Abstract
Purpose:
To explore temporal trends in age at first-ever ischemic stroke onset in a bi-ethnic, population-based study.
Methods:
Cases of first-ever ischemic stroke (N=3,252) were identified in the Brain Attack Surveillance in Corpus Christi (BASIC) Project (2000–2012). Demographics and risk factors were abstracted from medical records. Trends in age at stroke onset were assessed overall and by ethnicity (Mexican American (MA) and non-Hispanic white (NHW)) using generalized additive models. Differences by ethnicity were tested by including an interaction term between time and ethnicity. Models were run unadjusted and adjusted for age of the population at-risk for stroke.
Results:
Mean age at first-ever ischemic stroke significantly decreased from an average of 71.7 years in 2000 to an average of 69.3 years in 2012 (p=0.0043). Ethnicity significantly modified the temporal trends (p<0.001) with declines greater in NHWs than in MAs; mean age was estimated to decrease from 74.8 to 71.3 over the 13 years for NHWs, while for MAs, mean age was estimated to decrease from 68.9 to 66.9 after adjusting for ethnic-specific average age of the population at risk.
Conclusions:
Average age at first-ever stroke onset declined over time in this community. Efforts should be made to prevent stroke by controlling risk factors prior to and during midlife.
Keywords: age, ischemic stroke, trends, ethnicity
Introduction
Stroke is the leading cause of adult disability and the fifth leading cause of death in the United States (US).(1) In recent decades, the incidence rate for stroke has declined.(2, 3) However, several studies have reported that this decline is not present in those younger than 65 years of age.(3, 4) Moreover, modest yet significant increases in stroke incidence in the population younger than 55 years have been reported in both the US and Europe.(5, 6) It is possible that these trends in incidence will translate into a lower average age at stroke onset.
Lower average age at stroke onset would have considerable public health implications. As stroke mortality has decreased dramatically over time,(7) especially in those younger than 65 years,(4) strokes in younger persons carry the potential for greater years of disability and lifetime cost.(8) Further, stroke survivors often face a loss of income, and loss of earnings for individuals who experience stroke at younger ages is expected to be greater.(9)
Although age at stroke onset is an important outcome from a public health perspective, data on contemporary US trends in age at stroke onset are limited. One study from the Greater Cincinnati/Northern Kentucky Stroke Study (GCNKSS) found that mean age at stroke significantly decreased from 71.2 years to 69.2 years over a twelve-year period from 1993 to 2005 in both blacks and whites.(10) Similar data for other populations and race-ethnic groups, including Hispanic Americans, are not available.
There are several reasons why understanding temporal trends in age at stroke in Hispanic Americans is important. People of Hispanic origin are now the nation’s largest ethnic minority and they are currently youthful, with a median age of 27.3 years old, suggesting stroke will take on increasing importance as this population ages.(11) Mexican Americans (MAs) are the largest sub-group of Hispanic Americans. Previous research has revealed that stroke incidence is higher, particularly at younger ages, and the outcome is worse in MAs compared with NHWs.(3, 12) In addition, stroke incidence has remained stable over time in MAs 45 to 59 years of age, in contrast to the declining incidence seen in older MAs.(3)
The aim of this study was to describe temporal trends in age at ischemic stroke onset overall and by ethnicity using data from a large population-based stroke study conducted in a biethnic community. We hypothesized that age at stroke onset has decreased over time and that MAs have experienced greater declines compared with NHWs.
Methods
Patients and Setting
The Brain Attack Surveillance in Corpus Christi (BASIC) Project is a population-based stroke surveillance study in Nueces County, Texas. The BASIC Project methods have been previously published.(13) The population of Nueces County was 361,350 in 2016, of which 63.4% were MAs.(14) The community has been stable over time with fewer than 6% of the county residents in 2010 moving to another county in 2011, lower than the average for the state of Texas.(15) Corpus Christi, the major city in Nueces County, is more than 150 miles away from referral centers in San Antonio and Houston, and adjacent counties are sparsely populated. Thus, medical care in Nueces County is highly self-contained. There are two health systems with seven acute-care community hospitals and all of them have computed tomography (CT) and magnetic resonance imaging (MRI).
