Abstract
Objective.
To assess the diagnostic and clinical utility of the two-item Generalized Anxiety Disorder Scale (GAD-2) for screening anxiety symptoms in individuals with multiple sclerosis (MS).
Design.
Cross-sectional.
Setting.
University-affiliated MS neurology and rehabilitation center.
Participants.
The sample was comprised of 99 adults (ages 19 to 72; M = 46.2; SD = 13.0; 75% female) with a physician-confirmed MS diagnosis who were receiving care in a university affiliated MS center. Disease durations ranged from 1 to 37 years (M = 10.7; SD = 8.4).
Interventions.
Not applicable.
Main Outcome Measures.
Participants completed the GAD-7 and GAD-2. Internal consistency was calculated for both measures. Area under the receiver operating characteristics curve (AUC), the 95% confidence interval for the AUC, and Youden’s J were calculated to determine the optimal GAD-2 cut-off score for identifying clinically significant anxiety symptoms, as defined by the previously validated GAD-7 cut-off score of ≥ 8.
Results.
Internal consistency was excellent for the GAD-7 (Cronbach α = .91) and acceptable for the GAD-2 (α = .77), and the measures were highly correlated (r = .94). The GAD-2 had excellent overall accuracy for identifying clinically significant anxiety symptoms (AUC = 0.97, 95% CI 0.94 – 1.00). A GAD-2 cut-off score of ≥ 3 provided an optimal balance of good sensitivity (0.87) and excellent specificity (0.92) for detecting clinically significant anxiety symptoms. Alternatively, a cut-off score of ≥ 2 provided excellent sensitivity (1.00) and fair specificity (0.76).
Conclusions.
The GAD-2 is a clinically useful and psychometrically valid tool for screening anxiety symptoms in MS rehabilitation and neurology care settings. Importantly, this tool has the potential to identify individuals with MS who are at risk for anxiety disorders and who may benefit from rehabilitation psychology interventions to ultimately improve functioning and quality of life.
Keywords: multiple sclerosis, anxiety, screening
Multiple sclerosis (MS) is a progressive neurodegenerative disease of the central nervous system that can profoundly interfere with individuals’ physical and psychological functioning and well-being.1–6 Individuals who are coping with a new MS diagnosis and those who have been living with the disease for many years often experience uncertainty and worry about the disease. Uncertainty about the pace and severity of disease progression can contribute to emotional distress in the form of depression and/or anxiety symptoms.7–9 Rehabilitation health care providers (e.g., physicians, psychologists, and rehabilitation therapists) with a specialty in MS have long recognized the increased prevalence of depressive symptoms in this population (4060%) compared to the general population (15–20%).10 Research over the past few decades has increasingly focused on improving the detection, assessment, and treatment of depression in individuals with MS. Screening tools such as the nine-item Patient Health Questionnaire (PHQ9), as well as the brief two-item PHQ-2, have been validated for use in individuals with MS and are often used as part of routine care in rehabilitation and neurology clinics.11
In contrast to the wealth of research dedicated to understanding and treating depression in MS, research investigating anxiety and its treatment in this population is still in its infancy. One of the first studies in this area noted that individuals with MS are at increased risk of developing anxiety disorders (36%) relative to the general population (29%), and that a history of depression may place individuals with MS at greater risk for developing anxiety disorders.10,12,13 Since that time, several additional studies have been published on anxiety in MS with regard to prevalence rates, clinical correlates (e.g., disability, MS subtype), psychiatric comorbidities, and overlapping physiologic symptoms (e.g., pain, sleep disturbance). Importantly, the presence of anxiety is a risk factor for suicidal ideation in depressed individuals with MS.14 However, despite evidence for increased risk of anxiety and its negative effects on functioning and morbidity, anxiety remains underdiagnosed in MS and is not routinely or systematically evaluated during medical appointments.15
