Abstract
AIM
To investigate the causes of the recurrent carpal tunnel syndrome (CTS) and implemented surgical interventions.
METHODS
Four hundred and eighty-seven patients, who were diagnosed with CTS and underwent surgical intervention between October 2016 and September 2007, were evaluated in this retrospective study. The age, gender, physical evaluation findings, electrophysiological examination reports and implemented surgical treatment methods were analyzed.
RESULTS
Thirty-nine of the cases were operated due to recurrent CTS. Further examination of the patients with recurrent CTS revealed that ten cases had diabetic polyneuropathy, three cases had hypothyroidism, two cases had rheumatoid arthritis and one case had systemic amyloidosis. Postoperative electromyography confirmed the neuropathy was due to systemic diseases. The remaining 23 patients with recurrent CTS did not have any systemic disease and all of them had applied previously to another health center.
CONCLUSION
We concluded that the recurrence rates in CTS might be decreased with exploration and incision of the entire transverse ligament. Damage to the motor and sensory branches of the median nerve could be avoided with an incision on the ulnar side.
Keywords: Carpal tunnel, Electromyography, Median nerve, Retrospective study, Entrapment neuropathies
Core tip: In this study, 23 cases of recurrent carpal tunnel syndrome did not have any systemic disease and all of them had undergone a surgical intervention in another center. The incision was made starting distal to the volar wrinkle, passed between the thenar and hypothenar region, 2-3 mm medially to the thenar wrinkle and extended 2-3 cm to the lateral side of the third finger. In recurrent cases, an appropriate differential diagnosis, re-operation without delay to avoid the development of the interfacial fibrosis, and implementation of a precise and careful surgical technique play important roles in improving the surgical outcome.
INTRODUCTION
Entrapment neuropathies are disorders of peripheral nerves characterized by pain, numbness or loss of function. The symptoms depend on the compression caused by the adjacent anatomical structures. Carpal tunnel syndrome (CTS) is the most common peripheral nerve entrapment neuropathy and CTS surgery is the most commonly performed operation in the hand region[1-4]. Surgical decompression was first performed by Amadio[5] in 1995 and by Learmonth[6] in 1933. A variety of surgical decompression techniques have been described over the years[7-9] (Table 1). The prevalence of CTS is 0.6%-3.4% in the general population[10,11]. It has a higher prevalence in certain occupational groups[12,13]. CTS is five times more common in women than men between the ages of 30-60 years and the involvement is usually bilateral[12]. An increase in pressure within the carpal tunnel is the major factor known in the etiology. The increased pressure impairs the blood supply of the median nerve and causes nerve damage[14].
Table 1.
Milestones of carpal tunnel syndrome decompression surgery
| References | Year | Accomplishment |
| Marie et al[38] | 1913 | Defined median nerve compression |
| Amadio[5] | 1924 | Median nerve decompression by transecting the transverse carpal ligament |
| Learmonth[6] | 1933 | Median nerve decompression by transecting the transverse carpal ligament |
| Cannon et al[39] | 1946 | Reported good results with the release of transverse carpal ligament with median nerve compression |
| Phalen et al[8] | 1950 | Started using standard open approach |
| Chow[26] | 1989 | Described dual portal endoscopic decompression technique |
| Agee et al[27] | 1992 | Single proximal portal endoscopic decompression technique |
| Biyani et al[40] | 1993 | Described mini-open double-incision technique |
| Bromley[41] | 1994 | Single distal mini-open technique |
A specific etiological factor may not be detected in the majority of patients with CTS. CTS is idiopathic in approximately 50% of the patients. Most patients are occupied in work requiring repetitive wrist motions[12,15,16]. Patients with congenital narrow carpal tunnel are more prone to CTS. Secondary causes include anatomical causes such as abnormalities in bone structure, traumatic structural disorders such as occupational recurrent microtrauma, and systemic diseases such as amyloidosis, diabetes, hypothyroidism, rheumatic diseases, and cancer[11,17]. The sense of prickling in the hand, radiating numbness in three fingers, and pain in the hand, wrist and medial side of the arm may emerge in early stages of the disease. Weakness and atrophy in the thenar muscles, loss of hand skills, and impairment in daily life activities are the major symptoms in advanced and chronic cases.
MATERIALS AND METHODS
Study objective
Four hundred and eighty-seven patients, who had undergone surgical intervention due to the diagnosis of CTS between September 2007 and October 2016, were evaluated retrospectively. The age, gender, physical evaluation findings, electrophysiological examination reports of the patients, and the implemented surgical treatment methods were recorded.