Subjects are eligible for BASIC if they are ≥45 years of age, have had a stroke not as a result of head trauma, and reside in Nueces County for at least 6 months per year. Only MA and NHW cases were included in the current study due to low numbers of individuals with other race-ethnicities. The University of Michigan Institutional Review Board (IRB) and the IRBs of both Nueces County hospital systems approved the BASIC project.
Case Ascertainment
Procedures to identify stroke cases in the BASIC project include active and passive surveillance.(3, 13) Trained abstractors review emergency room and admission logs daily to identify stroke patients using validated screening terms. In addition, hospital wards and intensive care units are examined for in-house strokes or those not ascertained through the screening logs. The active surveillance is supplemented by monthly review of hospital passive listings of International Classification of Disease discharge codes for stroke. Minor changes to the case ascertainment procedures during this project have been previously reported.(16)
Cases are validated by stroke fellowship trained physicians using source documentation, blinded to ethnicity. Stroke diagnosis is based on published international clinical criteria(17) that require onset of a focal neurologic deficit specifically attributable to a cerebrovascular distribution that persists for greater than 24 hours and not explainable by a nonvascular etiology. CT and MRI imaging assists in determining the stroke type. Only validated cases of incident (no documented history of stroke/TIA in medical record) ischemic stroke between January 1, 2000 and June 30, 2012 were included.
Data Collection
Age at onset was abstracted from the medical record. Time in years since 2000 (primary exposure) was based on date of first presentation to the hospital. Demographics and risk factors were also collected from the medical record. Risk factors represent documented history (present versus absent) of a given risk factor in the medical record and included atrial fibrillation, coronary artery disease, excessive alcohol, diabetes, high cholesterol, hypertension, and ever smoker. Race-ethnicity in the medical record agrees highly with self-reported race-ethnicity in this community (kappa=0.94).(13) Initial stroke severity was assessed by the National Institute of Health Stroke Scale (NIHSS), which was abstracted from the medical record or calculated using a published algorithm.(18) Data from the 2000 and 2010 US Census, and from 2001–2009 and 2011–2012 intercensal estimates, were used to estimate yearly average age of the population at risk for stroke overall and by ethnicity. Yearly estimates were calculated by first multiplying yearly population counts in each 5-year age interval by the median age of the interval. Products were then summed and divided by the yearly population counts to determine yearly average age in the population.
Statistical Analysis
Descriptive statistics were calculated overall and by ethnicity. Mean change of each variable (demographics and risk factors) over time was evaluated by fitting a linear regression model with robust standard errors. To display changes over time in a more intuitive way, the characteristics (age, sex, race-ethnicity, NIHSS) and prevalence of risk factors (atrial fibrillation, coronary artery disease, excessive alcohol, diabetes, high cholesterol, hypertension, ever smoker) were also calculated for the early (2000–2002) and late (2010–2012) time periods. Temporal trends in age at stroke were investigated using generalized additive models (GAMs) with time in years since 2000 modeled through a smoothing spline.(19) The crude model included only time. To explore effect modification of temporal trends in age at stroke by ethnicity, ethnicity and the interaction term between ethnicity and time were included in a second model. To adjust for changes in the age of the population at risk, yearly average ages overall and by ethnicity were included in the previous two models, respectively. Other potential confounders were not included in the models as our goal was to describe overall trends in age at stroke onset over time. In sensitivity analyses, we re-ran the model excluding the 2009 year as mean age in this year was abnormally high compared to other years.
Post-hoc Analysis
Because there has been an increased use of imaging over time, it is possible that in the more recent time period a greater number of mild strokes in younger people are being detected that would have been missed in the earlier study time period.(20) For this reason, a post-hoc analysis was conducted to describe temporal trends in stroke severity by age group to investigate increases in the use of imaging over time. A GAM model was used to look at stroke severity over time by age group with stroke severity modeled as natural logarithm of NIHSS plus one.