One of the barriers, commonly cited by health care providers, to assessing mental health symptoms, including anxiety, is limited clinical time. With appointments typically lasting 30 minutes or less, assessment of emotional distress may be limited to a few qualitative interview questions about mood. As previously noted, however, use of brief, validated questionnaires like the PHQ-2 has the potential to more accurately screen for depressive symptoms and promote appropriate referrals to health or rehabilitation psychologists for further assessment and treatment. Recent efforts have been made to validate similar tools for the assessment of anxiety symptoms in MS, including the 7-item anxiety subscale from the Hospital Anxiety and Depression Scale (HADS) and the 7-item Generalized Anxiety Disorder Scale (GAD-7).16,17
The HADS anxiety subscale and the GAD-7 exhibit good to excellent psychometric properties and are especially effective for screening symptoms of generalized anxiety disorder, which is the most common anxiety disorder both in MS and the general population.10,18 As noted by Terrill and colleagues, the GAD-7 offers the specific advantage of being open-source and having established cut-off scores for mild, moderate, and severe levels of anxiety.17 However, because the GAD-7 includes items related to physical MS symptoms (e.g., restlessness, feeling tense, trouble relaxing) that may be present even in the absence of anxiety, additional work is needed to assess and validate brief anxiety screening measures that do not include physiologic items. Analogous work has been performed on the PHQ-2, which focuses on cognitive and affective depressive symptoms (i.e., depressed mood and anhedonia) and not the physiologic symptoms (i.e., fatigue, poor sleep, appetite, psychomotor speed) included in the full PHQ-9. To address the issue of physiologic symptom overlap in the assessment of anxiety, a two-item version of the GAD-7 (GAD-2) was developed, which specifically assesses anxiousness/nervousness and uncontrollable worry. The two-item version does not include the physiologic symptoms noted above.19 The GAD-2 also features a recommended cut-off score (≥ 3), which has been validated against a gold standard clinical interview for detecting generalized anxiety disorder in the general population.19
The GAD-2 offers great potential for accurately and efficiently detecting anxiety symptoms in individuals with MS; however, to date, the diagnostic and clinical utility of the measure, including its sensitivity and specificity for detecting clinically significant anxiety, has not been psychometrically tested in this population. Therefore, the goal of the present study is to establish the sensitivity and specificity of the GAD-2 with respect to the previously established cut-off score of the GAD-7. We hypothesize that the GAD-2 will provide an accurate and useful clinical measure of anxiety, and that analyses will yield a sensitive and specific GAD-2 cut-off score for detecting clinically significant anxiety symptoms in MS. Importantly, results of this study will help directly inform clinical rehabilitation and neurological care of individuals with MS by offering a brief, useful, and accurate tool that: 1) can readily be integrated into clinical practice; 2) does not require significant provider time or resources; and 3) can facilitate decision-making for directing appropriate referrals to rehabilitation-focused mental health services.
Method
Participants and Procedures
All procedures were approved by the Institutional Review Board. Community-dwelling individuals with MS were recruited from a university-affiliated MS center to participate in a study of cognitive function in MS. The present study featured a secondary analysis of data collected from that primary study. To be eligible for the study, patients were required to be 18 years of age or older and have a physician-confirmed MS diagnosis. Exclusion criteria included: a neurologic disorder other than MS; symptomatic involvement of the upper extremities severe enough to interfere with writing or pressing keys on a computer tablet; and cognitive impairment severe enough to interfere with comprehension of study instructions. Participants were recruited during the course of their routine clinic visits. Participants completed a series of self-report questionnaires, which assessed demographics, MS characteristics, depressive symptoms, and anxiety symptoms. A total of 100 participants were enrolled in the primary study. One participant did not complete the self-report measures; thus, 99 participants were included in the final sample for the present study.
Measures
GAD-7 and GAD-2.
