Abstract
Mechanical forces in blood circulation such as shear stress play a predominant role in many physiological and pathophysiological processes related to vascular responses or vessel remodeling. Arteriogenesis, defined as the growth of pre-existing arterioles into functional collateral arteries compensating for stenosed or occluded arteries, is such a process. Midkine, a pleiotropic protein and growth factor, has originally been identified to orchestrate embryonic development. In the adult organism its expression is restricted to distinct tissues (including tumors), whereby midkine is strongly expressed in inflamed tissue and has been shown to promote inflammation. Recent investigations conferred midkine an important function in vascular remodeling and growth. In this review, we introduce the midkine gene and protein along with its cognate receptors, and highlight its role in inflammation and the vascular system with special emphasis on arteriogenesis, particularly focusing on shear stress-mediated vascular cell proliferation and vasodilatation.
Keywords: midkine, nitric oxide synthases, VEGF, endothelial-cell proliferation, vasodilation, arteriogenesis, hypoxia, shear stress, reactive oxygen species, tumor
1. Introduction
After the discovery of the cytokine midkine (MK) in 1988, its main function was believed to orchestrate embryonic development [1]. However, multiple studies during the last three decades clearly indicated a functional impact of MK on the adult organism as well. By far, most of the studies on MK addressed its role in malignant diseases and suggested a detrimental effect for the host [2,3,4,5]. A significant part of the literature on MK has shown its ability to promote inflammatory responses. Different mechanisms of how MK could reinforce acute or chronic inflammation have been proposed as well and will be partially reviewed here [6]. In addition, recent studies demonstrated that MK serves as a major regulator of angiogenesis and arteriogenesis during pathological conditions in the vascular system. In light of the fast-growing burden of cardiovascular diseases, which are predominantly associated with atherosclerosis and occlusive arterial disease, e.g., in the heart, interventional strategies to modulate arteriogenesis, i.e., the growth of pre-existing arteriolar connections bypassing an occluded artery, may become novel noninvasive treatment modalities for patients with ischemia-related pathologies. In this review, we will summarize the recent findings on the functional impact of MK on the vascular system with a special focus on arteriogenesis and vascular remodeling.
2. Midkine
2.1. MK Gene and Protein
In 1988 Kadomatsu and colleagues discovered MK in retinoic acid-differentiated mouse embryonic carcinoma cells, an experimental model to study the early steps of embryogenesis [1]. Expression of MK was upregulated exclusively during the midgestation period in mouse embryogenesis [7]. This fact, together with a predominant expression of MK in the kidneys of adult organisms, finally led to the name mid-kine (mid-gestation, ki-dney) [6,7]. The mouse MK gene is located on chromosome 2, while the human gene, consisting of four coding exons with seven mRNA isoforms [8], was identified on chromosome 11 [9,10]. Among a retinoic acid response element and a binding site for the product of the Wilms tumor-suppressor gene WT-1, a hypoxia-responsive element has been identified in the promoter region of the MK gene [11,12,13].
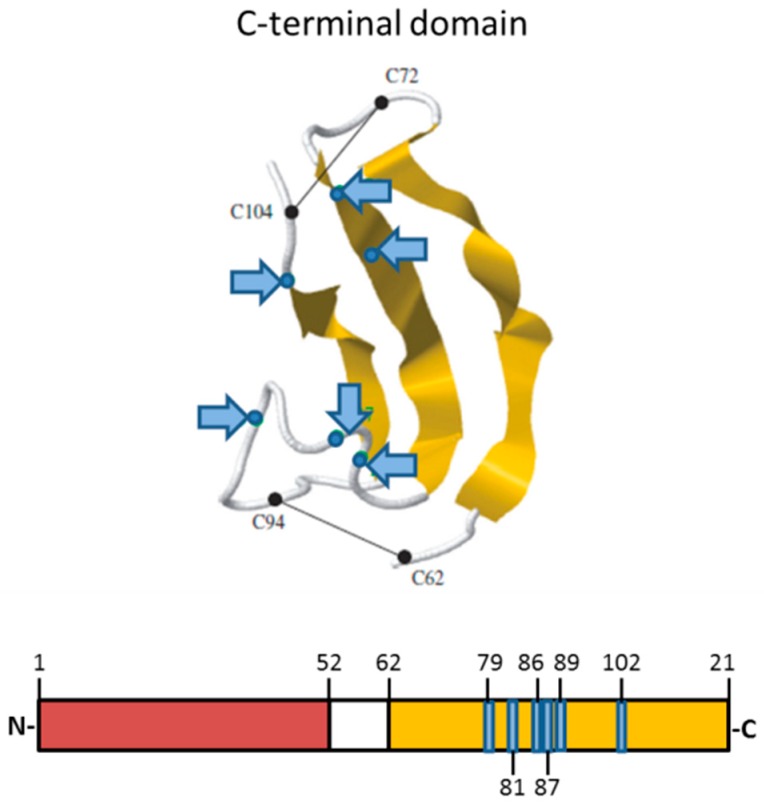
The human MK protein—composed of 121 amino acids—is a heparin-binding growth factor with a molecular weight of 13 kDa consisting of two similar domains, an N-terminal (amino acids 1–52) and a C-terminal domain (amino acids 62–121), which are connected by a hinge domain (amino acids 53–61) [14]. Each domain contains three antiparallel β-strands [14]. Ten cysteine residues, which are highly conserved among different species, form five disulfide bonds (two bonds in the C-terminal domain and three bonds in the N-terminal domain), building the structure of the domains [14]. MK is a positively charged protein containing two heparin-binding clusters with a number of arginine and lysine residues (cluster 1: K79, R81, K102; cluster 2: K86, K87, R89), located in the C-terminal domain (Figure 1) [6,14]. MK may interact via its positively charged heparin-binding sites with heparin-like glycosaminoglycans of endothelial cells, enabling MK to be immobilized on the luminal site of the vessel wall [15,16].
Figure 1.
Protein structure of midkine (MK). The protein consists of an N-terminal domain (red) and a C-terminal domain (yellow), which are connected by a hinge region (white). The heparin-binding domains, which consist of basic amino acids, are located in the C-terminal domain (labeled in blue, blue arrows). Adapted from Weckbach et al., 2011 [6], with the permission of the authors.
MK together with pleiotrophin (PTN) forms its own so-called MK family [17], which is structurally not related to any other protein family. Both proteins show a 50% sequence identity and complete conservation of positions of all cysteine residues [18]. The heparin-binding sites are also conserved in MK and PTN with only one basic amino acid exchanged (K84 in MK, R84 in PTN) [19]. A phylogenetic analysis showed a high conservation of the MK protein among different species with an amino acid sequence identity between human and murine MK of 87% [20]. In zebrafish, a very popular and established experimental animal model organism for a variety of human diseases, two MK molecules, midkine-a and midkine-b, have been discovered and most likely represent gene duplicates [21]. Drosophila melanogaster expresses two proteins sharing similarities with MK and PTN, named miple-1 and miple-2. Both proteins predominantly resemble the C-terminal domain of MK [22].
2.2. MK Receptors
For MK, a wide variety of receptors have been identified (Table 1), which are believed to function as receptor complexes [6]. In general, MK receptors, co-receptors and additional components assemble to form a specific functional receptor complex to promote particular functions of MK. There is evidence that MK signaling via the receptor-like protein tyrosine phosphatase β/protein tyrosine phosphatase ζ (PTPζ) involves phosphatidylinositol 3-kinase (PI3K), mitogen-activated protein kinase (MAPK), Src family kinases, and protein kinase C as downstream-signaling partners of MK [23,24]. PI3K and MAPK signal transduction was also observed upon MK binding to anaplastic lymphoma kinase (ALK), suggesting a common signaling pathway for at least some MK receptors [25]. Furthermore, members of the low-density lipoprotein (LDL) family, including the LDL-receptor-related protein-1 (LRP-1), megalin/brushin, LRP-6, or apoE receptor-2 have been shown to act as MK receptors [26]. MK binding to LRP-1 led to a conformational change of β2 integrins [27], a prerequisite for neutrophil adhesion during acute inflammation, as detailed below. Although MK did not directly bind to β1 integrins on neutrophils [27], MK mediates migration of UMR-106 osteoblast-like cells via α4β1 integrins and neurite outgrowth of embryonic neurons via α4β1 integrins, respectively [28]. MK has been shown to bind with high affinity to different glycosaminoglycans including heparan sulfate-trisulfated units and chondroitin sulfate E [29]. In addition, members of the heparan sulfate proteoglycan families of syndecans and glypicans serve as cellular-binding components for MK during neuronal development [30,31,32]. The binding of MK to Notch2 resulted in the upregulation of nuclear factor kappa-light-chain-enhancer of activated B cells (NFκB), implying that MK is involved in inflammatory reactions [33] by, e.g., upregulating the expression of intercellular adhesion molecule-1 (ICAM-1) [34]. Whether the altered combination of components in receptor complexes leads to the modification of MK-dependent signaling in cells remains to be investigated. Moreover, further receptors of MK might be identified in the future.
Table 1.
Midkine receptors.
| Receptor Family | Receptor | Reference |
|---|---|---|
| Protein tyrosine phosphatase (PTP) | PTPζ | Maeda et al., 1999 [23] |
| Qi et al., 2001 [24] | ||
| LDL-receptor-related protein (LRP) | LRP-1 | Muramatsu et al., 2000 [26] |
| megalin/brushin | Muramatsu et al., 2000 [26] | |
| LRP-6 | Muramatsu et al., 2004 [28] | |
| apoE receptor-2 | Muramatsu et al., 2000 [26] | |
| Integrins | α4β1 | Muramatsu et al., 2004 [28] |
| α6β1 | Muramatsu et al., 2004 [28] | |
| Notch | notch2 | Huang et al., 2008 [35] |
| Receptor tyrosine kinase | ALK | Stoica et al., 2007 [25] |
| Glycosaminoglycans | Heparan sulfate trisulfated units | Ueoka et al., 2000 [29] |
| Chondroitin sulfate E units | Ueoka et al., 2000 [29] | |
| Syndecan-1 | Nakanishi et al., 1997 [32] | |
| Syndecan-3 | Nakanishi et al., 1997 [32] | |
| Glypican-2 | Kurosawa et al., 2001 [31] |
Table adapted from Weckbach et al. [6].