Results
There were 3,496 first-ever ischemic strokes ascertained between January 1, 2000 and June 30, 2012; 244 were excluded as they were not NHW or MA. Tables 1a and b include demographic characteristics, as well as risk factor prevalences, and their mean changes during the study period by ethnicity. For MAs, median age at stroke onset was 67.0 years (IQR: 57.0–78.0) and for NHWs, it was 75.0 years (IQR: 63.0–83.0). Fifty-three percent of MAs had diabetes, and the estimated mean change in prevalence of diabetes was 6.5% over the 13 years. Twentyfive percent of NHWs had diabetes, and the estimated mean change in prevalence was 7.9% over the 13-year study period. In both ethnic groups, prevalence of uninsured, hypertension, and high cholesterol increased significantly from 2000 to 2012 (p < 0.001 for all). In NHWs, the prevalence of atrial fibrillation and ever smoking increased over the study period with a mean change of 12.7% and 11.9%, respectively. The distribution of sex did not change significantly over time in either ethnic group. Supplemental Table 1 includes the demographics and risk factors for the overall population.
Table 1a.
Characteristics of acute ischemic stroke in Mexican Americans between January 1, 2000 and June 30, 2012
| Variable | Overall % (n) or median (Q1, Q3) | 2000–2002 | 2010–2012 | Mean change in 2000–2012* | 95% CI | P-value |
|---|---|---|---|---|---|---|
| Age (y) | 67.0 (57.0, 78.0) | 70.0 (59.0, 78.0) | 65.0 (57.0, 77.0) | −1.28 | −3.12, 0.57 | 0.1741 |
| Sex (% females) | 50.19 (915) | 53.08 | 48.59 | −3.92 | −11.48, 3.64 | 0.3096 |
| NIH Stroke Scale | 4.0 (2.0, 7.0) | 4.0 (2.0, 7.0) | 4.0 (2.0, 8.0) | 1.06 | 0.03, 2.09 | 0.0441 |
| Health Insurance (% uninsured) | 9.84 (179) | 7.76 | 14.32 | 8.08 | 3.44, 12.71 | 0.0006 |
| Atrial Fibrillation (%) | 9.16 (167) | 7.52 | 9.72 | 3.1 | −1.16, 7.36 | 0.1539 |
| CAD (%) | 30.28 (552) | 30.98 | 28.64 | 0.62 | −6.36, 7.60 | 0.8618 |
| Excessive Alcohol (%) | 6.36 (116) | 5.69 | 7.42 | 0.73 | −2.91, 4.38 | 0.6935 |
| Diabetes Mellitus (%) | 52.83 (963) | 51.03 | 57.29 | 6.47 | −1.06, 14.00 | 0.0922 |
| High Cholesterol (%) | 33.30 (607) | 19.36 | 45.27 | 33.26 | 26.55, 39.97 | <0.0001 |
| Hypertension (%) | 76.80 (1400) | 69.48 | 82.86 | 17.66 | 11.26, 24.05 | <0.0001 |
| Ever Smoker (%) | 30.62 (554) | 27.04 | 32.05 | 5.12 | −1.80, 12.04 | 0.1469 |
Risk factors ascertained from medical records.
In a linear regression model: Variable = β0+ β1time + ∈, the mean change of variable from 2000 to 2012 was calculated by 12β1. 95% CI and Pvalue was calculated using empirical standard errors.
Table 1b.