Inclusion and exclusion criteria
Of all cases, 448 (91.9%) had primary CTS and the remaining 39 (8.1%) cases had recurrent CTS. Twenty-three of the patients included in this study had recurrent CTS, complaints for at least 3 mo, no additional neural pathology, and persistent conduction disorders in sensory and motor fibers observed bv electromyography (EMG). Sixteen patients with recurrent CTS who had systemic diseases such as diabetes mellitus and thyroid disorders were excluded from the study.
Operative procedures
Hypoesthesia in the median nerve sensation area, loss of strength in the radial three fingers, thenar muscle atrophy, and Tinnel and Phalen signs were evaluated during the clinical examination. Preoperative wrist x-ray images were evaluated, and preoperative and postoperative (1st and 6th months) EMG images were examined for each patient. All patients were operated on by the same surgeon. Regarding the prophylaxis of the infection, a single dose of a parenteral antibiotic was administered before the intervention and continued with an oral antibiotic for the next 3 d. All patients were discharged on the same day. An elastic bandage was used for the first 24 h and the arm was positioned in a 90° flexion. Postoperative wrist splinting was not used. The next day after the operation, dressings were changed and finger exercises were started. Stitches were removed on the 10th day and exercises with a softball and hot water bath were initiated. The mean follow-up time was 8.6 mo (range: 7.2-13 mo).
Surgical technique
Open surgery with a standard incision, open surgery with a mini-incision, or closed surgery such as endoscopic surgery and retinaculotomy may be used in CTS. We preferred a 2-3 cm mini-incision so that the entire transverse ligament could be visualized (Figure 1).
Figure 1.

Mini open incision method. A: Local anesthetic application to the incision line; B: The standard incision starts from the distal volar wrinkle, passes between the thenar and hypothenar region 2-3 mm medially to thenar wrinkle and extends 2-3 cm distally to the lateral side of the third finger; C: Placement of the skin retractor after sharp dissection.
Open surgery with a mini-incision was performed under local anesthesia without a tourniquet (Figure 1A). The patients were positioned supine on the operating table. The arm was placed on the surgical table slightly elevated and a small silicone pad was placed under the wrist, while the arm was in 90° abduction. Our standard incision starts distal to the volar wrinkle, passes between the thenar and hypothenar region, 2-3 mm medial to the thenar wrinkle and extends 2-3 cm distally to the lateral side of the third finger (Figure 1B). Regarding the patients with recurrent CTS, we preferred an open surgery with a 1-1.5 cm mini-incision over the previous long incision scar in patients who had previously undergone open surgery. A similar incision was done just at the distal side of the previous incision scar in patients who had a transverse incision over the volar wrinkle, and a similar incision was done again between the previous incision lines in patients who had previously undergone endoscopic surgery (Figure 1C). Following the local anesthetic infiltration into the incision line, a vertical skin and subcutaneous incision was carried out. The skin and subcutaneous tissues were sharply incised with a No 15 blade and a skin retractor was inserted. The sharp dissection was deepened. After passing through the subcutaneous fat and the granulation tissue, the palmar aponeurosis and transverse ligament were exposed. The skin retractor was re-positioned and the transverse ligament was fully visualized. The ligament was completely and cautiously incised on the ulnar side of the median nerve with a No. 15 scalpel. Subsequently, a dissector was used to check whether the decompression was sufficient or not on the proximal and distal sides (Figure 2). Hemostasis was achieved by compressing the palm for a few minutes. The skin was sutured with 4/0 vicryl and the wound was closed with a sterile dressing. The strength of abductor pollicis brevis and other flexor muscles and sensation in the thenar region was controlled at the end-stage of the operation.
Figure 2.

Extended mini-open incision technique in a patient previously operated on using the uniprotal endoscopic method. A: Endoscopic portal scar over the distal wrist wrinkle (red arrow); B: Incomplete incision of the transverse carpal ligament and compression on the median nerve (black arrow); C: The incision is completed and the median nerve is fully decompressed.
Statistical analysis
Due to small sub-group numbers and no subjects for comparison, statistical analysis was not carried out.
