Abstract
Background
Low-calorie sweeteners (LCSs), artificial sweeteners, or high-intensity sweeteners are incorporated into foods, beverages, and food and beverage additions (FBAs). Many prior studies have focused on LCS beverage consumption, but not included LCS consumption from foods or FBAs.
Objectives
We aimed to describe the prevalence of LCS consumption by US adults, and to examine the relation between intake of products containing LCSs and macronutrients.
Methods
Two nonconsecutive 24-h dietary recalls from NHANES 2007–2012 and the National Cancer Institute usual intake method were used to estimate prevalence of LCS intake from foods, beverages, and FBAs, and macronutrients among US adults aged ≥19 y (n = 14,098, weighted n = 218,391,752) in a cross-sectional study. The prevalence of LCS consumption from reported foods, beverages, and FBAs among US adults was examined by sociodemographic characteristics and body mass index (BMI). Logistic regression estimated ORs and 95% CIs for associations between sociodemographic characteristics and LCS use (overall and in foods, beverages, and FBAs).
Results
Among adults, 47.8% reported intake of ≥1 food, beverage, or FBA containing LCSs over 2 d. Intake was higher among: women non-Hispanic whites, college graduates or higher, and those with higher income and obese BMIs (P < 0.001). Intake of beverages containing LCSs was higher for ages 51–70 y than 19–30 y and those with overweight and obese BMIs (P < 0.001) than for normal-weight individuals. Calories, carbohydrate, and sugar intake were lower and fiber was higher in LCS-consumers than in nonconsumers. Specifically, calories from beverages were lower in those who reported LCS intake.
Conclusions
Individuals reporting LCS consumption demonstrated lower total energy intake than did individuals without LCS intake. Although the main source of LCSs in the US adult diet was beverages (31.9%), we found that FBAs also present a significant contribution (25.2%), surpassing food (9.3%). This enables targeted understanding of national consumption of these products as well as dietary education and intervention opportunities.
Keywords: NHANES, low-calorie sweetener, artificial sweetener, high-intensity sweetener, adults, macronutrient, dietary, nutritive sweetener
Introduction
Low-calorie sweeteners (LCSs), artificial sweeteners, or high-intensity sweeteners are incorporated into foods, beverages, and food and beverage additions (FBAs) as an alternative to sugars or nutritive sweeteners (NSs). Compared with NSs, LCSs can result in overall dietary calorie reduction and have been successfully used in weight management (1, 2). It also has been suggested that LCSs can assist with weight loss and management of diabetes (3–8). Lower overall total caloric intake has been reported among adults with normal weight, but not overweight or obese, BMIs consuming LCSs (9). In addition, some studies have reported a relation between consumption of LCS-containing beverages and obesity risk (7, 8), whereas a recent study found dietary intake and glycemic response to be equal or better after consumption of beverages containing LCSs compared with water (10). However, controversy still exists with regard to LCS consumption and health effects including weight management (11).
The question of whether LCSs are directly beneficial for weight loss also has been examined in rodent models by multiple authors. Swithers and Davidson (12) reported weight gain and increased adiposity in rats after intake of yogurt with added saccharin compared with added glucose, and consumption of more calories by rats that consumed saccharin-sweetened yogurt (12). Rodents on a high energy, fat, and sugar diet (HE or Westernized diet) fed saccharin compared with glucose yogurt supplements experienced increased adiposity, weight gain, and energy intake (13). However, a recent Australian study replicating Swithers and Davidson's 2008 work found the opposite: greater weight gain and fat pad mass for rats fed glucose-sweetened compared with saccharin-sweetened yogurt (14).
LCS consumption has been associated with healthier lifestyle choices, such as increased physical activity, greater fruit and vegetable intake, and higher overall Healthy Eating Index (HEI) scores (15); however, recent reports suggest LCS intake is increasing in the United States in parallel with rates of overweight and obesity (16, 17). Although diet quality has been assessed in relation to LCS intake through the use of HEI-2010 and macronutrient intake assessed in consumers of LCS-containing beverages, only 1 study has assessed macronutrient intake in consumers of foods, beverages, and packets containing LCSs (18). Some studies have assessed LCS intake from foods and beverages or beverages alone; however, none have fully incorporated the concept of FBAs (2, 19, 20). Examining LCS use in the context of the total diet (foods, beverages, FBAs) is important to better provide targeted food intake guidance.
In the current study our purpose was to assess the prevalence of LCS intake in the total diet of foods, beverages, and FBAs among US adults through the use of 2 nonconsecutive 24-h dietary recalls from the NHANES 2007–2012 and the National Cancer Institute (NCI) usual intake method (21–23). We also examined the relation among overall, no/low, and high intake of LCSs and NSs in items consumed as well as calorie and dietary macronutrient intake levels among individuals with and without reported intake of LCS- and NS-containing items.
Methods
Study design and population
Sociodemographic and dietary data were obtained from the 3 most recent NHANES cycles (2007–2008, 2009–2010, 2011–2012) for this cross-sectional study. The NHANES survey and physical exam are administered in 2-y cycles by the National Center for Health Statistics (NCHS) to a national sample of US adults and children (24). Each NHANES continuous cycle used a complex, multistage probability sample to obtain national-level data with oversampling of certain population subgroups (25). Two nonconsecutive 24-h dietary recalls were collected by trained dietary interviewers for each included NHANES cycle, of which the first was in-person and the second followed 3–10 d later by phone. The USDA Food and Nutrient Database for Dietary Studies (FNDDS) was used to code all food and beverage items reported consumed in the NHANES dietary interview component (What We Eat in America, WWEIA) and to obtain nutrient content (26). The NCI usual intake method was used to estimate macronutrient intake in US adults (defined as ≥19 y old) who did and did not use LCSs (23).
The pooled NHANES 2007–2012 data included 30,442 individuals, of which 18,191 were adults aged ≥19 y. After limiting to adults with data considered reliable by the NCHS, excluding pregnant and lactating women (n = 477) and those without 2 complete nonconsecutive 24-h dietary recalls (n = 3616), the analytic sample was 14,098 US adults (men, n = 6925; women, n = 7173; weighted n = 218,391,752). Those with underweight BMI (n = 237) or missing BMIs (n = 173) also were excluded.