The GAD-7 is a seven-item self-report screening tool assessing the severity of an individual’s anxiety symptoms.20 The items on the scale correspond to criteria for diagnosing generalized anxiety disorder based on the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition – Text Revision. Each item is rated on a 4-point Likert scale based on how frequently the respondent has experienced the symptom in the past two weeks. Item scores range from 0 (not at all) to 3 (nearly every day), with total scores ranging from 0 to 21. Higher scores indicate more severe anxiety symptoms. A cut-off score of 8 is typically used to indicate clinically significant anxiety symptoms in the general population; however, cut-off scores of 5, 10, and 15 may also be used to indicate mild, moderate, and severe levels of anxiety, respectively.20 In addition to use in the general population, the GAD-7 has been validated for use in individuals with MS and has been shown to have good correspondence with the HADS anxiety subscale.17 The GAD-2 consists of the first two items of the GAD-7 (“feeling nervous, anxious, or on edge” and “not being able to stop or control worrying”), with total scores ranging from 0 to 6. A score of ≥ 3 on the GAD-2 has been identified as an acceptable cut-off for identifying clinically significant anxiety symptoms in the general population.19 Although the GAD-7 and GAD-2 are not currently recognized as criterion standard diagnostic instruments, a recent meta-analysis comparing the GAD-7 and GAD-2 against criterion standard assessments (e.g., the Structured Clinical Interview for DSM-IV-TR Axis I Disorders)21 found the GAD-7 and GAD-2 to have acceptable psychometric properties for identifying generalized anxiety disorder.19
PHQ-2.
Given the significant overlap of depressive and anxious symptoms, the PHQ-2 was also administered to all participants. Each item of the PHQ-2 is rated on a 4-point scale based on how frequently the respondent has experienced the symptom in the past two weeks. Item scores range from 0 (not at all) to 3 (nearly every day), with total scores ranging from 0 to 6. A score of ≥ 3 has been identified as an acceptable cut-off for the PHQ-2 in individuals with MS and in the general population.11,22
Data Analysis
Descriptive statistics were calculated for participant demographics, MS characteristics, and responses on the PHQ-2, GAD-7, and GAD-2. Cronbach’s alpha was calculated for the GAD-7 and GAD-2 to determine internal consistency. A Pearson product-moment correlation was calculated to determine the correspondence between total scores on the GAD-7 and GAD-2. GAD-2 scores were then compared against the reference criterion (GAD-7 ≥ 8) using receiver operating characteristic curve analysis. Area under the curve (AUC), the 95% CI for the AUC, sensitivity, specificity, and Youden’s J (J = sensitivity + specificity – 1) were calculated to determine the optimal GAD-2 cut-off score for identifying participants at risk for clinically significant anxiety symptoms.
Results
Descriptive statistics for all study variables are presented in Table 1. The sample ranged in age from 19 to 72 (M = 46.2; SD = 13.0) and was 75% female. Participants reported an average of 15.5 years of education (SD = 2.5), ranging from 10 to 22 years. Disease duration ranged from 1 to 37 years (M = 10.7; SD = 8.4). MS subtypes were known for 88 (89%) participants and were reported as follows: 76 were relapsing remitting (RRMS); 8 were secondary progressive (SPMS); 3 were primary progressive (PPMS), and 1 was progressive relapsing (PRMS). PHQ-2 scores ranged from 0 to 6, with 22 (22%) participants exceeding the recommended cut-off for depression.
Table 1.
Descriptive statistics for demographics, MS characteristics, GAD-7 and GAD-2
| n | Min | Max | M | SD | |
|---|---|---|---|---|---|
| Age (years) | 19 | 72 | 46.2 | 13.0 | |
| Sex | |||||
| Female | 73 | ||||
| Male | 24 | ||||
| Education (years) | 10 | 22 | 15.5 | 2.5 | |
| MS Duration | 1 | 37 | 10.7 | 8.4 | |
| MS Subtype | |||||
| RRMS | 76 | ||||
| SPMS | 8 | ||||
| PPMS | 3 | ||||
| PRMS | 1 | ||||
| PHQ-2 | 0 | 6 | 1.4 | 1.7 | |
| GAD-7 | 0 | 21 | 4.8 | 5.0 | |
| GAD-2 | 0 | 6 | 1.5 | 1.7 |
Note. n = 99.