RESULTS
Patient demographics and characteristics
Regarding the patients with recurrent CTS cases (n = 23), 15 were females (65.2%) and eight were males (34.8%). The mean age was 46.5 years (range: 21-69 years). In 12 (52.1%) of these cases the left hand was affected, and in 11 (47.9%) cases the right hand was affected. The closed technique was previously performed in ten (43.4%) of the patients with recurrent CTS (uniprotal endoscopic technique (n = 4), biportal endoscopic (n = 4) and retinaculotomy technique (n = 2) were used). Regarding the previous interventions, open surgery was used in six (26.1%) cases with recurrent CTS, and transverse mini-incision was used in seven (30.4%) cases with recurrent CTS (Figure 3).
Figure 3.
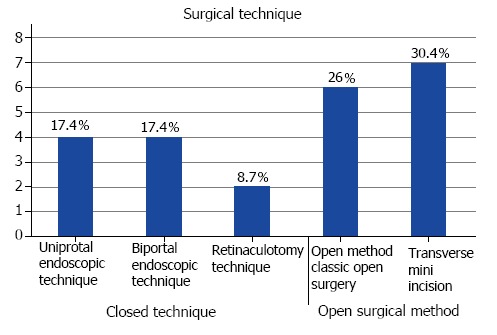
Ten (43.4%) recurrent cases were previously operated with closed technique (uniprotal endoscopic technique in four, biportal endoscopic technique in four and retinaculotomy technique in two cases). Six (26%) recurrent cases were previously operated with open surgical method and seven (30.4%) recurrent cases were previously operated with transverse mini incision.
Preoperative examination findings
Following the first operation, all patients continued to have one or more complaints, which included nocturnal pain, sensory loss, and pain increasing with activity over the median nerve distribution area. The patients with recurrent symptoms stated that they still had the same complaints they had in the preoperative period for an average of 3.2 mo (1-7 mo) after the previous surgery. The clinical findings of the physical examination were the following: sensory impairment in 16 cases (69.5%), nocturnal pain (awoken from sleep) in 18 cases (78.2%), and loss of hand strength in 13 cases (56.5%). Tinel sign and Phalen test sign were positive in 16 (69.5%) and in 13 (56.5%) cases, respectively. The thenar atrophy was detected in 14 (60.8%) cases (Figure 4).
Figure 4.
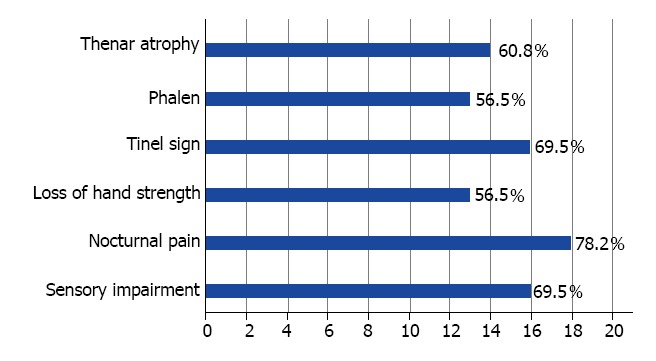
Thenar atrophy in 14 (60.8%) cases. Phalen test was positive in 13 (56.5%) cases. Tinel sign was found in 16 (69.5%) cases. Loss of hand strength in 13 (56.5%) cases, nocturnal pain in 18 (78.2%) cases and sensory impairment was detected in 16 (69.5%) cases.
Preoperative EMG findings
Preoperative EMG examinations of patients with recurrent CTS revealed low amplitudes of action potentials (severe) (n = 4), conduction disorders (moderate) both in sensory and motor fibers (n = 13), and conduction disorders affecting only the sensory fibers (n = 6). Two cases of severe EMG changes had denervation potentials in the thenar muscles and severe damage to the median nerve.
Surgical results
Patients were operated on using the open mini-incision technique. The mean duration of the operation was 12 min (range: 10-15 min). None of the cases had any additional complications concerning the motor and sensory branch of the median nerve. Wound infection emerged in two cases and a hematoma in one case. The one patient who developed a hematoma was immediately re-operated on and the hematoma was excised. Two patients with wound site infection were treated with oral antibiotics. The mean duration of return to daily living was 21 d (range: 16-27 d).
Postoperative EMG findings
The EMG examination performed in the 6th month after the operation showed irreversible axonal damage to the median nerve in two patients (these patients had findings of denervation in the thenar muscles in the preoperative EMG examination). Improved latency in motor and sensory fibers of the median nerve was reported in all other cases.
