferguson LL, Horikawa K. Toll-like receptors and cancer: MYD88 mutation and inflammation. Front Immunol. 2014;5:367. doi: 10.3389/fimmu.2014.00367 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Madonna G, Ullman CD, Gentilcore G, Palmieri G, Ascierto PA. NF-κB as potential target in the treatment of melanoma. Journal of translational medicine. 2012;10(1):53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li S, Qian X, Zhou W, et al. Time-dependent inflammatory factor production and NFκB activation in a rodent model of intermittent hypoxia. Swiss Med Wkly. 2011;141:w13309. [DOI] [PubMed] [Google Scholar]
- 50.Gudas LJ, Fu L, Minton DR, Mongan NP, Nanus DM. The role of HIF1α in renal cell carcinoma tumorigenesis. Journal of Molecular Medicine. 2014;92(8):825–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang X, Peng L, Lyu Z, Jiang X, Du Y. Obstructive sleep apnoea and the incidence and mortality of cancer: A meta‐analysis. European journal of cancer care. 2017;26(2):e12427. [DOI] [PubMed] [Google Scholar]
- 52.Shantha GPS, Kumar AA, Cheskin LJ, Pancholy SB. Association between sleep-disordered breathing, obstructive sleep apnea, and cancer incidence: A systematic review and meta-analysis. Sleep Med. 2015;16(10):1289–1294. [DOI] [PubMed] [Google Scholar]
- 53.Martinez-Garcia MA, Campos-Rodriguez F, Barbe F. Cancer and OSA: Current evidence from human studies. Chest. 2016;150(2):451–463. doi: 10.1016/j.chest.2016.04.029 [doi]. [DOI] [PubMed] [Google Scholar]
- 54.Martinez-Garcia M, Campos-Rodriguez F, Nagore E, et al. Sleep-disordered breathing is independently associated with increased aggressiveness of cutaneous melanoma. A multicentre observational study in 443 patients. Chest. 2018. [DOI] [PubMed] [Google Scholar]
- 55.Torres M, Campillo N, Nonaka PN, et al. Aging reduces intermittent hypoxia-induced lung carcinoma growth in a mouse model of sleep apnea. American journal of respiratory and critical care medicine. 2018(ja). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wang F, Xu Y. Body mass index and risk of renal cell cancer: A dose‐response meta‐analysis of published cohort studies. International journal of cancer. 2014;135(7):1673–1686. [DOI] [PubMed] [Google Scholar]
- 57.Genkinger JM, Spiegelman D, Anderson KE, et al. A pooled analysis of 14 cohort studies of anthropometric factors and pancreatic cancer risk. International journal of cancer. 2011;129(7):1708–1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Munsell MF, Sprague BL, Berry DA, Chisholm G, Trentham-Dietz A. Body mass index and breast cancer risk according to postmenopausal estrogen-progestin use and hormone receptor status. Epidemiol Rev. 2014;36(1):114–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schwartz AR, Patil SP, Laffan AM, Polotsky V, Schneider H, Smith PL. Obesity and obstructive sleep apnea: Pathogenic mechanisms and therapeutic approaches. Proceedings of the American Thoracic Society. 2008;5(2):185–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shipman A, Millington G. Obesity and the skin. Br J Dermatol. 2011;165(4):743–750. [DOI] [PubMed] [Google Scholar]
- 61.Bjørge T, Engeland A, Tretli S, Weiderpass E. Body size in relation to cancer of the uterine corpus in 1 million norwegian women. International journal of cancer. 2007;120(2):378–383. [DOI] [PubMed] [Google Scholar]
- 62.Bhaskaran K, Douglas I, Forbes H, dos-Santos-Silva I, Leon DA, Smeeth L. Body-mass index and risk of 22 specific cancers: A population-based cohort study of 5 24 million UK adults. The Lancet. 2014;384(9945):755–765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Shi Y, Hu FB. The global implications of diabetes and cancer. Lancet. 2014;383(9933):1947–1948. doi: 10.1016/S0140-6736(14)60886-2 [doi]. [DOI] [PubMed] [Google Scholar]
- 64. [accessed 2/20/2018.]; Https://Www.doh.wa.gov/portals/1/documents/pubs/345-271-ChronicDiseaseProfileKing.pdf.