2.3. Sources of MK and Levels of the Protein in the Vascular System
MK is present in the serum and plasma of healthy subjects and levels may become elevated in patients [36]. Yet, the cellular source of MK in the vascular system has not been fully elucidated. Elevated MK serum levels are found in patients with different tumor entities and have been shown to correlate with poor prognosis and recurrence after tumor removal [2,3,4]. The tumor cells may be the source of MK in this case, as malignant tissue often shows high MK expression [5]. The low plasma levels of MK in healthy subjects are rapidly elevated upon administration of heparin. These high post-heparin plasma levels of MK are an indication for the storage of MK in or its association with vascular cells via heparan sulfate proteoglycans [16]. This feature of MK is shared by other heparin-releasable proteins, such as chemokines, antithrombin, or lipoprotein lipase, which bind via their heparin-binding sites to the luminal phase of the endothelium [16]. After administration, heparin in the circulation may compete for these solid-phase heparin-binding sites on the vessel wall and result in protein mobilization.
Although it is not established which cells provide the source of MK in the vascular system in vivo, endothelial cells are able to synthesize MK under resting conditions in vitro [16]. Moreover, the release of MK into the cell supernatants was elevated under hypoxic conditions in vitro [37]. Immune cells may also represent a vascular source of MK, whereby increased MK expression was detected in isolated human neutrophils and monocytes upon hypoxia. Although earlier studies in the adult murine system suggested a restricted expression of MK to the kidney [7], MK was also detected in the plasma of an anephric patient and elevated in the circulation after heparin administration, indicating that the kidney does not represent the sole source of circulating MK [16]. The exact location and regulation of MK expression in the vascular system still needs to be studied.
2.4. MK in Inflammation
Due to the distinct expression pattern of MK during embryonic development, MK was initially believed to predominantly regulate embryogenetic processes. However, the role of MK in situations of acute and chronic inflammation has been increasingly acknowledged.
Under physiological conditions, MK is restrictively expressed in the adult organism. In contrast, inflamed synovial tissue of patients with rheumatoid arthritis showed strong MK expression, whereas no MK expression was detected in healthy control tissue [38]. Elevated MK expression was also observed in kidneys of patients with diabetic nephropathy, a pathological condition that is associated with tubulointerstitial and glomerular inflammation [39]. Inflammation caused by injury after implantation of vascular stents led to increased MK expression in the injured vascular wall compared to control vessels, in which MK could hardly be detected [40]. In a mouse model of experimental autoimmune encephalomyelitis (EAE), which has often been used to study the process underlying multiple sclerosis, MK mRNA was elevated in the spinal cord of EAE mice compared to control mice [41]. These examples demonstrate increased expression of MK under inflammatory conditions in different organs or tissues.
A common feature of inflammatory models using MK-deficient animals was reduced infiltration of leukocytes into the inflamed tissue, which was accompanied by reduced tissue damage [42,43,44]. The underlying cellular and molecular mechanisms of a decreased leukocyte infiltration and subsequent inflammation in the absence of MK were addressed by Weckbach et al. [27]: During the leukocyte recruitment process in postcapillary venules of the inflamed cremaster muscle (a well-established model to study leukocyte trafficking in vivo), the adhesion and subsequent extravasation steps were significantly impaired in MK-deficient mice compared to control animals [27]. In vitro, immobilized MK was able to promote adhesion of isolated neutrophils by stimulating a high affinity state of β2 integrins on neutrophils, which is essential for the firm adhesion and transmigration process of these cells [45].
While different receptor (complexes) for MK have been identified to be operative in various biological situations [6], the MK-mediated promotion of high-affinity-state β2 integrins was found to be abolished by blocking LRP-1 using the receptor-associated protein (RAP), suggesting that the MK-LRP-1 axis was involved in leukocyte adhesion to inflamed endothelium [27]. LRP1 is a large transmembrane receptor consisting of a large extracellular domain (515 kDa), non-covalently linked to a transmembrane domain (85 kDa). Four cysteine-rich complement-like repeats (CR) represent the majority of binding sites for a variety of non-related extracellular ligands, and most of them bind to CRII and CRIV of LRP-1 [46,47]. Based on its interaction with CRII of LRP-1 on rolling neutrophils [48] as well as with heparan proteoglycans on the endothelium, immobilized MK appears to be able to engage β2 integrins on neutrophils. In fact, an interaction and modification of β2 integrin function by LRP1 has been demonstrated in macrophages [49]. Additional mechanistic relations between MK and leukocyte-mediated inflammation have been proposed. Matsuda et al. showed that MK induced T cell expansion and regulated Th1 cell differentiation in a mouse model of lupus nephritis [50]. In a mouse model of EAE, MK increased inflammation by suppressing the development of tolerogenic dendritic cells, thereby inhibiting the differentiation of regulatory T cells [51]. Whether MK also directly affects T cell trafficking—as shown for neutrophils—has not yet been investigated. In addition to its role in modulating leukocyte recruitment during inflammation, MK has been demonstrated to display strong antibacterial activity, especially against gram-positive bacteria [52]. In septic patients, MK levels were significantly elevated compared to healthy controls, whereby the highest serum values were found in patients with gram-positive bacterial infections [53]. Phylogenetic and structural studies suggested that the peptide regions in MK and PTN for anti-microbial activity are conserved in MK orthologues in the zebrafish as well. The orthologue of MK and PTN in Drosophila melanogaster miple-2 also showed strong antibacterial properties, suggesting that the function of MK as intrinsic protective factor may be highly conserved among species [52]. There is growing evidence that MK reinforces the immune defense directly and by engaging and guiding leukocytes. However, there are additional functions of MK in the vascular system, which will be in part reviewed below.
3. Arteriogenesis
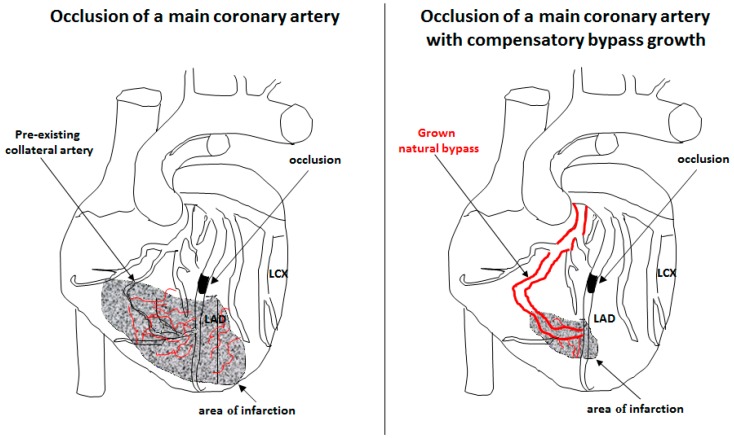
Coronary heart disease, stroke, and peripheral artery diseases, commonly referred to as cardiovascular diseases, are the leading causes of death worldwide and are associated with significant morbidity as well. The World Health Organization predicts around 23 million deaths due to cardiovascular diseases for the year 2030 [54]. Current state-of-the art treatment strategies for patients with occlusive diseases comprise percutaneous transluminal angioplasty (PTA), percutaneous transluminal coronary angioplasty (PTCA), or bypass surgery. However, certain patients do not require invasive procedures, because they benefit from the growth of pre-existing arteriolar collaterals into functional arteries, compensating for the loss of an artery due to occlusion (Figure 2). This process, defined as arteriogenesis [55,56], may be associated with patient survival. Indeed, a recent meta-analysis provided evidence that patients with high coronary collateralization showed a reduced risk of mortality [57]. Accordingly, much effort is made to decipher the molecular mechanisms of arteriogenesis aiming to identify drug targets and to enable clinicians to promote collateral-artery growth non-invasively.
Figure 2.
Collateral artery growth. Occlusion of a main coronary artery (left picture) results in severe ischemic cardiac-tissue damage (area of infarction) associated with extensive capillary sprouting in order to remove cell debris. If the loss of the occluded artery is compensated by natural bypass growth (arteriogenesis) (right picture), the extent of tissue damage and newly formed capillary network is strongly reduced. Coronary arteries: Left Anterior Descending (LAD), Left Circumflex (LCX). Adapted from Deindl et al., 2006 [63], with the permission of The FASEB Journal.
3.1. Innate Immunity
Intensive investigations over the last 20 years revealed that arteriogenesis is mediated by a local and temporary inflammatory response. Upon the narrowing of an artery, e.g., due to atherosclerotic plaque formation, blood flow is re-directed into pre-existing arteriolar connections. These vessels now experience an increased mechanical load, i.e., shear stress, which activates the endothelium of the small arterioles, finally resulting in collateral artery growth [58]. This inflammatory process is initiated by platelets [59] and the subsequent steps appear to be a blueprint of the inflammatory cell responses, known for the innate immunity process. Upon transient interaction with the stressed endothelium, mediated by the platelet receptor glycoprotein 1bα (GPIbα), P-selectin is expressed on the surface of platelets [60]. Subsequently, P-selectin binds to P-selectin glycoprotein ligand 1 (PSGL-1) provoking platelet-neutrophil aggregate (PNA) formation, which is associated with the activation of neutrophil NADPH oxidase 2 (Nox2) to produce high doses of reactive oxygen radicals (ROS) [61]. In the perivascular space, these ROS activate mast cells to de-granulate, which, in turn, create an inflammatory environment. By increasing the bioavailability of tumor necrosis factor α (TNFα) and monocyte chemoattractant protein-1 (MCP-1), mast cells recruit neutrophils in a positive feedback loop and contribute to the recruitment of T cells and macrophages [61]. Although the functional role of T cells in arteriogenesis remains to be elucidated, macrophages play a crucial role for collateral artery growth by supplying growth factors and cytokines to the growing vessel [62].
