Abstract
Neuroendocrine tumors (NETs) are an uncommon diagnosis which often present asymptomatically or with vague symptoms. They can originate from many different organs such as the GI tract, lungs, pancreas and others. 68Gallium DOTATATE positron emission topography/computed topography has been shown to be an effective imaging modality for diagnosing NET and evaluating management options for patients. Here, we present two cases of positive findings in the distal pancreas on the DOTATATE PET/CT scans without any morphological lesion found to be NET in a healthy 48-year-old male and 68-year-old male.
INTRODUCTION
Neuroendocrine tumors (NETs) originate from neuroendocrine cells and are predominantly found in the respiratory or gastrointestinal tract. The incidence has increased over the past decades [1]. Due to their heterogeneity, nonspecific presentation symptoms, and indolent behavior, patients with NETs may undergo significant delay in diagnosis [1].
It was discovered that well differentiated NETs express high levels of somatostatin receptors [6] and thus somatostatin receptor imaging was born. 111Indium-DTPA-penteoctreotide (Octreoscan) was one of the first functional imaging modalities to diagnose NET, yet, it suffered from limited imaging quality and spatial resolution as well as prolonged imaging protocols [2]. Recently, 68Gallium-DOTA-D-Phe1-Tyr3-Thr8-octreotide positron emission topography/computed topography (DOTATATE PET/CT) imaging has shown to be superior to Octreoscan [3]. This has led to a uniquely quick adoption of this imaging modality for the detection of NETs.
Endoscopic ultrasound (EUS) has been shown to accurately localize pancreatic NET (PNET) with a high sensitivity and specificity [4]; detection can be limited by chronic pancreatitis, distal pancreatic tail lesions and other factors [5]. Here, the following case reports describe detecting PNET in two patients utilizing 68Gallium DOTATATE PET/CT imaging without preoperative tissue diagnosis.
CASE PRESENTATION #1
A 48-year-old Caucasian male with a medical history significant for hypertension was referred to the general surgery clinic for chronic abdominal pain for the past 6 months. The patient was suffering from nausea, postprandial facial flushing and crampy/colicky epigastric pain radiating to the RLQ. Initial laboratory work up including complete blood count, complete metabolic panel, serum CA-19-9, serum CEA, urinary 5-HIAA, serum chromogranin A and serum neuron specific enolase were all unremarkable. Additionally, right upper quadrant ultrasound and CT abdomen/pelvis were unremarkable. However, the patient symptoms persisted, and therefore a 68Ga DOTATATE PET/CT scan was ordered. Imaging revealed increased DOTATATE activity (SUV 9.7) in the distal pancreatic tail without an underling mass on CT (Fig. 1A). EUS fine needle aspiration was unremarkable. Additional laboratory analysis revealed elevated C-peptide (4.9 ng/ml) and proinsulin levels (76 pmol/l), concerning for an insulinoma. In addition, a HIDA scan showed a gallbladder ejection fraction of 34%, consistent with chronic cholecystitis.
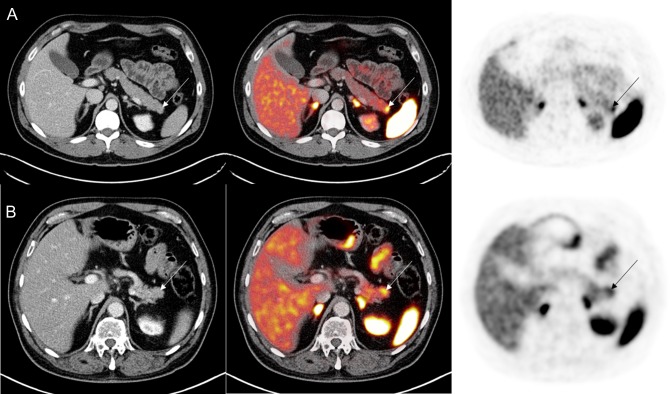
Figure 1:
(A) 68Ga PET/CT DOTATATE demonstrating increased DOTATATE uptake (SUVmax 9.7) in the distal pancreas without underlying pancreatic mass in the first case study. (B) In the second case study, 68Ga PET/CT DOTATATE revealed increased DOTATATE uptake (SUVmax 7.6) in the pancreatic tail without any CT abnormality.
