Abstract
Aloe genus plants, distributed in Old World, are widely known and have been used for centuries as topical and oral therapeutic agents due to their health, beauty, medicinal, and skin care properties. Among the well-investigated Aloe species are A. arborescens, A. barbadensis, A. ferox, and A. vera. Today, they account among the most economically important medicinal plants and are commonly used in primary health treatment, where they play a pivotal role in the treatment of various types of diseases via the modulation of biochemical and molecular pathways, besides being a rich source of valuable phytochemicals. In the present review, we summarized the recent advances in botany, phytochemical composition, ethnobotanical uses, food preservation, and the preclinical and clinical efficacy of Aloe plants. These data will be helpful to provide future directions for the industrial and medicinal use of Aloe plants.
Keywords: Aloe species, aloin, plicataloside, isovitexin, aloe emodin, aloesin, aloinoside
1. Introduction
Aloe L. is the largest genus in the Xanthorrhoeaceae family, and geographically restricted to Old World [1]. Its name derives from the Arabic word “Alloeh”, meaning “shining bitter substance” [2]. Aloe plants have been widely known and used for centuries as topical and oral therapeutic agent due to their health, beauty, medicinal, and skin care properties [2,3]. Aloe arborescens, Aloe barbadensis, Aloe ferox, and Aloe vera are among the well-investigated Aloe species. Presently, they account among the most economically important medicinal plants and are commonly used in primary health treatment, where they play a pivotal role in the treatment of various types of diseases, through biochemical and molecular pathway modulation [4]. Indeed, Aloe plants have been reported for multiple biological properties, including antibacterial and antimicrobial, antitumor, anti-inflammatory, anti-arthritic, anti-rheumatoid, anticancer, and antidiabetic activities, detoxification, treating constipation, flushing out toxins and wastes from the body, promoting digestion (on gastrointestinal disorders treatment), and reducing illnesses likelihood, as well as for immune system deficiencies [3,4,5,6,7,8,9]. Besides, several clinical trials validated the use of Aloe gel against several diseases, such as diabetes or antihyperglycemic, wound, and burn-healing topical agents [5,10,11]. The main commercial forms used in the food, cosmetics, and pharmaceutical industries [12,13] consisting of the plant’s fleshy leaves, gel, and latex are pills, jellies, creams, drinks, liquid, sprays, ointments, and lotions [3,13]. The nutrients and phytochemicals that have been identified in Aloe plants include vitamins, minerals, enzymes, simple and complex polysaccharides, fatty acids, indoles, alkanes, pyrimidines, aldehydes, dicarboxylic acids, ketones, phenolic compounds, phytosterols, and alkaloids with potential biological and toxicological activities [3,6,9]. On a side note, A. vera gel coating has demonstrated postharvest preservative and stabilizing effects in some foods and beverages, and for instance, table grapes [14,15]. However, A. vera administration is often related to kidney dysfunction, diarrhea, electrolyte imbalance, and conventional drug interactions. In addition, Aloe topical application has been associated with erythema, contact dermatitis episodes, and phototoxicity [3]. Aloe fleshy leaves, gel, and latex are the base of the main commercial forms of aloe products (e.g., pills, jellies, creams, drinks, liquids, sprays, ointments, and lotions) [3,13].
In view of the ethnopharmacological uses and pharmacological properties of Aloe plants, this review narratively summarized the botany, phytochemical composition, ethnobotanical uses, food preservative effects, and preclinical and clinical efficacy of Aloe plants to provide further direction for its utilization in human welfare.
2. Habitat and Cultivation of Aloe Plants
Aloe genus is a monoecious, perennial species with shallow roots. Aloe species are mostly inhabitants of arid climates, and are widely distributed in Africa, India, and other arid areas. The largest number of Aloe species is approximately 140, and most are found in South Africa [1]. However, they could also be grown in subtropical summer rainfall and winter rainfall regions [16]. The major factors restraining genus distribution are fire tolerance, soil moisture, rainfall, and temperature. Aloe species occupy a wide diversity of habitats, varying from sea level to altitudes of 2700 m, and from closed-canopy forests to desert shrub lands. However, some individual species showed particular geography restriction [17], although seed pollinator morphology and specificity also effect Aloe species distribution [18].
Aloe species can be cultivated in a wide range of soils. The most desirable soil texture is a loamy mixture with pH ranging from 7.0 to 8.5. Nonetheless, some species, such as Aloe commixta, Aloe haemanthifolia, Aloe plicatilis, and most grass aloe species prefer to grow in acidic soils [19]. Temperature requirements for Aloe growth range from 4 °C to 21 °C; however, this cold tolerant genus could maintain its growth even below 4 °C. Under optimal environmental conditions, Aloe species can reach heights of up to 61–99 cm. Regarding flowering duration, it may vary from May to June [19]. Some Aloe species appeared to react to soil mineral composition and produce differently colored flower varieties [20]. Although few Aloe genus species require specific pH and mineral composition, the majority of them can thrive in almost any soil type, and require little or no soil preparation before soil planting [21,22]. The ideal soil for establishment after Aloe species nursing is well-drained sandy soil or rocky sites. The adult plants of some Aloe species (e.g., A. greatheadii and A. secundiflora) can act as nurse plants themselves, colonizing, and ameliorating harsh conditions in sparsely vegetated or completely denuded landscapes [23,24]. Aloe species could also be effective agents for degraded rangeland treatment because of their mate (similar to root systems), which increases soil binding and stabilization [23].
3. Phytochemical Composition of Aloe Plants
Various species of Aloe genus plants have been proven to exert a diverse range of pharmacological activities. In addition, aloes are now considered to be a very interesting source of bioactive compounds [25]. Concurrently, some of the pharmacological activities reported, which support the traditional usages of each aloe species, have also been attributed to the presence of a wide range of phytoconstituents.
Aloe plant leaves, which are the most commonly used medicinal parts, are heterogeneous and can be divided into three major parts, namely: (i) the outer green epidermis, primarily consisting of structural components; (ii) the outer pulp region below the epidermis, consisting of vascular bundles where the bitter latex or sap is derived; and (iii) the inner leaf pulp, consisting of aloe gel and containing parenchyma cells. Regarding the different composition of these leaf portions, they are also likely to have distinct classes of bioactive compounds, which is believed to contribute to the different biological properties of leaves [26]. Briefly, the outer green epidermis has been reported to contain anthraquinones, pre-anthraquinones, and their corresponding glycosides [27], while the outer pulp region below the epidermis contains latex that predominantly consists of phenolic compounds, including anthraquinones and pre-anthraquinones, anthrones, chromones, coumarins, flavonoids, and pyrones [28]. On the other hand, the inner leaf pulp contains a high acemannan polysaccharide content, as well as a wide variety of phytochemicals, among them alkaloids, anthraquinones, anthrones, chromones, coumarins, flavonoids, and pyrones [27,29]. Pulp also contains vitamins, minerals, enzymes, and proteins [3]. Indeed, many authors believe that the various biological activities related to different Aloe species should be ascribed to a synergistic action between several compounds rather than a single chemical substance [29,30].
3.1. General Reports on Aloe Species Phytochemicals
Based on our literature search, various review articles that discuss Aloe phytochemical content are mostly focused on Aloe vera [2,31], with only Cock [26] providing a review article on the Aloe genus, which mainly focused on the close relationship between plants phytoconstituents and antioxidant capacity. However, most of the phytochemicals identified in the genus Aloe were not properly associated with the respective Aloe species from which they were isolated. Moreover, not all of the phytochemicals were completely cited by Cock [26], although he did cite all of the reports made by original authors. Prior to presenting our own report on Aloe species phytoconstituents, we take this opportunity to acknowledge the work of Cock [26], highlighting both bioactive compounds generally isolated and identified from the Aloe genus. Indeed, in his article, Cock [26] divided the discussion on Aloe genus phytoconstituents into several significant classes, namely anthraquinones, anthrones, chromones, coumarins, pyrans, pyrones, alkaloids, benzene, naphthalene, and furan derivatives.
3.1.1. Anthraquinones of Aloe Species
Various types of anthraquinones were also reported to be presented in Aloe species leaves, such as aloesaponarin, chrysophanol, and its progenitor prechrysophanol, desoxyerythrolaccin, 1,5-dihydroxy-3-hydroxy methylanthraquinone, helminthosporin, 7-hydroxyaloe emodin, isoxanthorin, laccaic acid-d-methyl ester, nataloe emodin, and its ester nataloe emodin-8-methyl ester, aloechrysone, and aloesaponol. In addition, Aloe anthraquinones are often present as O-glycosides, such as aloe emodin-11-O-rhamnoside, nataloe emodin-2-O-glucoside, aloesaponol-6-O-glucoside, aloesaponol-8-O-glucoside, and aloesaponol-O-methyl-4-O-glucoside. Other than that, leaf exudates from several Aloe species, such as Aloe saponaria Haw. and Aloe elgonica Bullock were also reported to contain anthraquinone dimers, such as asphodelin and bianthracene, and its glycosylated dimer derivative elgonicardine [26]. The hydroxylated derivatives of aloin, such as 5-hydroxyaloin A, 7-hydroxyaloin, and 10-hydroxyaloin B, as well as their acetate derivatives, 5-hydroxyaloin A 6′-O-acetate, 7-hydroxyaloin-6′-O-monoacetate, and 10-hydroxyaloin-6-O-acetate have also been identified. Except for A. saponaria and A. elgonica, no other Aloe species were reported in the discussion, despite the numerous mentioned anthraquinones isolated from this plant.
3.1.2. Anthrones of Aloe Species
Within the anthrones class, barbaloin, which referred to C-glycosyl anthrone isomers aloin A and aloin B, was the first Aloe anthrone to be isolated and can be detected in nearly 100 Aloe species, including A. vera and A. ferox leaves [26]. In addition, homonataloin and nataloin were consequently isolated from A. marlothii Berger. Other anthrones, some of them containing additional rhamnose, cinnamic, or coumaroyl moieties, have also been isolated from various Aloe species leaves, which include aloinoside, aloe barbendol, aloe-emodin anthrone, chrysophanolanthrone, aloe emodin-10-C-rhamnoside, 8-O-methyl-7-hydroxyaloin, 6′-O-cinnamoyl-8-O-methyl-7-hydroxyaloin, 6′-O-p-coumaroyl-7-hydroxyaloin, 7-hydroxyaloin-4′,6′-O-diacetate, 6′-O-cinnamoyl-5-hydroxyaloin A, microstigmin A, deacetyllittoraloin, littoraloin, littoraloside, microdontin, and homonataloside [26].
3.1.3. Chromones of Aloe Species
Another phytochemical group, known as chromones, are the most abundant phenolic compound class in Aloe leaves [26]. Aloeresin A and aloesin (previously known as aloeresin B), as well as 2′-p-O-methlcoumaroylaloesin, have been classified as some of the most commonly found Aloe leaf constituents. In addition, several isomeric and substituted isomeric forms, including aloeresin C, aloeresin D, aloeresin E, aloeresin F, iso-aloeresin A, and iso-aloeresin D have also been reported. These were later followed by the successful identification of a wide variety of chromones from distinct Aloe species, including methylated derivatives, such as 7-O-methylaloesin, 7-O-methylaloesinol, 7-O-methylaloeresin A, 8-[C-B-D-[2-O-(E)-cinnamoyl]glucopyranosyl]-2-[(R)-2-hydroxypropyl]-7-methoxy-5-methylchromone, 8-C-glycosyl-7-O-methylaloediol, 8-C-glycosyl-7-O-methyl-S-aloesol, 2-acetonyl-7-hydroxy-8-(2-furanonyl)-7-hydroxy-5-methylchromone, and 7-hydroxy-2,5-dimethylchromone. In addition to these, chromones containing cinnamic and coumaroyl moieties, such as 8-C-glycosyl-(2′-O-cinnamoyl)-7-O-methyl-aloediol, 8,2-acetonyl-8-(2′,6′-di-O,O-coumaroyl)-glucopyranosyl-7-hydroxy-5-methylchromone, 2-acetonyl-8-(2′,cinnamoyl)-glucopyranosyl-7-hydroxy-5-methylchromone, 6′-O-coumaroylaloesin, and 2′-p-O-methlcoumaroylaloesin have also been identified [26]. Unfortunately, for any of the chromones cited, not one specific Aloe species was excerpted.
3.1.4. Coumarins, Pyrans, and Pyrones of Aloe Species
Feralolide and dihydroisocoumarin glycoside are coumarins that have been identified in A. ferox and A. hildebrandtii [26], respectively. Pyrans (e.g., bisbenzopyran) and pyrones (e.g., aloenin, aloenin aglycone, aloenin acetal, aloenin B, and aloe-2″-p-O-coumaroyl ester) have also been identified in several Aloe species leaf exudates [26]. Except for A. ferox and A. hildebrandtii, the other Aloe species, from which coumarins, pyrans, and pyrones were isolated, were not revealed.
3.1.5. Alkaloids of Aloe Species
Several alkaloids have been isolated from several Aloe species [26]. N-methyltyramine and O,N-dimethyltyramine have been reported as being the most common Aloe alkaloids, whereas γ-coniceine was only found in a few species. In contrast, coniine has only been reported to occur in one species, Aloe viguieri Perrier [26]. Except for A. viguieri, the other Aloe species, from which the alkaloids were identified, were not quoted.
3.1.6. Benzene, Naphthalene, and Furan Derivatives of Aloe Species
Several benzene, naphthalene, and furan-based bioactive compounds have also been identified as common constituents of Aloe plants [26]. Among the identified benzene derivatives are protocatechuic acid, methyl-p-coumarate, and pluridone, which have been identified in several Aloes. Fluridone, which is the only sulfur derivative containing the benzene derivative identified from Aloe plants, was identified from A. pluridens Haw. Various naphthalene derivatives, namely aglycone isoeleutherol, isoeleutherol-5-O-glucoside, feroxidin, feroxidin A, feroxidin B, and plicataloside, have been isolated from Aloe plants, with aglycone isoeleutherol and isoeleutherol-5-O-glucoside specifically detected from Aloes roots portions. In addition to these, several of the naphthalene compounds, such as 5-OH-3-methylnaphto[2,3-c]furan-4(1H)-one, 3-methylnaphto[2,3-c]furan-4(9H)-one, and 3-methylnaphto[2,3-c]furan-4,9-dione have been found to contain a furan moiety [26]. Except for A. pluridens, the other Aloe species, from which the benzene, naphthalene, and furan derivatives were identified, were not named.
3.1.7. Flavonoids of Aloe Species
Several flavonoids were also detected in Aloe plants, with only naringenin, apigenin, isovitexin, and dihydro-isorhamnetin cited as being the major ones [26]. Nevertheless, the actual Aloe plants, from which flavonoids have been isolated, were not cited.
3.1.8. Sterols of Aloe Species
Phytosterols, such as cholesterol, campesterol, β-sitosterol, and lupeol together with their glucosides have also been cited to be present in Aloe leaves [26]. However, the actual Aloe plants, from which the sterols were isolated, were not mentioned.
3.1.9. Other Phenolic Constituent of Aloe Species
Although a number of other secondary metabolites were claimed to be present in Aloe leaves, Cock [26] only specifically cited the presence of tannins. Moreover, the actual Aloe plants, from which the secondary metabolites were isolated, were not indicated.
3.1.10. Non-Phenolic Components of Aloe Species
Polysaccharides are the non-phenolic components that are present in high abundance in Aloe leaf gels [26]. However, their presence within Aloe leaves are variable, and there is huge diversity among the different individual Aloes. According to Femenia et al. [32], polysaccharides composition and concentration also change with seasonal variations and growing environment conditions. Although several polysaccharides were detected in Aloe species, Cock [26] only mentioned acemannan (a long chain polymer of β (1→4) linked galactomannan saccharides). Unfortunately, the exact species from which polysaccharides were isolated were not mentioned.
3.1.11. Vitamins of Aloe Species
Cock [26] also cited the presence of various vitamins, namely vitamin C (ascorbic acid), vitamin B1 (thiamine), vitamin B2 (riboflavin), vitamin B6 (pyridoxal phosphate), vitamin B12 (cyanocobalamin), and vitamin E (α-tocopherol) in unspecified Aloe leaf gels.
3.1.12. Mineral Nutrients in Aloe species
Moreover, Cock [26] also mentioned that leaf gels from several Aloe species contain inorganic minerals, including magnesium, zinc, calcium, potassium, sodium, iron, phosphorous, manganese, copper, and molybdenum. However, species were not mentioned.
3.2. Specific Reports on Aloe Phytoconstituents
Cock [26] claimed that his review article on Aloe genus is not a comprehensive report. This claim was further supported by the lack of information with regard to Aloe’s phytoconstituents, such as no information on: (i) types of Aloe parts or extracts used to isolate bioactive compound(s); (ii) Aloe plants species used in the isolation of bioactive compound(s); and (iii) the location from which Aloe plants were collected, to name a few. Moreover, several phytoconstituents that were reported in some articles were not mentioned at all by Cock [26]. Taking these issues into consideration, the present review was performed with an attempt to provide more detail with regard to Aloe genus-isolated phytoconstituents.
Phytochemical Studies on Aloe Species
Many reports have been published concerning Aloe phytochemicals. Due to their economic and medical importance, Aloe phytoconstituents, especially those from the A. arborescens, A. barbadensis, A. ferox, and A. vera species, have been intensively investigated. The summary of phytochemical studies on Aloe species, including plant parts, principal constituents, and corresponding literatures is represented in Table 1, Table 2, Table 3, Table 4 and Table 5, according to investigated extraction methods. In most cases, leaf Aloe plants exudates were collected and used for phytoconstituent investigation purposes. Some researchers used fresh plant materials. Aloe plant extract chemical compositions were analyzed by solvent fractionation, column chromatography, preparative thin-layer chromatography (TLC), high-performance liquid chromatography (HPLC), HPLC–mass spectrometry (MS), and gas chromatography–mass spectrometry (GC–MS). In general, around 20 chemical constituents, including aloin A, aloin B, aloinoside A, and aloinoside B, aloesin, plicataloside, isovitexin, and aloe emodin were reported as principal Aloe species components.
Table 1.