Abbreviations: GAD-2 = Generalized Anxiety Disorder Scale - 2; GAD-7 = Generalized Anxiety Disorder Scale – 7; MS = multiple sclerosis; PHQ-2 = Patient-Health Questionnaire – 2; PRMS = progressive relapsing MS; PPMS = primary progressive MS; RRMS = relapsing remitting MS; SPMS = secondary progressive MS.
Total scores on the GAD-2 and GAD-7 spanned the full range of possible values (0 to 6 for the GAD-2 and 0 to 21 for the GAD-7), with the mean score falling below the clinical range for both measures (see Table 1). Using the established GAD-7 cut-off score of ≥ 8, 23% of participants scored in the clinically significant range. Although not the focus of the present analyses, it is also useful to note that 28%, 9%, and 7% of participants fell in the mild, moderate, and severe ranges on the GAD-7, respectively. GAD-7 and GAD-2 scores did not differ by sex (GAD-7: X2 = 13.06, p = .79; GAD-2: X2 = 4.95, p = .55) or by MS subtype (GAD-7: X2 = 8.93, p = .96; GAD2: X2 = 3.00, p = .81). GAD-7 and GAD-2 were both correlated with age (GAD-7: r = −.37, p < .001; GAD-2: r = −.33, p < .01), disease duration (GAD-7: r = −.25, p = .01; GAD-2: r = −.21, p = .04), and depression symptoms (GAD-7: r = .66, p <.001; GAD-2: r = .65, p < .001) with greater levels of anxiety associated with younger age, shorter disease duration, and greater levels of depression. With regard to reliability, the GAD-7 demonstrated excellent internal consistency (Cronbach’s α = 0.91) and the GAD-2 demonstrated acceptable internal consistency (Cronbach’s α = 0.77). As expected, the GAD-2 was highly correlated with the GAD-7 (r = .94, p < .001).
GAD-2 Accuracy and Optimal Cut-off Scores for Predicting Clinically Significant Anxiety
Table 2 presents the sensitivity, specificity, and Youden’s J for all GAD-2 scores at the recommended GAD-7 cut-off. At the recommended threshold of ≥ 3 for the general population, the GAD-2 correctly categorized 87% of participants who screened positive (sensitivity) and 92% of participants who screened negative (specificity) for anxiety on the GAD-7 (≥ 8).
Table 2.
Sensitivity, specificity, and Youden’s J for GAD-2 scores in relation to a the GAD-7 cut-off score of ≥ 8
| GAD-2 Scores | Sensitivity | Specificity | Youden's J |
|---|---|---|---|
| ≥1 | 1.00 | 0.59 | 0.59 |
| ≥2 | 1.00 | 0.76 | 0.76 |
| ≥3* | 0.87 | 0.92 | 0.79 |
| ≥4 | 0.61 | 1.00 | 0.61 |
| ≥5 | 0.30 | 1.00 | 0.30 |
| ≥6 | 0.09 | 1.00 | 0.09 |
Note. n = 99.
indicates GAD-2 cut-off score that provides the best balance between sensitivity and specificity.
Abbreviations: GAD-2 = Generalized Anxiety Disorder Scale - 2; GAD-7 = Generalized Anxiety Disorder Scale – 7.