DISCUSSION
Conservative methods should be primarily considered in the treatment of CTS, but surgical treatment should be preferred in cases where patients are not responding to conservative treatments[16,18,19]. The goal of the surgical treatment is to release transverse carpal ligament (TCL) completely and to decompress the canal. Decompression of the median nerve with complete dissection of the TCL leads to a clinical improvement in the vast majority of patients[16,19-21]. Several surgical methods have been described in CTS surgery, including open and closed techniques. Although there is no significant difference between these surgical methods in respect to clinical and electrophysiological outcome, recurrence may be encountered due to the incomplete or insufficient release of the transverse ligament[19,21,22].
Carpal tunnel decompression surgery using open technique, which was first performed by Amadio[5] in 1995 and later described by Learmont[6] in 1933, is still preferred[23-25]. Although it has been reported that this technique provides satisfying results, there are also certain disadvantages such as pain at the incision site, sensitivity to the scar tissue, and delayed return to daily activities and work[16]. Thus, alternative methods have been developed to avoid postoperative morbidity after open surgery[1]. Chow[26] and Agee et al[27] reported that with the widespread use of endoscopic methods, new developments in endoscopic instruments and more experienced surgeons, the postoperative morbidity is decreased, the time until return to work after the surgery is shortened, and the scars are more cosmetic and painless. However, endoscopic techniques may also lead to high complication rates when performed without adequate knowledge of endoscopic anatomy and experience[15,18,28].
An evaluation of the entire carpal tunnel may not be possible during endoscopic surgery and cutting the transverse ligament without adequate visualization may increase the risk of median nerve injury[28]. Lee reported that the median nerve was injured in two cases in their series[29]. It is also possible that space-occupying lesions may be overlooked during endoscopic surgery. Endoscopic surgery also requires a high level of surgical experience and special instrumentation, and cannot be implemented in cases of neurolysis or tenosynovectomy[30].
With the open mini-incision technique, the entire transverse ligament can be visualized and the median nerve and canal may be fully investigated. All 23 patients with recurrent CTS who were included in our study had been previously operated with different surgical techniques in different centers. We observed in all of these patients that the release of the transverse ligament was incomplete and the median nerve was still under compression. We resolved the inadequate decompression with a complete incision of the ligament (Figure 2). All cases stated that their nocturnal pain, which was awakening them from sleep, was relieved on the first day after the operation. The carpal tunnel decompression with open surgery is considered as the gold standard in the treatment of CTS[1,18,21]. Although successful results have generally been reported with this method, certain disadvantages may also be encountered, such as weakness in the hand, sensitivity to the scar tissue, and delayed return to daily activities and work[1,31]. Various complications including injury to the palmar cutaneous branch (PCB) of the median nerve, hypertrophic incision scarring, reflex sympathetic dystrophy, and increased tension in flexor tendons have also been reported after open surgery[1]. In our cases, we did not encounter these aforementioned complications, with the exception of wound infection and hematoma.
PCB arises from the median nerve before the TCL. This branch provides the sensitive innervation of the thenar region of the hand and plays a major role in the planning of surgical incisions for carpal tunnel surgery. According to some authors, this sensory branch extends to the ulnar side[10]. For this reason, Franzini et al[32] preferred a 1 cm longitudinal incision proximal to the wrist flexor line. Abdullah et al[22] reported that PCB was arising from the radial side of the median nerve and is always located lateral to the palmaris longus (PL) tendon, so they were using a transverse incision at the medial side of the PL tendon. In our cases, we used a mini-incision starting from the distal side of the wrist flexor line and extending 2-3 mm to the medial side of the thenar line. We exposed the entire transverse ligament, identified PCB, and incised the transverse ligament on the medial side of the median nerve.
Regarding recurrence after CTS surgery, the most common reason is the incomplete release of the distal part of the TCL[21]. A 2-3 cm open mini-incision enables the visualization of the distal part of the ligament. However, in patients with recurrent CTS in this study, we extended the mini-incision about 1-1.5 cm due to fibrotic scar tissue formation. The median nerve is divided into two main trunks (lateral and medial) at the distal end of the TCL. The branch, which provides motor innervation, originates from the lateral trunk. Several anatomic variations of this motor branch should be taken into consideration during the planning of the surgical incision[10]. According to the Lanz classification, variations of the motor branch include extra-ligamentous, subligamentous, and less commonly transligamentous localizations[33]. This branch rarely originates from the ulnar side of the median nerve and rarely gives recurrent motor branches[33]. We believe that the implementation of the closed techniques (e.g., endoscopic methods) and the dissection of the transverse ligament without fully visualizing the median nerve may cause iatrogenic neural injuries, depending on the anatomic variations of the median nerve. In addition, recurrence may also be encountered in the closed techniques due to the incomplete dissection of TCL and the inadequate decompression of the median nerve.