Characteristics
Age was categorized into the following age groups: 19–30, 31–50, 51–70, and ≥71 y. Race/ethnicity was classified as: non-Hispanic white, non-Hispanic black, Hispanic, or other which included non-Hispanic persons reporting multiple races. Education was categorized as: high school graduate/General Educational Development or lower, completing some college or an associate degree, or college graduate or higher. Poverty income ratio was defined as: below the poverty line, at/above the poverty line, or above 3 times the poverty line. BMI (kg/m2) was classified as: underweight (<18.5), normal weight (18.5–24.9), overweight (25–29.9), or obese (≥30).
Food and beverage items, including FBAs, and sweeteners
Those items that were primarily consumed on their own were classed as foods or beverages; however, items not typically used on their own but rather added to or consumed with a food or beverage item were termed “FBAs” (e.g., creamer, sugar/packaged LCSs, ketchup, butter, and salad dressing). Food, beverage, and FBA items were coded as containing LCSs if the USDA item descriptions such as “with low/no-calorie sweetener”, “sugar-free”, or “dietetic/low sugar” were used; or if review of the online ingredients list for processed foods or the recipes for homemade ethnic foods indicated that the items contained LCSs or NSs. The USDA listing of inclusion of sugar and related ingredients was also consulted (https://fnic.nal.usda.gov/food-composition/nutritive-and-nonnutritive-sweetener-resources). The adjudication process for coding of ingested items was described previously (27). If an individual reported intake of food, beverage, or FBA containing LCSs over the 2-d period (two 24-h recalls: 1 in person and 1 by telephone) they were considered positive for LCS intake whereas individuals who did not report LCS intake were considered negative for intake. In addition, individuals were dichotomized based on LCS intake specific to food, beverages, or FBAs. We were also interested in the number of times a person used NSs and total sugars consumed based on reported foods over the 2 d of recall. Based on an initial distribution, we identified NS use ≤6 times over 2 d, which corresponded to 21.5% of the population, as low frequency of NS use and high frequency of NS use was defined as NSs >6 times over 2 d. The following LCS and NS intake groups were used: no or low NSs and no LCSs (10.6%), no or low NSs along with LCSs (10.9%), high NSs and no LCSs (41.6%), or high NSs along with LCSs (36.9%).
Statistical analysis
Demographic characteristics, socioeconomic status (SES) factors, and BMI were compared by food, beverage, and FBA items containing LCSs with the use of descriptive statistics, such as Wald chi-square tests. All analyses accounted for the clustered sampling design and oversampling, and adjustments were made for differential noncoverage and nonresponse adjusted by the 3 continuous NHANES cycles (25, 28). We used multivariate logistic regression to evaluate the associations between demographic characteristics and SES factors, with LCS use (overall and separately in foods, beverages, and FBAs) being the outcome of interest through calculation of ORs and 95% CIs. Models adjusted for covariates including: NHANES cycle, sex, race/ethnicity, age, education, poverty income ratio, and BMI category.
Usual dietary intake levels of nutrients over two 24-h recalls were examined by LCS intake with adjustment for age, race, sex, day, and weekend day through the use of the NCI usual intake estimation methodology (21–23). Usual dietary intake levels of nutrients were also assessed by NS/LCS use and BMI category after adjustment for age, race, sex, day, weekend day, and other NS/LCS intake categories.
All analyses were conducted via SAS, version 9.3 and its complex survey-specific procedures (SAS Institute; Cary, NC). Institutional Review Board approval was not required by the Medical University of South Carolina because the study involved a secondary data analysis and was not deemed to be human subjects research.
Results
The national prevalence of LCS intake overall and in foods, beverages, and FBAs among US adults over 2 d is presented in Table 1. Approximately 48% of adults reported consuming foods (9.3%), beverages (31.9%), or FBAs (25.2%) containing LCSs. Over a 2-d period, 3.0% ± 0.2% of adults reported LCS intake in foods only; 17.5% ± 0.6% in beverages only; and 11.3% ± 0.4% in FBAs only (data not shown). Most individual respondents reported consuming LCSs from multiple dietary sources. Hence, the 25.2% who reported LCS intake in FBAs includes adults who reported LCSs in FBAs only (11.3%); LCSs in beverages and FBAs (9.7%); LCSs in foods and FBAs (1.6%); and LCSs in food, beverages, and FBAs (2.6%) (data not shown). Women, non-Hispanic whites, college graduates or higher, those aged ≥71 y, and those of higher income were more likely to consume food containing LCSs (P < 0.001) than the respective comparison groups. Individuals of these groups (except those aged ≥71 y) as well as obese individuals (BMI > 30) and those aged 51–70 y were also more likely to consume beverages or FBAs containing LCSs than the respective comparison groups (P < 0.001).
TABLE 1.