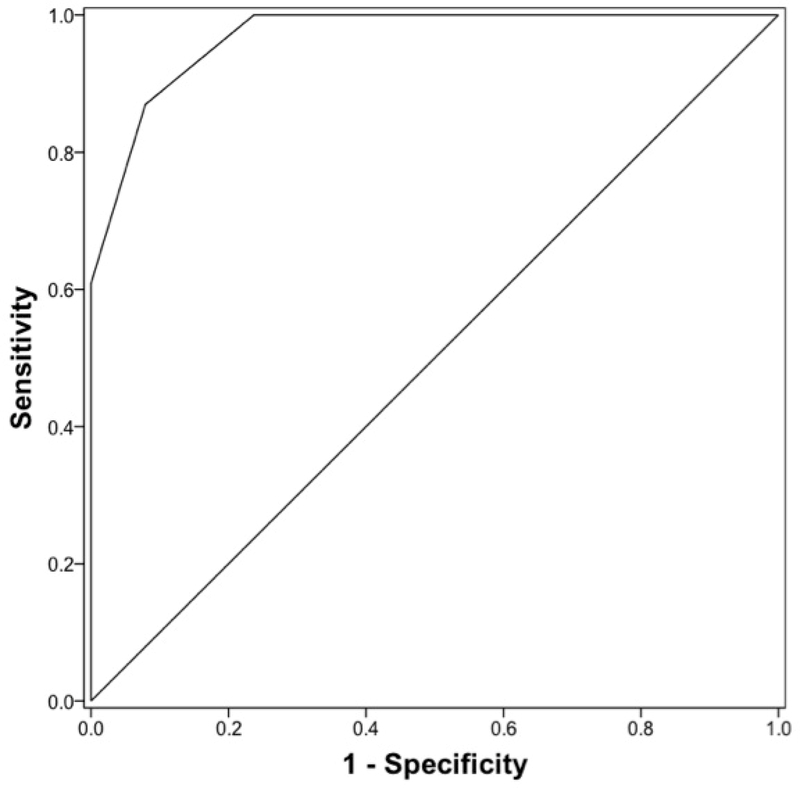
The GAD-2 demonstrated excellent overall accuracy relative to the GAD-7, with an AUC of 0.97 (95% CI: 0.94 to 1.00). Examination of Youden’s J values indicated a GAD-2 score of ≥ 3 provided the optimal balance between sensitivity and sensitivity. A score of ≥ 2 was also acceptable, with excellent specificity (100%) and fair specificity (76%) (figure 1).
Figure 1.
Receiver operating characteristic (ROC) curve for GAD-2 scores for clinically significant anxiety symptoms (GAD-7 ≥ 8). Area under the ROC curve = 0.97 (95% CI: 0.94 – 1.00).
Discussion
The present study was the first to examine the diagnostic and clinical utility of the brief GAD-2 for assessing anxiety symptoms in individuals with MS. Consistent with the recommended GAD-2 cut-off score for the general population, a score of ≥ 3 offered the best balance of sensitivity and specificity for detecting clinically significant anxiety in this sample of individuals with MS. This cut-off score provided good sensitivity for detecting anxiety, whiles also ensuring a low risk for false positives (<10%). However, for clinicians wishing to maximize sensitivity, they may also consider using the lower, but still acceptable, cut-off of ≥ 2, with the understanding that they are likely to experience greater risk for false positives (24%). For clinical settings that have resources to manage higher false positive rates, or that prefer to maximize sensitivity, providers may consider using the lower cut-off score.
Of note, GAD-2 and GAD-7 scores were moderately correlated with depressive symptoms (PHQ-2), such that individuals who endorsed greater anxiety also endorsed greater depression. These results are consistent with prior studies and warrant future research to determine the unique and shared contributions of depression and anxiety to daily function and quality of life in MS.17 The degree to which responses on the GAD-2 may predict meaningful clinical outcomes above and beyond commonly used depressive symptom screeners (e.g., PHQ-2) is an area warranting further investigation.
Overall, the present study featured several strengths and important implications for clinical practice. First, results supported the hypotheses that the GAD-2 cut-off score generated from the present sample would yield adequate sensitivity and specificity for detecting clinically significant anxiety symptoms. Having established this cut-off, rehabilitation and neurology clinics may be more confident in using this measure with patients. Second, the sample comprised a range of individuals with MS in terms of age, disease duration, MS subtype, and depressive and anxious symptoms. Because the sample was recruited from a multidisciplinary MS clinic, the study allowed for inclusion of patients receiving a range of medical services (e.g., neurology, physiatry, psychology, rehabilitation therapies). Diversity of the sample is especially important, as previous studies investigating depression and anxiety in MS have often been limited to individuals seeking treatment for those conditions, thus yielding a restricted range of symptoms.