Although there was no tissue diagnosis for the suspected insulinoma on the distal pancreas, a laparoscopic distal pancreatectomy, splenectomy and cholecystectomy was recommended. Of note, the intraoperative ultrasound of the pancreas was unremarkable. The distal pancreas was removed and frozen section confirmed no insulinoma at the margins. Pathological examination revealed microscopic (0.5 cm) well differentiated (KI 67 < 1%) NET (Fig. 2). Six benign regional lymph nodes were also removed. In addition, there was evidence of focal chronic pancreatitis. Patient did well postoperatively.
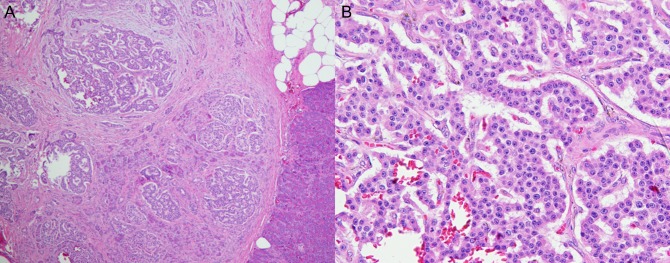
Figure 2:
Pathology from the first operation on the first case study patient. (A) H&E stain at low magnification (×40) shows a well-defined border between the tumor and normal pancreatic tissue (right lower). (B) High magnification (×200) shows the tumor cells forming anastomosing cords, with ‘salt-and-pepper’ chromatin and eosinophilic, granular cytoplasm.
Patient was compliant with his follow-up appointment at 1, 6 and 12 months. His preoperative symptoms have resolved. His postoperative laboratory workup and imaging has been negative for recurrence.
CASE PRESENTATION #2
A 68-year-old male with a medical history for hypertension and type 2 diabetes mellitus, was referred to the general surgery clinic with three bouts of acute pancreatitis of unclear etiology from February 2017 to March 2018. He had intermittent severe postprandial epigastric pain and nausea. Patient denied other symptoms. Initial laboratory work up was unremarkable except for an elevated chromogranin A (393 ng/ml). CT abdomen and pelvis as well as magnetic resonance cholangiopancreatography were unable to identify any lesion. Therefore, the patient underwent a 68Ga DOTATATE PET/CT scan which revealed increased uptake in the distal pancreas (SUVmax 7.6) without any underling lesion (Fig. 1B). EUS fine needle aspiration showed no abnormalities. Given the multiple bouts of acute pancreatitis, he was recommended to have a laparoscopic distal pancreatectomy and splenectomy. Intraoperative ultrasound demonstrated a normal pancreas. Pathology revealed a NET (10 mm in size) and margins were negatives. Eleven benign lymph nodes were resected. His 2-week postoperative follow up in late April 2018 was unremarkable. He denied new symptoms and previous symptoms have resolved. No imaging or laboratory work up was done at this time.
DISCUSSION
NETs are considered rare tumors. However, the incidence has been increasing in the USA over the past decades [1]. They arise from multiple different organs not limited to but include the GI tract, pancreas, ovaries and pituitary gland [1]. These tumors are indolent, slow growing and therefore, patients present asymptomatically [6]. Some patients present with carcinoid syndrome, a constellation of symptoms including mainly facial flushing and diarrhea [1]. Pathologic values of urinary 5-HIAA and chromogranin A levels are a common finding.