3.2. Mechanosensing/Shear Stress
Mechanosensing plays an important role in all kind of physiological processes during embryonic development, e.g., in pruning of the immature vascular plexus [64], but also in the adult organism. Sensing of mechanical forces is not only involved in touching or hearing, but plays an important role in the cardiovascular system, in vascular homeostasis, atherosclerosis, and also arteriogenesis [58,65]. For laminar shear stress, which is the triggering force for arteriogenesis, manifold sensors (underlined in the text below) have been identified [66]. Interestingly, some of them are identical to receptors described for MK (see above), or induce identical signal transduction cascades, suggesting that MK is involved in the process of mechanosensing.
The luminal, polyanionic endothelial cell glycocalyx consists of different glycoproteins, hyaluronic acid, and proteoglycans such as syndecans. Due to its negative charge, this extended inner surface layer of all blood (and lymphatic) vessels allows the binding of a diverse range of positively charged proteins, with a variety of functions [66]. As the glycocalyx mitigates the variable shear forces experienced by endothelial cells at different locations in the vascular tree, cytoskeleton-linked syndecans (particularly syndecan-1) appear to be responsible for mechanical load transfer into cells where the translation into chemical messages occurs [67,68]. Syndecans not only act as co-receptors for cytokines, but also cooperate with integrins [67] and are involved in flow-induced NFκB activation [69]. Moreover, syndecan-1 has been demonstrated to play a role in Akt activation [70], being part of the phosphoinositide 3-kinase/Akt/endothelial nitric oxide synthase (PI3K/Akt/eNOS) pathway. However, mechanosensors such as primary cilia, and ion channels such as the transient receptor potential vanilloid 4 (TRPV-4), which are involved in endothelium calcium influx, were also related to nitric oxide (NO) production and accordingly to vasodilation [71,72].
Together with their associated seven transmembrane receptors, heterotrimeric G-proteins participate in shear stress-induced signaling by forming mechanosensitive complexes with other mechanosensors. For example, the G-protein Gαq/11 forms a complex with platelet-endothelial cell adhesion molecule-1 (PECAM-1), stabilized by heparan sulfates [73]. While PECAM-1 and integrins activate shear stress-evoked PI3K signaling essential for eNOS activation, a mechanosensory trimolecular complex consisting of PECAM-1, vascular endothelial cell cadherin (VE-Cadherin), and vascular endothelial growth factor receptor 2 (VEGFR2), has been shown to be involved in shear stress sensing relevant for collateral-artery growth [74].
3.3. Vascular Cell Proliferation
3.3.1. Vascular Endothelial Growth Factor A (VEGF-A)
VEGF-A is well described to promote angiogenesis by interacting with VEGFR2. In contrast to arteriogenesis, which involves the proliferation of endothelial cells and smooth muscle cells, angiogenesis solely relies on the proliferation of endothelial cells forming capillaries. Capillaries have the function to distribute oxygen and metabolites locally, e.g., under conditions of tumor growth. However, in ischemic tissue, capillaries remove cell debris (Figure 2). Therefore, only collateral arteries, but not capillaries, can compensate for the loss of an artery caused by stenosis.
The functional role of VEGF-A in arteriogenesis has been controversially discussed for a long time, particularly based on the findings that administration of VEGF-A can hardly improve collateral-vessel formation. However, the blockade of VEGFR2 severely interfered with collateral-artery growth [75]. We were recently able to show that the bioavailability of VEGF-A is significantly increased after induction of arteriogenesis. Such elevated VEGF-A levels are critical and sufficient to promote collateral artery growth, whereas low concentrations of VEGF-A, as observed in MK-deficient mice, strongly hampered arteriogenesis. Moreover, treatment of wild-type mice with VEGF-A did not further promote the process of collateral artery growth [76]. Neither during the process of arteriogenesis, nor during the process of angiogenesis, VEGF-A is locally supplied by the tissue but by leukocytes, recruited to the sites of vessel growth [77,78]. For the process of angiogenesis, it has been demonstrated that chemokine (C-X-C motif) ligand 1 (CXCL-1), which is considered as the murine analogue to interleukin-8 (IL-8), and macrophage inflammatory protein-2 (MIP-2) locally recruit neutrophils, and that the release of VEGF-A from neutrophils is strictly dependent on CXCL-1/MIP-2 [78]. For arteriogenesis, it has been shown that CXCL-1 is upregulated in endothelial cells under conditions of increased shear stress in vivo [79] and in vitro [80]. Moreover, platelets, which we have shown to play an important role in arteriogenesis and to be involved in activating neutrophils by PNA formation, are a rich source of CXCL-1 [59,61,76]. In a recent study, it was shown that administration of CXCL-1 significantly promoted arteriogenesis, while blocking its receptor chemokine (C-X-C motif) receptor 2 (CXCR2) strongly interfered with collateral artery growth [79]. While CXCL-1 is relevant for initial neutrophil recruitment and release of VEGF-A in the early stages of arteriogenesis [61,76,78], MCP-1 likely overtakes these functions for macrophages [81,82], which become subsequently recruited to the perivascular tissue of growing collaterals as indicated before [61].
Interestingly, VEGF-A is only relevant for the proliferation of endothelial cells in growing collaterals, but not for smooth muscle cells [76]. This is even more astonishing as the activation of the VEGFR2/Neuropilin (NRP)1 receptor complex by VEGF-A [76,83] induces the release of von Willebrand factor (vWF) from endothelial cells [84]. vWF presents the major ligand of the platelet receptor GPIbα, and this interaction may initiate the inflammatory cascade, which is critical for the process of arteriogenesis.
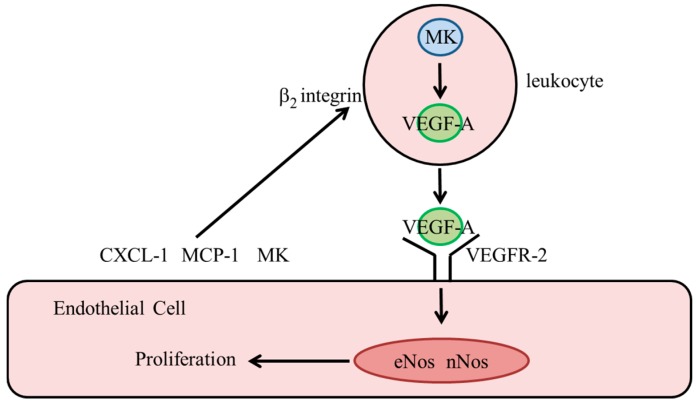
3.3.2. Midkine
Using a murine hindlimb model of collateral artery growth, we have recently shown that the process of arteriogenesis was severely compromised in MK-deficient mice, which was caused by a reduced bioavailability of VEGF-A [76]. MK deficiency resulted in hypertrophic outward remodeling, a process occurring when endothelial cell proliferation is reduced, while the proliferation of medial and adventitial cells remains unaffected [85]. MK was present in high amounts in neutrophils and macrophages [76,86], and indeed our results evidenced that leukocyte-derived MK was essential for collateral artery growth. A recent study demonstrated that overexpression of MK raised the expression level as well as the cellular release of VEGF-A [87]. Together, these data indicate that endothelial cell proliferation in arteriogenesis is dependent on the function of MK to mediate leukocyte (neutrophil and macrophage)-derived bioavailability of VEGF-A. We have previously shown that angiogenesis is severely impaired in MK-deficient mice, suggesting that MK also regulates the bioavailability of leukocyte-derived VEGF-A for endothelial cell proliferation in capillary sprouting [37]. These findings might have a major impact on the treatment of highly vascularized tumors as well, as tumor cells are likely to produce MK [5] to promote or even induce the vascularization of the tumor tissue itself. Accordingly, MK may represent a powerful tumor target. Further in-depth studies are required to prove this hypothesis. Whether there is a relationship between MK and the truncated variant of the somatostatin receptor subtype 5, sst5TMD4, which has been shown to elevate levels of VEGF when expressed in breast cancer cell lines [88], remains to be investigated.
Leukocyte recruitment and extravasation consists of several serial steps, starting with the capturing of free-flowing leukocytes, followed by leukocyte rolling on the endothelium, firm arrest, and finally diapedesis [89]. During rolling, leukocytes are activated by pro-inflammatory cytokines such as CXCL-1, which is associated with a rapid conformational change of β2 integrins [90,91,92]. The high-affinity conformation of β2 integrins is relevant for firm arrest of leukocytes to the endothelium by binding to ICAM-1 [93,94]. In a previous study, we have shown that MK supports adhesion of neutrophils by promoting the high-affinity conformational change of β2 integrins [27]. Another study demonstrated that activation of β2 integrins by MCP-1 resulted in increased expression levels of VEGF-A in macrophages [82].
In terms of arteriogenesis, the following scenario is proposed (Figure 3): During the recruitment process, leukocytes are in close contact with the inflamed endothelial surface, to which MCP-1, CXCL-1, and possibly MK are bound via ionic interactions. Juxtracrine signaling of these immobilized cytokines results in the stimulation of approximated leukocytes with the inside-out activation of their β2 integrins as well as an increased expression level and release of VEGF-A. Since bone marrow cell-derived, but not endothelial MK appears to be critical for arteriogenesis, MK concentrated within the glycocalyx of endothelial cells might be derived from bone-marrow cells. Moreover, MK expressed and stored in leukocytes might also contribute to the increased bioavailability of VEGF-A. Further research needs to uncover the cellular sources of MK and its signal-transduction mechanism in this particular context.
Figure 3.
Proposed model for the mechanistic function of MK in regulating vascular endothelial cell proliferation in arteriogenesis. During recruitment, leukocytes get in close contact with the endothelial cell surface, which is covered with CXCL-1, MCP-1 and MK. Upon integrin β2 activation, VEGF-A is increased, expressed, and released from leukocytes. However, not only MK stored on endothelial cell surface, but also MK stored in leukocytes might contribute to increased bioavailability of VEGF-A. Upon binding to VEGFR2, VEGF-A promotes the expression of eNOS and nNOS relevant for endothelial cell proliferation. Adapted from Lautz et al., 2018 [76].