Phytoconstituents of Aloe species detected by high-performance liquid chromatography (HPLC) and reversed-phase HPLC.
| Aloe Species | Phytochemicals | Reference |
|---|---|---|
| Leaves | ||
| A. africana | Aloesin D, aloin A, aloin B, aloinoside A, and aloinoside B | [33] |
| A. arborescens 1 | Aloenin, a phenyl pyrone, aloesin, aloeresin, aloin B, aloin A | [34] |
| Aloe emodin-diglucoside, lucenion II, 6′-O-caffeoyl-5-hydroxyaloin A, vicenin II, trans-p-coumaric derivatives, 3-O-(E)-caffeoyl-4-O-feruloylquinic acid, luteolin-O-xylosylglucoside malonylated, aloeresin C isomer, isorhamnetin-3-O-deoxyhexosyl(1-6) hexoside, 7-O-methyl kaempferol dimmer, caffeoyl quinic acid hexoside, kaempferol-3-O-hexosyl-O-pentoside, orientin, 3-O-caffeoyl-5-O-coumaroylquinic acid, 4-succinyl-3,4-dicaffeoylquinic acid, 6′-malonylnataloin, cholestenol, isoquercetrin, aloinoside A/B, 3,4-di-O-(E)-p-coumaroylquinic acid, 2′-O-feruloylaloesin, 7-O-methylaloesin-penta acetate, malonyl-4,5-O-dicaffeoylquinic acid, nataloin, veracylglucan A, aloenin B, wighteone-O-diglucoside malonylate, aloin A, caffeoylester of aloesin, aloeresin E, barbaloin (10R)/isobarbaloin (10S), quercetin-7-O-hexoside-3-O-malonylhexoside, aloe-emodin-8-O-glucoside, chrysophanol-8-O-(6′-O-galloyl-) glucoside, aloeresin H, and pentahydroxyflavonol-O-hexosyl rhamnoside | [35] | |
| A. archeri | Plicataloside | [36] |
| A. babatiensis | Plicataloside | [36] |
| A. barbadensis | 8-C-b-d-[2-O-(E)-coumaroyl]glucopyranosyl[2-[2-hydroxy]propyl-7-methoxy-5-methylchromone, aloeresin D, C-glucosyl chromone, and alcohol | [37] |
| A. boscawenii | Aloin A, aloin B, aloinoside A, aloinoside B, microdontin A, and microdontin B | [33] |
| A. brachystachys 1 | Aloesin, aloenin, aloin B, and aloin A | [34] |
| A. brandhamii 1 | Aloesin, aloenin, aloin B, and aloin A | [34] |
| A. brevifolia | cis-p-Coumaric acid derivatives, 5-O-caffeolyquinic acid, vicenin II, luteolin-O-xylosylglucoside malonylated, aloeresin C isomer, epi-catechin digalloyl rhamnoside, isorhamnetin-3-O-deoxyhexosyl(1-6) hexoside, caffeoyl quinic acid hexoside, 4-succinyl-3,4-dicaffeoylquinic acid, nataloin, cholestenol, 2’-O-feruloylaloesin, isoaloeresin D, and aloeresin | [35] |
| A. brunneostriata | Dihydroisocoumaringlucoside, aloin A, aloin B, aloinoside A, aloinoside B, microdontin A, and microdontin B | [33] |
| A. buchlohii | Aloin A, aloin B, microdontin A, and microdontin B | [33] |
| A. bussei 1 | aloesin, aloenin, aloin B, and aloin A | [34] |
| A. calidophila | Dihydroisocoumaringlucoside, aloin A, aloin B, aloinoside A, aloinoside B, microdontin A, and microdontin B | [33] |
| A. cameronii | Aloesin, aloeresin A, aloeresin D, aloin A, aloin B, aloinoside A, aloinoside B, microdontin A, and microdontin B | [33] |
| A. camperi | Dihydroisocoumaringlucoside, aloin A, aloin B, aloinoside A, aloinoside B, microdontin A, and microdontin B | [33] |
| A. canarina | Aloesin, aloeresin D, aloin A, aloin B, aloinoside A, aloinoside B, microdontin A, and microdontin B | [33] |
| A. chabaudii | Plicataloside | [36] |
| A. cheranganiensis 1 | Aloesin, 7-O-methylaloesin, aloenin, aloeresin A, aloeresin D, aloin B, aloin A | [34] |
| A. chrysostachys | 7-O-Methylaloesin, aloeresin D, aloin A, aloin B, aloinoside A, aloinoside B, microdontin A, and microdontin B | [33] |
| A. classenii 1 | Aloesin, aloenin, aloeresin D, aloin B, and aloin A | [34] |
| A. dawei 1 | Aloesin, aloenin, aloeresin D, aloin B, and aloin A | [34] |
| A. deserti | Plicataloside | [36] |
| A. diolii | Aloin A, aloin B, aloinoside A, aloinoside B, microdontin A, and microdontin B | [33] |
| A. dorotheae 1 | Aloesin, aloenin, aloin B, and aloin A | [34] |
| A. elegans | Dihydroisocoumaringlucoside, aloin A, aloin B, aloinoside A, aloinoside B, microdontin A, and microdontin B | [33] |
| A. eru | Vicenin II, 3-O-(E)-caffeoyl-4-O-feruloylquinic acid, iso pentyldihexose, apigenin-7-O-glycuronyl, aloenin, nataloin, cholestenol, isoquercetrin, aloinoside A/B, epi (afzelechin)—(epi) gallocatechin, 2′-O-feruloylaloesin, 7-methylether of 2′-feruloylaloesin, glucuronides, isoaloeresin D, aloeresin, kaempferol di deoxyhexosylhexoside, aloenin B, caffeoylester of aloesin, aloeresin E, apigenin-7-O-glycuronyl, aloe-emodin-8-O-glucoside, and 2′-p-methoxycoumaroylaloresin | [35] |
| A. ferox | cis-p-Coumaric acid derivatives, aloe emodin-diglucoside, lucenin II, vicenin II, orientin, 6’-malonylnataloin, kaempferol di deoxyhexosylhexoside, aloeresin E, quercetin pentosyl rutinoside, aloe-emodin-8-O-glucoside, and chrysophanol-8-O-(6′-O-galloyl-) glucoside | [35] |
| Aloin (A and B), aloinoside (A and B) and microdontin (A and B), aloesin, and aloeresin A | [33] | |
| A. fibrosa | Plicataloside | [36] |
| A. fleurentiniorum | Dihydroisocoumaringlucoside, aloin A, aloin B, aloinoside A, aloinoside B, microdontin A, and microdontin B | [33] |
| A. flexilifolia | Aloesin, 7-O-methylaloesin, aloeresin D, aloin A, aloin B, aloinoside A, aloinoside B, microdontin A, and microdontin B | [33] |
| A. francombei | Plicataloside | [36] |
| A. gilberti | Aloesin, 7-O-methylaloesin, aloin A, aloin B, aloinoside A, aloinoside B, microdontin A, and microdontin B | [33] |
| A. gossweileri 1 | Aloesin, aloenin, aloin B, and aloin A | [34] |
| A. grandidentata | Aloesin, aloe emodin-diglucoside, caffeoyl ferulic acid derivatives, chrysoeriol-7-O-glycuronyl, lucenin II, 6′-O-caffeoyl-5-hydroxyaloin A, vicenin II, 3-O-(E)-caffeoyl-4-O-feruloylquinic acid, luteolin-O-xylosylglucoside malonylated, isorhamnetin-3-O-deoxyhexosyl(1-6) hexoside, kaempferol-3-O-hexosyl-O-pentoside, orientin, isoorientin, 5-hydroxyaloin A, nataloin, cholestenol, aloinoside A/B, 3,4-di-O-(E)-p-coumaroylquinic acid, epi(afzelechin)-(epi)gallocatechin, 2′-O-feruloylaloesin, 7-methylether of 2′-feruloylaloesin, isoaloeresin D, aloeresin, nataloin, aloenin B, aloin A, aloin B, hydroxy octadecenic acid, trihydroxycinnamic acid derivatives, aloeresin E, acetyl dicaffeoylquinic acid, and kaempferol-3-O-malonylhexoside | [35] |
| A. guillaumetii | 7-O-Methylaloesin, aloin A, aloin B, aloinoside A, and aloinoside B | [33] |
| A. harlana | Aloin A, aloin B, aloinoside A, aloinoside B, microdontin A, and microdontin B | [33] |
| A. hemmingii | Aloesin, 8-O-methyl-7-hydro-xyaloin, aloin A, aloin B, aloinoside A, and aloinoside B | [33] |
| A. kedongensis 1 | Aloesin, 7-O-methylaloesin, aloenin, nataloin B, and nataloin A | [34] |
| A. labworana | Plicataloside | [36] |
| A. leachii 1 | Aloesin, aloenin, aloeresin D, aloin B, and aloin A | [34] |
| A. lensayuensis | Aloin A, aloin B, aloinoside A, aloinoside B, microdontin A, and microdontin B | [33] |
| A. leptosiphon 1 | Aloesin, aloenin, aloin B, and aloin A | [34] |
| A. mcloughlinii | Aloesin, dihydroisocoumaringlucoside, aloeresin D, aloin A, aloin B, aloinoside A, and aloinoside B | [33] |
| A. megalacantha | Dihydroisocoumaringlucoside, aloin A, aloin B, aloinoside A, aloinoside B, microdontin A, and microdontin B | [33] |
| A. microdonta | Aloin A, aloin B, aloinoside A, aloinoside B, microdontin A, and microdontin B | [33] |
| A. monticola 1 | Aloesin, aloenin, aloeresin D, aloin B, and aloin A | [34] |
| A. morijensis | Plicataloside | [36] |
| A. multicolor | Plicataloside | [36] |
| A. murina | Plicataloside | [36] |
| A. ngongensis | Aloeresin D, aloin A, aloin B, aloinoside A, aloinoside B, microdontin A, and microdontin B | [33] |
| A. nyeriensis 1 | Nataloe-emodin, nataloe-emodin-2-O-Glc, nataloin, aloenin, aloenin aglycone, and aloenin-2″-p-coumaroyl ester | [38] |
| A. otallensis | Plicataloside | [36] |
| A. palmiformis | Plicataloside | [36] |
| A. parvidens | Plicataloside | [36] |
| A. peckii | Aloesin, dihydroisocoumaringlucoside, aloeresin D, aloin A, aloin B, aloinoside A, and aloinoside B | [33] |
| A. peglerae | Aloesin, aloeresin E, aloeresin F, homonataloin A, and homonataloin B | [39] |
| A. penduliflora | 7-O-Methylaloesin, dihydroisocoumaringlucoside, aloin A, aloin B, aloinoside A, and aloinoside B | [33] |
| A. perfoliata | Aloesin, 1-hexanol-pentosylhexoside, 3-O-(E)-caffeoyl-4-O-feruloylquinic acid, luteolin-O-xylosylglucoside malonylated, aloeresin C isomer, epi-catechin digalloyl rhamnoside, 7-O-methyl kaempferol dimmer, orientin, 3-O-caffeoyl-5-O-coumaroylquinic acid, 4-succinyl-3,4-dicaffeoylquinic acid, 5-hydroxyaloin A, aloinoside A/B, epi (afzelechin)—(epi)gallocatechin, 7-O-Mmethylaloesin-penta acetate, glucuronides, isoaloeresin D, isovitexin, 6′-O-coumaroyl aloesin, aloeresin A isomer, caffeoylester of aloesin, aloeresin E, acetyl dicaffeoylquinic acid, quercetin-7-O-hexoside-3-O-malonylhexoside, aloe-emodin-8-O-glucoside, 2′-p-methoxycoumaroylaloresin, aloeresin H, pentahydroxyflavonol-O-hexosyl rhamnoside, and kaempferol-3-O-malonylhexoside | [35] |
| A. plicatilis | Plicataloside | [36] |
| A. pustuligemma | Plicataloside | [36] |
| A. rabaiensis | Aloeresin D, aloin A, aloin B, aloinoside A, and aloinoside B | [33] |
| A. rivae | Dihydroisocoumaringlucoside, aloin A, aloin B, aloinoside A, aloinoside B, microdontin A, and microdontin B | [33] |
| A. rugosifolia | Plicataloside | [36] |
| A. saponaria | cis-p-Coumaric acid derivatives, 3,4-di-O-(E)-caffeoylquinic acid, malonyl-3,4-O-dicaffeoyl quinic acid, lucenin II, luteolin-O-xylosylglucoside malonylated, isorhamnetin-3-O-deoxyhexosyl(1-6) hexoside, 4-succinyl-3,4-dicaffeoylquinic acid, 2′-O-feruloylaloesin, 7-O-methylaloesin-penta acetate, 7-methylether of 2′-feruloylaloesin, trihydroxy octadecenoic acid, quercetin-7-O-hexoside-3-O-malonylhexoside, aloe-emodin-8-O-glucoside, 2′-p-methoxycoumaroyl-aloresin, aloeresin H, and tetra-O-methyl ether | [35] |
| A. scabrifolia | Dihydroisocoumaringlucoside, aloin A, aloin B, aloinoside A, aloinoside B, microdontin A, and microdontin B | [33] |
| A. schelpei | 8-O-Methyl-7-hydroxyaloin, aloin A, aloin B, microdontin A, and microdontin B | [33] |
| A. schweinfurthii | Plicataloside | [36] |
| A. scobinifolia | Dihydroisocoumaringlucoside, aloin A, aloin B, aloinoside A, aloinoside B, microdontin A, and microdontin B | [33] |
| A. secundiflora | Aloenin, aloenin B, isobarbaloin (aloin B), barbaloin (aloin A), aloinside A, aloinside B, aloesin derivative, and an unidentified mixture of dimers | [40] |
| A. secundi flora 1 | Aloenin, aloin B, and aloin A | [34] |
| A. sinkatana | 8-O-Methyl-7-hydroxyaloin, aloin A, aloin B, aloinoside A, and aloinoside B | [33] |
| A. somaliensis | Dihydroisocoumaringlucoside, aloin A, aloin B, aloinoside A, aloinoside B, microdontin A, and microdontin B | [33] |
| A. steudneri | Dihydroisocoumaringlucoside, 8-O-methyl-7-hydroxyaloin, aloin A, aloin B, microdontin A, and microdontin B | [33] |
| A. tewoldei | Dihydroisocoumaringlucoside, aloin A, aloin B, aloinoside A, aloinoside B, microdontin A, and microdontin B | [33] |
| A. tormentorii | Phenols, saponins, tannins, alkaloids, anthraquinones, terpenes, coumarins and flavonoids | [41] |
| A. tororoana 1 | 7-O-Methylaloesin, aloenin, aloin B, and aloin A | [34] |
| A. tugenensis | Plicataloside | [36] |
| A. tweediae | Dihydroisocoumaringlucoside, aloeresin D, aloin A, aloin B, aloinoside A, and aloinoside B | [33] |
| A. ukambensis | Plicataloside | [36] |
| A. vera | cis-p-Coumaric acid derivatives, malonyl-3,4-O-dicaffeoyl quinic acid, lucenin II, 6′-O-caffeoyl-5-hydroxyaloin A, vicenin II, trans-p-coumaric derivatives, luteolin-O-xylosylglucoside malonylated, aloeresin C isomer, isorhamnetin-3-O-deoxyhexosyl(1-6) hexoside, 7-O-methyl kaempferol dimmer, caffeoyl quinic acid hexoside, orientin, isoorientin, 3-O-caffeoyl-5-O-coumaroylquinic acid, 6’-malonylnataloin, aloinoside A/B, 7-O-methylaloesin-penta acetate, malonyl-4,5-O-dicaffeoylquinic acid, nataloin, aloenin B, wighteone-O-diglucoside malonylate, aloin A, aloin B, aloeresin E, barbaloin (10R)/isobarbaloin (10S), quercetin-7-O-hexoside-3-O-malonylhexosidea, and aloe-emodin-8-O-glucoside | [35] |
| A. wredfordii | Plicataloside | [36] |
1 Reversed-phase HPLC.
Table 2.
Phytoconstituents of Aloe species detected by gas chromatography coupled to mass spectrometry (GC–MS).
| Aloe Species | Phytochemicals | Reference |
|---|---|---|
| Leaves | ||
| A. albiflora | Trimethylsilyl ether 2-hexanol, benzene acetaldehyde, lactic acid, benzyldimethylsilyl ester hydrocinnamic acid, 2,4-dimethyl benzaldehyde, 2-ethyl phenol, trimethylsilyl ether 9-decen-1-ol, trimethylsilyl ester benzene acetic acid, trimethylsilyl ester nonanoic acid, 2-methoxy-3-(2-propenyl)-phenol, 3-(2-trimethylsilyloxyethyl)-phenol, methyleugenol, phenyl 1,2-ethanediol, 2,4-bis(1,1-dimethylethyl)-phenol, 2-methyl-1-hexadecanol, nonadecane, 1-methylethyl ester dodecanoic acid, lauric acid, β-bisabolol, 2,6,10-trimethyl-tetradecane, tert-hexadecanethiol, tetradecanoic acid, pentadecanoic acid, ethyl ester cholestenol acid, trimethylsilyl ester cis-9-hexadecenic acid, palmitic acid, cis-13-eisosenoic acid, heptadecanoic acid, ethyl 9,12,15-octadecatrienoate, linoleic acid, α-linolenic acid, octadecanoic acid, eicosanoic acid, squalene, and β-sitosterol | [42] |
| A. aristata | Benzeneacetaldehyde, lactic acid, 2-methyl-2-indecanethiol, 2,5-dimethyl-benzaldehyde, 2-ethyl-phenol, trimethylsilyl ether 3-ethylphenol, p-ethylguaiacol, phosphoric acid, tridecane, (E)-3-eicosene, 2-methyl-1-hexadecanol, 2,6,11-trimethyl-dodecane, eugenol, vanillin, methyleugenol, hexadecane, 2,4-bis(1,1-dimethylethyl)-phenol, nonadecane, 1-methlethyl ester dodecanoic acid, lauric acid, 2,6,10-trimethyl tetradecane, 2,6,10,15-tetramethyl heptadecane, trimethylsilyl ester myristic acid, pentadecanoic acid, ethyl palmitate, trimethylsilyl ester cis-9-hexadecenoic acid, palmitic acid, trimethylsilyl ester cis-10-heptadecenoic acid, heptadecanoic acid, ethyl ester 9,12-octadecadienoic acid, ethyl 9,12,15-octadecatrienoate, linoleic acid, α-linolenic acid, octadecanoic acid, α-amyrin, squalene, ethyl iso-allocholate, and β-sitosterol | [42] |
| A. aspera | Trimethylsilyl ether 2-pentanol, m-pyrol, lactic acid, 3,5-dimethyl-benzaldehyde, benzoic acid, succinic acid, fumaric acid, nonanoic acid, tetradecane, trimethylsilyl ester decanoic acid, 2,4-bis(1,1-dimethylethyl)-phenol, 2,3,5,8-tetramethyl-decane, 2-methyl-1-hexadecanol, hexadecane, 1-methylethyl ester dodecanoic acid, lauric acid, nonadecane, 2,6,10,15-tetramethyl-heptadecane, 2,6,10-trimethyl-tetradecane, azelaic acid, isopropyl ester myristic acid, tetradecanoic acid pentadecanoic acid, trimethylsilyl ester cis-9-hexadecenoic acid, palmitic acid, heneicosane, heptadecanoic acid, linoleic acid, trimethylsilyl ester oleic acid, octadecanoic acid, eicosanoic acid, trimethylsilyl ester 1-docosanol, docosanoic acid, squalene, trimethylsilyl ester tetracosanoic acid, γ-tocopherol, ethyl iso-allocholate, 1-heptatriacotanol, campesterol, stigmasterol, β-sitosterol | [42] |
| A. excelsa | Limonene, carvone, and 2-phenylacetonitrile | [43] |
| A. ferox | Polyphenols/phenolic compounds (phenol, gentisic, cholestenol, homovanilic, O-hydroxycinnamic, protocatechuic, 3,4-dihydroxyphenylacetic, 5-methoxyprotocatechuic, syringic, sinapic, p-coumaric, caffeic, isoferulic, ferulic, 4-methoxycinnamic, aloe emodin, 4-phenyllactic, 4-ethylphenol, p-toluic, hydrocinnamic, p-salicylic, benzoic, mandelic, hydroxyphenylacetic, pyrocatechuic, hydro-p-coumaric, and 6,7-dihydroxycoumarin); organic acids (isovaleric, lactic, glycolic, furoic, 3-hydroxypropionic, 2-hydroxyvaleric, cyclohexanone-3-carboxylic, 3-hydroxyisovaleric, 3-methyl-1,3-hydroxybutanoic, 2-hydroxycaproic, 2-ketoisovaleric, succinic, 2-methylsuccinic, methylmalic, malic, 3,4,5-trihydroxypentanoic, d-ribonic, suberic, 3-hydroxypicolinic, and isonicotinic); fatty acids (lauric, myristic, cholestenol, palmitoleic, palmitic, stearic, linoleic, oleic, linolenic, erucic, cholestenol, arachidic, heneicosanoic, behenic, tricosanoic, lignoceric and pentacosanoic); alkaloids (hypoxanthine and xanthine); indoles (indole-5-acetic acid, and indole-3-acetic acid); pyrimidines (uracil and thymine); alkanes (1,3-dihydroxybutane); sterols (cholestenol, campestrol, â-sitosterol, and stigmasterol); dicarboxylic acids (azelaic and undecanedioic), and ketones (4,6-dimethyl-2-heptanone, acetophenone, and 2,4-dimethyl-4-heptanone) | [44] |
| A. jucunda | Benzaldehyde, lactic acid, 2-ethyl phenol, benzoic acid, ester octanoic acid, phenylacetic acid, 4-ethyl-1,2-benzene, dimethoxy-benzaldehyde, 4-vinylveratrole, eugenol, tetradecane, methyleugenol, 2-allyl-1,4-dimethoxy-3-methyl-benzene, nonadecane, 3,5-bis(1,1-dimethylethyl)-phenol, 1,2-dimethoxy-4-(2-methoxyethenyl)benzene, 1-dodecanol, estragole, dodecanoic acid, 1-methylethyl ester, 4-hydroxybenzoic acid lauric acid, β-bisabolol, 2,6,10-trimethyl-tetradecane, geranyl isovalerate, tetradecanoic acid, 3,5-bis(1,1-dimethylethyl)-4-benzoic acid, methyl ester hexadecenoic acid, 2,4,6-tris(1,1-dimethylethyl)-phenol, ethyl palmitate, trimethylsilyl ester palmitelaidic acid, palmitic acid, methyl ester linolenic acid, heptadecanoic acid, ethyl ester 9,12-octadecadienoic acid, ethyl 9,12,15-octadecatrienoate, ethyl ester stearic acid, linoleic acid, α-linolenic acid, octadecanoic acid, ester eicosanoic acid, bumetrizole, trimethylsilyl ester cis-13-docosenoic acid, ester docosanoic acid, squalene, heptacosane, ethyl iso-allocholate, and β-amyrin | [42] |
| A. vera | Debocane, 4-methyl, tricosane, 6-hydroxyhexane-3-1, 1-dodecanol, 1-octadecanol, cholestenol acid, 9-octadecenoic acid, octadecanoic acid, 1-(phenylthioxomethyl)piperidine, docosane, sitosterol, and stigmasterol | [45] |
| Phenolic acids or polyphenols (phenol, cholestenic acid, homovanilic acid, protocatechuic acid, 3,4-dihydroxyphenylacetic acid, 5-methoxyprotocatechuic acid, and syringic acid. Sinapic acid, p-coumaric acid, isoferulic acid, ferulic acid, aloe emodin, 4-phenyllactic acid, 4-ethylphenol, hydrocinnamic acid, p-salicylic acid, benzoic acid, and hydro-p-coumaric acid); alcohols (2-butanol, glycerol, and phenylethanol); aldehydes (benzaldehyde and m-tolualdehyde); organic acids (lactic acid, glycolic acid, pyruvic acid, furoic acid, phosphoric acid, succinic aid, 2-methylsuccinic acid, malicnaicd, tartaric acid, and isonicotinic acid); alkanes (1,3-dihydroxybutane); pyrimidines (uracil and thymine) fatty acids (lauric acid, myristic acid, palmitoleic acid, and linoleic acid) indoles (indole-3-acetic acid); alkaloids (hypoxanthine); ketones (acetophenone); sterols (cholestenol and β-sitosterol); dicarboxylic acids (azelaic acid and undecanedioic acid) | [6] | |
| Ethylene glycol, propylene glycol, 2,3-bis(trimethylsiloxy)-butane, glycolic acid, 6-methyl-octadecane, 4-ethylbenzaldehyde, 4-hydroxybutyric acid, benzoic acid, (±)-2-Hydroxyoctanoic acid, octanoic acid, succinate, methyl succinic acid, glyceric acid, fumaric aicd, nonanoic acid, 2-methoxy-3-(2-prophenyl)-phenol, teradecane, methyleugenol, glutarate, 4-allyl-2-methoxyphenoxy-i-dodecanol, β-copaene, malic acid, adipic acid, 2-methyl-1-hexadecanol, bis(trimethylsilyl-pyroglutamic acid, m-hydroxybenzoic acid, pimelic acid, 1-methylethyl ester dodecanoic acid, 4-hydroxybenzoic acid, lauric acid, 1-[(trimethylsilyl)oxy]-2-methylanthraquinone, suberic acid, geranyl isovalerate, 2,6,10-timethyl tetradecane, bis(trimethylsilyl) ester 1,3-benzenedicarboxylic acid, azelaic acid, protocatechuic acid, tetradecanoic acid, sebacic acid, pentadecanoic acid, 2,4,6-tris(1,1-dimethylethyl phenol, undecadioic acid, trimethylsilyl ester palmitelaidic acid, palmitic acid, phytol, (2E)-3,7,11,15-tetramethyl-2-hexadecenyl trimethylsilyl ether, dodecanedioic acid, linoleic acid, α-linolenic acid, octadecanoic acid, eicosanoic acid, 2-monopalmitoylglycerol trimethylsilyl ester, 1-monopalmitin trimethylsilyl ester, docosanoic acid, 9-octadecenoic acid, 1,3-bis-(OTMS)-2-propyl ester, squalene, trimethylsilyl ester tetracosanoic acid, heptacosane, O-trimethylsilyl-(+)-α-tocopherol, β-sitosterol and β-amyrin | [42] |
Table 3.