Percentages ± SEs of NHANES participants reporting LCS intake overall and from foods, beverages, and FBAs by sociodemographic characteristics of the US adult population based on two 24-h dietary recalls1
| Characteristic | Sample, n | Estimate of total US population, n | Any LCS intake | LCS intake in food | LCS intake in beverages | LCS intake in FBAs |
|---|---|---|---|---|---|---|
| Overall mean | 14,098 | 218,391,752 | 47.8 ± 0.7 | 9.3 ± 0.4 | 31.9 ± 0.7 | 25.2 ± 0.7 |
| NHANES cycle | ||||||
| 2007–2008 | 4696 | 71,297,655 | 46.9 ± 1.0 | 8.7 ± 0.6 | 31.9 ± 1.3† | 25.9 ± 1.1 |
| 2009–2010 | 5055 | 72,226,896 | 48.7 ± 1.2 | 10.1 ± 0.7 | 34.0 ± 0.7 | 25.2 ± 1.4 |
| 2011–2012 | 4347 | 74,867,201 | 47.7 ± 1.5 | 9.1 ± 0.6 | 29.9 ± 1.6 | 24.5 ± 1.3 |
| Sex | ||||||
| Male | 6925 | 106,074,482 | 42.9 ± 1.0* | 7.0 ± 0.6* | 28.8 ± 0.9* | 21.4 ± 0.7* |
| Female | 7173 | 112,317,269 | 52.4 ± 0.9 | 11.6 ± 0.5 | 34.8 ± 1.0 | 28.8 ± 1.0 |
| Race/ethnicity | ||||||
| NH white | 6493 | 149,994,144 | 52.9 ± 0.8* | 11.0 ± 0.5* | 35.8 ± 1.0* | 27.9 ± 0.9* |
| NH black | 3045 | 25,268,838 | 34.4 ± 1.3 | 6.2 ± 0.6 | 21.6 ± 1.1 | 18.9 ± 0.9 |
| Hispanic | 3536 | 29,792,822 | 38.7 ± 1.3 | 5.3 ± 0.4 | 24.3 ± 1.3 | 20.5 ± 1.0 |
| Other | 1054 | 1,333,594 | 36.3 ± 2.7 | 5.9 ± 1.1 | 24.7 ± 2.4 | 17.4 ± 1.9 |
| Age category, y | ||||||
| 19–30 | 2672 | 4,619,435 | 35.0 ± 1.6* | 4.6 ± 0.5* | 24.4 ± 1.4* | 14.1 ± 1.3* |
| 31–50 | 4605 | 81,004,552 | 45.5 ± 1.3 | 8.3 ± 0.7 | 32.0 ± 1.3 | 22.0 ± 1.0 |
| 51–70 | 4554 | 6,772,176 | 56.0 ± 1.4 | 12.2 ± 0.8 | 36.9 ± 1.5 | 32.4 ± 1.1 |
| 71–80 | 2267 | 23,471,084 | 57.3 ± 1.4 | 14.0 ± 0.9 | 32.0 ± 1.3 | 37.2 ± 1.6 |
| Education | ||||||
| High school grad/GED or lower | 6765 | 86,882,020 | 42.7 ± 0.9* | 7.5 ± 0.6* | 28.7 ± 1.1* | 22.3 ± 0.9† |
| Some college or associates degree | 3883 | 65,220,752 | 46.3 ± 1.2 | 8.5 ± 0.7 | 30.0 ± 1.1 | 25.5 ± 1.0 |
| College graduate or higher | 3062 | 62,112,675 | 58.0 ± 1.6 | 13.2 ± 0.8 | 39.3 ± 1.9 | 29.9 ± 1.5 |
| Poverty income ratio | ||||||
| Below poverty line | 5964 | 68,310,309 | 37.7 ± 1.1* | 5.9 ± 0.4* | 24.5 ± 0.9* | 19.1 ± 0.8* |
| At/above poverty line | 3707 | 6,106,448 | 48.1 ± 1.5 | 8.7 ± 0.6 | 32.4 ± 1.3 | 25.1 ± 1.0 |
| Above 3× poverty line | 3270 | 74,646,259 | 57.8 ± 1.1 | 12.9 ± 0.8 | 39.2 ± 1.4 | 31.5 ± 1.2 |
| BMI category2 | ||||||
| Underweight | 237 | 3,442,943 | 27.1 ± 4.2* | 7.6 ± 2.3 | 10.3 ± 3.1* | 15.1 ± 2.9* |
| Normal weight | 3828 | 64,638,135 | 39.5 ± 1.6 | 8.5 ± 0.6 | 24.1 ± 1.2 | 20.0 ± 1.3 |
| Overweight | 4636 | 71,655,950 | 49.3 ± 1.1 | 9.4 ± 0.6 | 32.5 ± 1.3 | 26.0 ± 0.9 |
| Obese | 5224 | 76,608,215 | 54.4 ± 1.3 | 10.0 ± 0.6 | 39.2 ± 1.3 | 29.3 ± 1.0 |
1Values are % ± SEs unless otherwise indicated. *Statistically significant differences between categories within a column at P < 0.001 (i.e., for Any LCS intake the prevalence is different in men and women). FBA, food and beverage addition; GED, General Educational Development test; LCS, low-calorie sweetener; NH, non-Hispanic.
2BMI (kg/m2) was defined as: underweight (<18.5), normal weight (18.5–24.9), overweight (25–29.9), or obese (≥30), and was unavailable for 173 individuals.
Table 2 displays ORs and 95% CIs predicting LCS intake across 2 d overall and in foods, beverages, and FBAs among US adults. The odds of LCS intake overall and in food and FBAs increased with age. More specifically, the odds of LCS use in FBAs were 1.37 (95% CI: 1.10, 1.71) for 31- to 50-y-olds, more than 2-fold for 51- to 70-y-olds (OR = 2.20, 95% CI: 1.73, 2.79), and 3-fold for ≥71-y-olds (OR = 3.06, 95% CI: 2.36, 3.96) compared with 19- to 30-y-olds. LCS intake in foods had higher odds among persons of all age groups than 19- to 30-y-olds, whereas LCS intake in beverages had higher odds among 51- to 70-y-olds. The odds of LCS intake overall and in foods and beverages were elevated among those with college education or higher compared with high school education or lower. Differences in LCS intake were also observed by BMI category with higher odds overall and in beverages and FBAs among those classed as overweight and obese BMIs compared with normal weight.
TABLE 2.