3.3.3. Nitric Oxide Synthases
All isoforms of nitric oxide synthases, i.e., eNOS, neuronal NOS (nNOS), and inducible NOS (iNOS) have been described to contribute to arteriogenesis [76,95,96]. For angiogenesis, NO derived from eNOS has been implicated in endothelial cell proliferation [97,98,99]. As reduced perfusion recovery of eNOS-deficient mice was improved by administration of an NO donor, it was originally hypothesized that eNOS in arteriogenesis is only relevant for vasodilation [96,100]. We have recently shown that nNOS deficiency was not associated with reduced perfusion recovery in a hindlimb model of arteriogenesis. However, in contrast to eNOS deficiency, administration of an NO donor showed deleterious effects in nNOS-deficient mice [76]. Interestingly, MK-deficient mice showed reduced expression levels of eNos and nNos. Accordingly, we were interested whether the reduced levels of NO synthases were causative for impaired arteriogenesis in MK-deficient mice. Our results evidenced that treatment with an NO donor completely rescued diminished endothelial cell proliferation and hence the process of arteriogenesis in MK-deficient mice [76].
While eNOS has mainly been described to produce NO, nNOS is more involved in the generation of H2O2 [101,102], although uncoupling of eNOS promotes H2O2 production as well [103]. Both NO [97] as well as H2O2 [104,105] have been demonstrated to contribute to endothelial cell proliferation, and both NOS isoforms, eNOS and nNOS, can replace each other [106]. In a rodent model of cerebral aneurysm formation, the pathology outcome was neither affected in eNOS- nor in nNOS-deficient mice, but severely increased in mice deficient for both genes. While neither eNOS- nor nNOS-deficiency affects endothelial cell proliferation during arteriogenesis, it is strongly compromised in MK-deficient mice. Owing to the reduced expression levels of both eNOS and nNOS in MK-deficient mice, it is fair to deduce that both NOS isoforms can substitute for each other in their functional activities during arteriogenesis in terms of promoting endothelial cell proliferation.
It has been described that NO and VEGF-A affect their expression in a bi-directional manner [107,108]. In MK-deficient mice, administration of an NO donor did not restore the reduced VEGF-A level, whereas administration of VEGF-A rescued the reduced expression of eNOS and nNOS [76]. These data clearly demonstrate that during arteriogenesis, VEGF-A apparently regulates the expression levels of both NOS that are crucial for vascular endothelial-cell proliferation. The fact that the upstream MK regulates the bioavailability of VEGF-A renders MK a conductor to orchestrate endothelial cell proliferation during arteriogenesis (Figure 3).
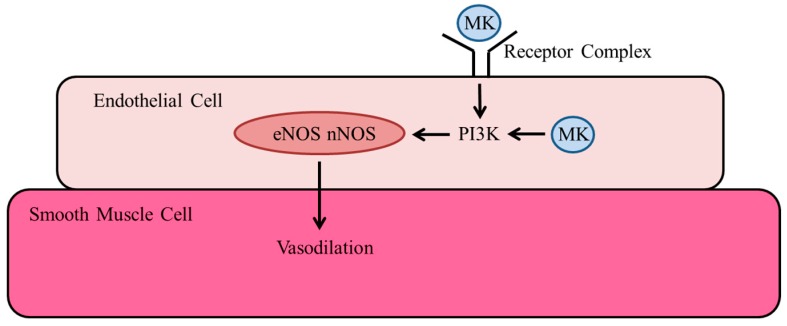
3.4. Vasodilation
NO is the most potent known vasodilator. We have recently shown that administration of VEGF-A did not promote vasodilation in wild-type mice, whereas administration of MK significantly increased vasodilation [76]. These data indicate that MK activates NOS independently from the VEGF-A pathway. It implies a direct action of MK on receptors of endothelial cells. It has previously been demonstrated in human umbilical vein endothelial cells (HUVECs) that stimulation with MK resulted in binding and phosphorylation of the MK receptor ALK and activation of PI3K and MAPK signaling [25]. In a murine model of myocardial infarction, it was shown that enhanced angiogenesis, induced by exogenous administered MK, was associated with PI3K/Akt and MAPK activation, and expression of syndecan-1, -3, and -4 [109]. Syndecan-1 is well-described to promote Akt activation [70]. Moreover, syndecans are co-receptors of integrins, and both, syndecan-1 as well as integrins, have not only been described to be receptors for MK and to be involved in Akt activation, but also to be involved in mechanosensing (see above).
There is a variety of studies relating PI3K to nNOS expression [110], as well as nNOS [111] and eNOS [112] activation. Interestingly, retinoic acid, which is described to induce the expression of MK [7], has also been shown to induce nNOS expression via the PI3K/Akt pathway [113]. Together, the available data suggest that a receptor complex on endothelial cells, which is involved in mechanosensing, is responsible for MK-mediated signal transduction pathways, resulting in NOS activation, which in turn is responsible for vasodilation. However, it appears that also intracellular MK can activate PI3K signaling and hence vasodilation [114].
Fujiwara et al. have recently described that MK is likely to act on growth hormone cells via the protein tyrosine phosphatase receptor-type Z, Ptprz1 [115], and Rubinek and Modan-Moses suggested that klotho is a direct regulator of growth hormone secretion [116,117]. In the literature, there are a several reports available demonstrating that growth hormone promotes vasodilation and restores endothelial function [118,119,120]. Accordingly, it is tempting to speculate that midkine might also promote vasodilation indirectly by increasing the bioavailability of growth hormone. However, further studies are necessary to confirm the relation between MK and growth hormone.
In one of our recent studies, we have shown that administration of MK to wild-type mice resulted in prolonged vasodilation, an effect that was not observed when mice were treated with an NO donor [76]. In patients, currently available NO donors do not show long-term vasodilation due to rapid tolerance, and here, MK may provide a novel alternative to induce the activation of NOS (Figure 4).
Figure 4.
Proposed model for the function of MK to promote vasodilation. Upon binding to a receptor complex, MK activates NOS via the phosphoinositide 3-kinase (PI3K)/Akt pathway. However, MK located in endothelial cells might also contribute by directly activating this signal transduction cascade. Adapted from Lautz et al., 2018 [76].
4. Conclusions
MK was originally identified as a modulator of embryonic development and was later assigned a role in tumor growth and inflammatory diseases. Meanwhile, MK is discovered as major determinant of the cardiovascular system involved in such important processes as translation of mechanical forces. It is not only engaged in vascular cell proliferation but even in regulation of the circulation.
Abbreviations
| MK | midkine |
| PTN | pleiotrophin |
| PTPζ | receptor-like protein tyrosine phosphatase β/protein tyrosine phosphatase ζ |
| WT-1 | Wilms tumor suppressor gene |
| PI3K | phosphatidylinositol 3-kinase |
| MAPK | mitogen-activated protein kinase |
| ALK | anaplastic lymphoma kinase |
| LRP | low-density-lipoprotein receptor-related protein |
| ICAM-1 | intercellular adhesion molecule-1 |
| NFκB | nuclear factor kappa-light-chain-enhancer of activated B cells |
| EAE | autoimmune encephalomyelitis |
| CR | cysteine rich complement-like repeats |
| PTA | percutaneous transluminal angioplasty |
| PTCA | percutaneous transluminal coronary angioplasty |
| GPIbα | glycoprotein 1bα |
| PSGL-1 | P-selectin glycoprotein ligand 1 |
| PNA | platelet-neutrophil aggregate |
| Nox2 | neutrophil-NADPH oxidase 2 |
| uPA | urokinase plasminogen activator |
| ROS | reactive oxygen species |
| TNFα | tumor necrosis factor α |
| MCP-1 | monocyte chemoattractant protein-1 |
| LAD | Left Anterior Descending |
| LCX | Left Circumflex |
| NO | nitric oxide |
| PECAM-1 | platelet adhesion molecule-1 |
| VE-Cadherin | vascular endothelial cell cadherin |
| VEGFR2 | vascular endothelial growth factor receptor 2 |
| TRPV-4 | transient receptor potential vanilloid 4 |
| VEGF-A | vascular endothelial growth factor A |
| CXCL-1 | chemokine (C-X-C motif) ligand 1 |
| MIP-2 | macrophage inflammatory protein-2 |
| CXCR2 | chemokine (C-X-C motif) receptor 2 |
| IL-8 | CXCL-8/interleukin-8 |
| NRP1 | Neuropilin 1 |
| vWF | von Willebrand factor |
| Mac-1 | macrophage-1 antigen |
| LFA-1 | lymphocyte function-associated antigen 1 |
| iNOS | inducible NOS |
| nNOS | neuronal NOS |
| CA | cerebral aneurisma |
Author Contributions
L.T.W., K.T.P., and D.E. wrote the paper.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Kadomatsu K., Tomomura M., Muramatsu T. cDNA cloning and sequencing of a new gene intensely expressed in early differentiation stages of embryonal carcinoma cells and in mid-gestation period of mouse embryogenesis. Biochem. Biophys. Res. Commun. 1988;151:1312–1318. doi: 10.1016/S0006-291X(88)80505-9. [DOI] [PubMed] [Google Scholar]