Characteristics of acute ischemic stroke in Non-Hispanic Whites between January 1, 2000 and June 30, 2012
| Variable | Overall % or median (Q1, Q3) |
2000–2002 | 2010–2012 | Mean change in 2000–2012* | 95% CI | P-value |
|---|---|---|---|---|---|---|
| Age (y) | 75.0 (63.0, 83.0) | 76.0 (67.0, 83.0) | 71.0 (60.0, 82.0) | −2.76 | −4.88, −0.64 | 0.0108 |
| Sex (% females) | 51.15 (731) | 51.26 | 48.13 | −4.21 | −12.72, 4.30 | 0.3325 |
| NIH Stroke Scale | 4.0 (2.0, 8.0) | 3.0 (1.0, 7.0) | 4.0 (2.0, 9.0) | 1.66 | 0.38, 2.94 | 0.0112 |
| Health Insurance (% uninsured) | 5.18 (74) | 4.05 | 8.58 | 4.04 | −0.003, 8.08 | 0.0502 |
| Atrial Fibrillation (%) | 18.61 (266) | 12.88 | 23.88 | 12.69 | 6.05, 19.33 | 0.0002 |
| CAD (%) | 30.44 (435) | 31.06 | 24.25 | −2.66 | −10.37, 5.06 | 0.4999 |
| Excessive Alcohol (%) | 6.09 (87) | 6.06 | 7.84 | 1.99 | −2.37, 6.35 | 0.3714 |
| Diabetes Mellitus (%) | 25.47 (364) | 22.47 | 27.99 | 7.9 | 0.55, 15.25 | 0.035 |
| High Cholesterol (%) | 31.98 (457) | 17.93 | 43.66 | 33.58 | 25.95, 41.21 | <0.0001 |
| Hypertension (%) | 71.73 (1025) | 66.67 | 75.75 | 11.84 | 4.16, 19.53 | 0.0025 |
| Ever Smoker (%) | 37.90 (534) | 35.53 | 48.13 | 11.91 | 3.52, 20.30 | 0.0054 |
Risk factors ascertained from medical records.
In a linear regression model: Variable = β0+ β1time + ∈, the mean change of variable from 2000 to 2012 was calculated by 12β1. 95% CI and Pvalue was calculated using empirical standard errors.
Figure 1 illustrates crude and yearly average age adjusted trends in mean age at first-ever ischemic stroke over the study period. In unadjusted analysis, mean age at stroke onset decreased in the initial study period from 2000–2004, and then stayed relatively unchanged from 2005 to 2009. Since 2009, mean age at stroke onset declined slightly. Over the 13 years, mean age at first-ever ischemic stroke significantly decreased from an average of 71.7 years in 2000 to an average of 69.3 years in 2012 (p=0.0043, Figure 1A).
Figure 1.
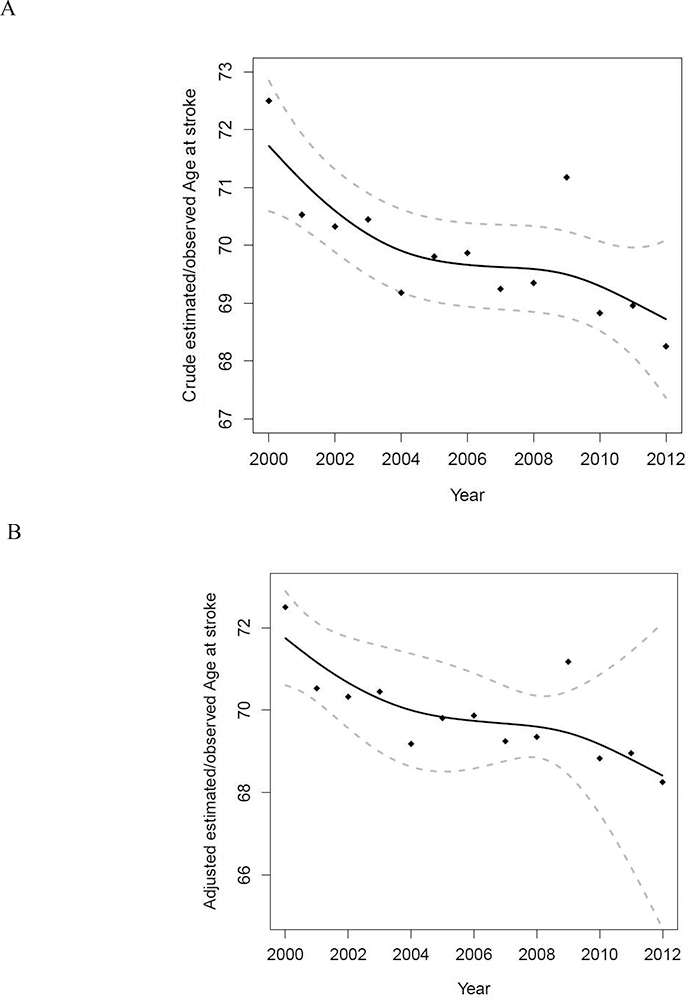
Temporal trends in age at stroke from validated cases of first-ever acute ischemic stroke in BASIC between January 1, 2000 and June 30, 2012. (A) Crude estimated/observed age at stroke. (B) Adjusted estimated/observed age at stroke. Dots indicate observed mean age each year. Black line indicates estimates from a generalized additive model (GAM) with smoothed time as the only predictor. Dashed lines indicate 95% confidence intervals (CI).