ORs and 95% CIs predicting LCS intake overall and in foods, beverages, and FBAs by US adults over 2 d1
| OR (95% CI) | ||||
|---|---|---|---|---|
| Characteristic | Any LCS intake | LCS intake in foods | LCS intake in beverages | LCS intake in FBAs |
| Sex | ||||
| Female | 1.00 | 1.00 | 1.00 | 1.00 |
| Male | 0.63 (0.56, 0.71) | 0.54 (0.42, 0.69) | 0.70 (0.62, 0.80) | 0.66 (0.59, 0.73) |
| NHANES cycle | ||||
| 2007–2008 | 1.00 | 1.00 | 1.00 | 1.00 |
| 2009–2010 | 1.08 (0.96, 1.22) | 1.20 (0.98, 1.48) | 1.10 (0.95, 1.27) | 0.96 (0.80, 1.15) |
| 2011–2012 | 1.05 (0.91, 1.22) | 1.09 (0.90, 1.32) | 0.90 (0.73, 1.10) | 0.94 (0.79, 1.13) |
| Race/ethnicity | ||||
| NH white | 1.00 | 1.00 | 1.00 | 1.00 |
| NH black | 0.52 (0.45, 0.60) | 0.68 (0.54, 0.87) | 0.51 (0.42, 0.61) | 0.70 (0.59, 0.82) |
| Hispanic | 0.78 (0.66, 0.91) | 0.70 (0.59, 0.83) | 0.68 (0.56, 0.83) | 0.98 (0.82, 1.17) |
| Other | 0.62 (0.49, 0.78) | 0.57 (0.39, 0.83) | 0.74 (0.56, 0.97) | 0.69 (0.50, 0.96) |
| Age category, y | ||||
| 19–30 | 1.00 | 1.00 | 1.00 | 1.00 |
| 31–50 | 1.15 (0.96, 1.37) | 1.39 (1.03, 1.89) | 1.10 (0.91, 1.32) | 1.37 (1.10, 1.71) |
| 51–70 | 1.66 (1.39, 1.99) | 2.06 (1.52, 2.81) | 1.27 (1.03, 1.58) | 2.20 (1.73, 2.79) |
| ≥71 | 1.98 (1.59, 2.45) | 2.74 (2.04, 3.69) | 1.09 (0.86, 1.38) | 3.06 (2.36, 3.96) |
| Education | ||||
| High school grad/GED or lower | 1.00 | 1.00 | 1.00 | 1.00 |
| Some college or associates degree | 1.03 (0.89, 1.19) | 0.99 (0.73, 1.33) | 0.93 (0.78, 1.11) | 1.15 (0.93, 1.41) |
| College graduate or higher | 1.64 (1.40, 1.92) | 1.64 (1.24, 2.19) | 1.39 (1.14, 1.69) | 1.36 (1.07, 1.73) |
| Poverty income ratio | ||||
| Below poverty line | 1.00 | 1.00 | 1.00 | 1.00 |
| At/above poverty line | 1.30 (1.13, 1.50) | 1.30 (1.05, 1.60) | 1.31 (1.12, 1.53) | 1.24 (1.06, 1.46) |
| Above 3× poverty line | 1.71 (1.52, 1.92) | 1.76 (1.32, 2.36) | 1.56 (1.38, 1.76) | 1.63 (1.34, 1.99) |
| BMI category2 | ||||
| Underweight | 0.69 (0.41, 1.17) | 1.07 (0.42, 2.74) | 0.38 (0.17, 0.85) | 0.89 (0.54, 1.47) |
| Normal weight | 1.00 | 1.00 | 1.00 | 1.00 |
| Overweight | 1.54 (1.28, 1.84) | 1.20 (0.94, 1.54) | 1.57 (1.29, 1.92) | 1.40 (1.18, 1.67) |
| Obese | 2.13 (1.81, 2.51) | 1.30 (1.08, 1.57) | 2.35 (1.99, 2.78) | 1.70 (1.46, 1.97) |
1Adjusted for column covariates: sex, race/ethnicity, age, education, poverty income ratio, and BMI category. Sample: 12,440 people with completed data across all covariates modeled. Models compared LCS intake overall and in food, beverages, and FBAs among characteristics by columns. FBA, food and beverage addition; GED, General Educational Development test; LCS, low-calorie sweetener; NH, non-Hispanic.
2BMI (kg/m2) defined as: underweight (<18.5), normal weight (18.5–24.9), overweight (25–29.9), or obese (≥30).
The nutrient intake (mean ± SE) of individuals by reported LCS intake is shown in Table 3 with adjustment for age, race, sex, day, and weekend day. Compared with nonconsumers, mean calorie (2299 compared with 2122 kcal), carbohydrates (286.5 compared with 253.2 g), and total sugars (135.7 compared with 110.9 g) were significantly lower for LCS consumers (P < 0.001). Fiber intake was significantly higher for LCS consumers than nonconsumers (17.7 compared with 16.4 g; P < 0.001).
TABLE 3.
Mean ± SE usual dietary intake levels of nutrients by US adults by LCS category of consumption over 2 d1
| Nutrient | No LCS intake (52.2%) | LCS intake (47.8%) | P value2 |
|---|---|---|---|
| Energy, kcal | 2299 ± 44 | 2122 ± 69 | <0.001* |
| From food | 1668 ± 32.4 | 1629 ± 59.0 | 0.4468 |
| From beverages | 515 ± 12.1 | 339.4 ± 7.6 | <0.001* |
| From food and beverage additions | 158 ± 7.4 | 154 ± 8.8 | 0.7266 |
| Energy density, kcal/g | 0.68 ± 0.0 | 0.60 ± 0.0 | <0.001* |
| Carbohydrate, g | 286.5 ± 3.3 | 253.2 ± 5.8 | <0.001* |
| Protein, g | 81.7 ± 2.2 | 81.8 ± 2.7 | 0.6497 |
| Total fat, g | 84.7 ± 1.9 | 81.2 ± 3.5 | 0.0776 |
| Total sugars, g | 135.7 ± 2.1 | 110.9 ± 1.9 | <0.001* |
| Dietary fiber, g | 16.4 ± 0.4 | 17.7 ± 0.5 | <0.001* |
1Adjusted for: age, race, sex, day, and weekend day. Sample: 14,098 people representative of 218,391,752 adults nationally. *Statistically significant at P < 0.001. LCS, low-calorie sweetener.
2 P values compared usual dietary intake levels of nutrients by LCS use.
The national prevalence (percentage ± SE) of NS use is reported in Table 4. Only 0.1% of the population reported no NS intake over the 2-d period; whereas 21.5% reported intake of foods, beverages, or FBAs containing NSs ≤6 times. As expected, mean total sugars consumed increased from 27.5 g among individuals whose diet did not include NSs to 158.8 g among individuals who used NSs ≥11 times over the 2-d period. The prevalence of LCS use ranged from 15.6% among individuals without reported dietary NS intake to 54.4% among those who used NSs 4 times over the 2-d period. Based on the distribution of the reported NS intake times over 2 d, 21.5% of adults were categorized as having no or low frequency of NS use (≤6 times) and 78.5% of individuals were categorized as having high frequency of NS use (>6 times).
TABLE 4.