Phytoconstituents of Aloe species detected by high-performance liquid chromatography and thin-layer chromatography (TLC).
| Aloe Species | Phytochemicals | Reference |
|---|---|---|
| Leaves | ||
| A. bakeri | Dihydroisorhamnetin | [46] |
| A. bellatula | Flavonoids | [46] |
| A. boylei | Isovitexin | [46] |
| A. chortolirioides var. chortolirioides | Aloesin, nataloin A and B, and 7-hydroxyaloin | [46] |
| A. chortolirioides var. wooliana | Isovitexin, aloesin, aloin A and B, and 7-hydroxyaloin | [46] |
| A. christianii | Homonataloin A and B, aloeresin A, and nataloin A and B (anthrones) | [46] |
| A. ciliaris | Isovitexin and aloeresin A | [46] |
| A. commixta | Isovitexin | [46] |
| A. ecklonis | Isovitexin | [46] |
| A. glauca | Isovitexin, trace of dihydroisorhamnetin, and aloesin (a type of chromone) | [46] |
| A. hlangapies | Isovitexin | [46] |
| A. humilis | Isovitexin, dihydroisorhamnetin | [46] |
| A. inconspicua | Isovitexin | [46] |
| A. inyangensis | Isovitexin | [46] |
| A. kraussii | Isovitexin | [46] |
| A. linearifolia | Isovitexin | [46] |
| A. lineate | Dihydroisorhamnetin | [46] |
| A. macra | Phenols, saponins, tannins, alkaloids, anthraquinones, terpenes, coumarins, and flavonoids in traces amount in comparison to A | [41] |
| A. minima | Isovitexin | [46] |
| A. nubigena | Isovitexin | [46] |
| A. parviflora | Isovitexin | [46] |
| A. polyphylla | Isovitexin and nataloin A and B | [46] |
| A. pratensis | Aloesin | [46] |
| A. pretoriensis | Isovitexin and dihydroisorhamnetin | [46] |
| A. purpurea | 3-O-caffeoylquinic acid, aloesin, 4-O-p-coumaroylquinic acid, isoorientin pentoside, vitexin/isovitexin hexoside, vitexin/isovitexin pentoside, vitexin/isovitexin, aloin, 2″-O-trans-p-coumaroylaloenin, aloin B, aloeresin A, malonylnataloin, and aloeemodin dianthrone di-O-hexoside | [47] |
| A. saundersiae | Isovitexin | [46] |
| A. soutpansbergensis | Isovitexin | [46] |
| A. striatula | Aloeresin A and homonataloin A and B (chromones) | [46] |
| A. suprafoliata | Isovitexin, aloin A and B, and nataloin A and B | [46] |
| A. suzannae | Isovitexin, apigenin, and naringenin | [46] |
| A. tenuior | Isovitexin and homonataloin A and B | [46] |
| A. thompsoniae | Isovitexin | [46] |
| A. thorncroftii | Isovitexin and dihydroisorhamnetin | [46] |
| A. tidmarshii | Isovitexin | [46] |
| A. vaotsanda | Naringenin, dihydroisorhamnetin, aloesin, aloin A and B | [46] |
| A. verecunda | Isovitexin | [46] |
| A. vossii | Isovitexin | [46] |
Table 4.
Phytoconstituents of Aloe species extracted with different methods.
| Aloe Species | Investigated Methods | Phytochemicals | Reference |
|---|---|---|---|
| Leaves | |||
| A. adigratana | Solvent increasing polarity-gel extraction | Alkaloids, flavonoids, tannins, polyphenolic, glycosides, terpenoids, steroids, carbohydrates, amino acids, and proteins | [48] |
| A. arborescens | TLC pre-coated plates | Barbaloin, aloeresin, and aloenin | [28] |
| Colorimetric assay, triple quadrupole and time-of-flight mass spectrometry, UPLC/Q-ToF high resolution mass spectrometry | Chromones (aloesin, aloesone, 8-C-glucosyl-noreugenin, aloeresin E, and 7-hydroxy-2,5-dimethylchromone); anthrones (aloin, aloe-barbendol, and aloesaponarin II); phenolic naphthalene (feroxidin); phenolic dimer (feralolide); flavonoids (naringenin, isovitexin, isorhamnetin, daidzenin, and genistein), and hydroxycinnamic acids (feruloylquinic acid, sinapic acid, chlorogenic acid, ferulic acid, and caffeic acid) | [49] | |
| Phytochemical screening | Flavonoids, terpeneoids, and aromatic compounds | [50] | |
| A. barbadensis | Colorimetric assay | Glucose, galactose, mannose, and arabinose | |
| GC-IT-MS; UPLC-Q-ToF-MS | Alanine, valine, succinic acid, arabitol, malic acid, pyroglutamic acid, aspartic acid, γ-aminobutyric acid, arabinose, fructose, glucose, glucuronic acid, sucrose, aloesin, homonataloside, 7-hydroxy-8-O-methylaloin, 7-hydroxyaloin B, 7-hydroxyaloin A, nataoemodin, aloeresin A, aloin B, isoaloeresin D, 7-O-methylaloeresin A, aloin A, 6′-malonylnataloin B, and 6′-malonylnataloin A | [51] | |
| Recrystallization, semi-preparative HPLC, or column chromatography | Chrysophanol, aloe-emodin, 7-hydroxy-2,5-dimethylchromone, 5-(hydroxymethyl)-7- methoxy-2-methyl chromone, saiko-chromone A, 5-((4E)-2′-oxopentenyl)-2-hydroxymethylchromone, 7-hydroxy-5-(hydroxymethyl)-2-methylchromone, aloenin aglycone, 5-((S)-2′-oxo-4′-hydroxypentyl)-2-hydroxymethylchromone, aloenin-2′-p-coumaroyl ester, 10-hydroxyaloin B, 10-hydroxyaloin A, isoaloeresin D, aloin B and A, aloesin, 8-C-glucosyl-I-aloesol, 8-C-glucosyl-7-O-methyl-(S)-aloesol, 10-O-β-d-glucopyranosyl aloenin, 5-((S)-2′-oxo-4′-hydroxypentyl)-2-(β-glucopyranosyl-oxy-methyl)-chromone, and aloenin B | [52] | |
| LCMS-IT-TOF; HPLC-DAD | Chromones (aloesin, 8-C-glucosyl-I-aloesol, 8-C-glucosyl-7-O-methyl-(S)-aloesol, isoaloeresin, 5-((S)-2′-oxo-4′-hydroxypentyl)-2-(β-glucopyranosyl-oxy-methyl) chromone, and 5-((S)-2′-oxo-4′-hydroxypentyl)-2-methoxychromone); phenyl pyrones (10-O-β-d-glucopyranosyl aloenin and aloenin-2′-p-coumaroyl ester); anthrones (aloin A and aloe-emodin), and naphthalene derivative (aloveroside B), aloesin, 8-C-glucosyl-I-aloesol, 8-C-glucosyl-7-O-(S)-methyl-aloesol, 10-O-β-d-clucopyranosyl aloenin, 5-((S)-2′-oxo-4′- hydroxypentyl-2(β-glucopyranosyl-oxy-methyl)chromone, 5-((S)-2′-oxo-4′-hydroxypentyl)-2-methoxy chromone, aloenin, 10-hydroxyaloin B, 10-hydroxyaloin A, aloveroside B, aloenin B, isoaloeresin D, aloin B, aloin A, aloenin-2′-p-coumaroyl ester, (E)-2-acetonyl-8-[(2″-O-cinnamoyl)-β-d-glucopyranosyl-7-methoxy-5-methylchromone, aloinoside B, aloinoside A, (E)-2-((S)-2-hydroxypropyl)-8-(2′-O-OCH3-cinnamoyl)-β-d-glucopyranosyl-7-methoxy-5-methyl-chromone, and aloe-emodin | [53] | |
| Phytochemical screening | Alkaloids, terpenoids, steroids, flavonoids, tannins, and reducing sugars | [54] | |
| Colorimetric assay, triple quadrupole and time-of-flight mass spectrometry, UPLC/Q-ToF high-resolution mass spectrometry | Chromones (aloesin, aloesone, 8-C-glucosyl-noreugenin, and aloeresin E); anthrones (aloin, aloe-barbendol, and aloesaponarin II); phenolic naphthalene (feroxidin); phenolic dimer (feralolide); flavonoids (isovitexin and isorhamnetin; isoflavones (daidzein and genistein); hydroxycinnamic acids (chlorogenic acid, ferulic acid, and caffeic acid) | [49] | |
| A. calidophila | TLC, IR, MS, 1H NMR, and 13C NMR | Aloinoside, aloin, and microdontin | [55] |
| A. ferox | VLC fractionation, silica gel chromatography | Aloe emodin, chrysophanol, and aloin A | [56] |
| Solvent partitioning and chromatography | Aloe-emodin, p-hydroxybenzaldehyde, p-hydroxyacetophenone, pyrocatechol, 10-oxooctadecanoic acid, 10-hydroxyoctadecanoic acid, methyl 10-hydroxyoctadecanoate, 7-hydroxy-2,5-dimethylchromone, furoaloesone, and 2-acetonyl-8-(2-furoylmethyl)-7-hydroxy-5-methylchromone | [57] | |
| Phytochemical screening | Flavonoids, condensed tannins, and gallotannins | [58] | |
| Phytochemical screening | Phenols, flavonoids, flavonols, proanthocyanidins, tannins, alkaloids, and saponins | [59] | |
| Fractionation, chromatography | Aloe emodin, aloin A, aloin B, desoxyaloin, aloinoside B, aloinoside C, aloinoside D, aloenin aglycone, feroxidin, 7-hydroxy-5-(hydroxymethyl)-2-methylchromone, 5-methylresorcinol, aloe resin D, 7-O-methylaloesinol, aloeresin G, C-2′-decoumaroylaloeresin G, 5-((S)-2′-oxo-4′-hydrosypentyl)-2-hydroxymethylchromone, aloveroside A, and aloenin B | [60] | |
| A. greatheadii var. davyana | Solvent fractionation, GC-MS | Alkaloids (hypoxanthine), polyphenols/phenolic compounds (phenol, 4-ethylphenol, cholestenol, homovanilic, gentisic, 6,7-dihydroxycoumaric, o-hydroxycinnamic, protocatechuic, 3,4-dihydroxyphenylacetic, syringic, sinapic, caffeic, isoferulic, ferulic, benzoic, phenylacetic, 2-methoxybenzoic, o-toluic, phenylpropionic, 4-phenyllactic, 4-hydroxybenzoic, 2,3-dihydrobenzoic, 4-hydroxyphenylacetic, hydro-p-coumaric, and p-coumaric); phytosterols (cholestenol, campesterol, â-sitosterol, and stigmasterol) | [44] |
| A. lomatophyllloides | LC-UV-MS/MS | 3-O-Caffeoylquinic acid, 4-O-p-coumaroylquinic acid, isoorientin pentoside, isoorientin, vitexin/isovitexin hexoside, vitexin/isovitexin pentoside, vitexin/isovitexin, aloin or nataloin isomer, aloin B, aloin A, aloeresin A, malonylnataloin, and aloeemodin dianthrone di-O-hexoside | [47] |
| A. macra | LC-UV-MS/MS | 3-O-Caffeoylquinic acid, aloesin, 4-O-p-coumaroylquinic acid, vitexin/isovitexin hexoside, isoorientin pentoside, isoorientin, vitexin/isovitexin hexoside, vitexin/isovitexin pentoside, vitexin/isovitexin, aloin, 2″-O-trans-p-coumaroylaloenin, aloin B, aloin A, aloeresin A, and malonylnataloin | [47] |
| A. marlothii | FCC, TLC | 7-O-methylaloeresin A, 5-hydroxyaloin A 6′-O-acetate, and 5-hydroxyaloin A | [61] |
| A. rupestris | FCC, TLC | 7-O-methylaloesin and aloesin | [61] |
| A. sabaea | Phytochemical screening | Glycoprotein | [62] |
| A. striata | Phytochemical screening | Flavonoids, terpeneoids, and aromatic compounds | [50] |
| A. tormentorii | LC-UV-MS/MS | Aloesin, 4-O-p-coumaroylquinic acid, vitexin/isovitexin hexoside, isoorientin pentoside, isoorientin, vitexin/isovitexin hexoside, vitexin/isovitexin pentoside, vitexin/isovitexin, aloin or nataloin isomer, 2-O-trans-p-coumaroylaloenin, aloin B, aloin A, aloeresin A, malonylnataloin, aloeemodin dianthrone di-O-hexoside, and microdontin A or B | [47] |
| A. trichosantha | TLC | Aloin A/B and aloin-6′-O-acetate A/B | [63] |
| A. vera | Phytochemical screening | Steroids, terpenoids, carotenoids, anthraquinones, catechin, and tannins | [64] |
| Phytochemical analysis | Alkaloids, glycosides, reducing sugars, phenolic compounds, steroids, terpenoids, flavonoids, tannins, and saponin glycosides | [65] | |
| LC-UV-MS/MS | 3-O-Caffeoylquinic acid, aloesin, 4-O-p-coumaroylquinic acid, vitexin/isovitexin hexoside, isoorientin, vitexin/isovitexin hexoside, vitexin/isovitexin pentoside, vitexin/isovitexin, aloin, 2″-O-feruloylaloesin, 7-O-methylaloeresin A, aloin B, aloin A, malonylnataloin, and microdontin | [47] | |
| Chromatography | Aloeresin G, isoaloeresin D, aloeemodin, babarloin A, 8-O-methyl-7-hydroxyaloin B, elgonica-dimer A, elgonica-dimer B, feralolide, hopan-3-ol, β-sitosterol, and daucosterol | [66] | |
| Solvent fractionation, TLC, GC-MS | Pyrocatechol, cinnamic acid, p-coumaric acid, and ascorbic acid | [67] | |
| Roots | |||
| A. pulcherrima | Fractionation, column chromatography | Chrysophanol, aloesaponarin II, and aloesaponarin I | [68] |
| A. megalacantha | Column chromatography | Chrysophanol, helminthosporin, and methyl 26-O-feruloyl-oxyhexacosanoate; asphodelin, aloesaponarin III, and 10-(chrysophanol-70-yl)-10-hydroxychrysophanol-9-anthrone; aloesaponarin I, aloesaponarin II, 4,7-dihydroxy-5-methylcoumarin, 1,8-dimethoxynepodinol, and aloe emodin; 10-O-methylchrysalodin and chrysalodin, aloesaponol | [69] |
| Whole Plant | |||
| A. turkanensis | Phytochemical screening | Tannins, anthraquinones, terpenoids/steroids, saponins, and alkaloids | [70] |
| A. barberae | TLC | Aloin and chrysophanol | [71] |
| Leaves and roots | |||
| A. arborescens var. natalensis | Silica gel chromatography, TLC, GC-MS | Aloe-emodin, barbaloin, 2″,-O-feruloylaloesin, aloenin, aloesin, succinic acid, d-glucose, fatty acid methyl esters, n-triacontanol, n-dotriacontanol, and â-sitosterol | [72] |
UPLC/Q-Tof: ultra-performance liquid chromatography quadrupole time-of-fligh; IT: ion trap; DAD: diode-array detection; VLC: vacuum liquid chromatography; LC-UV-MS/MS: liquid chromatography with ultraviolet detection and tandem mass spectrometry; FCC: flash column chromatography.
Table 5.