- 2.Shaheen K.Y., Abdel-Mageed A.I., Safwat E., AlBreedy A.M. The value of serum midkine level in diagnosis of hepatocellular carcinoma. Int. J. Hepatol. 2015;2015:146389. doi: 10.1155/2015/146389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vu Van D., Heberling U., Wirth M.P., Fuessel S. Validation of the diagnostic utility of urinary midkine for the detection of bladder cancer. Oncol. Lett. 2016;12:3143–3152. doi: 10.3892/ol.2016.5040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jia Q., Meng Z., Xu K., He X., Tan J., Zhang G., Li X., Liu N., Hu T., Zhou P., et al. Serum midkine as a surrogate biomarker for metastatic prediction in differentiated thyroid cancer patients with positive thyroglobulin antibody. Sci. Rep. 2017;7:43516. doi: 10.1038/srep43516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang L., Song X., Shao Y., Wu C., Jiang J. Prognostic value of Midkine expression in patients with solid tumors: A systematic review and meta-analysis. Oncotarget. 2018;9:24821–24829. doi: 10.18632/oncotarget.23892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weckbach L.T., Muramatsu T., Walzog B. Midkine in inflammation. Sci. World J. 2011;11:2491–2505. doi: 10.1100/2011/517152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kadomatsu K., Huang R.P., Suganuma T., Murata F., Muramatsu T. A retinoic acid responsive gene MK found in the teratocarcinoma system is expressed in spatially and temporally controlled manner during mouse embryogenesis. J. Cell Biol. 1990;110:607–616. doi: 10.1083/jcb.110.3.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Muramatsu T. Structure and function of midkine as the basis of its pharmacological effects. Br. J. Pharmacol. 2014;171:814–826. doi: 10.1111/bph.12353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaname T., Kuwano A., Murano I., Uehara K., Muramatsu T., Kajii T. Midkine gene (MDK), a gene for prenatal differentiation and neuroregulation, maps to band 11p11.2 by fluorescence in situ hybridization. Genomics. 1993;17:514–515. doi: 10.1006/geno.1993.1359. [DOI] [PubMed] [Google Scholar]
- 10.Simon-Chazottes D., Matsubara S., Miyauchi T., Muramatsu T., Guenet J.L. Chromosomal localization of two cell surface-associated molecules of potential importance in development: Midkine (Mdk) and basigin (Bsg) Mamm. Genome. 1992;2:269–271. doi: 10.1007/BF00355437. [DOI] [PubMed] [Google Scholar]
- 11.Reynolds P.R., Mucenski M.L., Le Cras T.D., Nichols W.C., Whitsett J.A. Midkine is regulated by hypoxia and causes pulmonary vascular remodeling. J. Biol. Chem. 2004;279:37124–37132. doi: 10.1074/jbc.M405254200. [DOI] [PubMed] [Google Scholar]
- 12.Matsubara S., Take M., Pedraza C., Muramatsu T. Mapping and characterization of a retinoic acid-responsive enhancer of midkine, a novel heparin-binding growth/differentiation factor with neurotrophic activity. J. Biochem. 1994;115:1088–1096. doi: 10.1093/oxfordjournals.jbchem.a124462. [DOI] [PubMed] [Google Scholar]
- 13.Adachi Y., Matsubara S., Pedraza C., Ozawa M., Tsutsui J., Takamatsu H., Noguchi H., Akiyama T., Muramatsu T. Midkine as a novel target gene for the Wilms’ tumor suppressor gene (WT1) Oncogene. 1996;13:2197–2203. [PubMed] [Google Scholar]
- 14.Iwasaki W., Nagata K., Hatanaka H., Inui T., Kimura T., Muramatsu T., Yoshida K., Tasumi M., Inagaki F. Solution structure of midkine, a new heparin-binding growth factor. EMBO J. 1997;16:6936–6946. doi: 10.1093/emboj/16.23.6936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kojima T., Katsumi A., Yamazaki T., Muramatsu T., Nagasaka T., Ohsumi K., Saito H. Human ryudocan from endothelium-like cells binds basic fibroblast growth factor, midkine, and tissue factor pathway inhibitor. J. Biol. Chem. 1996;271:5914–5920. doi: 10.1074/jbc.271.10.5914. [DOI] [PubMed] [Google Scholar]
- 16.Novotny W.F., Maffi T., Mehta R.L., Milner P.G. Identification of novel heparin-releasable proteins, as well as the cytokines midkine and pleiotrophin, in human postheparin plasma. Arterioscler. Thromb. 1993;13:1798–1805. doi: 10.1161/01.ATV.13.12.1798. [DOI] [PubMed] [Google Scholar]
- 17.Muramatsu T. Midkine and pleiotrophin: Two related proteins involved in development, survival, inflammation and tumorigenesis. J. Biochem. 2002;132:359–371. doi: 10.1093/oxfordjournals.jbchem.a003231. [DOI] [PubMed] [Google Scholar]
- 18.Fabri L., Maruta H., Muramatsu H., Muramatsu T., Simpson R.J., Burgess A.W., Nice E.C. Structural characterisation of native and recombinant forms of the neurotrophic cytokine MK. J. Chromatogr. 1993;646:213–225. doi: 10.1016/S0021-9673(99)87023-X. [DOI] [PubMed] [Google Scholar]
- 19.Asai T., Watanabe K., Ichihara-Tanaka K., Kaneda N., Kojima S., Iguchi A., Inagaki F., Muramatsu T. Identification of heparin-binding sites in midkine and their role in neurite-promotion. Biochem. Biophys. Res. Commun. 1997;236:66–70. doi: 10.1006/bbrc.1997.6905. [DOI] [PubMed] [Google Scholar]
- 20.Tsutsui J., Uehara K., Kadomatsu K., Matsubara S., Muramatsu T. A new family of heparin-binding factors: Strong conservation of midkine (MK) sequences between the human and the mouse. Biochem. Biophys. Res. Commun. 1991;176:792–797. doi: 10.1016/S0006-291X(05)80255-4. [DOI] [PubMed] [Google Scholar]
- 21.Winkler C., Schafer M., Duschl J., Schartl M., Volff J.N. Functional divergence of two zebrafish midkine growth factors following fish-specific gene duplication. Genome Res. 2003;13:1067–1081. doi: 10.1101/gr.1097503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Englund C., Birve A., Falileeva L., Grabbe C., Palmer R.H. Miple1 and miple2 encode a family of MK/PTN homologues in Drosophila melanogaster. Dev. Genes Evol. 2006;216:10–18. doi: 10.1007/s00427-005-0025-8. [DOI] [PubMed] [Google Scholar]
- 23.Maeda N., Ichihara-Tanaka K., Kimura T., Kadomatsu K., Muramatsu T., Noda M. A receptor-like protein-tyrosine phosphatase PTPzeta/RPTPbeta binds a heparin-binding growth factor midkine. Involvement of arginine 78 of midkine in the high affinity binding to PTPzeta. J. Biol. Chem. 1999;274:12474–12479. doi: 10.1074/jbc.274.18.12474. [DOI] [PubMed] [Google Scholar]
- 24.Qi M., Ikematsu S., Maeda N., Ichihara-Tanaka K., Sakuma S., Noda M., Muramatsu T., Kadomatsu K. Haptotactic migration induced by midkine. Involvement of protein-tyrosine phosphatase zeta. Mitogen-activated protein kinase, and phosphatidylinositol 3-kinase. J. Biol. Chem. 2001;276:15868–15875. doi: 10.1074/jbc.M005911200. [DOI] [PubMed] [Google Scholar]
- 25.Stoica G.E., Kuo A., Powers C., Bowden E.T., Sale E.B., Riegel A.T., Wellstein A. Midkine binds to anaplastic lymphoma kinase (ALK) and acts as a growth factor for different cell types. J. Biol. Chem. 2002;277:35990–35998. doi: 10.1074/jbc.M205749200. [DOI] [PubMed] [Google Scholar]
- 26.Muramatsu H., Zou K., Sakaguchi N., Ikematsu S., Sakuma S., Muramatsu T. LDL receptor-related protein as a component of the midkine receptor. Biochem. Biophys. Res. Commun. 2000;270:936–941. doi: 10.1006/bbrc.2000.2549. [DOI] [PubMed] [Google Scholar]
- 27.Weckbach L.T., Gola A., Winkelmann M., Jakob S.M., Groesser L., Borgolte J., Pogoda F., Pick R., Pruenster M., Muller-Hocker J., et al. The cytokine midkine supports neutrophil trafficking during acute inflammation by promoting adhesion via beta2 integrins (CD11/CD18) Blood. 2014;123:1887–1896. doi: 10.1182/blood-2013-06-510875. [DOI] [PubMed] [Google Scholar]
- 28.Muramatsu H., Zou P., Suzuki H., Oda Y., Chen G.Y., Sakaguchi N., Sakuma S., Maeda N., Noda M., Takada Y., et al. alpha4beta1- and alpha6beta1-integrins are functional receptors for midkine, a heparin-binding growth factor. J. Cell Sci. 2004;117:5405–5415. doi: 10.1242/jcs.01423. [DOI] [PubMed] [Google Scholar]
- 29.Ueoka C., Kaneda N., Okazaki I., Nadanaka S., Muramatsu T., Sugahara K. Neuronal cell adhesion, mediated by the heparin-binding neuroregulatory factor midkine, is specifically inhibited by chondroitin sulfate E. Structural ans functional implications of the over-sulfated chondroitin sulfate. J. Biol. Chem. 2000;275:37407–37413. doi: 10.1074/jbc.M002538200. [DOI] [PubMed] [Google Scholar]
- 30.Ichihara-Tanaka K., Oohira A., Rumsby M., Muramatsu T. Neuroglycan C is a novel midkine receptor involved in process elongation of oligodendroglial precursor-like cells. J. Biol. Chem. 2006;281:30857–30864. doi: 10.1074/jbc.M602228200. [DOI] [PubMed] [Google Scholar]
- 31.Kurosawa N., Chen G.Y., Kadomatsu K., Ikematsu S., Sakuma S., Muramatsu T. Glypican-2 binds to midkine: The role of glypican-2 in neuronal cell adhesion and neurite outgrowth. Glycoconj. J. 2001;18:499–507. doi: 10.1023/A:1016042303253. [DOI] [PubMed] [Google Scholar]