NS intake in food, beverage, and FBA by US adults over 2 d: frequency, mean ± SE grams of total sugars consumed by NS count, and prevalence of any LCS intake by NS count1
| NS category | NS intake over 2 d, n | Distribution, % ± SE | Total sugars, mean ± SE, g | Any LCS intake, % yes ± SE |
|---|---|---|---|---|
| No or low NS intake2 21.5% + 0.58% | 0 | 0.1 ± 0.1 | 27.5 ± 4.4 | 15.6 ± 8.4 |
| 1 | 0.5 ± 0.1 | 44.9 ± 5.3 | 33.8 ± 6.0 | |
| 2 | 1.3 ± 0.1 | 54.3 ± 5.2 | 39.3 ± 5.8 | |
| 3 | 2.7 ± 0.2 | 61.6 ± 2.6 | 50.7 ± 3.9 | |
| 4 | 4.0 ± 0.3 | 68.3 ± 2.7 | 54.4 ± 3.2 | |
| 5 | 5.7 ± 0.3 | 81.7 ± 2.3 | 51.7 ± 2.5 | |
| 6 | 7.1 ± 0.3 | 88.1 ± 2.3 | 51.7 ± 2.5 | |
| High NS intake2 78.5% + 0.58% | 7 | 8.1 ± 0.4 | 99.0 ± 2.8 | 44.4 ± 2.0 |
| 8 | 9.2 ± 0.3 | 109.9 ± 2.0 | 51.1 ± 2.1 | |
| 9 | 8.9 ± 0.3 | 113.7 ± 2.7 | 47.3 ± 2.6 | |
| 10 | 9.9 ± 0.4 | 122.4 ± 3.2 | 50.0 ± 2.0 | |
| ≥11 | 42.4 ± 0.7 | 158.8 ± 2.3 | 45.9 ± 0.8 |
1Adjusted for: day and weekend day. Sample: 14,098 people representative of 218,391,752 adults nationally. FBA, food and beverage addition; LCS, low-calorie sweetener; NS, nutritive sweetener.
2No or low-frequency NS use was defined as ≤6 times over a 2-d period and high-frequency NS use was defined as >6 times over 2 d.
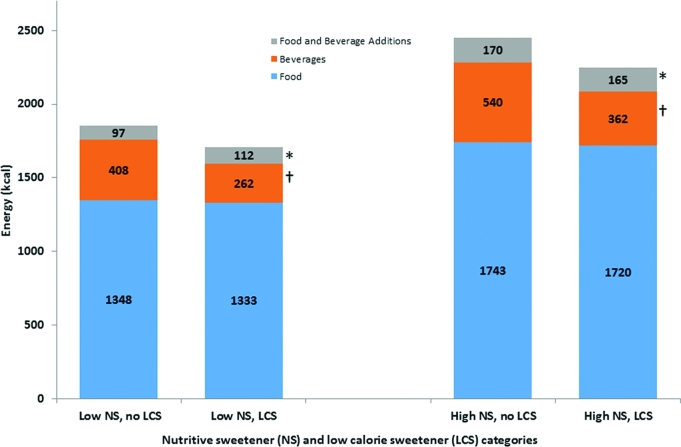
Figure 1 presents mean ± SE macronutrient intake of energy for US adults by LCS and NS intake categories adjusted for age, race, sex, day, and weekend day. Among individuals consuming NSs ≤6 times over the 2 d, mean intake of energy (1797 compared with 1699 kcal) was significantly lower for LCS consumers than nonconsumers (P < 0.05), as were carbohydrates (211.2 compared with 188.6 g) and total sugars (80.8 compared with 72.2 g) (data not shown). Among NS consumers who used NSs ≤6 times over the 2 d, dietary fiber was significantly higher than among nonconsumers of LCSs (14.8 compared with 14.2 g; P < 0.05) (data not shown). Results were similar in those reporting NS use ≥6 times over the 2 d with total fat also differing significantly between the 2 groups.
FIGURE 1.
Usual dietary intake levels of energy from foods, beverages, and food and beverage additions by LCS category over 2 d stratified by NS category. Low NS was defined as using NS ≤6 times over a 2-d period and high NS was defined as using >6 times over a 2-d period. Adjusted for age, race, sex, day, weekend day, and other NS/LCS categories. †Statistically significant at P < 0.05; *Statistically significant at P < 0.001. LCS, low-calorie sweetener; NS, nutritive sweetener.
The nutrient intake (mean ± SE) of individuals by reported LCS intake was also examined by BMI category with adjustment for age, race, sex, day, and weekend day (Table 5). The energy, carbohydrate, and total sugar intake among overweight or obese (BMI) US adults who reported use of LCS-containing foods, beverages, or FBAs were significantly lower compared with those without LCS intake, whereas fiber was significantly higher (P < 0.05). Moreover, when examining energy from food, beverages, and FBAs in those with reported LCS use, reduced energy was largely the result of reduced calories from beverages in individuals with either an overweight or obese BMI, and from both food and beverages in those with a normal BMI.
TABLE 5.