Effect modification of the trend in age at stroke onset by ethnicity was significant in the crude model (p<0.001, Figure 2A). Although the overall pattern of declining age at stroke onset was similar in the two ethnic groups, NHWs experienced greater declines compared with MAs. The mean age was estimated to decrease from 74.8 to 71.3 over the 13 years for NHWs, while for MAs, mean age was estimated to decrease from 68.9 to 66.9 after adjusting for ethnicspecific average age of the population at risk population.
Figure 2.
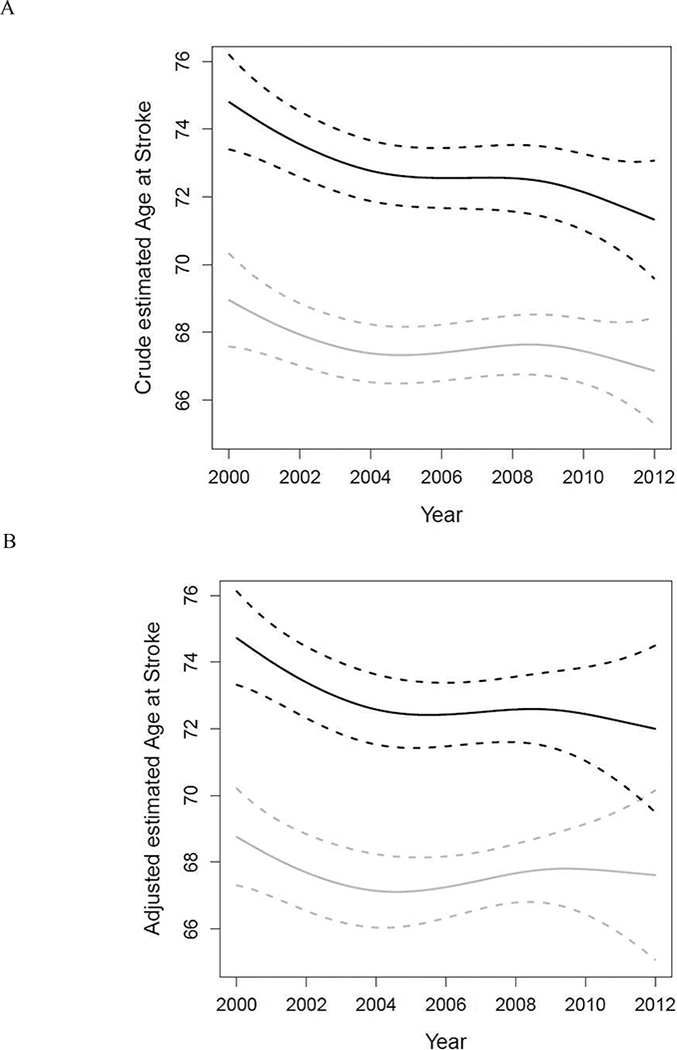
Temporal trends in age at stroke by ethnicity from validated cases of first-ever acute ischemic stroke in BASIC between January 1, 2000 and June 30, 2012. (A) Crude estimated age at stroke. (B) Adjusted estimated age at stroke. Estimates were from a GAM with smoothed time, ethnicity and the interaction term between time and ethnicity as predictors. Grey lines indicate estimates and 95% confidence intervals (CI) for Mexican Americans. Black lines indicate estimates and 95% CI for non-Hispanic whites.
The population ages 45–59 grew by 25.6% during the study period, whereas the population greater than 75 years of age increased by 23.3% (Supplemental Table 2). In 2000, those 45–59 years of age comprised 54.5% of the population ages ≥45 years. In 2012, this percentage dropped to 52.7%. Population growth was greater in MAs compared with NHWs (Supplemental Table 3). In both ethnic groups, the largest increases were in those 60–74 years of age. After controlling for average age of the population at risk, mean age at stroke onset still significantly decreased over time in a similar pattern overall (Figures 1B) and by ethnicity (p=0.248, Figure 2B).