- 32.Nakanishi T., Kadomatsu K., Okamoto T., Ichihara-Tanaka K., Kojima T., Saito H., Tomoda Y., Muramatsu T. Expression of syndecan-1 and -3 during embryogenesis of the central nervous system in relation to binding with midkine. J. Biochem. 1997;121:197–205. [PubMed] [Google Scholar]
- 33.Gungor C., Zander H., Effenberger K.E., Vashist Y.K., Kalinina T., Izbicki J.R., Yekebas E., Bockhorn M. Notch signaling activated by replication stress-induced expression of midkine drives epithelial-mesenchymal transition and chemoresistance in pancreatic cancer. Cancer Res. 2011;71:5009–5019. doi: 10.1158/0008-5472.CAN-11-0036. [DOI] [PubMed] [Google Scholar]
- 34.Orr A.W., Sanders J.M., Bevard M., Coleman E., Sarembock I.J., Schwartz M.A. The subendothelial extracellular matrix modulates NF-kappaB activation by flow: A potential role in atherosclerosis. J. Cell Biol. 2005;169:191–202. doi: 10.1083/jcb.200410073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huang Y., Hoque M.O., Wu F., Trink B., Sidransky D., Ratovitski E.A. Midkine induces epithelial-mesenchymal transition through Notch2/Jak2-Stat3 signaling in human keratinocytes. Cell Cycle. 2008;7:1613–1622. doi: 10.4161/cc.7.11.5952. [DOI] [PubMed] [Google Scholar]
- 36.Campbell V.K., Anstey C.M., Gately R.P., Comeau D.C., Clark C.J., Noble E.P., Mahadevan K., Hollett P.R., Pollock A.J., Hall S.T., et al. Urine and serum midkine levels in an Australian chronic kidney disease clinic population: An observational study. BMJ Open. 2017;7:e014615. doi: 10.1136/bmjopen-2016-014615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Weckbach L.T., Groesser L., Borgolte J., Pagel J.I., Pogoda F., Schymeinsky J., Muller-Hocker J., Shakibaei M., Muramatsu T., Deindl E., et al. Midkine acts as proangiogenic cytokine in hypoxia-induced angiogenesis. Am. J. Physiol. Heart Circ. Physiol. 2012;303:429–438. doi: 10.1152/ajpheart.00934.2011. [DOI] [PubMed] [Google Scholar]
- 38.Takada T., Toriyama K., Muramatsu H., Song X.J., Torii S., Muramatsu T. Midkine, a retinoic acid-inducible heparin-binding cytokine in inflammatory responses: Chemotactic activity to neutrophils and association with inflammatory synovitis. J. Biochem. 1997;122:453–458. doi: 10.1093/oxfordjournals.jbchem.a021773. [DOI] [PubMed] [Google Scholar]
- 39.Kosugi T., Yuzawa Y., Sato W., Arata-Kawai H., Suzuki N., Kato N., Matsuo S., Kadomatsu K. Midkine is involved in tubulointerstitial inflammation associated with diabetic nephropathy. Lab. Investig. 2007;87:903–913. doi: 10.1038/labinvest.3700599. [DOI] [PubMed] [Google Scholar]
- 40.Banno H., Takei Y., Muramatsu T., Komori K., Kadomatsu K. Controlled release of small interfering RNA targeting midkine attenuates intimal hyperplasia in vein grafts. J. Vasc. Surg. 2006;44:633–641. doi: 10.1016/j.jvs.2006.04.044. [DOI] [PubMed] [Google Scholar]
- 41.Liu X., Mashour G.A., Webster H.F., Kurtz A. Basic FGF and FGF receptor 1 are expressed in microglia during experimental autoimmune encephalomyelitis: Temporally distinct expression of midkine and pleiotrophin. Glia. 1998;24:390–397. doi: 10.1002/(SICI)1098-1136(199812)24:4<390::AID-GLIA4>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 42.Wang J., Takeuchi H., Sonobe Y., Jin S., Mizuno T., Miyakawa S., Fujiwara M., Nakamura Y., Kato T., Muramatsu H., et al. Inhibition of midkine alleviates experimental autoimmune encephalomyelitis through the expansion of regulatory T cell population. Proc. Natl. Acad. Sci. USA. 2008;105:3915–3920. doi: 10.1073/pnas.0709592105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Maruyama K., Muramatsu H., Ishiguro N., Muramatsu T. Midkine, a heparin-binding growth factor, is fundamentally involved in the pathogenesis of rheumatoid arthritis. Arthritis Rheum. 2004;50:1420–1429. doi: 10.1002/art.20175. [DOI] [PubMed] [Google Scholar]
- 44.Horiba M., Kadomatsu K., Nakamura E., Muramatsu H., Ikematsu S., Sakuma S., Hayashi K., Yuzawa Y., Matsuo S., Kuzuya M., et al. Neointima formation in a restenosis model is suppressed in midkine-deficient mice. J. Clin. Investig. 2000;105:489–495. doi: 10.1172/JCI7208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Walzog B., Scharffetter-Kochanek K., Gaehtgens P. Impairment of neutrophil emigration in CD18-null mice. Am. J. Physiol. 1999;276:1125–1130. doi: 10.1152/ajpgi.1999.276.5.G1125. [DOI] [PubMed] [Google Scholar]
- 46.Lillis A.P., Mikhailenko I., Strickland D.K. Beyond endocytosis: LRP function in cell migration, proliferation and vascular permeability. J. Thromb. Haemost. JTH. 2005;3:1884–1893. doi: 10.1111/j.1538-7836.2005.01371.x. [DOI] [PubMed] [Google Scholar]
- 47.Lillis A.P., Van Duyn L.B., Murphy-Ullrich J.E., Strickland D.K. LDL receptor-related protein 1: Unique tissue-specific functions revealed by selective gene knockout studies. Physiol. Rev. 2008;88:887–918. doi: 10.1152/physrev.00033.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen S., Bu G., Takei Y., Sakamoto K., Ikematsu S., Muramatsu T., Kadomatsu K. Midkine and LDL-receptor-related protein 1 contribute to the anchorage-independent cell growth of cancer cells. J. Cell Sci. 2007;120:4009–4015. doi: 10.1242/jcs.013946. [DOI] [PubMed] [Google Scholar]
- 49.Ranganathan S., Cao C., Catania J., Migliorini M., Zhang L., Strickland D.K. Molecular basis for the interaction of low density lipoprotein receptor-related protein 1 (LRP1) with integrin alphaMbeta2: Identification of binding sites within alphaMbeta2 for LRP1. J. Biol. Chem. 2011;286:30535–30541. doi: 10.1074/jbc.M111.265413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Masuda T., Maeda K., Sato W., Kosugi T., Sato Y., Kojima H., Kato N., Ishimoto T., Tsuboi N., Uchimura K., et al. Growth Factor Midkine Promotes T-Cell Activation through Nuclear Factor of Activated T Cells Signaling and Th1 Cell Differentiation in Lupus Nephritis. Am. J. Pathol. 2017;187:740–751. doi: 10.1016/j.ajpath.2016.12.006. [DOI] [PubMed] [Google Scholar]
- 51.Sonobe Y., Li H., Jin S., Kishida S., Kadomatsu K., Takeuchi H., Mizuno T., Suzumura A. Midkine inhibits inducible regulatory T cell differentiation by suppressing the development of tolerogenic dendritic cells. J. Immunol. 2012;188:2602–2611. doi: 10.4049/jimmunol.1102346. [DOI] [PubMed] [Google Scholar]
- 52.Svensson S.L., Pasupuleti M., Walse B., Malmsten M., Morgelin M., Sjogren C., Olin A.I., Collin M., Schmidtchen A., Palmer R., et al. Midkine and pleiotrophin have bactericidal properties: Preserved antibacterial activity in a family of heparin-binding growth factors during evolution. J. Biol. Chem. 2010;285:16105–16115. doi: 10.1074/jbc.M109.081232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Krzystek-Korpacka M., Mierzchala M., Neubauer K., Durek G., Gamian A. Midkine, a multifunctional cytokine, in patients with severe sepsis and septic shock: A pilot study. Shock. 2011;35:471–477. doi: 10.1097/SHK.0b013e3182086001. [DOI] [PubMed] [Google Scholar]
- 54.World-Health-Organisation . WHO Fact Sheet N317: Cardiovascular Diseases. World-Health-Organisation; Geneva, Switzerland: 2013. [Google Scholar]
- 55.Deindl E., Schaper W. The art of arteriogenesis. Cell Biochem. Biophys. 2005;43:1–15. doi: 10.1385/CBB:43:1:001. [DOI] [PubMed] [Google Scholar]
- 56.Faber J.E., Chilian W.M., Deindl E., van Royen N., Simons M. A brief etymology of the collateral circulation. Arterioscler. Thromb. Vasc. Biol. 2014;34:1854–1859. doi: 10.1161/ATVBAHA.114.303929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Seiler C., Stoller M., Pitt B., Meier P. The human coronary collateral circulation: Development and clinical importance. Eur. Heart J. 2013;34:2674–2682. doi: 10.1093/eurheartj/eht195. [DOI] [PubMed] [Google Scholar]
- 58.Pipp F., Boehm S., Cai W.J., Adili F., Ziegler B., Karanovic G., Ritter R., Balzer J., Scheler C., Schaper W., et al. Elevated fluid shear stress enhances postocclusive collateral artery growth and gene expression in the pig hind limb. Arterioscler. Thromb. Vasc. Biol. 2004;24:1664–1668. doi: 10.1161/01.ATV.0000138028.14390.e4. [DOI] [PubMed] [Google Scholar]
- 59.Chandraratne S., von Bruehl M.L., Pagel J.I., Stark K., Kleinert E., Konrad I., Farschtschi S., Coletti R., Gartner F., Chillo O., et al. Critical role of platelet glycoprotein ibalpha in arterial remodeling. Arterioscler. Thromb. Vasc. Biol. 2015;35:589–597. doi: 10.1161/ATVBAHA.114.304447. [DOI] [PubMed] [Google Scholar]
- 60.Goto S., Ichikawa N., Lee M., Goto M., Sakai H., Kim J.J., Yoshida M., Handa M., Ikeda Y., Handa S. Platelet surface P-selectin molecules increased after exposing platelet to a high shear flow. Int. Angiol. 2000;19:147–151. [PubMed] [Google Scholar]