Mean ± SE usual dietary intake levels of nutrients from food, beverage, and FBA items by LCS intake among US adults over 2 d stratified by BMI category1
| LCS intake | |||
|---|---|---|---|
| No (51.8%) | Yes (48.2%) | P value | |
| Normal weight2 | |||
| Energy, kcal | 2346 ± 48.2 | 2080 ± 97.8 | <0.001* |
| From food | 1696 ± 41.3 | 1570 ± 85.8 | 0.004† |
| From beverages | 517 ± 15.6 | 369 ± 15.0 | <0.001* |
| From FBAs | 162 ± 8.8 | 157 ± 12.5 | 0.7302 |
| Energy density, kcal/g | 0.69 ± 0.01 | 0.61 ± 0.02 | <0.001* |
| Carbohydrate, g | 292.9 ± 5.7 | 256.1 ± 11.9 | <0.001* |
| Protein, g | 83.0 ± 2.2 | 77.9 ± 3.2 | 0.004† |
| Total fat, g | 85.2 ± 2.2 | 77.0 ± 4.4 | <0.001* |
| Total sugars, g | 138.1 ± 3.6 | 115.9 ± 3.7 | <0.001* |
| Dietary fiber, g | 17.4 ± 0.5 | 18.1 ± 1.0 | <0.001* |
| Overweight2 | |||
| Energy, kcal | 2305 ± 53.8 | 2164 ± 58.8 | <0.001* |
| From food | 1675 ± 43.4 | 1648 ± 43.1 | 0.364 |
| From beverages | 512 ± 20.0 | 356 ± 12.3 | <0.001* |
| From FBAs | 157 ± 11.8 | 154 ± 11.8 | 0.6175 |
| Energy density, kcal/g | 0.68 ± 0.01 | 0.59 ± 0.02 | <0.001* |
| Carbohydrate, g | 285.4 ± 3.6 | 259.5 ± 3.4 | <0.001* |
| Protein, g | 82.7 ± 2.7 | 82.5 ± 3.6 | 0.6923 |
| Total fat, g | 85.3 ± 2.7 | 81.1 ± 4.4 | 0.1596 |
| Total sugars, g | 135.6 ± 2.5 | 114.7 ± 2.4 | <0.001* |
| Dietary fiber, g | 16.3 ± 0.7 | 18.5 ± 0.6 | <0.001* |
| Obese | |||
| Energy, kcal | 2258 ± 36.1 | 2127 ± 51.2 | 0.0033† |
| From food | 1640 ± 25.0 | 1662 ± 48.2 | 0.133 |
| From beverages | 512 ± 16.7 | 307 ± 9.4 | <0.001* |
| From FBAs | 150 ± 6.8 | 151 ± 6.7 | 0.8465 |
| Energy density, kcal/g | 0.66 ± 0.01 | 0.59 ± 0.01 | <0.001* |
| Carbohydrate, g | 281.2 ± 4.0 | 247.2 ± 5.1 | <0.001* |
| Protein, g | 80.2 ± 2.4 | 83.9 ± 1.9 | 0.0173† |
| Total fat, g | 83.7 ± 1.7 | 84.3 ± 2.8 | 0.3703 |
| Total sugars, g | 133.2 ± 2.9 | 105.1 ± 2.2 | <0.001* |
| Dietary fiber, g | 15.5 ± 0.4 | 16.7 ± 0.5 | <0.001* |
1Adjusted for: age, race, sex, day, and weekend day. Sample: 13,688 people representative of 212,902,300 adults nationally. BMI (kg/m2) was defined as: normal weight (18.5–24.9), overweight (25–29.9), or obese (≥30). Those with underweight (<18.5, n = 237) or missing (n = 173) BMIs were excluded. †Statistically significant at P < 0.05; *statistically significant at P < 0.001. FBA, food and beverage addition; LCS, low-calorie sweetener.
2Ten percent of individuals with a normal-weight BMI used LCSs and 20.0% did not, 15.1% of individuals with an overweight BMI used LCSs and 18.6% did not, and 18.2% of individuals with an obese BMI used LCSs and 17.8% did not use LCSs.
Discussion
Our study examined characteristics associated with the prevalence of LCS intake in adults from 2007–2012. Over a 2-d period, 48% of US adults reported LCS intake in foods, beverages, or FBAs, which is higher than past reports based on earlier NHANES cycles involving 1-d (16, 29) or 2-d (18) recall. The majority of LCS intake was in beverages (31.9%); however, an additional 15.9% of individuals reported LCS intake in foods and/or FBAs who did not report consumption of LCSs in beverages. Consistent with previous research, there were higher odds of LCS intake among non-Hispanic whites, women, elderly (aged ≥71 y), and persons of higher SES (29), although we also observed higher odds of LCS intake among individuals with obese BMIs. LCS intake in FBAs and food appeared to increase with age, whereas intake in beverages was highest among 51–70-y-olds.
Nutrient intake was also examined and calorie, carbohydrate, and sugar intake were found to be significantly lower (and fiber higher) in individuals who reported intake of foods, beverages, and FBAs containing LCSs than in individuals who did not report LCS intake. Our findings of fewer kilocalories per gram among individuals who report LCS intake are consistent with previous studies (1) and hold when stratified by level of NS use. Because obesity is a potential confounder of the relation between LCSs and nutrient level, LCS intake was further stratified by BMI category as consistent with the literature (16). Differences in nutrient levels were observed within different BMI categories. Compared with adults with reported LCS intake, energy, carbohydrate, and sugar levels were elevated in adults without reported LCS intake regardless of BMI category.
Previous studies
LCS intake in beverages has been assessed by previous studies, but few have assessed intake in food and/or FBAs (2, 9, 16, 18, 30). Sylvetsky et al. (18) examined LCS intake from foods, beverages, and packets over two 24-h dietary recalls with the use of USDA FNDDS food descriptions. They also assessed LCS intake through meals and snacks and when consumed alone (separate from foods, beverages, meals, or snacks) (18). Meal occasions were defined according to past studies (31); FBAs such as pickle relish, mayonnaise, or ketchup were considered as foods in the analysis (18) (AC Sylvetsky, George Washington University, BP Marriott, personal communication, 2017).
Piernas et al. (2) found lower diet quality among LCS-beverage consumers than nonconsumers. However, Drewnowski and Rehm (15) reported higher dietary quality scores (via the HEI-2005) among consumers of LCS beverages and foods. In addition to providing fewer kilocalories per gram than caloric sweeteners, LCS use has been associated with healthier lifestyle choices, such as increased fruit/vegetable intake (2) and physical activity levels (15). Although a large proportion of LCS intake results from LCS-containing beverages, this pertains to only a single behavior. The addition of foods and separately FBAs to this analysis gives insight into eating as well as drinking behaviors, enabling identification of dietary behaviors as targets for intervention.
From 1999 to 2008, the prevalence of LCS intake in the United States increased with ≥50-y-olds and women experiencing the greatest increase, although an increase was not observed over NHANES cycles, 2005–2008 (16, 29). Intake of beverages containing LCSs also increased among women during this period (29). However, these studies involved only a single dietary recall which may underestimate the true prevalence of LCS use. Further, recent studies utilizing NHANES data have not evaluated macronutrient intake in relation to LCSs (16, 29).
Strengths and limitations
Our results were based on dietary information from two 24-h recalls, and are subject to limitations. For the 24-h recall data available from NHANES, underreporting portion size of all food and drink items has been cited as an issue and may affect nutrient levels, which may underestimate overall LCS and NS intake among US adults (32). Although differential misclassification may occur owing to misreporting by BMI category, after further stratifying LCS intake by BMI category, differences in nutrient levels including total energy remained. Moreover, capturing use in food and FBAs reduces misclassification when categorizing individuals based on reported LCS intake. Our use of dietary data from 3 continuous NHANES cycles (2007–2012), and the matching versions of USDA's FNDDS 5.0 (26), does not reflect current (2018 LCS) intake or market availability in food, beverage, and FBA items. Further, our ability to identify the specific type of LCS and other sweeteners included in this analysis was limited by the FNDDS database, which may differ based on subject demographics, BMI, or other factors. Despite the potential limitations of NHANES and FNDDS, it is the most comprehensive nationally representative data for dietary intake studies in the United States. Further, the USDA's Automated Multiple-Pass Method used to collect the dietary intake data aims to minimize misreporting of all food, beverage, and FBA items (33, 34). A third limitation is the cross-sectional design which limits our scope to associations and prevents examination of temporal relations between the factors examined. Unlike previous reports of only beverages, we examined all food, beverage, and FBA items reported in two 24-h periods along with macronutrient intake. In addition, we used existing FNDDS food group categories to examine the food items, along with similar grouping for all beverages reported in order to assess LCSs among all items.