We used an open mini-incision technique in our cases and carried out a small incision to release the median nerve and cut the TCL, volar carpal ligament and deep palmar fascia. Shapiro[34] reported good results in 96% of patients with a technique named “carpal tunnel release with microsurgery”, which is performed by a mini-incision using special instruments (microscope and Easyloupe). Decompression of the transligamentous motor branch with this incision is also possible. However, the most common disadvantage of this incision is a large scar and loss of hand function[22]. One of the most frequently discussed issues is “should the incision be longitudinal or transverse?”[35]. The authors, who prefer a longitudinal incision, suggest that PCB injuries may be avoided with this incision. However, according to the experience gained from the anatomic studies, PCB rarely extends to the medial side of the PL tendon[10]. Therefore, PCB can be preserved by an incision that does not extend to the lateral side of the PL tendon[35]. In our cases, we incised the transverse ligament from the ulnar side of the median nerve.
The average time to return to daily activities was longer after the open surgical method compared to the endoscopic and open mini-incision surgical methods[30]. This duration was 14-17 d after the closed technique and 28 d after the open surgery technique[24]. In our cases, the average time to return to the daily activities was 17 d (14-21 d). The comparison of the outcome in both groups does not show any significant difference between open and closed surgical methods. However, 10-15% of patients who had undergone endoscopic surgery encountered an inadequate relief in symptoms or an early onset of recurrence[25]. Median, ulnar and digital nerve injuries have been reported in the literature for both open and closed technique[36]. In our cases, no additional neural damage was observed. In addition to the relatively simpler technique and it being easier to learn, the lower cost of the surgical instruments used in open mini-incision surgery is another advantage in comparison to the endoscopic and retinaculotomy techniques[37] Surgical experience, special instruments and appropriate assistance are required for the endoscopic surgery and retinaculotomy methods. One of the major disadvantages of the closed technique is the increased injury risk of the ulnar-radial artery arch[26]. Other advantages of the open mini-incision surgical incision technique, which we used in our study, include the easy access to the proximal and the distal end of the TCL, prevention of the damage to the superficial palmar arch, and preservation of the motor branch, which innervates the m. abductor pollicis brevis.
Our patients stated that nocturnal paresthesia was immediately relieved the day after CTS surgery. If the pain is not immediately relieved after the surgery, an incomplete incision of TCL should be considered[10]. We believe that the preference for an open surgical technique with complete incision of the carpal transverse ligament will enable a complete decompression of the median nerve and, consequently, a significant reduction in the recurrence and neuronal injury rates. In patients with recurrent CTS, an appropriate differential diagnosis, re-operation without delay to avoid the development of interfacial fibrosis, implementation of a precise and careful surgical technique, and initiation of an appropriate exercise program in the postoperative period are the factors contributing to the improvement of surgical outcome.
ARTICLE HIGHLIGHTS
Research background
The reasons for recurring carpal tunnel have been researched since the 1990s. Studies have investigated fibrosis and surgical techniques. This study, however, demonstrates that the median nerve should be relieved by full incision of the transverse ligament.
Research motivation
In carpal tunnel surgery, the recurrence rate was increased following the widespread use of the endoscopic and minimally-invasive techniques. A satisfying surgical outcome cannot be achieved if the compression caused by the transverse ligament cannot be completely relieved. The development of the endoscopic and minimally-invasive techniques and the proper training of relevant surgeons will decrease recurrence rates. The critical step in carpal tunnel syndrome surgery is the complete incision of the transverse ligament on the median nerve and the relief of the compression. Independent of the selected surgical technique, the complete incision of the transverse ligament should be ensured.
Research objectives
The main aim of the study is to perform carpal tunnel surgery with the appropriate surgical method without the need for a second operation. Re-operation on patients with recurrence prolongs the hospitalization time with consequential economic loss. Careful and appropriate surgery will prevent this. Appropriate surgical methods will also prevent surgeons from encountering medicolegal problems. Complete incision of the transverse ligament will reduce recurrence rates following carpal tunnel surgery.