- 61.Chillo O., Kleinert E.C., Lautz T., Lasch M., Pagel J.I., Heun Y., Troidl K., Fischer S., Caballero-Martinez A., Mauer A., et al. Perivascular Mast Cells Govern Shear Stress-Induced Arteriogenesis by Orchestrating Leukocyte Function. Cell Rep. 2016;16:2197–2207. doi: 10.1016/j.celrep.2016.07.040. [DOI] [PubMed] [Google Scholar]
- 62.Arras M., Ito W.D., Scholz D., Winkler B., Schaper J., Schaper W. Monocyte activation in angiogenesis and collateral growth in the rabbit hindlimb. J. Clin. Investig. 1998;101:41–50. doi: 10.1172/JCI119877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Deindl E., Zaruba M.M., Brunner S., Huber B., Mehl U., Assmann G., Hoefer I.E., Mueller-Hoecker J., Franz W.M. G-CSF administration after myocardial infarction in mice attenuates late ischemic cardiomyopathy by enhanced arteriogenesis. FASEB J. 2006;20:956–958. doi: 10.1096/fj.05-4763fje. [DOI] [PubMed] [Google Scholar]
- 64.Lucitti J.L., Jones E.A., Huang C., Chen J., Fraser S.E., Dickinson M.E. Vascular remodeling of the mouse yolk sac requires hemodynamic force. Development. 2007;134:3317–3326. doi: 10.1242/dev.02883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Malota Z., Glowacki J., Sadowski W., Kostur M. Numerical analysis of the impact of flow rate, heart rate, vessel geometry, and degree of stenosis on coronary hemodynamic indices. BMC Cardiovasc. Disord. 2018;18:132. doi: 10.1186/s12872-018-0865-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Givens C., Tzima E. Endothelial Mechanosignaling: Does One Sensor Fit All? Antioxid. Redox Signal. 2016;25:373–388. doi: 10.1089/ars.2015.6493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Tkachenko E., Rhodes J.M., Simons M. Syndecans: New kids on the signaling block. Circ. Res. 2005;96:488–500. doi: 10.1161/01.RES.0000159708.71142.c8. [DOI] [PubMed] [Google Scholar]
- 68.Weinbaum S., Zhang X., Han Y., Vink H., Cowin S.C. Mechanotransduction and flow across the endothelial glycocalyx. Proc. Natl. Acad. Sci. USA. 2003;100:7988–7995. doi: 10.1073/pnas.1332808100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Liu Y., Sweet D.T., Irani-Tehrani M., Maeda N., Tzima E. Shc coordinates signals from intercellular junctions and integrins to regulate flow-induced inflammation. J. Cell Biol. 2008;182:185–196. doi: 10.1083/jcb.200709176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Voyvodic P.L., Min D., Liu R., Williams E., Chitalia V., Dunn A.K., Baker A.B. Loss of syndecan-1 induces a pro-inflammatory phenotype in endothelial cells with a dysregulated response to atheroprotective flow. J. Biol. Chem. 2014;289:9547–9559. doi: 10.1074/jbc.M113.541573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Cabral P.D., Garvin J.L. TRPV4 activation mediates flow-induced nitric oxide production in the rat thick ascending limb. Am. J. Physiol. Renal Physiol. 2014;307:666–672. doi: 10.1152/ajprenal.00619.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nauli S.M., Kawanabe Y., Kaminski J.J., Pearce W.J., Ingber D.E., Zhou J. Endothelial cilia are fluid shear sensors that regulate calcium signaling and nitric oxide production through polycystin-1. Circulation. 2008;117:1161–1171. doi: 10.1161/CIRCULATIONAHA.107.710111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.dela Paz N.G., Melchior B., Shayo F.Y., Frangos J.A. Heparan sulfates mediate the interaction between platelet endothelial cell adhesion molecule-1 (PECAM-1) and the Galphaq/11 subunits of heterotrimeric G proteins. J. Biol. Chem. 2014;289:7413–7424. doi: 10.1074/jbc.M113.542514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tzima E., Irani-Tehrani M., Kiosses W.B., Dejana E., Schultz D.A., Engelhardt B., Cao G., DeLisser H., Schwartz M.A. A mechanosensory complex that mediates the endothelial cell response to fluid shear stress. Nature. 2005;437:426–431. doi: 10.1038/nature03952. [DOI] [PubMed] [Google Scholar]
- 75.Jazwa A., Florczyk U., Grochot-Przeczek A., Krist B., Loboda A., Jozkowicz A., Dulak J. Limb ischemia and vessel regeneration: Is there a role for VEGF? Vasc. Pharmacol. 2016;86:18–30. doi: 10.1016/j.vph.2016.09.003. [DOI] [PubMed] [Google Scholar]
- 76.Lautz T., Lasch M., Borgolte J., Troidl K., Pagel J.I., Caballero-Martinez A., Kleinert E.C., Walzog B., Deindl E. Midkine Controls Arteriogenesis by Regulating the Bioavailability of Vascular Endothelial Growth Factor A and the Expression of Nitric Oxide Synthase 1 and 3. EBioMedicine. 2018;27:237–246. doi: 10.1016/j.ebiom.2017.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Deindl E., Buschmann I., Hoefer I.E., Podzuweit T., Boengler K., Vogel S., van Royen N., Fernandez B., Schaper W. Role of ischemia and hypoxia-inducible genes in arteriogenesis after femoral artery occlusion in the rabbit. Circ. Res. 2001;89:779–786. doi: 10.1161/hh2101.098613. [DOI] [PubMed] [Google Scholar]
- 78.Scapini P., Morini M., Tecchio C., Minghelli S., Di Carlo E., Tanghetti E., Albini A., Lowell C., Berton G., Noonan D.M., et al. CXCL1/macrophage inflammatory protein-2-induced angiogenesis in vivo is mediated by neutrophil-derived vascular endothelial growth factor-A. J. Immunol. 2004;172:5034–5040. doi: 10.4049/jimmunol.172.8.5034. [DOI] [PubMed] [Google Scholar]
- 79.Vries M.H., Wagenaar A., Verbruggen S.E., Molin D.G., Dijkgraaf I., Hackeng T.H., Post M.J. Erratum to: CXCL1 promotes arteriogenesis through enhanced monocyte recruitment into the peri-collateral space. Angiogenesis. 2015;18:173. doi: 10.1007/s10456-014-9458-x. [DOI] [PubMed] [Google Scholar]
- 80.Hagiwara H., Mitsumata M., Yamane T., Jin X., Yoshida Y. Laminar shear stress-induced GRO mRNA and protein expression in endothelial cells. Circulation. 1998;98:2584–2590. doi: 10.1161/01.CIR.98.23.2584. [DOI] [PubMed] [Google Scholar]
- 81.Ito W.D., Arras M., Winkler B., Scholz D., Schaper J., Schaper W. Monocyte chemotactic protein-1 increases collateral and peripheral conductance after femoral artery occlusion. Circ. Res. 1997;80:829–837. doi: 10.1161/01.RES.80.6.829. [DOI] [PubMed] [Google Scholar]
- 82.Morrison A.R., Yarovinsky T.O., Young B.D., Moraes F., Ross T.D., Ceneri N., Zhang J., Zhuang Z.W., Sinusas A.J., Pardi R., et al. Chemokine-coupled beta2 integrin-induced macrophage Rac2-Myosin IIA interaction regulates VEGF-A mRNA stability and arteriogenesis. J. Exp. Med. 2014;211:1957–1968. doi: 10.1084/jem.20132130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lanahan A., Zhang X., Fantin A., Zhuang Z., Rivera-Molina F., Speichinger K., Prahst C., Zhang J., Wang Y., Davis G., et al. The neuropilin 1 cytoplasmic domain is required for VEGF-A-dependent arteriogenesis. Dev. Cell. 2013;25:156–168. doi: 10.1016/j.devcel.2013.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Fischer S., Nishio M., Peters S.C., Tschernatsch M., Walberer M., Weidemann S., Heidenreich R., Couraud P.O., Weksler B.B., Romero I.A., et al. Signaling mechanism of extracellular RNA in endothelial cells. FASEB J. 2009;23:2100–2109. doi: 10.1096/fj.08-121608. [DOI] [PubMed] [Google Scholar]
- 85.Mulvany M.J. Vascular remodelling of resistance vessels: Can we define this? Cardiovasc. Res. 1999;41:9–13. doi: 10.1016/S0008-6363(98)00289-2. [DOI] [PubMed] [Google Scholar]
- 86.Narita H., Chen S., Komori K., Kadomatsu K. Midkine is expressed by infiltrating macrophages in in-stent restenosis in hypercholesterolemic rabbits. J. Vasc. Surg. 2008;47:1322–1329. doi: 10.1016/j.jvs.2007.12.037. [DOI] [PubMed] [Google Scholar]
- 87.Zhao S.L., Zhang Y.J., Li M.H., Zhang X.L., Chen S.L. Mesenchymal stem cells with overexpression of midkine enhance cell survival and attenuate cardiac dysfunction in a rat model of myocardial infarction. Stem Cell Res. Ther. 2014;5:37. doi: 10.1186/scrt425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Gahete M.D., Rincon-Fernandez D., Duran-Prado M., Hergueta-Redondo M., Ibanez-Costa A., Rojo-Sebastian A., Gracia-Navarro F., Culler M.D., Casanovas O., Moreno-Bueno G., et al. The truncated somatostatin receptor sst5TMD4 stimulates the angiogenic process and is associated to lymphatic metastasis and disease-free survival in breast cancer patients. Oncotarget. 2016;7:60110–60122. doi: 10.18632/oncotarget.11076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ley K., Laudanna C., Cybulsky M.I., Nourshargh S. Getting to the site of inflammation: The leukocyte adhesion cascade updated. Nat. Rev. Immunol. 2007;7:678–689. doi: 10.1038/nri2156. [DOI] [PubMed] [Google Scholar]
- 90.Abram C.L., Lowell C.A. The ins and outs of leukocyte integrin signaling. Annu. Rev. Immunol. 2009;27:339–362. doi: 10.1146/annurev.immunol.021908.132554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Jakob S.M., Pick R., Brechtefeld D., Nussbaum C., Kiefer F., Sperandio M., Walzog B. Hematopoietic progenitor kinase 1 (HPK1) is required for LFA-1-mediated neutrophil recruitment during the acute inflammatory response. Blood. 2013;121:4184–4194. doi: 10.1182/blood-2012-08-451385. [DOI] [PubMed] [Google Scholar]