In conclusion, our findings indicate that individuals who report intake of LCS-containing items, alone or in combination with no or low NSs, have lower total energy intake than individuals without reported LCS intake and with reported LCS intake with high NSs. These data confirmed that the main source of LCSs in the US adult diet was beverages at roughly 32% but identified that a quarter of the US adult population consumed LCSs from FBAs with only 9% having foods as a LCS source. These results provide significant new understanding of eating patterns in the United States and thus targets for specific dietary education and intervention.
Acknowledgments
BPM, KJH, DMDV, DG, and JVSP: designed the research; BPM, KJH, DMDV, and AMM: conducted the research including acquiring data; KJH and AMM: analyzed the data and performed statistical analysis; AMM and KJH: wrote the manuscript draft; AMM, KJH, and BPM: had responsibility for final content; BPM, as corresponding author, had full access to the data in the study and final responsibility for the decision to submit for publication; and all authors: inspected and contributed to the interpretation of the data and contributed to, read, and approved the final manuscript.
Notes
Supported as a collaborative project by the PepsiCo R&D Research Fellows Program of PepsiCo, Inc. (Medical University of South Carolina contract no. 2013–2129806 to BMM).
Scientists from the sponsor were involved in the study design; interpretation of data; writing of the report; and in the decision to submit the article for publication. The opinions expressed in this report are those of the authors and do not necessarily represent the position or policy of PepsiCo, Inc.
Author disclosures: JVSP is a full-time employee of PepsiCo, Inc.; DG is a former employee of PepsiCo,Inc. AMM, KJH, DMDV, and BPM, no conflicts of interest
Present address for DMDV: Department of Nutrition, Athletic Training and Exercise Science, Marywood University, Scranton, PA 18509. Present address for DG: NutriSci, Inc., Mt. Kisco, NY 10549.
Abbreviations used:
- FBA
food and beverage addition
- FNDDS
Food and Nutrient Database for Dietary Studies
- HEI
Healthy Eating Index
- LCS
low-calorie sweetener
- NCI
National Cancer Institute
- NS
nutritive sweetener
- SES
socioeconomic status
- WWEIA
What We Eat in America
References
- 1. Anderson GH, Foreyt J, Sigman-Grant M, Allison DB. The use of low-calorie sweeteners by adults: impact on weight management. J Nutr 2012;142(6):1163S–9S. [DOI] [PubMed] [Google Scholar]
- 2. Piernas C, Mendez MA, Ng SW, Gordon-Larsen P, Popkin BM. Low-calorie- and calorie-sweetened beverages: diet quality, food intake, and purchase patterns of US household consumers. Am J Clin Nutr 2014;99(3):567–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gardner C, Wylie-Rosett J, Gidding SS, Steffen LM, Johnson RK, Reader D, Lichtenstein AH; American Heart Association Nutrition Committee of the Council on Nutrition, Physical Activity and Metabolism, Council on Arteriosclerosis, Thrombosis and Vascular Biology, Council on Cardiovascular Disease in the Young, and the American Diabetes Association Nonnutritive sweeteners: current use and health perspectives: a scientific statement from the American Heart Association and the American Diabetes Association. Circulation 2012;126(4):509–19. [DOI] [PubMed] [Google Scholar]
- 4. Tate DF, Turner-McGrievy G, Lyons E, Stevens J, Erickson K, Polzien K, Diamond M, Wang X, Popkin B. Replacing caloric beverages with water or diet beverages for weight loss in adults: main results of the Choose Healthy Options Consciously Everyday (CHOICE) randomized clinical trial. Am J Clin Nutr 2012;95(3):555–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Peters JC, Wyatt HR, Foster GD, Pan Z, Wojtanowski AC, Vander Veur SS, Herring SJ, Brill C, Hill JO. The effects of water and non-nutritive sweetened beverages on weight loss during a 12-week weight loss treatment program. Obesity (Silver Spring) 2014;22(6):1415–21. [DOI] [PubMed] [Google Scholar]
- 6. Rogers PJ, Hogenkamp PS, de Graaf C, Higgs S, Lluch A, Ness AR, Penfold C, Perry R, Putz P, Yeomans MR et al. , Does low-energy sweetener consumption affect energy intake and body weight? A systematic review, including meta-analyses, of the evidence from human and animal studies. Int J Obes (Lond) 2016;40(3):381–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fowler SP, Williams K, Hazuda HP. Diet soda intake is associated with long-term increases in waist circumference in a biethnic cohort of older adults: the San Antonio Longitudinal Study of Aging. J Am Geriatr Soc 2015;63(4):708–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fowler SP, Williams K, Resendez RG, Hunt KJ, Hazuda HP, Stern MP. Fueling the obesity epidemic? Artificially sweetened beverage use and long-term weight gain. Obesity (Silver Spring) 2008;16(8):1894–900. [DOI] [PubMed] [Google Scholar]
- 9. Bleich SN, Wolfson JA, Vine S, Wang YC. Diet-beverage consumption and caloric intake among US adults, overall and by body weight. Am J Public Health 2014;104(3):e72–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Leahy M, Ratliff JC, Riedt CS, Fulgoni VL. Consumption of low-calorie sweetened beverages compared to water is associated with reduced intake of carbohydrates and sugar, with no adverse relationships to glycemic responses: results from the 2001–2012 National Health and Nutrition Examination Surveys. Nutrients 2017;9(9):928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sylvetsky AC, Rother KI. Trends in the consumption of low-calorie sweeteners. Physiol Behav 2016;164(Pt B):446–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Swithers SE, Davidson TL. A role for sweet taste: calorie predictive relations in energy regulation by rats. Behav Neurosci 2008;122(1):161–73. [DOI] [PubMed] [Google Scholar]