Excluding data from 2009 in sensitivity analysis resulted in a more linear pattern to the declines in age at stroke onset (data not shown). However, declines in age at stroke over time were still greater among NHWs than MAs.
Post-hoc Analysis
A significant difference in the trend in NIHSS between age groups was found (Supplemental Figure 1, p<0.001). Patients aged 75 and above had the highest estimated NIHSS compared to the other two age groups and the greatest increase in severity over time. Estimated NIHSS among those who were aged 60–74 decreased in the first three years and then increased since 2002. For the youngest age group (45–59), mean NIHSS increased steadily from 2000 to 2012.
Discussion
In this population-based study, age at first-ever ischemic stroke declined significantly over time, especially from 2000 to 2005. Ethnicity significantly modified this association such that a greater decline in age at first-ever ischemic stroke was observed among NHWs compared with MAs. If life expectancy continues to increase, stroke occurring at a younger ages will likely result in patients living with more years of stroke-related disability. Earlier stroke also means greater lifetime costs due to stroke for patients and families. Our study found that declines in age at stroke onset were present in both ethnic groups suggesting an increasing lifetime stroke burden in both populations. Although declines in age at stroke onset were greater in NHWs than in MAs, MAs still experienced stroke at younger ages on average compared with NHWs suggesting this population continues to face a disproportionate stroke burden.
One hypothesis for the observed trend in age at stroke onset is more growth of the younger at risk population versus the older population. Overall, in this study community, the population of those ages 45–59 has grown by 25.6% whereas the population greater than 75 years of age has increased by 23.3%. However, those 45–59 years of age comprise a lower proportion of the population ≥45 years in 2012 compared with 2000 arguing against this hypothesis. To account for temporal trends in age distributions of the at-risk population, we controlled for average yearly age in our models and found that the results were largely unchanged. Although residual confounding is possible, these findings raise the hypothesis that the declines in age at stroke onset may be due to other factors.
We found significant increases in the prevalence of hypertension, diabetes, high cholesterol, and atrial fibrillation over time. Other studies have reported similar increases in the prevalence of hypertension and diabetes in the general population aged 40 to 59 years.(21, 22) Therefore, one hypothesis is that temporal trends in stroke risk factors in the midlife have contributed to the observed decline in age at stroke onset. This hypothesis requires further study in a different study design. Alternatively, the increases in risk factors over time may be a result of better detection versus true increases in the prevalence of these factors. Regardless, the significant increase in the proportion of uninsured in this community indicates that there are likely greater challenges to accessing health care for primary stroke prevention, especially for those less than 65 years who are not yet eligible for Medicare. Data on trends in risk factor modification before stroke and how these trends correlate with the increasing prevalence in uninsured would also be useful for policy makers.
A third hypothesis for the observed trend in age at stroke onset is change in the detection of stroke over time with increased use of imaging.(20) It could be that over time a greater number of mild strokes in younger people are being detected that would have been missed in the earlier study time period. In our post-hoc analysis of trends in stroke severity by age group, we did find that stroke severity was lower in the younger age group but severity was increasing over time in all age groups which somewhat detracts from the hypothesis of earlier detection of mild strokes. Given changes in acute stroke care in this community during the time period of the study, including two hospitals becoming certified as Joint Commission Primary Stroke Centers, the increases in initial stroke could also be an artifact of more examiner reported versus chart abstracted NIHSS scores and better documentation of severity in the medical record. The impact of stroke detection on trends in age at stroke onset requires further study.
Our finding of a decline in age at stroke onset is in line with the findings from the GCNKSS which noted a decrease from 1993/1994 to 2005.(10) A recent study, conducted in a low-income Chinese population, found that mean age of stroke onset in men significantly decreased by 0.22 years for ischemic stroke annually, from 1992 to 2014.(23) Investigators of this study also found significant increases in the prevalence of risk factors in adults aged 64 years or less, from 1992 to 2011. Collectively, these data suggest that declines in age at stroke and increases in prevalence of stroke risk factors may be happening worldwide, not just in the US.