Research methods
Four hundred and eighty-seven patients were evaluated retrospectively. The age, gender, physical evaluation findings, electrophysiological examination reports of the patients, and the implemented surgical treatment methods were recorded in this research.
Research results
Fibrosis and surgical methods have been criticized in the literature. However, this manuscript emphasizes the importance of removing ligament integrity completely. If the complete incision of the transverse ligament is not ensured with endoscopic and minimally-invasive methods, an open surgery technique must be implemented.
Research conclusions
Relief of the median nerve in carpal tunnel surgery occurs when the transverse ligament is completely incised. Recurrence rates therein decrease. Regardless of the surgical procedure, it should be ensured that the transverse ligament is completely incised. If minimally-invasive methods are insufficient in nerve decompression, open surgery should be performed.
Research perspectives
Complete incision of the transverse ligament will reduce recurrence rates following carpal tunnel surgery. This study demonstrates that the median nerve should be relieved by full incision of the transverse ligament. This manuscript emphasizes the importance of completely removing ligament integrity. A satisfying surgical outcome cannot be achieved if the compression caused by the transverse ligament cannot be completely relieved. The relief of the median nerve in carpal tunnel surgery occurs when the transverse ligament is completely incised. Recurrence rates therein decrease. If minimally-invasive methods are insufficient in nerve decompression, open surgery should be performed.
Footnotes
Institutional review board statement: The manuscript has been approved by Ministry of Health Haydarpaşa Sultan Abdülhamid Education and Research Hospital, Review Board of Neurosurgery.
Informed consent statement: It has been declared that all relevant persons involved (subjects or legally authorized representative) gave their informed consent (written or verbal, as appropriate).
Conflict-of-interest statement: All authors have no conflicts of interest to report.
Manuscript source: Unsolicited manuscript
Peer-review started: April 8, 2018
First decision: May 16, 2018
Article in press: August 11, 2018
Specialty type: Medicine, research and experimental
Country of origin: Turkey
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Sergi CM, Vento S S- Editor: Ma YJ L- Editor: Filipodia E- Editor: Wu YXJ
Contributor Information
Ahmet Eroğlu, Department of Neurosurgery, Haydarpaşa Sultan Abdülhamid Education and Research Hospital, Istanbul 34000, Turkey. drahmeteroglu@gmail.com.
Enes Sarı, Department of Orthopaedics and Traumatology, Near East University Hospital, Lefkoşa 99010, Cyprus.
Ali Kıvanç Topuz, Department of Neurosurgery, Baypark Hospital, Istanbul 34000, Turkey.
Hakan Şimşek, Department of Neurosurgery, Haydarpaşa Sultan Abdülhamid Education and Research Hospital, Istanbul 34000, Turkey.
Serhat Pusat, Department of Neurosurgery, Haydarpaşa Sultan Abdülhamid Education and Research Hospital, Istanbul 34000, Turkey.
References
- 1.Jimenez DF, Gibbs SR, Clapper AT. Endoscopic treatment of carpal tunnel syndrome: a critical review. J Neurosurg. 1998;88:817–826. doi: 10.3171/jns.1998.88.5.0817. [DOI] [PubMed] [Google Scholar]
- 2.Paget J. Lectures on Surgical Pathology. Lindsay and Blakiston, 3rd ed. Philadelphia 1854: 173-179 [Google Scholar]