- 13. Swithers SE, Sample CH, Davidson TL. Adverse effects of high-intensity sweeteners on energy intake and weight control in male and obesity-prone female rats. Behav Neurosci 2013;127(2):262–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Boakes RA, Kendig MD, Martire SI, Rooney KB. Sweetening yoghurt with glucose, but not with saccharin, promotes weight gain and increased fat pad mass in rats. Appetite 2016;105:114–28. [DOI] [PubMed] [Google Scholar]
- 15. Drewnowski A, Rehm CD. Consumption of low-calorie sweeteners among U.S. adults is associated with higher Healthy Eating Index (HEI 2005) scores and more physical activity. Nutrients 2014;6(10):4389–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sylvetsky AC, Welsh JA, Brown RJ, Vos MB. Low-calorie sweetener consumption is increasing in the United States. Am J Clin Nutr 2012;96(3):640–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zick CD, Stevens RB. Time spent eating and its implications for Americans’ energy balance. Soc Indic Res 2011;101(2):267–73. [Google Scholar]
- 18. Sylvetsky AC, Jin Y, Clark EJ, Welsh JA, Rother KI, Talegawkar SA. Consumption of low-calorie sweeteners among children and adults in the United States. J Acad Nutr Diet 2017;117(3):441–8.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. An R. Beverage consumption in relation to discretionary food intake and diet quality among US adults, 2003 to 2012. J Acad Nutr Diet 2016;116(1):28–37. [DOI] [PubMed] [Google Scholar]
- 20. Gibson SA, Horgan GW, Francis LE, Gibson AA, Stephen AM. Low calorie beverage consumption is associated with energy and nutrient intakes and diet quality in British adults. Nutrients 2016;8(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tooze JA, Midthune D, Dodd KW, Freedman LS, Krebs-Smith SM, Subar AF, Guenther PM, Carroll RJ, Kipnis V. A new statistical method for estimating the usual intake of episodically consumed foods with application to their distribution. J Am Diet Assoc 2006;106(10):1575–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Souverein OW, Dekkers AL, Geelen A, Haubrock J, de Vries JH, Ocke MC, Harttig U, Boeing H, van 't Veer P; EFCOVAL Consortium Comparing four methods to estimate usual intake distributions. Eur J Clin Nutr 2011;65(Suppl 1):S92–101. [DOI] [PubMed] [Google Scholar]
- 23. NCI Division of Cancer Control & Population Sciences Usual dietary intakes: the NCI method. Bethesda, MD: The National Cancer Institute's Division of Cancer Control and Population Sciences; 2015[cited 2017 July 31]. Available from: https://epi.grants.cancer.gov/diet/usualintakes/method.html. [Google Scholar]
- 24. CDC About the National Health and Nutrition Examination Survey. Atlanta, GA: CDC/National Center for Health Statistics; 2017[cited 2017 July 31]. Available from: https://www.cdc.gov/nchs/nhanes/about_nhanes.htm. [Google Scholar]
- 25. Johnson CL, Paulose-Ram R, Ogden CL, Carroll MD, Kruszon-Moran D, Dohrmann SM, Curtin LR. National Health and Nutrition Examination Survey: analytic guidelines, 1999–2010. National Center for Health Statistics Vital Health Stat 2013;161:1–24. [PubMed] [Google Scholar]
- 26. Martin CL, Montville JB, Steinfeldt LC, Omolewa-Tomobi G, Heendeniya KY, Adler ME, Moshfegh AJ. USDA Food and Nutrient Database for Dietary Studies 2011–2012: Documentation and User Guide. Beltsville, MD: US Department of Agriculture, Agricultural Research Service, USDA Food Surveys Research Group; 2012[updated October 2014]. Available from: https://www.ars.usda.gov/ARSUserFiles/80400530/pdf/fndds/fndds_2011_2012_doc.pdf. [Google Scholar]
- 27. DellaValle DM, Malek AM, Hunt KJ, St. Peter JV, Greenberg D, Marriott BP. Low calorie sweeteners in foods, beverages, and food and beverage additions: NHANES 2007–2012. Curr Dev Nutr 2018; 10.1093/cdn/nzy024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. CDC, NCHS National Health and Nutrition Examination Survey: analytic guidelines, 2011–2012. Statistics 2013. Available from: https://stacks.cdc.gov/view/cdc/44830. [Google Scholar]
- 29. Drewnowski A, Rehm CD. Socio-demographic correlates and trends in low-calorie sweetener use among adults in the United States from 1999 to 2008. Eur J Clin Nutr 2015;69(9):1035–41. [DOI] [PubMed] [Google Scholar]
- 30. Piernas C, Ng SW, Popkin B. Trends in purchases and intake of foods and beverages containing caloric and low-calorie sweeteners over the last decade in the United States. Pediatr Obes 2013;8(4):294–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Murakami K, Livingstone MB. Associations between meal and snack frequency and diet quality in US adults: National Health and Nutrition Examination Survey 2003–2012. J Acad Nutr Diet 2016;116(7):1101–13. [DOI] [PubMed] [Google Scholar]
- 32. Briefel RR, Sempos CT, McDowell MA, Chien S, Alaimo K. Dietary methods research in the third National Health and Nutrition Examination Survey: underreporting of energy intake. Am J Clin Nutr 1997;65(4 Suppl):1203S–9S. [DOI] [PubMed] [Google Scholar]
- 33. Moshfegh AJ, Rhodes DG, Baer DJ, Murayi T, Clemens JC, Rumpler WV, Paul DR, Sebastian RS, Kuczynski KJ, Ingwersen LA et al. , The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am J Clin Nutr 2008;88(2):324–32. [DOI] [PubMed] [Google Scholar]
- 34. Ahuja JKC, Montville JB, Omolewa-Tomobi G, Heendeniya KY, Martin CL, Steinfeldt LC, Anand J, Adler ME, LaComb RP, Moshfegh AJ. Appendix C. Dietary methods research: overview of What We Eat in America food categories: FSRG-defined food groups. Beltsville, MD: Department of Agriculture, Agricultural Research Service, USDA Food Surveys Research Group; 2012[updated October 2014]. Available from: http://www.ars.usda.gov/SP2UserFiles/Place/80400530/pdf/fndds/fndds5_doc.pdf#page=64. [Google Scholar]