Study Limitations
Although the present results have important clinical implications, several limitations must be acknowledged. First, the study featured a cross-sectional design. Use of the obtained cut-off score in predicting future physical and/or functioning will require a longitudinal design. It is possible that recommended cut-off may change over the course of an individual’s disease and lifetime, and research is currently too limited to speculate on how those changes may impact our understanding of anxiety in MS. Second, the study did not employ a criterion standard for diagnosing anxiety disorders such as the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I), as this was beyond the scope of the current study.21 Nonetheless, the GAD-7 has previously been validated against criterion diagnostic interviews. The close correspondence between the GAD-2 and GAD-7 suggests the GAD-2 would perform comparably against criteria like the SCID-I, though future work is needed to confirm this hypothesis. Third, disability severity ratings were not collected, limiting the potential to examine associations between disability severity and anxiety symptoms, and to confirm whether the sample’s range of disability was comparable to the diverse range in other collected demographic and clinical variables. Finally, compared to prior prevalence studies, a relatively smaller number (23, 23%) of the sample met criteria for clinically significant anxiety on the GAD-7. Part of this may be due to the distinction between lifetime prevalence rates, which have largely informed prior studies, versus the point-prevalence rate of the current study. Another explanation may be that prevalence studies have relied on clinical samples of patients who report anxiety and/or depression, as opposed to the present study, which did not exclusively recruit from psychological services. A third explanation may be that individuals with higher levels of anxiety declined to participate in the study because of the study’s cognitive testing procedures. Although we cannot confirm the reason for the study’s lower-than-expected GAD-7 scores, we acknowledge the sample may not generalize to the general MS population, and thus the present analyses should be replicated in a larger sample with greater levels of anxiety.
Conclusions
Despite these limitations, the present study supports the GAD-2 as a clinically useful, pragmatic, and psychometrically valid tool for assessing anxiety symptoms in individuals with MS. With a cut-off score of ≥ 3, the GAD-2 can identify, with high accuracy, clinically significant levels of anxiety. Finally, because the GAD-2 is open-source, brief, and independent of the physiologic symptoms that often accompany MS, this measure can be easily implemented in most clinical settings, including medical rehabilitation settings, and can help guide clinicians in making appropriate referrals to rehabilitation psychology services.
Acknowledgements
The work conducted in this manuscript has not been previously published, nor is it under consideration for publication elsewhere. The contents of this article were developed under a pilot grant from the Consortium of MS Centers (CMSC), Beier (PI). The corresponding author is supported by a grant from the National Institutes of Health, Grant K23HD086154, Hughes (PI).