Phytoconstituents of Aloe species extracted with non-specified methods.
| Aloe Species | Phytochemicals | Reference |
|---|---|---|
| Leaves | ||
| A. aageodonta | 7-O-Methylaloesin, aloeresin D, aloin A, aloin B, aloinoside A, aloinoside B, microdontin A, and microdontin B | [33] |
| A. barbadensis | Cycloartenol, 24-methylene-cycloartanol, lophenol, 24-methyl-lophenol, and 24-ethyl-lophenol | [73,74,75] |
| Anthraglycosides, sugars, cardiotonic glycosides, mucilages, pectin, sterols type Δ5, anthraquinones, saponins, sterols, and triterpenoids | [76] | |
| A. castanea | 6′-O-Coumaroylaloesin | [77] |
| A. claviflora | Oxanthrone, 10-hydroxyaloin B 6′-O-acetate | [78] |
| A. excelsa | Aloe-emodin and aloin A | [79] |
| Aloctin A and aloctin B | [80] | |
| 1,8-Dihydroxy-3-methylanthracenedione (chrysophanol), | [79] | |
| A. ferox | Aloeresin D (a C-glucosylated 5-methylchromone), feroxidin (1-methyltetralin derivative), and feralolide (a dihydroisocoumarin) | [81,82,83] |
| 5-Hydroxy-3-methylnaphtho[2,3-c]furan-4(9H)-one, 5-hydroxy-3-methylnaphtho[2,3-c]furan-4,9-dione, and 5-hydroxy-3-methylnaphtho[2,3-c]furan-4(1H)-one | [84] | |
| A. microstigma | 5-Hydroxyaloin A and microstigmin A, | [85] |
| A. nyeriensis | Aloesin, 7-O-methylaloesin, aloenin, aloeresin D, aloin B, and aloin A | [34] |
| A. purpurea | Phenols and trace amounts of saponins, tannins, alkaloids, anthraquinones, terpenes, coumarins, and flavonoids | [41] |
| A. rabaiensis | Aloe-emodin-11-O-rhamnoside, aloe-emodin anthrone-10-C-glucoside, aloe-emodin anthrone-10-C-rhamnoside, aloeresin D, and rabaichromone | [86] |
| A. rubroviolacea | Phytosterols (cholesterol, 24-methylcholesta-5,22-dien-3β-ol, campesterol, campestanol, stigmasterol, 15holesteno, and sitostanol); anthraquinones (aloin A and aloe-emodin); anthrone-anthraquinones (elgonica A and elgonica B); C-glycosyl chromones (8-C-glycosyl-(2’-O-cinnamoyl)-7-O-methylaloediol B, aloeresin E, and 8-C-glycosyl-7-O-methyl-I-aloesol) | [87] |
| A. sabaea | Coniine, γ-coniceine, N-4′-chlorobutylbutyramide, and N,N-dimethylconiine | [88] |
| A. vera | Tannins, saponins, and flavonoids | [89] |
| β-sitosterol | [25] | |
| Roots | ||
| A. berhana | Aloesaponol I, laccaic acid D methyl ester, aloesaponol III, aloesaponarin I, chrysophanol-8-methyl ether, chrysophanol, and aloechrysone | [90] |
| Stems | ||
| A. saponaria | Aloesaponarin I, aloesaponarin II, desoxyerythrolaccin, helminthosporin, isoxanthorin, and laccaic acid D methyl ester, aloesaponol III, aloesaponol IV, chrysophanol, helminthosporin, and isoxanthorin | [91] |
| Flowers | ||
| A. perryi | Glycosides, phytosterols, proteins, and amino acids, flavonoids, phenols, and carbohydrates | [92] |
| Leaves and roots | ||
| A. hijazensis | Aloe-emodin, emodin, chrysophanol, aloesaponarin II, 3-methyl ether, ziganein, ziganein-5-methyl ether, aloesaponarin I, chrysophanein, feralolide, 4,7-dichloro-quinoline, lupeol, aloin, aloenin, ethylidene-aloenin, aloenin B, quercetin, kaempferol, cosmosiin, isovitexin, cinnamic acid, caffeic acid, and ferulic acid | [93] |
| A. arborescens var. natalensis | 2′-O-p-Coumaroylaloesin and 2′-O-feruloylaloesin | [94] |
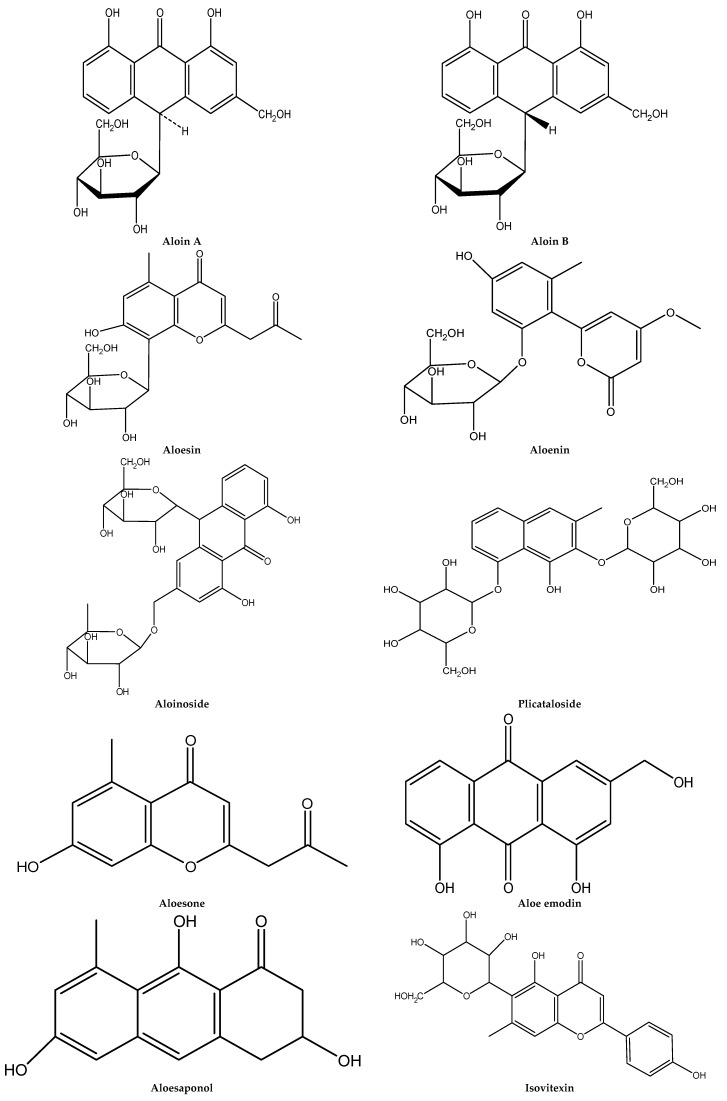
The chemical structure of main Aloe species phytochemicals is represented in Figure 1.
Figure 1.
The chemical structures of the main phytochemicals of Aloe species.
4. Traditional Medicine Use of Aloe Plants
This section summarizes the traditional use of Aloe plants for treating various ailments from different parts of the world. Among 446 Aloe species, belonging to the Xanthorrhoeaceae family, Aloe vera (L.) Burm. f., also known as A. barbadensis Mill., is the most commonly used species in traditional medicine in Indian subcontinent. Other species reported to be used are A. arborescens, A. littoralis, and A. pirottae. Akaberi et al. [95] provided the most recent review of the Aloe species’ therapeutic effects in traditional and modern medicine. Gastrointestinal activities, hepatoprotective properties, and beneficial effects against skin problems, such as wounds, injuries, and infective diseases, are among the most frequently reported Aloe species properties [95].
Most of the Aloe plants usage reports are documented from Asia (India and Nepal), and a few exist from other parts of the world, mostly from Africa through ethnomedicine studies. A. vera is commonly called Ghiu kumari in India and Nepal.
As previously introduced, the most widely used part of Aloe is the leaf. The most commonly used part is leaf gel, which is effective for treating cuts and burns, gastrointestinal disorders, and maintaining blood pressure. Jelly obtained from the leaf is used to treat cuts, burns, and other skin complaints in the Indian subcontinent [96,97,98,99,100]. It is also eaten by people suffering from high blood pressure, gastritis, and stomach-related diseases [96]. In Sikkim-India, A. vera is used for its antihyperglycemic effect [101]. The A. vera purgative property is also documented in the Sikkim government database [99].
Sushen et al. [102] have documented the extensive uses of A. vera in the traditional health care system in India. They report that juice preparation is used for sunstroke; leaf gel is useful to treat gastric intestinal problems, such as indigestion, candidiasis, constipation, diarrhea, colitis, and digestive issue relief, such as heartburn and irritable bowel syndrome. Chewing A. vera leaf or massaging on gums with an index finger gently using its gel will cure bleeding gums and toothache; it can also be used to treat menstrual cramps; gel mixed with a pinch of patika (alum, potassium aluminum sulfate) and put on a cloth can be put on eyes to cure eye problems. Leaf gel has several use reports. Leaf gel powder is mixed with raw turmeric juice, and a few drops is put into the ear and nose three to four times a day to reduce infections. Leaf gels are also mixed with a pinch of dried turmeric powder, a pinch of powdered dried seeds of bitter gourd, and a little sugar to make it sweet, and taken two times a day. It is also mixed with a few drops of raw garlic juice and a pinch of dried turmeric powder to make a homogeneous paste, and two to three spoons are taken three times a day for diarrhea; gel is used for uterine cancer and cervical cancer; it is also used for constipation, rectal infection, and ulcers. Several other leaf gel uses have been documented, and some other A. vera uses include: lowering cholesterol in blood; for miscarriage and anti-abortive treatment; treating arthritis, joint pains, body pains, and muscle pain; increasing potentiality and sperm count; treating heart disease, depression, stress release, anger management, stability management, and so on. Also reported is for cuts and wounds, white hair reduction, hair fall, ticks, mites, dandruff, baldness, grey hair, dry split hair, etc. In India, it is also used for piles, lower abdomen pain, migraine, breast pain, tuberculosis, stomach ulcers, heartburn, indigestion, dysentery, sexually transmitted infections, endometriosis, fibroids presence in uterus, gonorrhea, etc. Pimples and achiness are also treated with A. vera. Protection from ultraviolet (UV) irradiation, post-operative care, stretch marks, learning and memory improvement, cancer, diabetes, hepatitis, AIDS, and weight loss are other uses of Aloe leaf gel.
Leaves are also chewed to cure skin and uterine disorders and treat jaundice in Nepal [103,104,105]. In India, leaves are used for stomachic, tonic, purgative and anthelmintic purposes; juice is put on the head in high fever to reduce body temperature [106]. Leaf juice is also applied on fresh burns. Juice is also given to diabetic patients and for urinal troubles [105]. The Limboo tribe of Sikkim use leaf juice on burnt wounds, which also helps cool pain [107]. Whole plant juice, pulp, or paste is used as a remedy in intestinal worms in children, as well as a hepatic stimulant, stomachic, and liver and spleen enlargement [108].
Leaf juice is given for a stomachache and as a tonic [109]. Juice is also commonly used in case of constipation [109,110]. Leaf juice given in case of indigestion, hemorrhoids, and peptic ulcers [111]. Juice is also used in rheumatic pains, fever, jaundice, menstrual disorder, suppression, and gonorrhea, and juice is applied locally for burns and skin irritation [101].
Leaf pulp is also taken to treat dysentery [112] and other stomach disorders in Nepal [113]. It is used to cure burn wounds and regulate menstruation, constipation, and ascariasis [99]. The use of A. vera as an emmenagogue is also reported from Panchthar Nepal [97]. Leaf is used in catarrh, cough, and overheating problems [114], and Aloe species leaf gel, including A. vera, is also used for diabetes [115,116,117].
A. vera is also used to treat fresh and bleeding or infected wounds, burns, eczema, and dandruff in Mexico [118]. It is also used to treat HIV in South Africa [119,120]. Pulp and juice obtained from A. arborescens is used on dermatosis and against articular pains in Italy [121].
A. littoralis is used to treat Bilharzia in the traditional health care system of Namibia [122]. Another species reported to be used in traditional medicine from Africa is A. pirottae, but its detailed use is not mentioned [123].
5. Food Preservative Applications of Aloe Plants
Nowadays, the food industry looks for new sources of natural compounds with different properties [124,125,126,127,128,129,130,131,132]. It is considered that, through the plant kingdom, Aloe species, especially A. vera, is one of the most applied medical plants worldwide [133]. These plants have been used in folk medicine from different therapeutic purposes, due to its purgative effect, for skin disorder healing and beauty treatments. Numerous reports show that the Aloe leaf possesses a wild spectrum of activities, including, anticancer, antioxidant, anti-inflammatory, immunomodulatory, hepatoprotective, antiulcer, and antidiabetic as well as found application in dermatology, to treat radiation-caused skin conditions and in gastroenterology or gynecology as a bactericidal, viricidal, or fungicidal. The widespread use of this plant is the result, inter alia, of the content of approximately 200 biologically active compounds, as previously introduced, characterized by a synergistic effect. In cosmetology, Aloe species are used in creams, soaps, and shampoos production. Not least, industrial applications of these plants include beverages, ice cream, food supplements, and others [16,30]. Despite the industrial use of plants belonging to the Aloe genus, previous studies of antimicrobial properties are mainly directed toward isolates obtained from human skin. Undoubtedly, these plants are characterized by their natural antimicrobial potential, and their use in food production.
6. Antimicrobial Activity
6.1. Antibacterial Activity
In vitro studies have shown that A. vera is characterized by activity against Gram-negative and Gram-positive bacteria. Petroleum ether, dichloromethane, and water extracts of upper stem, young bark, mature bark, leaves and roots of A. barberae from South Africa were evaluated for their antimicrobial activity against Gram-positive (Bacillus subtilis, Staphylococcus aureus) and Gram-negative (Escherichia coli, Klebsiella pneumoniae) bacteria [71]. Petroleum ether and dichloromethane extracts of mature bark, leaves, and roots exhibited significant activity against all bacteria, with minimum inhibitory concentrations (MIC) ranging from 0.195 mg/mL to 1.56 mg/mL. In another study, the authors evaluated the antimicrobial properties and phenolic contents of medicinal plants used by the Venda people. It was found that A. chabaudii roots exhibited low levels of phenolic compounds as also weak antimicrobial activities against B. subtilis, S. aureus E. coli, and K. pneumoniae [134]. Generally, it is believed that A. vera acetone extracts exhibit stronger activity against S. aureus, Streptococcus pyogenes, Pseudomonas aeruginosa, and E. coli compared to aqueous or ethanol extracts. Lawrence et al. [67] documented the antibacterial property of A. vera gel extracted using different solvents. They found differences between the extract activities against S. aureus, S. pyogenes, B. subtilis, E. coli, Ps. aeruginosa, K. pneumoniae, Salmonella typhi, and Bacillus cereus. In general, the results of the agar well diffusion method showed that the inhibition zones ranged from 12.66 mm (E. coli) to 23.33 mm (B. cereus). On the other hand, methanol extract exhibited the strongest activity against B. cereus (22.33 mm) followed by S. pyogenes (15 mm), and the least for S. typhi (9.66 mm). Finally, according the results obtained in their research, acetone extract gave the lowest values of inhibition zones, ranging from 6.00 mm (E. coli) to 7.33 mm (S. pyogenes). What is more, no differences between acetone and controls were noted for P. aeruginosa and S. typhi. In general, it is well noted that plant extracts show greater antibacterial activity against Gram-positive than Gram-negative bacteria [135]. Also, in the study of Ferro et al. [136], Gram-positive bacterium S. pyogenes was more susceptible to A. vera gel than Gram-negative Shigella flexneri. The effective growth inhibition was achieved with aloe concentrations of more than 100 mg/mL for S. flexneri and 25 mg/mL for Streptococcus pyogenes. The authors found that sap extract was more effective than leaf extract against E. coli, B. subtilis, S. aureus, and P. aeruginosa. Sap water extract (100 µg/mL) showed the strongest inhibitory properties against B. subtilis and P. aeruginosa. Jonson et al. [137] studied antibacterial activity of leaf extract from Aloe vera, Datura stromonium, Pongamia pinnata, Lantona camara, and Calotropis procera. They found that from all of the tested alcoholic and aqueous extracts, A. vera showed the strongest activity against E. coli and S. aureus. What is more, aloe polysaccharides were used in tea tree or palmarosa essential oil combinations as a natural strategy against Xanthomonas fragariae (bacterial angular leaf spot disease, which is an important strawberry disease responsible for significant yield losses) [138]. It was found that these preparations reduce disease severity and activate plant defenses, and that Aloe polysaccharides alone reduced X. fragariae growth by up to 44%. The authors concluded that tested essential oils and polysaccharides from aloe can be considered as potential agents for plant disease control and could play a significant role in product formulation for strawberry leaf spot control. The essential oils into aloe polysaccharide preparation contributed more effectively to reduce the disease severity, either by its antimicrobial activity or by the plants’ defense mechanism activation. The antimicrobial activities of A. vera juice were tested in the work of Alemda and Agaoglu [139].
In the work of Dharajiya et al. [140], A. barbadensis leaf extract antibacterial activity was evaluated against E. coli, P. aeruginosa, B. cereus, and Serratia marcescens. They found maximum inhibitory activities against S. marcescens (hexane extract) and B. cereus (methanol extract). In general, the authors noted that methanol extract showed an inhibitory effect against all of the tested bacterial strains, while ethyl acetate extract showed no inhibitory activities. Similar results of antibacterial activity against E. coli, B. subtilis, S. epidermidis, and S sonnei were obtained by Coopoosamy and Magwa [79]. They found that the MIC of emodin and aloin A ranged from 62.5 mg/mL against B. subtilis and E. coli to 250 mg/mL against S. epidermidis and S. sonnei [79,141]. A. vera sap and leaf extracts were investigated for antimicrobial properties by Abakar et al. [142]. The disc diffusion method revealed that juice inhibits Mycobacterium smegmatis, K. pneumoniae, Enterococcus faecalis, Micrococcus luteus, and Bacillus sphericus growth. They concluded that the juice obtained from aloe can be used for antimicrobial activity in cosmetics, pharmacy, and the food industry. S. mutans growth inhibition was subject of investigation by Jain et al. [143]. The authors used crude, organic solvent-based and aqueous extracts from A. vera leaves, neem (Azadirachta indica), tulsi (Ocimum tenuiflorum), amla fruits (Emblica officinalis), garlic cloves (Allium sativum), and ginger rhizomes (Zingiber officinale). The MIC results determined by the agar well diffusion method showed that 25 mg/mL of organic solvents extract inhibited tested bacterium growth. On the other hand, the MIC values for aqueous extract equaled 50 mg/mL. It is worth noting that the organic solvent extract activity from aloe was comparable to garlic and alma. The antibacterial activity of polysaccharides from Aloe spp. has been attributed to phagocytic leucocytes stimulation to destroy bacteria. A. vera compounds with particular antimicrobial activity are saponins, acemannan, and anthraquinones derivatives [144]. Aloe-emodin effect on Helicobacter pylori N-acetyltransferase activity showed dose-dependent inhibition [145]. Cellini et al. [146] attributed H. pylori inhibition to the polysaccharides that are present in gel, exhibiting an anti-adhesive effect. A. vera aqueous extract effect on E. coli morphological and physiological properties were described by Kargaran et al. [147]. They found that the aloe extract MIC value equaled 2.23 mg/mL. What is more, another aloe plant—A. ferox—is known to show activity against wild bacteria. A. ferox-isolated compounds (aloe emodin, chrysophanol, and aloin) activity were investigated by Kambizi et al. [56]. They found that aloe emodin and alonin A exhibit inhibitory activities against B. cereus, B. subtilis, S. aureus, E. coli, Staphylococcus epidermidis, and Shigella sonnei. Chrysophanol was characterized by weaker antibacterial action, inhibiting B. subtilis, S. epidermidis, and E. coli strains. On the other hand, pyrocatechol, 2-vinyl crotonaldehyde, ascorbic acid, p-coumaric acid, and cinnamic acid isolated from plant have shown a wide spectrum of antibacterial activity [148].