- 3.Tulipan JE, Kim N, Abboudi J, Jones C, Liss F, Kirkpatrick W, Rivlin M, Wang ML, Matzon J, Ilyas AM. Open Carpal Tunnel Release Outcomes: Performed Wide Awake versus with Sedation. J Hand Microsurg. 2017;9:74–79. doi: 10.1055/s-0037-1603200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nazari G, Shah N, MacDermid JC, Woodhouse L. The Impact of Sensory, Motor and Pain Impairments on Patient- Reported and Performance Based Function in Carpal Tunnel Syndrome. Open Orthop J. 2017;11:1258–1267. doi: 10.2174/1874325001711011258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Amadio PC. The first carpal tunnel release? J Hand Surg Br. 1995;20:40–41. doi: 10.1016/s0266-7681(05)80013-0. [DOI] [PubMed] [Google Scholar]
- 6.Learmonth J. The princible of decompression in treatment of certain diseases of peripheral nerves. Surg Clin North Am. 1933;13:905–913. [Google Scholar]
- 7.Love JG. Median neuritis or carpal tunnel syndrome; diagnosis and treatment. N C Med J. 1955;16:463–469. [PubMed] [Google Scholar]
- 8.Phalen GS, Gardner WJ, La Londe AA. Neuropathy of the median nerve due to compression beneath the transverse carpal ligament. J Bone Joint Surg Am. 1950;32A:109–112. [PubMed] [Google Scholar]
- 9.Mirza MA, King ET Jr. Newer techniques of carpal tunnel release. Orthop Clin North Am. 1996;27:355–371. [PubMed] [Google Scholar]
- 10.Serarslan Y, Melek İ, Duman T. Karpal Tunel Sendromu. Pamukkale Tıp Dergisi. 2008;1:45–49. [Google Scholar]
- 11.Kürklü M, Türkkan S, Tüzün HY. Karpal tünel Sendromu ve Median Sinirin Diğer Tuzak Nöropatileri. TOTBİD Dergisi. 2015;14:566–571. [Google Scholar]
- 12.Papanicolaou GD, McCabe SJ, Firrell J. The prevalence and characteristics of nerve compression symptoms in the general population. J Hand Surg Am. 2001;26:460–466. doi: 10.1053/jhsu.2001.24972. [DOI] [PubMed] [Google Scholar]
- 13.Stevens JC, Beard CM, O’Fallon WM, Kurland LT. Conditions associated with carpal tunnel syndrome. Mayo Clin Proc. 1992;67:541–548. doi: 10.1016/s0025-6196(12)60461-3. [DOI] [PubMed] [Google Scholar]
- 14.Bland JD. Carpal tunnel syndrome. Curr Opin Neurol. 2005;18:581–585. doi: 10.1097/01.wco.0000173142.58068.5a. [DOI] [PubMed] [Google Scholar]
- 15.Urbaniak JR, Desai SS. Complications of nonoperative and operative treatment of carpal tunnel syndrome. Hand Clin. 1996;12:325–335. [PubMed] [Google Scholar]
- 16.Şavk O, Turgut M, Çullu E, Akyol A, Alparslan B. Karpal Tünel Sendromunun cerrahi dekompresyonunda standart ve mini insizyon tekniklerinin karşılaştırılması. ADÜ Tıp Fakültesi Dergisi. 2002;3:9–13. [Google Scholar]
- 17.Kıbıcı K, Köksal V. Mini Açk Teknikle Yapılan Karpal Tünel Cerrahisi ve Fonksiyonel Sonuçları. Türk Nöroşirürji Dergisi. 2010;20:7–14. [Google Scholar]
- 18.Zamborsky R, Kokavec M, Simko L, Bohac M. Carpal Tunnel Syndrome: Symptoms, Causes and Treatment Options. Literature Reviev. Ortop Traumatol Rehabil. 2017;19:1–8. doi: 10.5604/15093492.1232629. [DOI] [PubMed] [Google Scholar]
- 19.Vázquez-Alonso MF, Abdala-Dergal C. [Principal causes for recurrent carpal tunnel syndrome] Acta Ortop Mex. 2016;30:17–20. [PubMed] [Google Scholar]
- 20.Szabo RM, Steinberg DR. Nerve Entrapment Syndromes in the Wrist. J Am Acad Orthop Surg. 1994;2:115–123. doi: 10.5435/00124635-199403000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Dahlin LB, Salö M, Thomsen N, Stütz N. Carpal tunnel syndrome and treatment of recurrent symptoms. Scand J Plast Reconstr Surg Hand Surg. 2010;44:4–11. doi: 10.3109/02844310903528697. [DOI] [PubMed] [Google Scholar]
- 22.Abdullah AF, Wolber PH, Ditto EW 3rd. Sequelae of carpal tunnel surgery: rationale for the design of a surgical approach. Neurosurgery. 1995;37:931–935; discussion 935-936. doi: 10.1227/00006123-199511000-00012. [DOI] [PubMed] [Google Scholar]