Abbreviations:
- AUC
area under the curve
- GAD-2
Generalized Anxiety Disorder Scale – 2
- GAD-7
Generalized Anxiety Disorder Scale – 7
- MS
multiple sclerosis
- RRMS
relapsing-remitting MS
- PHQ-2
Patient Health Questionnaire – 2
- PHQ-9
Patient Health Questionnaire – 9
- PPMS
primary progressive MS
- PRMS
progressive relapsing MS
- SPMS
secondary progressive MS
Footnotes
Conflict of Interest
We certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on the authors or on any organization with which they are associated and we certify that all financial and material support for this research and work are clearly identified in the title page of the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mitchell AJ, Benito-León J, González J-MM, Rivera-Navarro J. Quality of life and its assessment in multiple sclerosis: integrating physical and psychological components of wellbeing. The Lancet Neurology. 2005;4(9):556–566. [DOI] [PubMed] [Google Scholar]
- 2.Askari F, Ghajarzadeh M, Mohammadifar M, Azimi A, Sahraian MA, Owji M. Anxiety in patients with multiple sclerosis: association with disability, depression, disease type and sex. Acta Med Iran. 2014;52(12):889–892. [PubMed] [Google Scholar]
- 3.Theaudin M, Romero K, Feinstein A. In multiple sclerosis anxiety, not depression, is related to gender. Mult Scler. 2016;22(2):239–244. [DOI] [PubMed] [Google Scholar]
- 4.Garfield AC, Lincoln NB. Factors affecting anxiety in multiple sclerosis. Disabil Rehabil. 2012;34(24):2047–2052. [DOI] [PubMed] [Google Scholar]
- 5.Feinstein A, O’Connor P, Gray T, Feinstein K. The effects of anxiety on psychiatric morbidity in patients with multiple sclerosis. Mult Scler. 1999;5(5):323–326. [DOI] [PubMed] [Google Scholar]
- 6.Amtmann D, Askew RL, Kim J, et al. Pain affects depression through anxiety, fatigue, and sleep in multiple sclerosis. Rehabil Psychol. 2015;60(1):81–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Janssens AC, van Doorn PA, de Boer JB, et al. Anxiety and depression influence the relation between disability status and quality of life in multiple sclerosis. Mult Scler. 2003;9(4):397–403. [DOI] [PubMed] [Google Scholar]
- 8.Wineman NM. Adaptation to multiple sclerosis: The role of social support, functional disability, and perceived uncertainty. Nurs Res. 1990;39(5):294–299. [PubMed] [Google Scholar]
- 9.Lynch SG, Kroencke DC, Denney DR. The relationship between disability and depression in multiple sclerosis: the role of uncertainty, coping, and hope. Multiple Sclerosis Journal. 2001;7(6):411–416. [DOI] [PubMed] [Google Scholar]
- 10.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders - Fourth Edition - Text Revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 11.Sjonnesen K, Berzins S, Fiest KM, et al. Evaluation of the 9-item Patient Health Questionnaire (PHQ-9) as an assessment instrument for symptoms of depression in patients with multiple sclerosis. Postgrad Med. 2012;124(5):69–77. [DOI] [PubMed] [Google Scholar]
- 12.Korostil M, Feinstein A. Anxiety disorders and their clinical correlates in multiple sclerosis patients. Mult Scler. 2007;13(1):67–72. [DOI] [PubMed] [Google Scholar]
- 13.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. [DOI] [PubMed] [Google Scholar]
- 14.Feinstein A, Magalhaes S, Richard JF, Audet B, Moore C. The link between multiple sclerosis and depression. Nat Rev Neurol. 2014;10(9):507–517. [DOI] [PubMed] [Google Scholar]
- 15.Marrie RA, Horwitz R, Cutter G, Tyry T, Campagnolo D, Vollmer T. The burden of mental comorbidity in multiple sclerosis: frequent, underdiagnosed, and undertreated. Mult Scler. 2009;15(3):385–392. [DOI] [PubMed] [Google Scholar]
- 16.Honarmand K, Feinstein A. Validation of the Hospital Anxiety and Depression Scale for use with multiple sclerosis patients. Mult Scler. 2009;15(12):1518–1524. [DOI] [PubMed] [Google Scholar]
- 17.Terrill AL, Hartoonian N, Beier M, Salem R, Alschuler K. The 7-Item Generalized Anxiety Disorder Scale as a Tool for Measuring Generalized Anxiety in Multiple Sclerosis. International Journal of MS Care. 2015;17(2):49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Korostil M, Feinstein A. Anxiety disorders and their clinical correlates in multiple sclerosis patients. Multiple Sclerosis. 2007;13(1):67–72. [DOI] [PubMed] [Google Scholar]
- 19.Plummer F, Manea L, Trepel D, McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry. 2016;39:24–31. [DOI] [PubMed] [Google Scholar]
- 20.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. [DOI] [PubMed] [Google Scholar]
- 21.First M, RL S, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version (SCID-I) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 22.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–1292. [DOI] [PubMed] [Google Scholar]