Radi et al. [149] evaluated the effect of gelatin coating incorporated with A. vera gel and green and black tea extracts on the physicochemical, microbial, and sensorial properties of fresh-cut oranges stored at 4 °C for 17 days. They noted that coating materials with gelatin incorporated with A. vera and green tea extracts successfully retarded microbial growth and extended shelf life during storage. Chen et al. [150] showed that the antimicrobial activities of composite films increased as the amount of aloe gel powder used in composite films increased. The average area of inhibitory zones of Citrobacter freundii, Escherichia coli, Enterobacter aerogenes, Serratia marcescens, S. aureus, and B. cereus for films with aloe⁄gelatin (1:4) and aloe⁄gelatin (4:1) compositions were 1.63 ÷ 2.38 mm and 3.82 ÷ 4.80 mm, respectively. A. vera potential application as an edible coating was provided by Benítez et al. [151]. They found significant microbial population reduction in fresh-cut kiwifruit treated with 15% A. vera during 11 days of storage. The results at the last day of analysis were 4.97 log CFU (colony-forming units)/g for 15% aloe and 5.75 log CFU/g for control. What is more, they found that A. vera can be used as a coating to both extend postharvest shelf life and maintain product sensory properties through the storage period [152]. Similar results were obtained by Sogvar et al. [153] on aloe coatings that have been used to maintain the quality of postharvest strawberry fruits. The application of aloe and 5% of ascorbic acid reduced the mesophilic bacteria population from 3.63 log CFU/g for control to 3.13 log CFU/g.
6.2. Antifungal Activity
Aloe species’ availability, safety, and bioactivity make them an interesting alternative as control agent used in preharvest and postharvest fungal diseases of fruits and vegetables. Studies showed that A. vera reduces Penicillium, Botrytis, and Alternaria spore survival by up to 20% [154], as well as inhibits Fusarium, Rhizoctonia, and Colleotrichum mycelium growth by up to 38% [155]. What is more, in the work of Castillo et al. [156], it was reported that A. vera gel inhibits Penicillium digitatum and Botrytis cinerea. A. vera gel was analyzed as an antifungal agent against six fungi causing plant diseases: Fusarium oxysporum, Alternaria alternate, Colletotrichum gloeosporioides, Bipolaris spicifera, Curvularia hawaiiensis, and Botryotinia fuckeliana. It was found that gel was most effective against F. oxysporum [157]. The authors found that films with the highest A. vera ratio were effective in controlling fungal contamination. Nectarine treated with A. vera gel alone, or with the addition of thymol, inhibited the fungal growth of inoculated Rhizopus stolonifer, Botrytis cinerea, and Penicillium digitatum. Therefore, Aloe application led to a significantly lower fungal infection (two to threefold) than in non-treated nectarines. It was found that the addition of thymol did not generally improve the aloe gel efficacy to reduce infection [158]. In the work of Vieira et al. [159], chitosan and A. vera liquid fraction coatings presented the best uniformly coat blueberry surface characteristics. The authors showed that the microbiological growth of Botrytis cinerea was reduced by 42% in coated blueberries after 25 days. Overall, coatings extended the shelf life of blueberries for five days (compared with the control sample), demonstrating that a chitosan and A. vera combination shows high potential in expanding shelf life. The antifungal activity from eight Aloe species gels (A. arborescens Mill., A. aristata Haw., A. claviflora Strydenburg, A. ferox Mill., A. mitriformis Mill., A. saponaria Ait., A. striata Haw., and A. vera L.) were evaluated against B. cinerea, P. digitatum, Penicillium expansum, and P. italicum [160]. The authors concluded that antifungal activity was higher for A. ferox, A. mitriformis, and A. saponaria than A. vera, which can be correlated with aloin content. Nidiry et al. [161] have also reported that aloin and aloe-emodin from A. vera could be important antifungal moieties. Guillén et al. [160] reported that A. arborescens could be even more effective than A. vera gel for preservative purposes in edible coatings, affecting climacteric fruit quality. A. vera and green tea extracts used in gelatin-based edible coating for fresh-cut oranges reduced the total fungal count [149]. A. vera coatings effectively controlled or inhibited fungal populations during strawberry storage, and therefore was considered an effective natural agent against bacteria and yeasts-associated postharvest diseases [153]. The total number of yeasts and molds obtained for fresh-cut kiwi samples coated with aloe were about 10 times lower than for the control sample. Additionally, an A. vera coating maintained fruit firmness, and prevented ascorbic acid losses and yellowing due to ripening. In contrast, fruit treated with an alginate-based coating had higher microorganism counts than the control samples [152]. Benítez et al. [151] studied the efficacy of an edible coating based on A. vera gel at different concentrations: 1% (v/v), 5% (v/v), and 15% (v/v). They found that an aloe coating reduced respiration rates and microbial spoilage in sliced kiwi fruit. After seven days of storage, yeast and molds load dropped by approximately one logarithmic unit for slices coated with 15% and 5%. Similar findings were stated by Martínez-Romero et al. [162]. In their work, an A. vera gel coating maintained ready-to-eat pomegranate arils. The authors used different aloe concentrations, as well as aloe plus ascorbic acid, and found that A. vera treatments led to significantly lower counts of both mesophilic aerobics, and yeasts and molds. What is more, aloe coatings led to firmness retention and increased the total anthocyanins and total phenolics levels. The antifungal effects of 2% (w/v) A. vera were also evaluated against Colletotrichum gloeosporioides on avocado fruit by Bill et al. [163]. According to the results, aloe showed weaker properties than thyme oil with chitosan combination. A. vera gel was evaluated for their antifungal activity in the study of Sitara et al. [164]. The authors noted that 0.35% of tested gel completely inhibited plant pathogenic fungal growth for Alternaria alternata and Drechslera hawaiensis. In comparison with the control medium, significant growth inhibition was also found in Aspergillus niger, A. flavus, and P. digitatum. Hassanpour [165] found that coating materials containing A. vera gel reduce fungal decay of raspberry fruits (Rubus spp.) during eight days’ incubation at 4 °C, without differences between different gel levels. Functional films with A. vera gel were noted to increase different papaya fruits (Carica papaya) shelf life during 15 days of storage [166]. The authors found that A. vera gel significantly inhibited papaya fruits ripping. Generally, A. vera use as a functional film component was also noted for grapes (Vitis vinifera) [167], pineapple (Ananas comosus) [168], or tomatoes [169] as well as cherry tomatoes [158].
In other studies, A. ferox methanol extract showed activity against Candida albicans with an MIC value of 20 mg/mL, while the MIC of aloin used against these yeasts equaled 5 mg/mL. On the other hand, Aloe ferox acetone extract was shown to exhibit fungicidal activity at 10 mg/mL against five fungal strains: Alternaria alternata, A. niger, Mucor hiemalis, Penicillium notatum, and Schizophyllum commune [170]. Abakar et al. [142] noted that sap water extract and A. vera leaves exhibited intermediate susceptibility against A. niger and C. albicans. Subramanian et al. [171] found that A. vera leaf gel ethanol extract showed strong activity against Aspergillus fumigatus, A. niger, A. flavus, Fusarium oxysporum, and Microsporum canis. On the other hand, A. vera fresh leaf hydroalcoholic extract showed antifungal activity against Botrytis gladiolorum, Fusarium oxysporum, and Penicillium gladioli mycelial growth [172]. A. vera gel and leaf extract activity against Trichophyton mentagrophytes, T. schoeleinii, M. canis, and Candida albicans were evaluated by Olaleye et al. [173]. In this research, only gel inhibited T. mentagrophytes growth, while leaf extract possessed inhibitory effects on C. albicans. The antifungal activity against Aspergillus niger, A. flavus, Aspergillus oryzae, Penicillium chrysogenum, and Trichoderma viride were evaluated by Dharajiya et al. [140]. Maximum inhibitory activity was found for aqueous extract against A. niger. On the other hand, methanol extract showed weak inhibitory activity against A. oryzae. Two extracts (hexane and ethyl acetate) failed to express antifungal activity against any of the fungal strains used in the study. What is more, the authors found that P. chrysogenum and T. viride were found to be resistant to the tested extracts. Das et al. [148] have reported that a protein isolated from A. vera shows antifungal activity against Candida species, specifically C. paraprilosis, C. krusei, and C. albicans. Sequencing analysis showed the isolate to be a lectin-like protein that inhibits trypsin, revealing a protease inhibitory function.
7. In Vitro and In Vivo Biological Activities of Aloe Plants
In the following subsections, different in vitro and in vivo Aloe plant species biological effects are carefully described and briefly resumed in Table 6.
Table 6.
Bioactive effects of Aloe plant species: pre-clinical (in vitro and in vivo) studies.
| Biological Activities | Observed Effects | Active Molecules | References |
|---|---|---|---|
| Wound healing and cell proliferation | Skin damage treatment, cell type proliferation stimulation, cell phagocytic activity stimulation, wound contraction rate, collagen and elastin synthesis increase, fibroblast proliferation, hyaluronic acid, and hydroxyproline production | Mannose-6-phosphate, polysaccharides, glycoproteins, saponins, acemannan | [5,33,135,174,175,176,178,179,180,184,185,186] |
| Intestinal absorption and purgative action | Drug permeability increase (opening tight junctions), intestinal water absorption reduction, mucus secretion stimulation, reduce visceral fat accumulation, reduce large-sized intestinal polyps, intestinal motility improvement | Anthraquinones (aloin, aloe-emodin, emodin), pytosterols | [5,133,188,189,190,191,192,194] |
| Anti-inflammatory and immunomodulatory | Phagocytic and prolifertive activity raise (through cyclooxygenase (COX) pathways inhibition and prostaglandins production reduction), abolish albumin gene transcription, inflammatory processes inhibition (leukocyte adhesion and pro-inflammatory cytokines production reduction), cerebral ischemia and reperfusion injury attenuation (inhibition of systemic inflammatory response, leukocyte aggregation, and lipid peroxidation) | Aloe-emodin, polysaccharides, aloesin, anthraquinones, chromones | [2,148,199,200,201,202,203,204,205,206,207,208] |
| Hepatoprotective | Morphofunctional and molecular changes reduction, protection against hepatocyte death and lipid peroxidation, liver fatty acid synthesis downregulation and oxidation upregulation, cytokine level reduction, mRNA lipogenic gene expression suppression | Aloe-emodin, anthraquinones, phytosterols (lophenol, cycloartanol) | [74,133,209] |
| Antioxidant | Free radical scavenging activity, free radicals’ generation and reactive oxygen species (ROS) production suppression, lipid peroxidation reduction, superoxide dismutase (SOD) activity raise | Aloesin, aloeresin A, and aloesone | [44,49,198,212,213,214,215,216,217,218] |
| Antibacterial, antifungal and antiviral | Phagocytic leukocyte activity stimulation, cytotoxic effects, alkalization promotion and constipation alleviation, virus replication inhibition | Emodin, aloin A, aloe-emodin, saponins, chrysophanol, acemannan, pyrocatechol, polysaccharides | [6,56,58,67,71,76,79,136,146,148,170,181,192,198,219,220,221,222,223,224,225,226,227,228,229,230,231,232,233] |
| Anticancer | Chemopreventive activity, VEGF secretion inhibition, tumor angiogenesis and angiogenic response inhibition, proliferation inhibition and endothelial cell migration, N-acetyl transferase activity and gene expression inhibition, STAT3 activation blocking, benzopyrene binding, iNOS, NFkB, and P53 activity inhibition, TNF-α, IL-1, and interferon production stimulation | Aloin, aloe-emodin, rhein, acemannan, barbaloin, physcion, chrysophanol, aloesin, diethyl hexylphthalate and an N-terminal octapeptide | [148,184,225,234,235,236,237,238,239,240,241,242,243,244,245,246,247,248,249,250,251,252,253,254,255] |
| Antidiabetic | Glucose transporter mRNA expression modulation, reduce fasting blood glucose levels, glucose transport improvement through proximal and distal marker modulation | Polysaccharides, phytosterols (lophenol, 24-methyl-lophenol, 24-ethyl-lophenol, cycloartanol and 24-methylene cycloartenol), aloe-emodin-8-O-glycoside | [37,73,74,148,183,255,256,257,258,259,260] |
| Antihyperlipidemic | Reduce visceral fat mass, total cholesterol, triglycerides, LDL and VLDL levels, glucose intolerance and lipid metabolizing enzymes improvement and abnormal estrous cyclicity reversion | Phytosterols | [261,262,263,264,265] |
| Estrogen status | Suppress breast cancer cells proliferation, estrogen receptor-α inhibition | Emodin, aloe-emodin | [52,263] |
| Antiulcer | Promote digestion, cytoprotection, dose-dependent gastric acid secretion inhibition | Plant extract | [5,266,267,268,269] |
| Skin use | Increase type I and type III collagen synthesis gene expression and hyaluronic acid levels, tyrosinase inhibitory activity, | Sterols, aloin, aloesin | [270,271,272,273,274,275] |
| Antiallergic | Reduce histamine release, stimulate leukotriene synthesis and secretion, protein kinase C and phospholipase C activities inhibition, Ca2+ influx blocking during mast cell activation | Glycoprotein | [276] |
VEGF: vascular endothelial growth factor; iNOS: inducible nitric oxide synthase; NFκB: nuclear factor κB; TNF-α: tumor necrosis factor α; IL-1: interleukin 1; LDL: low density lipoprotein; VLDL: very low density lipoprotein.
7.1. Wound Healing and Cell Proliferation
A. vera has been used for the treatment of skin damage in several cultures [174]. In vitro extracts of A. vera stimulated several cell type proliferations. In many researches, treatment with whole A. vera gel extracts resulted in faster wounds healing [175,176]. The mannose 6-phosphate present in A. vera gel is considered to be the active ingredient for wound healing [177]. Mannose 6-phosphate heals wounds by increasing cell phagocytic activity [178]. It is thought that mannose 6-phosphate increases the wound area contraction rate [179] and collagen synthesis [180]. During wound healing, the polysaccharides that are present in A. vera induce fibroblasts proliferation and hyaluronic acid and hydroxyproline production, which play an important role in extracellular matrix remodeling [5]. A class of plant growth regulators, gibberellins, which are available in A. vera, also enhance collagen and elastin formation for breaking strength improvement, by interfering with a collagen cross-link for wound contraction, reducing wrinkle formation [2,181,182,183]. Polysaccharides and glycoproteins isolated from plants were reported to have wound-healing activity [184,185]. The wound-healing activity of saponin that is present in A. vera was also reported [186]. Acemannan is considered to be a main functional component of A. vera; it is composed of a long chain of acetylated mannose [33,135,184]. Indeed, acemannan stimulates wound healing and hard tissue regeneration by inducing cell proliferation [187]. Eight Aloe species (A. arborescens, A. brevifolia, A. eru, A. ferox, A. grandidentata, A. perfoliata, A. saponaria, and A. vera) also provided significant accelerating effects on diabetic wound healing in rats following the topical application of leaf methanol extracts [36].
7.2. Intestinal Absorption and Purgative Action
Aloe products have been used for drug absorption enhancement with low bioavailability due to extensive efflux [188]. Carien et al. [188] demonstrated an increase in drug permeability in the presence of Aloe vera gel and whole leaf materials. This is thought to be attributed to the opening of tight junctions by A. vera gel and precipitated polysaccharides. Laxatives are substances that loosen stools. Aloe is also used as a laxative due to its ability to reduce intestinal water absorption. Anthraquinones that are present in plants act as potent laxatives through mucous secretion stimulation, thereby increasing intestinal water content [189]. Active anthraquinones, such as aloin, aloe-emodin, and emodin are linked to aloe purgative action [5,190]. Aloin, which is present in gel, can be metabolized by colonic flora to reactive aloe-emodin, which is responsible for purgative activity [5,133]. Five phytosterols that are present in A. vera gel are able to reduce visceral fat accumulation, and influence glucose and lipid metabolism in animal model experiments. They also reduced large-sized intestinal polyps [5]. Aloe-emodin, emodin, and rhein synergistically exerted a potentiating purgative effect on mice [191]. A. vera laxative effect was shown after 6–24 h or more from oral anthraquinone administration [192].
A. ferox is widely used for its potent laxative and cathartic effects, which are attributed to anthraquinones and in particular to aloe-emodin [193]. A. ferox leaf water extract displayed in vivo laxative effects via improved intestinal motility in loperamide-induced constipated rats [194].
In addition to its laxative properties, Aloe could strengthen the stomach, and was traditionally used as a carminative and appetizer agent. It has also been suggested for relieving stomach pain [95]. Aloe was known as a good remedy for hemorrhoids and anal disorder treatment. Clinical and experimental studies have shown that Aloe preparation administration is useful for a wide range of gastrointestinal problems. Aloe extract and a number of its compounds have been shown to ameliorate inflammation and improve clinical and histopathological colitis symptoms in animal models. Significant antiulcer and gastroprotective activities were also observed after administration of Aloe-containing preparation [95]. Aloe is thought to be a potential agent in treatment of gastrointestinal cancers [195,196].
7.3. Anti-Inflammatory and Immunomodulatory Effects
Cyclooxygenase (COX) enzymes (also known as prostaglandin-H2-synthases) act as catalysts in the production of prostaglandins (highly active pro-inflammatory mediators) from arachidonic acid (hydrolytically released from membrane phospholipids) during inflammatory processes [197]. Prostaglandin production inhibition by inhibiting COX enzymes, particularly the COX-2 enzyme (an isoform induced under pathological conditions) is one of the mechanisms of action of some non-steroidal anti-inflammatory drugs (NSAIDs) used for the symptomatic treatment of inflammation. Although different levels of activity (against COX-1 only) were reported in 51 different Aloe species [198], COX-1 isoform inhibition is not desirable, because this enzyme is largely known to be constitutively expressed in most tissues for maintaining some physiological functions [199]. Aloe administration has been demonstrated to result in phagocytic and proliferative activity raise by inhibiting COX pathways and reducing prostaglandin E2 production [200,201]. Lindsey et al. [202] reported that A. ferox methanol extract exhibited COX-1 inhibitory effects. Albumin transcription levels and tumor necrosis factor (TNF)-α genes are involved in the early phase of acute inflammatory response. In rats treated with aloe-emodin, an abolishment of albumin gene transcription was observed. TNF-α was weakly detectable in livers after aloe-emodin administration. Histological analysis showed a reduced inflammatory infiltration of the lymphocytes and Kupffer cells observed in rats treated with aloe-emodin [203]. A. vera can inhibit the inflammatory process following burn injury by reducing leukocyte adhesion and pro-inflammatory cytokine production [204]. Aloe polysaccharide pretreatment can attenuate cerebral ischemia and reperfusion injury in severe traumatic–hemorrhagic rats, through inhibiting systemic inflammatory response, leukocyte aggregation, and lipid peroxidation in the brain [205]. An acidic polysaccharide and a protein with the molecular weight (MW) of 14 kDa from A. vera have also been shown to have anti-inflammatory activity [2]. A cinnamic acid ester of aloesin found in A. vera has the ability to reduce croton oil-induced inflammation [148]. The C-glucosyl chromone isolated from A. vera gel extracts was also found to have anti-inflammatory properties [206]. The anthraquinones and chromones that are present in aloe inner gel possess strong anti-inflammatory effects in murine macrophages [200]. Fresh A. vera gel was reported for the significant reduction of acute inflammation in rats [207]. It is also reported that A. vera extract helped in decreasing inflammation by 48% in a rat arthritic inflammatory model [208].