We hypothesized that MAs would have greater declines in age at stroke onset compared to NHWs due to ethnic differences in temporal trends in stroke risk factors. Over the past several decades, the prevalence and incidence of diabetes have increased substantially, and the increase in incidence has been greater in MAs than in NHWs.(24, 25) Diabetes is a powerful risk factor for stroke in individuals 55 years of age or less, and stroke patients with diabetes are significantly younger than stroke patients without diabetes.(26) These data suggest that age at stroke onset may be declining over time and more so in MAs than NHWs. However, we found the opposite. The reasons why NHWs had greater declines are unclear. MAs experienced considerably larger growth of the younger population over time than NHWs so ethnic differences in the at-risk population do not appear to explain greater declines in age at onset in NHWs. Ethnic differences in trends in the prevalence of stroke risk factors may have contributed to greater declines in NHWs. Although MAs were more likely to have diabetes compared to NHWs, the prevalence of diabetes among stroke patients in our study population increased to a greater extent over time among NHWs compared with MAs. Atrial fibrillation, an independent risk factor for stroke,(27) also demonstrated a greater increase in prevalence over time among NHWs compared to MAs, although these data should be interpreted with caution as they reflect greater detection of atrial fibrillation over time versus a true increase in prevalence.
There are some limitations of this work. Information on risk factors was based on documented history in the medical record and therefore, there may be some individuals with undiagnosed risk factors. Results are based on one community and therefore, the results may not be generalizable.
In conclusion, we observed that age at first-ever ischemic stroke significantly decreased over time, with NHWs experiencing a greater decline compared with MAs. These findings suggest a potential increase in lifetime stroke burden in both ethnic groups. Efforts are needed to prevent and treat stroke risk factors to thwart earlier onset of ischemic stroke.
Supplementary Material
Acknowledgements
This work was supported by the National Institutes of Health (grant numbers R01NS38916, R01NS070941).
Footnotes
Disclosures
None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kochanek KD, Murphy S, Xu J, Arias E. Mortality in the United States, 2016. NCHS data brief. 2017(293):1–8. [PubMed] [Google Scholar]
- 2.Carandang R, Seshadri S, Beiser A, Kelly-Hayes M, Kase CS, Kannel WB, et al. Trends in incidence, lifetime risk, severity, and 30-day mortality of stroke over the past 50 years. JAMA. 2006;296(24):2939–46. [DOI] [PubMed] [Google Scholar]
- 3.Morgenstern LB, Smith MA, Sanchez BN, Brown DL, Zahuranec DB, Garcia N, et al. Persistent ischemic stroke disparities despite declining incidence in Mexican Americans. Ann Neurol. 2013;74(6):778–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koton S, Schneider AL, Rosamond WD, Shahar E, Sang Y, Gottesman RF, et al. Stroke incidence and mortality trends in US communities, 1987 to 2011. JAMA. 2014;312(3):259–68. [DOI] [PubMed] [Google Scholar]
- 5.Kissela B Age at stroke: Temporal trends in stroke incidence in a large, biracial population. Neurology. 2012;79(17):1781–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bejot Y, Daubail B, Jacquin A, Durier J, Osseby GV, Rouaud O, et al. Trends in the incidence of ischaemic stroke in young adults between 1985 and 2011: the Dijon Stroke Registry. J Neurol Neurosurg Psychiatry. 2014;85(5):509–13. [DOI] [PubMed] [Google Scholar]
- 7.Lackland DT, Roccella EJ, Deutsch AF, Fornage M, George MG, Howard G, et al. Factors influencing the decline in stroke mortality: a statement from the American Heart Association/American Stroke Association. Stroke. 2014;45(1):315–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Di Carlo A Human and economic burden of stroke. Age Ageing. 2009;38(1):4–5. [DOI] [PubMed] [Google Scholar]
- 9.McKevitt C, Fudge N, Redfern J, Sheldenkar A, Crichton S, Rudd AR, et al. Selfreported long-term needs after stroke. Stroke. 2011;42(5):1398–403. [DOI] [PubMed] [Google Scholar]
- 10.Kissela BM, Khoury JC, Alwell K, Moomaw CJ, Woo D, Adeoye O, et al. Age at stroke: temporal trends in stroke incidence in a large, biracial population. Neurology. 2012;79(17):1781–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.QuickFacts United States [cited 2018 May 23]. Available from: https://www.census.gov/quickfacts/fact/table/US/PST045216.