- 92.Lefort C.T., Rossaint J., Moser M., Petrich B.G., Zarbock A., Monkley S.J., Critchley D.R., Ginsberg M.H., Fassler R., Ley K. Distinct roles for talin-1 and kindlin-3 in LFA-1 extension and affinity regulation. Blood. 2012;119:4275–4282. doi: 10.1182/blood-2011-08-373118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hentzen E.R., Neelamegham S., Kansas G.S., Benanti J.A., McIntire L.V., Smith C.W., Simon S.I. Sequential binding of CD11a/CD18 and CD11b/CD18 defines neutrophil capture and stable adhesion to intercellular adhesion molecule-1. Blood. 2000;95:911–920. [PubMed] [Google Scholar]
- 94.Pick R., Brechtefeld D., Walzog B. Intraluminal crawling versus interstitial neutrophil migration during inflammation. Mol. Immunol. 2013;55:70–75. doi: 10.1016/j.molimm.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 95.Pagel J.I., Borgolte J., Hoefer I., Fernandez B., Schaper W., Deindl E. Involvement of neuronal NO synthase in collateral artery growth. Indian J. Biochem. Biophys. 2011;48:270–274. [PubMed] [Google Scholar]
- 96.Troidl K., Tribulova S., Cai W.J., Ruding I., Apfelbeck H., Schierling W., Troidl C., Schmitz-Rixen T., Schaper W. Effects of endogenous nitric oxide and of DETA NONOate in arteriogenesis. J. Cardiovasc. Pharmacol. 2010;55:153–160. doi: 10.1097/FJC.0b013e3181c9556f. [DOI] [PubMed] [Google Scholar]
- 97.Cai J., Jiang W.G., Ahmed A., Boulton M. Vascular endothelial growth factor-induced endothelial cell proliferation is regulated by interaction between VEGFR-2, SH-PTP1 and eNOS. Microvasc. Res. 2006;71:20–31. doi: 10.1016/j.mvr.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 98.Fukumura D., Gohongi T., Kadambi A., Izumi Y., Ang J., Yun C.O., Buerk D.G., Huang P.L., Jain R.K. Predominant role of endothelial nitric oxide synthase in vascular endothelial growth factor-induced angiogenesis and vascular permeability. Proc. Natl. Acad. Sci. USA. 2001;98:2604–2609. doi: 10.1073/pnas.041359198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lee P.C., Salyapongse A.N., Bragdon G.A., Shears L.L., 2nd, Watkins S.C., Edington H.D., Billiar T.R. Impaired wound healing and angiogenesis in eNOS-deficient mice. Am. J. Physiol. 1999;277:1600–1608. doi: 10.1152/ajpheart.1999.277.4.H1600. [DOI] [PubMed] [Google Scholar]
- 100.Mees B., Wagner S., Ninci E., Tribulova S., Martin S., van Haperen R., Kostin S., Heil M., de Crom R., Schaper W. Endothelial nitric oxide synthase activity is essential for vasodilation during blood flow recovery but not for arteriogenesis. Arterioscler. Thromb. Vasc. Biol. 2007;27:1926–1933. doi: 10.1161/ATVBAHA.107.145375. [DOI] [PubMed] [Google Scholar]
- 101.Capettini L.S., Cortes S.F., Lemos V.S. Relative contribution of eNOS and nNOS to endothelium-dependent vasodilation in the mouse aorta. Eur. J. Pharmacol. 2010;643:260–266. doi: 10.1016/j.ejphar.2010.06.066. [DOI] [PubMed] [Google Scholar]
- 102.Costa E.D., Rezende B.A., Cortes S.F., Lemos V.S. Neuronal Nitric Oxide Synthase in Vascular Physiology and Diseases. Front. Physiol. 2016;7:206. doi: 10.3389/fphys.2016.00206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Li H., Wallerath T., Munzel T., Forstermann U. Regulation of endothelial-type NO synthase expression in pathophysiology and in response to drugs. Nitric Oxide. 2002;7:149–164. doi: 10.1016/S1089-8603(02)00111-8. [DOI] [PubMed] [Google Scholar]
- 104.Li J., Wang J.J., Zhang S.X. NADPH oxidase 4-derived H2O2 promotes aberrant retinal neovascularization via activation of VEGF receptor 2 pathway in oxygen-induced retinopathy. J. Diabetes Res. 2015;2015:963289. doi: 10.1155/2015/963289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Oshikawa J., Urao N., Kim H.W., Kaplan N., Razvi M., McKinney R., Poole L.B., Fukai T., Ushio-Fukai M. Extracellular SOD-derived H2O2 promotes VEGF signaling in caveolae/lipid rafts and post-ischemic angiogenesis in mice. PLoS ONE. 2010;5:e10189. doi: 10.1371/journal.pone.0010189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Son H., Hawkins R.D., Martin K., Kiebler M., Huang P.L., Fishman M.C., Kandel E.R. Long-term potentiation is reduced in mice that are doubly mutant in endothelial and neuronal nitric oxide synthase. Cell. 1996;87:1015–1023. doi: 10.1016/S0092-8674(00)81796-1. [DOI] [PubMed] [Google Scholar]
- 107.Kimura H., Esumi H. Reciprocal regulation between nitric oxide and vascular endothelial growth factor in angiogenesis. Acta Biochim. Pol. 2003;50:49–59. [PubMed] [Google Scholar]
- 108.Kroll J., Waltenberger J. VEGF-A induces expression of eNOS and iNOS in endothelial cells via VEGF receptor-2 (KDR) Biochem. Biophys. Res. Commun. 1998;252:743–746. doi: 10.1006/bbrc.1998.9719. [DOI] [PubMed] [Google Scholar]
- 109.Takenaka H., Horiba M., Ishiguro H., Sumida A., Hojo M., Usui A., Akita T., Sakuma S., Ueda Y., Kodama I., et al. Midkine prevents ventricular remodeling and improves long-term survival after myocardial infarction. Am. J. Physiol. Heart Circ. Physiol. 2009;296:462–469. doi: 10.1152/ajpheart.00733.2008. [DOI] [PubMed] [Google Scholar]
- 110.Fujibayashi T., Kurauchi Y., Hisatsune A., Seki T., Shudo K., Katsuki H. Mitogen-activated protein kinases regulate expression of neuronal nitric oxide synthase and neurite outgrowth via non-classical retinoic acid receptor signaling in human neuroblastoma SH-SY5Y cells. J. Pharmacol. Sci. 2015;129:119–126. doi: 10.1016/j.jphs.2015.09.001. [DOI] [PubMed] [Google Scholar]
- 111.Wu Z.T., Ren C.Z., Yang Y.H., Zhang R.W., Sun J.C., Wang Y.K., Su D.F., Wang W.Z. The PI3K signaling-mediated nitric oxide contributes to cardiovascular effects of angiotensin-(1-7) in the nucleus tractus solitarii of rats. Nitric Oxide. 2016;52:56–65. doi: 10.1016/j.niox.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 112.Fisslthaler B., Dimmeler S., Hermann C., Busse R., Fleming I. Phosphorylation and activation of the endothelial nitric oxide synthase by fluid shear stress. Acta Physiol. Scand. 2000;168:81–88. doi: 10.1046/j.1365-201x.2000.00627.x. [DOI] [PubMed] [Google Scholar]
- 113.Nagl F., Schonhofer K., Seidler B., Mages J., Allescher H.D., Schmid R.M., Schneider G., Saur D. Retinoic acid-induced nNOS expression depends on a novel PI3K/Akt/DAX1 pathway in human TGW-nu-I neuroblastoma cells. Am. J. Physiol. Cell Physiol. 2009;297:1146–1156. doi: 10.1152/ajpcell.00034.2009. [DOI] [PubMed] [Google Scholar]
- 114.Khan N., Binder L., Pantakani D.V.K., Asif A.R. MPA Modulates Tight Junctions’ Permeability via Midkine/PI3K Pathway in Caco-2 Cells: A Possible Mechanism of Leak-Flux Diarrhea in Organ Transplanted Patients. Front. Physiol. 2017;8:438. doi: 10.3389/fphys.2017.00438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Fujiwara K., Horiguchi K., Maliza R., Tofrizal A., Batchuluun K., Ramadhani D., Syaidah R., Tsukada T., Azuma M., Kikuchi M., et al. Expression of the heparin-binding growth factor midkine and its receptor, Ptprz1, in adult rat pituitary. Cell Tissue Res. 2015;359:909–914. doi: 10.1007/s00441-014-2073-8. [DOI] [PubMed] [Google Scholar]
- 116.Caicedo D., Diaz O., Devesa P., Devesa J. Growth Hormone (GH) and Cardiovascular System. Int. J. Mol. Sci. 2018;19:290. doi: 10.3390/ijms19010290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Rubinek T., Modan-Moses D. Klotho and the Growth Hormone/Insulin-Like Growth Factor 1 Axis: Novel Insights into Complex Interactions. Vitam. Horm. 2016;101:85–118. doi: 10.1016/bs.vh.2016.02.009. [DOI] [PubMed] [Google Scholar]
- 118.Caicedo D., Devesa P., Arce V.M., Requena J., Devesa J. Chronic limb-threatening ischemia could benefit from growth hormone therapy for wound healing and limb salvage. Ther. Adv. Cardiovasc. Dis. 2018;12:53–72. doi: 10.1177/1753944717745494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Evans L.M., Davies J.S., Anderson R.A., Ellis G.R., Jackson S.K., Lewis M.J., Frenneaux M.P., Rees A., Scanlon M.F. The effect of GH replacement therapy on endothelial function and oxidative stress in adult growth hormone deficiency. Eur. J. Endocrinol. 2000;142:254–262. doi: 10.1530/eje.0.1420254. [DOI] [PubMed] [Google Scholar]
- 120.Setola E., Monti L.D., Lanzi R., Lucotti P., Losa M., Gatti E., Galluccio E., Oldani M., Fermo I., Giovannelli M., et al. Effects of growth hormone treatment on arginine to asymmetric dimethylarginine ratio and endothelial function in patients with growth hormone deficiency. Metabolism. 2008;57:1685–1690. doi: 10.1016/j.metabol.2008.07.024. [DOI] [PubMed] [Google Scholar]