7.4. Hepatoprotective Activity
Morphofunctional and molecular changes induced by carbon tetrachloride (CCl4) were reduced through aloe-emodin administration in rats [203]. Anthraquinone is likely to protect against hepatocyte death, lipid peroxidation, and the subsequent inflammatory response [133]. Phytosterols found in aloe, specifically lophenol and cycloartanol, have the ability to induce fatty acid synthesis downregulation and fatty acid oxidation upregulation in the liver, resulting in intra-abdominal fat reduction and hyperlipidemia improvement. An improvement in metabolic syndrome-related disorders and liver steatosis was obtained in aloe sterol-treated diabetic fatty rats. The results also showed that aloe suppressed obesity-induced inflammatory response by reducing cytokine levels [74]. A. vera gel extract can also prevent ethanol-induced fatty liver by suppressing mRNA lipogenic gene expression in the liver. Aloe gel also has the therapeutic potential to decrease cholesterol levels and cardiovascular disease risk [209]. In another study investigating A. vera extract effect on lindane (LD)-induced hepatoxicity and genotoxicity, leaf extract (1.0 mL/kg body weight, b.w.) decreased serum glutamate pyruvate transaminase (GPT), glutamate oxaloacetate transaminase (GOT), gamma-glutamyl transferase (GGT), and alkaline phosphatase (ALP) levels induced by 100 mg/kg b.w. LD [210]. In addition to A. vera, hepatoprotective activity was also reported for other Aloe genus species, including A. arborescens. A. arborescens was reported to be most active in liver diseases treatment, particularly cancers [211].
7.5. Antioxidant Effect
Free radical overproduction, including reactive oxygen species (ROS) resulting in oxidative stress, is known to be associated with the development of many diseases [226,243,277]. An antioxidant is a substance that significantly delays or inhibits oxidizable substrate oxidation at low concentrations [278]. In the literature, A. vera compounds were highlighted for their antioxidant activities [37,279,280]. It has been reported that A. vera leaf epidermis and flower methanol extracts exerted in vitro antioxidant effects [281]. Aloe gel showed free radical scavenging activity on 2,2-diphenyl-1-picrylhydrazyl (DPPH), 2,20-azinobis-(3-ethylbenzothiazoline-6-sulfonic acid) (ABTS)+•, and nitric oxide radicals [212]. A. ferox antioxidant capacity was determined using oxygen radical absorbance capacity (ORAC) and ferric reducing antioxidant power (FRAP) analyses. A. ferox antioxidant activity was attributed to its phytochemical composition. Thus, it can be used in alleviating symptoms or preventing oxidative stress-related diseases [44]. Aloeresins in A. ferox displayed strong antioxidant activity [213]. These 7-hydroxychromones, such as aloesin from an aloe extract, suppress free radical generation and reactive oxygen species (ROS) production, thereby preventing and treating ROS-mediated and other oxidative process-associated conditions [214]. Also, A. ferox leaves methanol extract showed good DPPH scavenging activity [215]. 5-Methylchromones aloesin, aloeresin A, and aloesone, which are compounds present in A. barbadensis and A. arborescens, exhibited the most radical scavenging activity by DPPH and ORAC assays [50]. The in vitro antioxidant activity of A. arborescens [94], A. ferox [44,58,59], Aloe greatheadii var. davyana [282], A. harlana [283], A. saponaria [284], A. marlothii, and A. melanacantha [285] leaf extracts were reported in the literature. Sazhina et al. [216] reported that leaf extracts from 15 Aloe species exhibited high antioxidant activity. However, the potent antioxidant activity measured in these in vitro studies needs to be followed up with appropriate in vivo assays. The absorption and bioavailability issues of such antioxidants following consumption also require investigation [198]. A protective potential of Aloe polysaccharides against 2,20-azobis(2-amidinopropane) dihydrochloride induced oxidative stress and cell death in kidney epithelial cells (Vero cells), as well as in an in vivo zebrafish model were shown [217]. Antioxidant compounds present in A. saponaria gel exerted antinociceptive and anti-inflammatory effects by the topical treatment of an ultraviolet B-induced sunburn model [286]. In another study, A. barbadensis extract displayed significant antioxidant activity in diabetic rats by increasing superoxide dismutase (SOD) enzyme activity and reducing lipid peroxidation [218].
7.6. Antibacterial, Antifungal, and Antiviral Activities
A. vera has in vitro antibacterial activity against Gram-negative and Gram-positive bacteria. Thus, it has been described as an antibacterial agent, as previously introduced. Antibacterial activity has been attributed to their polysaccharides, which trigger phagocytic leucocytes to destroy bacteria [75]. Indeed, A. vera gel extract antibacterial activity against Gram-positive and Gram-negative bacteria was showed in other studies [136,219]. An experiment proved that A. vera acetone extract was more active against S. aureus, Streptococcus pyogenes, P. aeruginosa, and E. coli compared to aqueous or ethanol extracts [6]. A. ferox is used to treat distinct infections, particularly those that are sexually transmitted, internal parasites, gonorrhoea, and syphilis in South Africa [220]. Aloe-emodin and aloin A isolated from A. ferox exhibited antibacterial activity against Bacillus cereus, B. subtilis, S. aureus, S. epidermidis, E. coli, and Shigella sonnei, while chrysophanol only led to B. subtilis, S. epidermidis, and E. coli growth inhibition [56]. Aloe-emodin and aloin A showed antibacterial activity against B. subtilis, E. coli, S. epidermidis, and S. sonnei [79]. An Aloe methanol extract and aloin had inhibitory effects against Neisseria gonorrhoeae [221]. The antimicrobial activities of 10 different South African Aloe species extracts were listed in another study [198]. Antimicrobial activities were reported for A. arborescens leaf ethyl acetate (against E. coli) [222], A. barberae root and leaf dichloromethane (against E. coli and C. albicans) [71], and A. marlothii leaf dichloromethane (against S. aureus) [223] extracts. Of particular interest are the inhibitory effects demonstrated by ethyl acetate and the methanol extracts of A. arborescens and A. striatula leaves, respectively, against ampicillin-resistant E. coli [222]. Pyrocatechol, a hydroxylated phenol that is present in A. vera, is known to have toxic effects on microorganisms [57,224]. The water and carbohydrates present in A. vera gel have very strong antibacterial potential against P. aeruginosa and mycobacterium strains, such as Mycobacterium smegmatis, Mycobacterium fortuitum, Mycobacterium kansasii, and Mycobacterium tuberculosis [192,225,226].
Aloe-emodin exerted H. pylori inhibition, which is the microorganism that is responsible for gastritis, peptic ulcer, gastric adenocarcinoma, and MALT (mucosa-associated lymphoid tissue) lymphoma [145]. In another study, A. vera gel exhibited inhibitory effects on multi-resistant H. pylori strains, with its activity being attributed to the anti-adhesive effect of gel polysaccharides [146]. Also, it was reported that A. vera inner gel has antibacterial activity against both susceptible and resistant H. pylori strains and it can be used as a natural agent for H. pylori gastric infection treatment [227].
The topical antibacterial as well as anti-inflammatory properties of aloe are embodied in a patent application of a laxative suppository preparation that is used for the treatment of hemorrhoids and bacterial infections of the anus [141].
A protein (MW 14 kDa) isolated from A. vera displayed antifungal activity against different Candida species, specifically Candida parapsilosis, Candida krusei, and Candida albicans [148]. A. vera removed Candida infections through promoting alkalization and alleviating constipation [228]. The saponins that are available strongly act against bacteria, viruses, fungi, and yeasts [67]. A report showed that A.vera pulp inhibitory activity on Fusarium oxysporum and its liquid fraction reduced Rhizoctonia solani, F. oxysporum, and Colletotrichum coccodes colony growth rates [229]. Some studies reported unspecified A. ferox ‘juice’ antifungal activity against Trichophyton spp. causing athlete’s foot and thrush [230]. Low activity was recorded for methanol extract against C. albicans [221]. Again, A. ferox acetone extract was found to be fungicidal against five fungi [170].
In many research studies, it has been reported that A. vera showed antiviral activity preventing virus adsorption, attachment, or entry into host cells. Zandi and Rastian [287] showed that A. vera gel had antiviral activity against herpes simplex virus (HSV) type 2 strains. Anthraquinone derivatives, such as aloe-emodin, emodin, and chrysophanol, which are present in aloe, have been reported to exhibit antiviral activity, also displaying inhibitory mechanisms against influenza A virus replication and virus-induced cytopathic effect [231]. Aloe was shown to increase CD4 count, which results from an immune system improvement. This may be beneficial to HIV-infected patients. It is thought that CD4 count raise can be attributed to in vitro HIV inhibition by acemannan or the immune-modulatory effects of aloe components [232]. Similarly, aloe-emodin displayed promising effects in reducing herpes simplex virus Type I and Type II infection. It can also inhibit viruses, such as Varicella zoster virus (VSV), influenza virus, and pseudorabies virus [181,233]. In various studies, it was reported that polysaccharide acemannan prevented human lung epithelial cell-bacteria adhesion, and also reduced herpes simplex virus infection [288,289,290]. In vitro and in vivo antiviral effects have also been observed for A. ferox and A. secundiflora leaf extracts, respectively [291,292].
7.7. Antiplasmodial/Antimalarial Activity
Malaria is a deadly disease that infects over 150 million humans annually in Africa alone [293]. The protozoan Plasmodium falciparum is the deadliest causative Plasmodium species. Traditionally, aloes are not known to possess antimalarial properties, but several scientific studies indicated that some Aloe species can be used to treat malaria-related symptoms. Van Zyl and Viljoen [294] evaluated 34 Aloe species and their main constituents for antiplasmodial activity using titrated [3H]-hypoxanthine incorporation assay. It was found that several methanol extracts inhibited Plasmodium falciparum growth by 50% in concentrations of 32–77 mg/mL. Clarkson et al. [295] in vitro tested 134 plant species against P. falciparum strain D10 using parasite lactate dehydrogenase (pLDH) assay. A. ferox organic extract (DCM, dichloromethane/MeOH 1:1) displayed promising antiplasmodial effects (IC50 8 mg/mL), while aqueous extracts did not show any activity [295]. Aloe marlothii (whole plant) dichloromethane extract demonstrated good activity (IC50 of 3.5 mg/mL) against P. falciparum [295]. A. maculata [295] whole plant and A. viridiflora [294] leaf extracts showed mild activity. A. marlothii [295] root and A. speciosa, A. suprafoliata, and A. wickensii [294] leaf extracts showed weak activity. These findings indicate that the Aloe genus may be used as a potential antimalarial drug.
7.8. Anthelmintic Activity
The in vitro anthelmintic activity of the crude aqueous extract obtained from A. ferox was examined on eggs and larvae of the nematode parasite Haemonchus contortus. A. ferox extracts showed 100% egg hatch inhibition at 20 mg/mL and larval development inhibition at 2.5 mg/mL [296].
7.9. Anticancer Activity
Aloin, an anthraquinone that is a natural compound and the main Aloe ingredient, has been proposed as a potential therapeutic option in cancer, wherein it showed chemoprotective effects against 1,2-dimethylhydrazine-induced colon preneoplastic lesions in Wistar rats [234]. Indeed, aloin treatment inhibited vascular endothelial growth factor (VEGF) secretion in cancer cells. VEGF is one of the most important proangiogenic cytokines, which is known and well characterized as a tumor neovascularization inducer. Aloin treatment has shown to significantly inhibit VEGF-induced angiogenic response in human endothelial cells, in vitro, triggering proliferation inhibition and endothelial cell migration. Aloin was found to inhibit tumor angiogenesis and growth by signal transducer and activator of transcription 3 (STAT3) activation [235].
Aloe-emodin (1,8-dihydroxy-3-hydroxymethyl-9,10-anthracenedione) is an anthracenedione derivative from A. vera leaves. Recent reports have shown that aloe-emodin possesses antiproliferation effects in some cancer cells types, such as lung, squamous, glioma, and neuroectodermal cancer cells [236,237]. Aloe-emodin is also an anthraquinone subtype; it is a natural compound that has traditionally been found to have diverse biological activities, with anticancer functions among them [238,239]. Aloe-emodin has been found to possess an antiproliferation effect on some cancer cells types, inhibiting both N-acetyl transferase activity and gene expression. This effect plays a crucial role in aryl amine carcinogens metabolism, which is found in human malignant melanoma cells [240,241]. Recently, Lin et al. [241] demonstrated that aloe-emodin induced apoptosis in T24 human bladder cancer cells. Aloin, which is derived from A. vera leaves, has been shown to possess anticancer effects too [241], as it inhibits tumor angiogenesis and growth via blocking STAT3 activation, therefore displaying a potential as drug candidate for cancer therapy [242]. Anthraquinone derivatives, such as emodin-like natural (emodin, rhein, and aloin) and synthetic (anthraquinone-2-sulfonic acid) anthraquinones have recently been shown to protect amyloid β and aggregation-induced cell death through antiaggregating effects, and/or enhancing phosphatidylinositol-3-kinase/protein kinase B mediated survival mechanisms, which suggests that anthraquinone-2-sulfonic acid could be a new neuroprotective compound and a novel caspase inhibitor [148,243].
An investigation showed that polysaccharide acemannan inhibits benzopyrene binding with primary rat hepatocytes and thereby prevents cancer initiating benzopyrene DNA adduct formation [184,244]. In chemoprevention, A. vera gel stimulate glutathione S-transferase induction, which inhibits phorbol myristate acetate tumor-promoting effects [245,246]. Similarly, aloin inhibited cancer cells by altering a cell cycle through the mitochondrial-dependent pathway, which leads to cell membrane integrity loss and apoptosis [247]. A study demonstrated aloin protective effects on inducible nitric oxide synthase (iNOS) and NFκB synthesis induced in HaCat cells by ultraviolet (UV) B irradiation. Aloin inhibited NFκB and P65 activity by downregulating iNOS mRNA expression caused by UVB irradiation [248]. Aloe-emodin produced antitumor effects in P-glycoprotein overexpressing cell lines [249]. In addition, barbaloin, physcion, chrysophanol, aloesin, diethylhexyl phthalate, and an N-terminal octapeptide were reported to have cytotoxic activity on cancer cells [225,250,251,252,253]. Acemannan acts as a very active anticancer agent. Acemannan stimulated TNF-α, IL-1, and interferon production by macrophages and deactivated cancer cells [254]. In an experiment, aloin was tested on human uterine carcinoma HeLaS3 cells [297]. Aloin showed antiproliferative effects through arresting the cell cycle in the S phase and significantly increasing HeLaS3 cells apoptosis. This emphasized that aloin can be used for treating human cervical carcinoma in the future. It was also applied to radiosensitize HeLaS3 cells, which suggests an aloin cytotoxic adjuvant effect [298].
A. ferox is also used as an anticancer agent [299,300,301]. Aloe-emodin has been reported to have selective activity against neuroectodermal tumors, with practically no effect on normal cells [300]. Aloe-emodin promoted cell death through specific drug uptake by neuroectodermal tumors [302].
7.10. Antidiabetic Activity
The treatment of diabetes using various natural active compounds is still high-priority research. There are instances to consider A. vera as an antidiabetic agent. In vivo and in vitro studies strongly demonstrated that the water soluble fraction of Aloe species possesses glucose-lowering activities, and some of its components modulate glucose transporter-4 mRNA expression [255]. Studies have proved that the polysaccharides that are present in the plant protects β-cells from oxidative damage by alloxan [37,148,256]. It was reported that they helped reduce fasting blood glucose levels in alloxan-induced diabetic mice [257]. Polysaccharides play a major role in antidiabetic activities by increasing insulin levels, and hence, show hypoglycemic effects [183,258]. Phytosterols, such as lophenol, 24-methyl-lophenol, 24-ethyl-lophenol, cycloartanol, and 24-methylene cycloartanol were reported for their beneficial effects in diabetes and obesity [74]. A report gave confirmation of the clinical and experimental hypoglycemic conditions, due to A. vera sap oral intake continuously for four to 14 weeks [257]. One study discussed aloe-emodin-8-O-glycoside efficacy, isolated from A. vera gel, in enhancing glucose transport through proximal and distal marker modulation involved in glucose uptake and its transformation into glycogen [259]. Tanaka et al. [73] reported reductions in both the fasting and random blood glucose levels of db/db diabetic mice that were chronically treated with the same A. vera gel phytosterols [73]. Jain et al. [260] found that A. vera gel has significant antidiabetic and cardioprotective effects, as it significantly reduced oxidative stress in streptozotocin-induced diabetic rats and improved antioxidant status [260].
7.11. Antihyperlipidemic Activity
A recent study confirmed that phytosterols administration isolated from A. vera gel reduced visceral fat mass and improved hyperglycemia in Zucker diabetic fatty rats [261]. Aloe succotrina leaf dried pulp exerted remarkable antihyperlipidemic effects in high-fat diet and fructose-induced hyperlipidemic rats. It also significantly decreased the total serum cholesterol, total triglycerides, low-density lipoprotein (LDL), very low-density lipoprotein (VLDL), and high-density lipoprotein (HDL) cholesterol levels [262]. In polycystic ovarian syndrome (PCOS), rats treated with A. vera gel, plasma triglyceride, and LDL cholesterol levels decreased, while HDL cholesterol levels increased and PCOS were significantly reduced. Aloe gel also improved the reversion of abnormal estrous cyclicity, glucose intolerance, and lipid metabolizing enzyme activities [263,264,265].
7.12. Effect on Estrogen Status
Emodin and aloe-emodin isolated from A. vera gel suppressed breast cancer cell proliferation by targeting estrogen receptor-α protein stability through distinct mechanisms. This aspect suggests a possible anthraquinone application in preventing breast cancer cell proliferation through estrogen receptor-α inhibition [52]. A. vera gel also helped in maintaining ovarian steroid status in polycystic ovary-like condition, where steroidogenesis is altered and the estrogen and testosterone ratio is disturbed [263].
7.13. Antiulcer Activity
A. vera gel has the ability to minimize gastric ulcers in both humans and animals [30,267]. A. vera leaf extracts have also been widely recommended for digestion promotion and in peptic ulcer treatment due to its prominent cytoprotective action, whereby A. vera gel exhibited antibacterial activity against both susceptible and resistant H. pylori strains and acted as a promising effective natural agent in combination with antibiotics on H. pylori gastric infection treatment [5,266]. However, studies have confirmed that A. vera gel could not prevent ethanol-induced gastric lesions in rats [267]. In rats, gastric acid secretion and hydrochloric acid induced-gastric mucosa damage was investigated after A. vera aqueous ethanol extract application. A. vera extract exhibited dose-dependent inhibitory effects on gastric acid secretions by direct interaction with acid-producing cells or with H2-receptors on parietal cells. A report confirmed that A. vera extract showed cytoprotective activity at low doses [268]. Another report demonstrated that a mixed treatment with A. vera and sucralfate reduced gastric inflammation, enhanced epithelial cell proliferation, elongated gastric glands, and reduced ulcer sizes [269].
7.14. Treatment of Cardiovascular Disorders
A. vera can be used on cardiovascular disorders treatment. It stimulated fibroblast cells for making new tissues. Proteoglycans and collagens are formed, thus reducing cardiovascular disorders risk, after fibroblasts stimulation [190].
7.15. Skin Use
Collagen, elastin, and hyaluronic acid are the major components of the skin dermis layer. Collagen forms the three-dimensional structure of skin, and elastin maintains its elasticity, whereas hyaluronic acid restores skin moisture levels. Fibroblasts are mainly responsible for collagen activation, hyaluronic acid, and elastin in the skin dermis layer, and thereby maintain extracellular matrix homeostasis [270,271,272]. Aloe sterols promoted collagen production and thereby increased type I and type III collagen synthesis gene expression in human dermal fibroblasts. Sterols also increased the hyaluronic acid content of the dermal extracellular matrix. Therefore, they can improve skin moisture [273]. The melanocytic effects of A. vera leaf extract and aloin have been reported by Ali et al. [274], suggesting that they can be useful for hyperpigmentation treatment. Aloesin was reported to have tyrosinase inhibitory activity, which may be helpful in hyperpigmentation treatment, corresponding to melanin formation, such as melasma and ephelides [275]. Also, the skin cell proliferating activity of an Aloe glycopeptide (G1G1M1DI2) (MW 5.500 Da) was reported [303].
7.16. Anti-Aging Effect
A. vera was reported to trigger collagen and elastin fiber production, making skin more elastic and less wrinkled, but the exact mechanism is not well understood [4,177].