- 12.Lisabeth LD, Sanchez BN, Baek J, Skolarus LE, Smith MA, Garcia N, et al. Neurological, functional, and cognitive stroke outcomes in Mexican Americans. Stroke. 2014;45(4):1096–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith MA, Risser JM, Moye LA, Garcia N, Akiwumi O, Uchino K, et al. Designing multi-ethnic stroke studies: the Brain Attack Surveillance in Corpus Christi (BASIC) project. Ethn Dis. 2004;14(4):520–6. [PubMed] [Google Scholar]
- 14.QuickFacts Nueces County, Texas [cited 2018 May 23]. Available from: https://www.census.gov/quickfacts/fact/table/nuecescountytexas/PST045216.
- 15.City-Data.com [cited 2018 May 23]. Available from: http://www.citydata.com/county/Nueces County-TX.html.
- 16.Asplund K, Tuomilehto J, Stegmayr B, Wester PO, Tunstall-Pedoe H. Diagnostic criteria and quality control of the registration of stroke events in the MONICA project. Acta Med Scand Suppl. 1988;728:26–39. [DOI] [PubMed] [Google Scholar]
- 17.Asplund K, Tuomilehto J, Stegmayr B, Wester P, TUNSTALL-PEDOE H. Diagnostic criteria and quality control of the registration of stroke events in the MONICA project. Acta medica Scandinavica. 1988;224(S728):26–39. [DOI] [PubMed] [Google Scholar]
- 18.Williams LS, Yilmaz EY, Lopez-Yunez AM. Retrospective assessment of initial stroke severity with the NIH Stroke Scale. Stroke. 2000;31(4):858–62. [DOI] [PubMed] [Google Scholar]
- 19.Hastie T, Tibshirani R. Generalized Additive Models. Statistical Science. 1986;1(3):297–310. [DOI] [PubMed] [Google Scholar]
- 20.Kleindorfer D, Khoury J, Alwell K, Moomaw CJ, Woo D, Flaherty ML, et al. The impact of Magnetic Resonance Imaging (MRI) on ischemic stroke detection and incidence: minimal impact within a population-based study. BMC neurology. 2015;15:175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303(20):2043–50. [DOI] [PubMed] [Google Scholar]
- 22.Mokdad AH, Ford ES, Bowman BA, Nelson DE, Engelgau MM, Vinicor F, et al. Diabetes trends in the U.S.: 1990–1998. Diabetes Care. 2000;23(9):1278–83. [DOI] [PubMed] [Google Scholar]
- 23.Wang J, Bai L, Shi M, Yang L, An Z, Li B, et al. Trends in Age of First-Ever Stroke Following Increased Incidence and Life Expectancy in a Low-Income Chinese Population. Stroke. 2016;47(4):929–35. [DOI] [PubMed] [Google Scholar]
- 24.Geiss LS, Wang J, Cheng YJ, Thompson TJ, Barker L, Li Y, et al. Prevalence and incidence trends for diagnosed diabetes among adults aged 20 to 79 years, United States, 1980–2012. JAMA. 2014;312(12):1218–26. [DOI] [PubMed] [Google Scholar]
- 25.Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014;103(2):137–49. [DOI] [PubMed] [Google Scholar]
- 26.Kissela BM, Khoury J, Kleindorfer D, Woo D, Schneider A, Alwell K, et al. Epidemiology of ischemic stroke in patients with diabetes: the greater Cincinnati/Northern Kentucky Stroke Study. Diabetes Care. 2005;28(2):355–9. [DOI] [PubMed] [Google Scholar]
- 27.Meschia JF, Bushnell C, Boden-Albala B, Braun LT, Bravata DM, Chaturvedi S, et al. Guidelines for the primary prevention of stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(12):3754–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