68Ga DOTATATE PET/CT scans are being utilized for the diagnosis of NET. It has been shown previously to be superior to its predecessor, Octreoscan [3]. Furthermore, this modality has a sensitivity, specificity, and positive predictive value of 81, 90 and 81%, respectively, in patients with suspected NET [7]. In addition, it is used in evaluating the treatment options, detecting metastatic disease, and presence of recurrent disease [8]. Therefore, it is crucial for the management of NETs.
Both cases exemplify the difficulty of establishing a preoperative diagnosis of NET. The patients had laboratory evidence of an NET, given the elevated C peptide and proinsulin in the first patient and elevated chromogranin A in the second patient.
Although these markers are highly sensitive and specific for NETs [9], there was no morphological evidence of any lesion. However, both did have functional evidence of NET on the distal pancreas (Fig. 1). EUS studies were unremarkable and unable to give a tissue diagnosis, which may have been secondary to the presence of pancreatitis or the location of the lesions in the distal pancreas. The patients underwent laparoscopic distal pancreatectomy and splenectomy and there was microscopic evidence for NET in the pathologic specimens.
In summary, these cases highlight the important of obtaining a 68Ga DOTATATE PET/CT scan for patients for suspected NET by history or biochemical evaluation with a paucity of other cross-sectional imaging findings. Additionally, patients can be considered for surgical resections of lesions that demonstrate increased DOTATATE uptake without preoperative tissue diagnosis as there is a high likelihood they are NETs.
CONFLICT OF INTEREST STATEMENT
No disclosure or conflict of interest to declare.
REFERENCES
- 1. Hallet J, Law CH, Cukier M, Saskin R, Liu N, Singh S. Exploring the rising incidence of neuroendocrine tumors: a population-based analysis of epidemiology, metastatic presentation, and outcomes. Cancer 2015;121:589–97. [DOI] [PubMed] [Google Scholar]
- 2. Maxwell JE, Sherman SK, Menda Y, Wang D, O’Dorisio TM, Howe JR. Limitations of somatostatin scintigraphy in primary small bowel neuroendocrine tumors. J Surg Res 2014;190:548–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gabriel M, Decristoforo C, Kendler D, Dobrozemsky G, Heute D, Uprimny C, et al. . 68Ga-DOTA-Tyr3-octreotide PET in neuroendocrine tumors: comparison with somatostatin receptor scintigraphy and CT. J Nucl Med 2007;48:508–18. [DOI] [PubMed] [Google Scholar]
- 4. Kim MK. Endoscopic ultrasound in gastroenteropancreatic neuroendocrine tumors. Gut Liver 2012;6:405–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Adler DG, Diehl DL. Missed lesions in endoscopic ultrasound. Endosc Ultrasound 2015;4:165–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Saha S, Hoda S, Godfrey R, Sutherland C, Raybon K. Carcinoid tumors of the gastrointestinal tract: a 44-year experience. South Med J 1989;82:1501–5. [DOI] [PubMed] [Google Scholar]
- 7. Haug AR, Cindea-Drimus R, Auernhammer CJ, Reincke M, Wangler B, Uebleis C, et al. . The role of 68Ga-DOTATATE PET/CT in suspected neuroendocrine tumors. J Nucl Med 2012;53:1686–92. [DOI] [PubMed] [Google Scholar]
- 8. Mojtahedi A, Thamake S, Tworowska I, Ranganathan D, Delpassand ES. The value of (68)Ga-DOTATATE PET/CT in diagnosis and management of neuroendocrine tumors compared to current FDA approved imaging modalities: a review of literature. Am J Nucl Med Mol Imaging 2014;4:426–34. [PMC free article] [PubMed] [Google Scholar]
- 9. Al-Risi ES, Al-Essry FS, Mula-Abed WS. Chromogranin a as a biochemical marker for neuroendocrine tumors: a single center experience at Royal Hospital, Oman. Oman Med J 2017;32:365–70. [DOI] [PMC free article] [PubMed] [Google Scholar]