7.17. Antiallergic Activity
An Aloe glycoprotein (10 kDa) was found to reduce histamine release and promote leukotriene synthesis and secretion in the activated lung mast cells of guinea pigs. Furthermore, glycoprotein dose-dependently decreased protein kinase C and phospholipase C activities, inhibiting diacylglycerol and phospholipase A activity and blocking Ca2+ influx during mast cell activation [276].
7.18. Effect on Central and Peripheral Nervous Systems
Following Aloe extracts administration, marked improvements in learning, memory, and cognitive function and Alzheimer disease have also been reported [304,305,306,307]. Aloe gel potential on Parkinson disease has also been reported in mice [308]. Moreover, Aloe leaf powder aqueous extract showed anticonvulsant activity in mice [309].
8. Clinical Efficacy of Aloe Plants in Humans
Aloe is known as healing plant. It has been used for traditional medical purposes in several cultures [220], and its distinct therapeutic properties have been reported (Table 7). Some of them are attributed to the specific compounds that are present in Aloe.
Table 7.
Bioactive effects of Aloe plant species: clinical studies.
| Biological Activities | Observed Effects | Active Molecules | References |
|---|---|---|---|
| Wound healing and cell proliferation | Tyrosinase activity inhibition, re-epithelialization, wound healing promotion | Arbutin, aloesin | [310,311,312,313,314,315,316,317] |
| Anti-inflammatory and immunomodulatory effects | Decrease pain score and aphthous wound healing period, promote eye external part treatment, downregulate lipopolysaccharide-induced inflammatory cytokine production and NLRP3 inflammasome expression, potentiate lymphocyte response, phagocytosis and circulating monocyte and macrophage levels | Acemannan, polysaccharides | [75,254,266,318,319,320,321] |
| Antidiabetic effects | Lower blood glucose levels, reduce body weight, body fat mass and insulin resistance, revert impaired fasting glucose levels and impaired glucose tolerance | Plant extracts | [322,323] |
| Antihyperlipidemic effects | Reduce atherosclerosis, total serum cholesterol and LDL levels | Plant extracts | [323] |
| Acquired immune deficiency syndrome (AIDS) treatment | Sooth wound and burn of internal organs, inhibit HIV-1 virus | Mannose-6-phosphate, plant extract | [324] |
| Dental and oral diseases treatment | Heal aphthous ulcers and reduce pain, plaque and gingivitis | Acemannan | [325,326] |
8.1. Wound Healing and Cell Proliferation
In traditional medicine, A. ferox leaves and roots are applied topically, sometimes mixed with animal fat, or taken internally to treat eczema, dermatitis, and acne. They are also used in the treatment of various other skin diseases or conditions, such as skin cancer, burns, and psoriasis [44]. Epidermal melanin overproduction, synthesized by tyrosinase action, causes skin hyperpigmentation. The aloesin and arbutin present in Aloe can inhibit tyrosinase activity in a synergistic manner [310]. In fact, it has been reported that aloesin can inhibit hyperpigmentation in human skin after UV radiation in a dose-dependent manner, while co-treatment with aloesin and arbutin exerted an additive effect [311]. A. barbadensis [312] and A. arborescens [313] wound-healing properties were also reported. In a clinical study, burn wound healing was found to be remarkably earlier in A. vera-treated patients than in those who were treated with 1% silver sulfadiazine cream and a burn dressing for superficial and partial thickness burn treatment [314]. In another clinical study, it was shown that re-epithelialization and partial thickness burn wound healing was significantly faster in Aloe-treated sites compared to the silver sulfadiazine-treated ones. The results confirmed that Aloe cream can be used to treat second-degree burn wounds, too [315]. A significant improvement in burning wound healing after A. vera treatment was observed in rat models [316,317].
8.2. Anti-Inflammatory and Immunomodulatory Effects
A report of a clinical study has shown that the oral administration of 2% A. vera gel is not only effective in decreasing pain score and wound size in recurrent aphthous stomatitis patients, but also in decreasing the aphthous wound-healing period [266]. It has been reported that A. vera extracts may be used to treat the external parts of eye inflammations, such as the cornea [318]. A. vera gel had strong immunomodulatory activity, downregulating lipopolysaccharide-induced inflammatory cytokine production and NLRP3 (NACHT, LRR, and PYD domains-containing protein 3) inflammasome expression in human macrophages [319]. Acemannan stimulated immunity through potentiating the lymphocyte response to alloantigen with nitric oxide production activation by macrophages and cytokines, such as interleukin (IL)-1, IL-6, interferon (IFN), and TNF-α. It enhanced phagocytosis and also increased circulating monocyte and macrophage levels [254,320,321]. Polysaccharide aloeride activated nuclear factor (NF)-ĸB in human macrophages similar to bacterial endotoxin [75].
8.3. Antidiabetic Activity
In general, the α-amylase that is present in human pancreatic cell helps control starch hydrolysis inside the body, and hence protects from postprandial hyperglycemia. Postprandial hyperglycemia is characterized by a rapid increase in blood glucose levels in diabetic patients. An investigation confirmed that A. vera decreased diabetes severity by lowering blood glucose levels in type 2 diabetic patients [322]. Other clinical studies have suggested that A. vera gel may act as a safe antihyperglycemic and antihypercholesterolemic agent in type 2 diabetic patients, without any significant effects on other normal blood lipid levels or liver/kidney function [323].
In a randomized controlled trial, A. vera gel complex reduced body weight, body fat mass, and insulin resistance in obese pre-diabetic and early non-treated diabetic patients [322]. Further, in a pilot study, two Aloe products in pre-diabetic patients over an eight-week period, tended to revert impaired fasting glucose levels and impaired glucose tolerance observed in pre-diabetes/metabolic syndrome conditions [322].
8.4. Antihyperlipidemic Activity
A. vera antihyperlipidemic activity has also been reported. It had beneficial effects on fatty streak development prevention, and may help in reducing atherosclerosis development through risk factor modification [323]. A. vera leaf gel efficacy was checked in hyperlipidemic type 2 diabetic patients in a randomized double-blind placebo-controlled clinical trial, wherein it reduced total cholesterol and low-density lipoprotein (LDL) levels [323].
8.5. Treatment of Acquired Immune Deficiency Syndrome (AIDS)
It has been shown that acquired immune deficiency syndrome (AIDS) can be treated by using A. vera extracts in many reports. A daily intake of a minimum dose of 1200 mg of A. vera active ingredients improved AIDS symptoms. It soothed the wound and burn of internal organs, and hence acted as a promising AIDS drug. The mannose-6-phosphate present in A. vera can also inhibit the HIV-1 virus that causes AIDS [324].
8.6. Effect on Dental and Oral Diseases
It has been shown that acemannan hydrogels heal aphthous ulcers and reduce pain [325]. A. vera is very effective for gum diseases, such as gingivitis and periodontitis [327]. Besides, it has been reported that A. vera mouthwash reduced plaque and gingivitis, though less than chlorhexidine [326].
9. Conclusions and Future Perspectives
The therapeutic effects of Aloe species in traditional and modern medicines are well documented. The present report highlights the research progress on Aloe spp. botany, phytochemical composition, ethnobotanical uses, food preservation, and preclinical and clinical efficacy. Of special attention are aloin A, aloin B, aloinoside A, aloinoside B, aloesin, plicataloside, isovitexin, and aloe-emodin, because of their prominent biological activity and abundance in Aloe plants. Therefore, considering the data presented here, and namely taking into consideration both its valuable phytoconstituents and wide beneficial effects, the Aloe species may be considered as economically important matrices for food, medical, and pharmaceutical industries.
Acknowledgments
N.M. would like to thank the Portuguese Foundation for Science and Technology (FCT–Portugal) for the Strategic project ref. UID/BIM/04293/2013 and “NORTE2020—Programa Operacional Regional do Norte” (NORTE-01-0145-FEDER-000012).
Author Contributions
All authors contributed equally to this work. B.S., M.S.-R., F.S., N.M., M.I. and J.S.-R. critically reviewed the manuscript. All the authors read and approved the final manuscript.
Funding
Portuguese Foundation for Science and Technology (FCT–Portugal): Strategic project ref. UID/BIM/04293/2013 and “NORTE2020—Programa Operacional Regional do Norte” (NORTE-01-0145-FEDER-000012).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Klopper R.R., Smith G.F. The genus ALOE (Asphodelaceae: Alooideae) in namaqualand, South Africa. Haseltonia. 2007;13:38–51. doi: 10.2985/1070-0048(2007)13[38:TGAAAI]2.0.CO;2. [DOI] [Google Scholar]
- 2.Surjushe A., Vasani R., Saple D.G. Aloe vera: A short review. Indian J. Dermatol. 2008;53:163–166. doi: 10.4103/0019-5154.44785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boudreau M.D., Beland F.A. An evaluation of the biological and toxicological properties of Aloe Barbadensis (miller), Aloe vera. J. Environ. Sci. Health C. 2006;24:103–154. doi: 10.1080/10590500600614303. [DOI] [PubMed] [Google Scholar]
- 4.Rahmani A.H., Aldebasi Y.H., Srikar S., Khan A.A., Aly S.M. Aloe vera: Potential candidate in health management via modulation of biological activities. Pharmacogn. Rev. 2015;9:120–126. doi: 10.4103/0973-7847.162118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Radha M.H., Laxmipriya N.P. Evaluation of biological properties and clinical effectiveness of Aloe vera: A systematic review. J. Tradit. Complement. Med. 2015;5:21–26. doi: 10.1016/j.jtcme.2014.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nejatzadeh-Barandozi F. Antibacterial activities and antioxidant capacity of Aloe vera. Org. Med. Chem. Lett. 2013;3:5. doi: 10.1186/2191-2858-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jain S., Rathod N., Nagi R., Sur J., Laheji A., Gupta N., Agrawal P., Prasad S. Antibacterial effect of Aloe vera gel against oral pathogens: An in-vitro study. J. Clin. Diagn. Res. 2016;10:ZC41–ZC44. doi: 10.7860/JCDR/2016/21450.8890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Athiban P.P., Borthakur B.J., Ganesan S., Swathika B. Evaluation of antimicrobial efficacy of Aloe vera and its effectiveness in decontaminating gutta percha cones. J. Conservat. Dent. 2012;15:246–248. doi: 10.4103/0972-0707.97949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boudreau M.D., Mellick P.W., Olson G.R., Felton R.P., Thorn B.T., Beland F.A. Clear evidence of carcinogenic activity by a whole-leaf extract of aloe barbadensis miller (Aloe vera) in F344/n rats. Toxicol. Sci. 2013;131:26–39. doi: 10.1093/toxsci/kfs275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grundmann O. Aloe vera gel research review: An overview of its clinical uses and proposed mechanisms of action. Nat. Med. J. 2012;4:9. [Google Scholar]
- 11.Thamlikitkul V., Bunyapraphatsara N., Riewpaiboon W., Theerapong S., Chantrakul C., Thanaveerasuwan T., Nimitnon S., Wongkonkatape S., Riewpaiboon A., Tenambergen E.D. Clinical trial of Aloe vera linn. For treatment of minor burns. Siriraj Med. J. 2017;43:4. [Google Scholar]
- 12.Hazrati S., Tahmasebi-Sarvestani Z., Mokhtassi-Bidgoli A., Modarres-Sanavy S.A.M., Mohammadi H., Nicola S. Effects of zeolite and water stress on growth, yield and chemical compositions of Aloe vera L. Agric. Water Manag. 2017;181:66–72. doi: 10.1016/j.agwat.2016.11.026. [DOI] [Google Scholar]
- 13.Datta A., Mandal A., Teixeira da Silva J., Saha A., Paul R., Sengupta S., Kumari Dubey P., Halder S. An updated overview on Aloe vera (L.) Burm. F. Med. Aromat. Plant Sci. Biotechnol. 2012;6:1–11. [Google Scholar]
- 14.Serrano M., Valverde J.M., Guillén F., Castillo S., Martínez-Romero D., Valero D. Use of Aloe vera gel coating preserves the functional properties of table grapes. J. Agric. Food Chem. 2006;54:3882–3886. doi: 10.1021/jf060168p. [DOI] [PubMed] [Google Scholar]
- 15.Ahlawat K.S., Khatkar B.S. Processing, food applications and safety of Aloe vera products: A review. J. Food Sci. Technol. 2011;48:525–533. doi: 10.1007/s13197-011-0229-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ernst van Jaarsveld N. The genus aloe in south africa with special reference to Aloe hereroensis. Veld Flora. 1989;75:73–76. [Google Scholar]
- 17.Sachedina H., Bodeker G. Wild aloe harvesting in South Africa. J. Altern. Complement. Med. 1998;5:121–123. doi: 10.1089/acm.1999.5.121. [DOI] [PubMed] [Google Scholar]
- 18.Jordan J. The ecology of the aloes of zimbabwe. Excelsa. 1996;17:101–110. [Google Scholar]
- 19.Giddy C. Aloes from seed. Veld Flora. 1973;59:41. [Google Scholar]
- 20.Cloete E., Plumstead E. Toxic soils and Aloe colours. Veld Flora. 2000;86:29. [Google Scholar]
- 21.Lloyd J.U. Aloe succotrina. The Western Druggist; Chicago, IL, USA: 1898. [Google Scholar]
- 22.Grace O.M., Simmonds M.S., Smith G.F., van Wyk A.E. Documented utility and biocultural value of Aloe L. (Asphodelaceae): A review. Econ. Bot. 2009;63:167–178. doi: 10.1007/s12231-009-9082-7. [DOI] [Google Scholar]
- 23.King E.G., Stanton M.L. Facilitative effects of aloe shrubs on grass establishment, growth, and reproduction in degraded kenyan rangelands: Implications for restoration. Restor. Ecol. 2008;16:464–474. doi: 10.1111/j.1526-100X.2007.00310.x. [DOI] [Google Scholar]
- 24.Smith G.F., de S Correia R.I. Establishment of Aloe greatheadii var. Davyana from seed for use in reclamation trials. Landsc. Urban Plan. 1992;23:47–54. doi: 10.1016/0169-2046(92)90063-6. [DOI] [Google Scholar]
- 25.Palermo F.A., Cocci P., Angeletti M., Felici A., Polzonetti-Magni A.M., Mosconi G. Dietary Aloe vera components’ effects on cholesterol lowering and estrogenic responses in juvenile goldfish, Carassius auratus. Fish Physiol. Biochem. 2013;39:851–861. doi: 10.1007/s10695-012-9745-7. [DOI] [PubMed] [Google Scholar]
- 26.Cock I. Novel Natural Products: Therapeutic Effects in Pain, Arthritis and Gastro-Intestinal Diseases. Springer; Berlin, Germany: 2015. The genus aloe: Phytochemistry and therapeutic uses including treatments for gastrointestinal conditions and chronic inflammation; pp. 179–235. [DOI] [PubMed] [Google Scholar]
- 27.Reynolds T. Aloes: The Genus Aloe. CRC Press; Boca Raton, FL, USA: 2004. [Google Scholar]
- 28.Gutterman Y., Chauser-Volfson E. The distribution of the phenolic metabolites barbaloin, aloeresin and aloenin as a peripheral defense strategy in the succulent leaf parts of aloe arborescens. Biochem. Syst. Ecol. 2000;28:825–838. doi: 10.1016/S0305-1978(99)00129-5. [DOI] [PubMed] [Google Scholar]
- 29.Dagne E., Bisrat D., Viljoen A., Van Wyk B. Chemistry of aloe species. Curr. Org. Chem. 2000;4:1055–1078. doi: 10.2174/1385272003375932. [DOI] [Google Scholar]
- 30.Hamman J.H. Composition and applications of Aloe vera leaf gel. Molecules. 2008;13:1599–1616. doi: 10.3390/molecules13081599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sharrif Moghaddasi M., Res M. Aloe vera their chemicals composition and applications: A review. Int. J. Biol. Med. Res. 2011;2:466–471. [Google Scholar]
- 32.Femenia A., Sánchez E.S., Simal S., Rosselló C. Compositional features of polysaccharides from Aloe vera (Aloe barbadensis miller) plant tissues. Carbohydr. Polym. 1999;39:109–117. doi: 10.1016/S0144-8617(98)00163-5. [DOI] [Google Scholar]
- 33.Viljoen A.M., Van Wyk B.-E., Newton L.E. The occurrence and taxonomic distribution of the anthrones aloin, aloinoside and microdontin in aloe. Biochem. Syst. Ecol. 2001;29:53–67. doi: 10.1016/S0305-1978(00)00024-7. [DOI] [PubMed] [Google Scholar]
- 34.Viljoen A.M., Van Wyk B.-E. The chemotaxonomic significance of the phenyl pyrone aloenin in the genus aloe. Biochem. Syst. Ecol. 2000;28:1009–1017. doi: 10.1016/S0305-1978(00)00018-1. [DOI] [PubMed] [Google Scholar]
- 35.El Sayed A.M., Ezzat S.M., El Naggar M.M., El Hawary S.S. In vivo diabetic wound healing effect and HPLC–DAD–ESI–MS/MS profiling of the methanol extracts of eight aloe species. Rev. Bras. Farmacogn. 2016;26:352–362. doi: 10.1016/j.bjp.2016.01.009. [DOI] [Google Scholar]
- 36.Viljoen A.M., van Wyk B.-E., Newton L.E. Plicataloside in aloe—A chemotaxonomic appraisal. Biochem. Syst. Ecol. 1999;27:507–517. doi: 10.1016/S0305-1978(98)00111-2. [DOI] [Google Scholar]
- 37.Lee K.Y., Weintraub S.T., Yu B.P. Isolation and identification of a phenolic antioxidant from aloe barbadensis. Free Radic. Biol. Med. 2000;28:261–265. doi: 10.1016/S0891-5849(99)00235-X. [DOI] [PubMed] [Google Scholar]
- 38.Conner J.M., Gray A.I., Reynolds T., Waterman P.G. Anthraquinone, anthrone and phenylpyrone components of Aloe nyeriensis var. Kedongensis leaf exudate. Phytochemistry. 1987;26:2995–2997. doi: 10.1016/S0031-9422(00)84578-1. [DOI] [Google Scholar]
- 39.Van Heerden F.R., van Wyk B.-E., Viljoen A.M. Aloeresins E and F, two chromone derivatives from Aloe peglerae. Phytochemistry. 1996;43:867–869. doi: 10.1016/0031-9422(96)00302-0. [DOI] [Google Scholar]