- 23.Cellocco P, Rossi C, El Boustany S, Di Tanna GL, Costanzo G. Minimally invasive carpal tunnel release. Orthop Clin North Am. 2009;40:441–448, vii. doi: 10.1016/j.ocl.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 24.Atroshi I, Johnsson R, Ornstein E. Endoscopic carpal tunnel release: prospective assessment of 255 consecutive cases. J Hand Surg Br. 1997;22:42–47. doi: 10.1016/s0266-7681(97)80013-7. [DOI] [PubMed] [Google Scholar]
- 25.Hulsizer DL, Staebler MP, Weiss AP, Akelman E. The results of revision carpal tunnel release following previous open versus endoscopic surgery. J Hand Surg Am. 1998;23:865–869. doi: 10.1016/S0363-5023(98)80164-0. [DOI] [PubMed] [Google Scholar]
- 26.Chow JC. Endoscopic release of the carpal ligament: a new technique for carpal tunnel syndrome. Arthroscopy. 1989;5:19–24. doi: 10.1016/0749-8063(89)90085-6. [DOI] [PubMed] [Google Scholar]
- 27.Agee JM, McCarroll HR Jr, Tortosa RD, Berry DA, Szabo RM, Peimer CA. Endoscopic release of the carpal tunnel: a randomized prospective multicenter study. J Hand Surg Am. 1992;17:987–995. doi: 10.1016/s0363-5023(09)91044-9. [DOI] [PubMed] [Google Scholar]
- 28.Chen AC, Wu MH, Cheng CY, Chan YS. Outcomes and Satisfaction with Endoscopic Carpal Tunnel Releases and the Predictors - A Retrospective Cohort Study. Open Orthop J. 2016;10:757–764. doi: 10.2174/1874325001610010757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee WP, Strickland JW. Safe carpal tunnel release via a limited palmar incision. Plast Reconstr Surg. 1998;101:418–424; discussion 425-426. doi: 10.1097/00006534-199802000-00025. [DOI] [PubMed] [Google Scholar]
- 30.Atroshi I, Johnsson R, Ornstein E. Patient satisfaction and return to work after endoscopic carpal tunnel surgery. J Hand Surg Am. 1998;23:58–65. doi: 10.1016/S0363-5023(98)80090-7. [DOI] [PubMed] [Google Scholar]
- 31.Bradley MP, Hayes EP, Weiss AP, Akelman E. A prospective study of outcome following mini-open carpal tunnel release. Hand Surg. 2003;8:59–63. doi: 10.1142/s0218810403001522. [DOI] [PubMed] [Google Scholar]
- 32.Franzini A, Broggi G, Servello D, Dones I, Pluchino MG. Transillumination in minimally invasive surgery for carpal tunnel release. Technical note. J Neurosurg. 1996;85:1184–1186. doi: 10.3171/jns.1996.85.6.1184. [DOI] [PubMed] [Google Scholar]
- 33.Lanz U. Anatomical variations of the median nerve in the carpal tunnel. J Hand Surg Am. 1977;2:44–53. doi: 10.1016/s0363-5023(77)80009-9. [DOI] [PubMed] [Google Scholar]
- 34.Shapiro S. Microsurgical carpal tunnel release. Neurosurgery. 1995;37:66–70. doi: 10.1227/00006123-199507000-00010. [DOI] [PubMed] [Google Scholar]
- 35.Kulick RG. Carpal tunnel syndrome. Orthop Clin North Am. 1996;27:345–354. [PubMed] [Google Scholar]
- 36.Bozentka DJ, Osterman AL. Complications of endoscopic carpal tunnel release. Hand Clin. 1995;11:91–95. [PubMed] [Google Scholar]
- 37.Lee H, Jackson TA. Carpal tunnel release through a limited skin incision under direct visualization using a new instrument, the carposcope. Plast Reconstr Surg. 1996;98:313–319; discussion 320. doi: 10.1097/00006534-199608000-00016. [DOI] [PubMed] [Google Scholar]
- 38.Marie P, Foix C. Atrophie isolée de l’éminence thenar d’origine névritique: rôle du ligament annulaire antérieur du carpe dans la pathogénie de la lesion. Rev Neurol. 1913;26:647–649. [Google Scholar]
- 39.Cannon BW, Love JG. Tardy median palsy; median neuritis; median thenar neuritis amenable to surgery. Surgery. 1946;20:210–216. [PubMed] [Google Scholar]
- 40.Biyani A, Downes EM. An open twin incision technique of carpal tunnel decompression with reduced incidence of scar tenderness. J Hand Surg Br. 1993;18:331–334. doi: 10.1016/0266-7681(93)90055-k. [DOI] [PubMed] [Google Scholar]
- 41.Bromley GS. Minimal-incision open carpal tunnel decompression. J Hand Surg Am. 1994;19:119–120. doi: 10.1016/0363-5023(94)90234-8. [DOI] [PubMed] [Google Scholar]