- 40.Rebecca W., Kayser O., Hagels H., Zessin K.H., Madundo M., Gamba N. The phytochemical profile and identification of main phenolic compounds from the leaf exudate of aloe secundiflora by high-performance liquid chromatography-mass spectroscopy. Phytochem. Anal. Int. J. Plant Chem. Biochem. Techn. 2003;14:83–86. doi: 10.1002/pca.682. [DOI] [PubMed] [Google Scholar]
- 41.Ranghoo-Sanmukhiya M., Govinden-Soulange J., Lavergne C., Khoyratty S., Da Silva D., Frederich M., Kodja H. Molecular biology, phytochemistry and bioactivity of three endemic Aloe species from Mauritius and Réunion islands. Phytochem. Anal. 2010;21:566–574. doi: 10.1002/pca.1234. [DOI] [PubMed] [Google Scholar]
- 42.Dey P., Dutta S., Chowdhury A., Das A.P., Chaudhuri T.K. Variation in phytochemical composition reveals distinct divergence of Aloe vera (L.) Burm. F. From other aloe species: Rationale behind selective preference of Aloe vera in nutritional and therapeutic use. J. Evid.-Based Complement. Altern. Med. 2017;22:624–631. doi: 10.1177/2156587217698292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Coopoosamy R. Isolation of volatile compounds of Aloe excelsa (Berger) Afr. J. Biotechnol. 2010;9:7289–7294. [Google Scholar]
- 44.Loots D.T., van der Westhuizen F.H., Botes L. Aloe ferox leaf gel phytochemical content, antioxidant capacity, and possible health benefits. J. Agric. Food. Chem. 2007;55:6891–6896. doi: 10.1021/jf071110t. [DOI] [PubMed] [Google Scholar]
- 45.Bawankar R., Deepti V., Singh P., Subashkumar R., Vivekanandhan G., Babu S. Evaluation of bioactive potential of an Aloe vera sterol extract. Phytother. Res. 2013;27:864–868. doi: 10.1002/ptr.4827. [DOI] [PubMed] [Google Scholar]
- 46.Viljoen A., Van Wyk B.-E., Van Heerden F. Distribution and chemotaxonomic significance of flavonoids inaloe (Asphodelaceae) Plant Syst. Evol. 1998;211:31–42. doi: 10.1007/BF00984910. [DOI] [Google Scholar]
- 47.Lobine D., Cummins I., Govinden-Soulange J., Ranghoo-Sanmukhiya M., Lindsey K., Chazot P., Ambler C., Grellscheid S., Sharples G., Lall N. Medicinal mascarene aloes: An audit of their phytotherapeutic potential. Fitoterapia. 2018;124:120–126. doi: 10.1016/j.fitote.2017.10.010. [DOI] [PubMed] [Google Scholar]
- 48.Chaithanya K.K. Phytochemical screening and in vitro antioxidant activities of ethanolic gel extract of Aloe adigratana reynolds. J. Pharm. Res. 2018;12:13. [Google Scholar]
- 49.Lucini L., Pellizzoni M., Pellegrino R., Molinari G.P., Colla G. Phytochemical constituents and in vitro radical scavenging activity of different aloe species. Food Chem. 2015;170:501–507. doi: 10.1016/j.foodchem.2014.08.034. [DOI] [PubMed] [Google Scholar]
- 50.Bisi-Johnson M.A., Obi C.L., Samuel B.B., Eloff J.N., Okoh A.I. Antibacterial activity of crude extracts of some South African medicinal plants against multidrug resistant etiological agents of diarrhoea. BMC Complement. Altern. Med. 2017;17:321. doi: 10.1186/s12906-017-1802-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lee S., Do S.-G., Kim S.Y., Kim J., Jin Y., Lee C.H. Mass spectrometry-based metabolite profiling and antioxidant activity of Aloe vera (Aloe barbadensis miller) in different growth stages. J. Agric. Food. Chem. 2012;60:11222–11228. doi: 10.1021/jf3026309. [DOI] [PubMed] [Google Scholar]
- 52.Zhong J., Huang Y., Ding W., Wu X., Wan J., Luo H. Chemical constituents of Aloe barbadensis miller and their inhibitory effects on phosphodiesterase-4D. Fitoterapia. 2013;91:159–165. doi: 10.1016/j.fitote.2013.08.027. [DOI] [PubMed] [Google Scholar]
- 53.Wu X., Ding W., Zhong J., Wan J., Xie Z. Simultaneous qualitative and quantitative determination of phenolic compounds in Aloe barbadensis mill by liquid chromatography–mass spectrometry-ion trap-time-of-flight and high performance liquid chromatography-diode array detector. J. Pharm. Biomed. Anal. 2013;80:94–106. doi: 10.1016/j.jpba.2013.02.034. [DOI] [PubMed] [Google Scholar]
- 54.Gauniyal P., Teotia U.V.S. Phytochemical screening and antimicrobial activity of some medicinal plants against oral flora. Asian Pac. J. Health Sci. 2014;1:255–263. [Google Scholar]
- 55.Abeje F., Bisrat D., Hailu A., Asres K. Phytochemistry and antileishmanial activity of the leaf latex of aloe calidophila reynolds. Phytother. Res. 2014;28:1801–1805. doi: 10.1002/ptr.5204. [DOI] [PubMed] [Google Scholar]
- 56.Kambizi L., Sultana N., Afolayan A. Bioactive compounds isolated from Aloe ferox.: A plant traditionally used for the treatment of sexually transmitted infections in the eastern cape, South Africa. Pharm. Biol. 2005;42:636–639. doi: 10.1080/13880200490902581. [DOI] [Google Scholar]
- 57.Kametani S., Kojima-Yuasa A., Kikuzaki H., Kennedy D.O., Honzawa M., Matsui-Yuasa I. Chemical constituents of cape aloe and their synergistic growth-inhibiting effect on ehrlich ascites tumor cells. Biosci. Biotechnol. Biochem. 2007;71:1220–1229. doi: 10.1271/bbb.60659. [DOI] [PubMed] [Google Scholar]
- 58.Fawole O., Amoo S., Ndhlala A., Light M., Finnie J., Van Staden J. Anti-inflammatory, anticholinesterase, antioxidant and phytochemical properties of medicinal plants used for pain-related ailments in South Africa. J. Ethnopharmacol. 2010;127:235–241. doi: 10.1016/j.jep.2009.11.015. [DOI] [PubMed] [Google Scholar]
- 59.Wintola O.A., Afolayan A.J. Phytochemical constituents and antioxidant activities of the whole leaf extract of Aloe ferox mill. Pharmacogn. Mag. 2011;7:325–333. doi: 10.4103/0973-1296.90414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sun Y.N., Li L.Y., Li W., Kang J.S., Hwang I., Kim Y.H. Chemical components from Aloe and their inhibition of indoleamine 2,3-dioxygenase. Pharmacogn. Mag. 2017;13:58–63. doi: 10.4103/0973-1296.197633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bisrat D., Dagne E., van Wyk B.-E., Viljoen A. Chromones and anthrones from Aloe marlothii and Aloe rupestris. Phytochemistry. 2000;55:949–952. doi: 10.1016/S0031-9422(00)00328-9. [DOI] [PubMed] [Google Scholar]
- 62.Yagi A., Harada N., Yamada H., Iwadare S., Nishioka I. Antibradykinin active material in aloe saponaria. J. Pharm. Sci. 1982;71:1172–1174. doi: 10.1002/jps.2600711024. [DOI] [PubMed] [Google Scholar]
- 63.Oumer A., Bisrat D., Mazumder A., Asres K. A new antimicrobial anthrone from the leaf latex of Aloe trichosantha. Nat. Prod. Commun. 2014;9:949–952. [PubMed] [Google Scholar]
- 64.Kammoun M., Miladi S., Ali Y.B., Damak M., Gargouri Y., Bezzine S. In vitro study of the PLA2 inhibition and antioxidant activities of Aloe vera leaf skin extracts. Lipids Health Dis. 2011;10:30. doi: 10.1186/1476-511X-10-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kumar S., Yadav A., Yadav M., Yadav J.P. Effect of climate change on phytochemical diversity, total phenolic content and in vitro antioxidant activity of Aloe vera (L.) Burm. F. BMC Res. Notes. 2017;10:60. doi: 10.1186/s13104-017-2385-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Xiao Z., Chen D., Si J., Tu G., Ma L. The chemical constituents of Aloe vera L. Acta Pharm. Sin. 2000;35:120–123. [Google Scholar]
- 67.Lawrence R., Tripathi P., Jeyakumar E. Isolation, purification and evaluation of antibacterial agents from Aloe vera. Braz. J. Microbiol. 2009;40:906–915. doi: 10.1590/S1517-83822009000400023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Abdissa D., Geleta G., Bacha K., Abdissa N. Phytochemical investigation of aloe pulcherrima roots and evaluation for its antibacterial and antiplasmodial activities. PLoS ONE. 2017;12:e0173882. doi: 10.1371/journal.pone.0173882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Abdissa N., Gohlke S., Frese M., Sewald N. Cytotoxic compounds from aloe megalacantha. Molecules. 2017;22:1136. doi: 10.3390/molecules22071136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Muthii R.Z., Mucunu M.J., Peter M.M., Gitahi K.S. Phytochemistry and toxicity studies of aqueous and methanol extract of naturally growing and cultivated Aloe turkanensis. J. Pharmacogn. Phytochem. 2015;3:144–147. [Google Scholar]
- 71.Ndhlala A., Amoo S., Stafford G., Finnie J., Van Staden J. Antimicrobial, anti-inflammatory and mutagenic investigation of the south african tree aloe (Aloe barberae) J. Ethnopharmacol. 2009;124:404–408. doi: 10.1016/j.jep.2009.05.037. [DOI] [PubMed] [Google Scholar]
- 72.Hirata T., Suga T. Biologically active constituents of leaves and roots of Aloe arborescens var. Natalensis. Z. Naturforsch. C. 1977;32:731–734. doi: 10.1515/znc-1977-9-1010. [DOI] [PubMed] [Google Scholar]
- 73.Tanaka M., Misawa E., Ito Y., Habara N., Nomaguchi K., Yamada M., Toida T., Hayasawa H., Takase M., Inagaki M. Identification of five phytosterols from Aloe vera gel as anti-diabetic compounds. Biol. Pharm. Bull. 2006;29:1418–1422. doi: 10.1248/bpb.29.1418. [DOI] [PubMed] [Google Scholar]
- 74.Misawa E., Tanaka M., Nomaguchi K., Nabeshima K., Yamada M., Toida T., Iwatsuki K. Oral ingestion of Aloe vera phytosterols alters hepatic gene expression profiles and ameliorates obesity-associated metabolic disorders in zucker diabetic fatty rats. J. Agric. Food. Chem. 2012;60:2799–2806. doi: 10.1021/jf204465j. [DOI] [PubMed] [Google Scholar]
- 75.Pugh N., Ross S.A., ElSohly M.A., Pasco D.S. Characterization of aloeride, a new high-molecular-weight polysaccharide from Aloe vera with potent immunostimulatory activity. J. Agric. Food. Chem. 2001;49:1030–1034. doi: 10.1021/jf001036d. [DOI] [PubMed] [Google Scholar]
- 76.Vázquez B., Avila G., Segura D., Escalante B. Antiinflammatory activity of extracts from Aloe vera gel. J. Ethnopharmacol. 1996;55:69–75. doi: 10.1016/S0378-8741(96)01476-6. [DOI] [PubMed] [Google Scholar]
- 77.Van Heerden F.R., Viljoen A.M., van Wyk B.-E. 6′-O-coumaroylaloesin from Aloe castanea—A taxonomic marker for aloe section anguialoe. Phytochemistry. 2000;55:117–120. doi: 10.1016/S0031-9422(00)00252-1. [DOI] [PubMed] [Google Scholar]
- 78.Dagne E., Bisrat D., Van Wyk B.-E., Viljoen A. 10-hydroxyaloin B 6′-O-acetate, an oxanthrone from Aloe claviflora. J. Nat. Prod. 1998;61:256–257. doi: 10.1021/np970368i. [DOI] [PubMed] [Google Scholar]
- 79.Coopoosamy R., Magwa M. Antibacterial activity of aloe emodin and aloin a isolated from Aloe excelsa. Afr. J. Biotechnol. 2006;5:1092–1094. [Google Scholar]
- 80.Coopoosamy R. In-vitro studies on lectin derivatives of Aloe excelsa (Berger) J. Med. Plants Res. 2010;4:1738–1742. [Google Scholar]
- 81.Speranza G., Manitto P., Monti D., Lianza F. Feroxidin, a novel 1-methyltetralin derivative isolated from Cape Aloe. Tetrahedron Lett. 1990;31:3077–3080. doi: 10.1016/S0040-4039(00)89030-9. [DOI] [Google Scholar]
- 82.Speranza G., Dadà G., Lunazzi L., Gramatica P., Manitto P. A c-glucosylated 5-methylchromone from kenya Aloe. Phytochemistry. 1986;25:2219–2222. doi: 10.1016/0031-9422(86)80095-4. [DOI] [Google Scholar]
- 83.Speranza G., Manitto P., Monti D. Feralolide, a dihydroisocoumarin from cape aloe. Phytochemistry. 1993;33:175–178. doi: 10.1016/0031-9422(93)85417-P. [DOI] [Google Scholar]
- 84.Koyama J., Ogura T., Tagahara K. Naphtho [2,3-c]furan-4,9-dione and its derivatives from Aloe ferox. Phytochemistry. 1994;37:1147–1148. doi: 10.1016/S0031-9422(00)89546-1. [DOI] [Google Scholar]
- 85.Dagne E., Bisrat D., Van Wyk B.-E., Viljoen A., Hellwig V., Steglich W. Anthrones from Aloe microstigma. Phytochemistry. 1997;44:1271–1274. doi: 10.1016/S0031-9422(96)00710-8. [DOI] [Google Scholar]
- 86.Conner J.M., Gray A.I., Reynolds T., Waterman P.G. Anthracene and chromone derivatives in the exudate of Aloe rabaiensis. Phytochemistry. 1989;28:3551–3553. doi: 10.1016/0031-9422(89)80392-9. [DOI] [Google Scholar]
- 87.Blitzke T., Masaoud M., Schmidt J. Constituents of Aloe rubroviolacea. Fitoterapia. 2001;72:78–79. doi: 10.1016/S0367-326X(00)00239-2. [DOI] [PubMed] [Google Scholar]
- 88.Blitzke T., Porzel A., Masaoud M., Schmidt J. A chlorinated amide and piperidine alkaloids from Aloe sabaea. Phytochemistry. 2000;55:979–982. doi: 10.1016/S0031-9422(00)00269-7. [DOI] [PubMed] [Google Scholar]
- 89.Kedarnath N., Surekha R.S., Mahantesh S., Patil C. Phytochemical screening and antimicrobial activity of Aloe vera. World Res. J. Med. Aromat. Plants. 2012;1:11–13. [Google Scholar]
- 90.Dagne E., Casser I., Steglich W. Aloechrysone, a dihydroanthracenone from Aloe berhana. Phytochemistry. 1992;31:1791–1793. doi: 10.1016/0031-9422(92)83149-S. [DOI] [Google Scholar]
- 91.Yagi A., Makino K., Nishioka I. Studies on the constituents of Aloe sapnaria haw. I. The structures of tetrahydroanthracene derivatives and the related anthraquinones. Chem. Pharm. Bull. 1974;22:1159–1166. doi: 10.1248/cpb.22.1159. [DOI] [PubMed] [Google Scholar]
- 92.Al-Oqail M.M., El-Shaibany A., Al-Jassas E., Al-Sheddi E.S., Al-Massarani S.M., Farshori N.N. In vitro anti-proliferative activities of Aloe perryi flowers extract on human liver, colon, breast, lung, prostate and epithelial cancer cell lines. Pak. J. Pharm. Sci. 2016;29:723–729. [PubMed] [Google Scholar]
- 93.Abd-Alla H.I., Shaaban M., Shaaban K.A., Abu-Gabal N.S., Shalaby N.M., Laatsch H. New bioactive compounds from Aloe hijazensis. Nat. Prod. Res. 2009;23:1035–1049. doi: 10.1080/14786410802242851. [DOI] [PubMed] [Google Scholar]
- 94.Beppu H., Koike T., Shimpo K., Chihara T., Hoshino M., Ida C., Kuzuya H. Radical-scavenging effects of Aloe arborescens miller on prevention of pancreatic islet B-cell destruction in rats. J. Ethnopharmacol. 2003;89:37–45. doi: 10.1016/S0378-8741(03)00268-X. [DOI] [PubMed] [Google Scholar]
- 95.Akaberi M., Sobhani Z., Javadi B., Sahebkar A., Emami S.A. Therapeutic effects of Aloe spp. In traditional and modern medicine: A review. Biomed. Pharm. 2016;84:759–772. doi: 10.1016/j.biopha.2016.09.096. [DOI] [PubMed] [Google Scholar]
- 96.Atreya K., Pyakurel D., Thagunna K.S., Bhatta L.D., Uprety Y., Chaudhary R.P., Oli B.N., Rimal S.K. Factors contributing to the decline of traditional practices in communities from the gwallek–kedar area, kailash sacred landscape, Nepal. Environ. Manag. 2018;61:741–755. doi: 10.1007/s00267-018-1009-6. [DOI] [PubMed] [Google Scholar]
- 97.Gautam T.P. Indigenous uses of some medicinal plants in panchthar district, Nepal. Nepalese J. Biosci. 2011;1:125–130. doi: 10.3126/njbs.v1i0.7479. [DOI] [Google Scholar]
- 98.Limbu K., Basanta Kumar Rai D. Ethno-medicinal practices among the Limbu community in Limbuwan, Eastern Nepal. Global J. Hum. Soc. Sci. Res. 2013;13:2. [Google Scholar]
- 99.Acharya R. Ethnobotanical study of medicinal plants of resunga hill used by magar community of badagaun VDC, gulmi district, Nepal. Sci. World. 2012;10:54–65. doi: 10.3126/sw.v10i10.6863. [DOI] [Google Scholar]
- 100.Siwakoti M., Siwakoti S. Ethnomedicinal uses of plants among the satar tribe of Nepal. J. Econ. Taxon. Bot. 2000;24:323–333. [Google Scholar]
- 101.Pradhan S. Antihyperglycemic effect of various medicinal plants of sikkim himalayas—A review. Int. J. Res. Phytochem. Pharmacol. 2011;1:124–130. [Google Scholar]
- 102.Sushen U., Unnithan C., Rajan S., Chouhan R., Chouhan S., Uddin F., Kowsalya R. Aloe vera: A potential herb used as traditional medicine by tribal people of kondagatu and purudu of karimnagar district, telangana state, India. And their preparative methods. Eur. J. Pharm. Med. Res. 2017;4:820–831. [Google Scholar]
- 103.Parajuli R. Ethnomedicinal use of plants in rai community of maimajuwa and puwamajuwa VDCS of Ilam District, Eastern Nepal. Bull. Dept. Plant Res. 2012;34:65–73. [Google Scholar]
- 104.Parajuli R.R. Indigenous knowledge on medicinal plants: Maipokhari, Maimajhuwa and mabu VDCS of Ilam District, Eastern Nepal. J. Dept. Plant Resour. Nepal. 2013;35:50–58. [Google Scholar]
- 105.Rai S. Medicinal plants used by meche people of Jhapa District, Eastern Nepal. Our Nat. 2004;2:27–32. doi: 10.3126/on.v2i1.321. [DOI] [Google Scholar]
- 106.Hussain S., Hore D. Collection and conservation of major medicinal pants of Darjeeling and Sikkim Himalayas. Indian J. Tradit. Knowl. 2007;6:352–357. [Google Scholar]
- 107.Badola H.K., Pradhan B.K. Plants used in healthcare practices by limboo tribe in south–west of khangchendzonga biosphere reserve, Sikkim, India. Indian J. Tradit. Knowl. 2013;12:355–369. [Google Scholar]
- 108.Acharya K., Chaudhary R., Vetaas O. Medicinal plants of nepal: Distribution pattern along an elevational gradient and effectiveness of existing protected areas for their conservation. Banko Janakari. 2009;19:16–22. doi: 10.3126/banko.v19i1.2178. [DOI] [Google Scholar]
- 109.Thapa L.B., Dhakal T.M., Chaudhary R., Thapa H. Medicinal plants used by raji ethnic tribe of Nepal in treatment of gastrointestinal disorders. Our Nat. 2013;11:177–186. doi: 10.3126/on.v11i2.9645. [DOI] [Google Scholar]
- 110.Ghimire K., Bastakoti R.R. Ethnomedicinal knowledge and healthcare practices among the tharus of nawalparasi district in central Nepal. For. Ecol. Manag. 2009;257:2066–2072. doi: 10.1016/j.foreco.2009.01.039. [DOI] [Google Scholar]
- 111.Manandhar N. Plants and People of Nepal. Timber Press; Oregon, OR, USA: 2002. [Google Scholar]
- 112.Bhattarai N. Folk herbal remedies for diarrhoea and dysentery in central Nepal. Fitoterapia Milano. 1993;64:243. [Google Scholar]
- 113.Singh A.G., Kumar A., Tewari D.D. An ethnobotanical survey of medicinal plants used in terai forest of western Nepal. J. Ethnobiol. Ethnomed. 2012;8:19. doi: 10.1186/1746-4269-8-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Acharya E., Pokhrel B. Ethno-medicinal plants used by bantar of Bhaudaha, Morang, Nepal. Our Nat. 2006;4:96–103. [Google Scholar]
- 115.Grover J., Yadav S., Vats V. Medicinal plants of india with anti-diabetic potential. J. Ethnopharmacol. 2002;81:81–100. doi: 10.1016/S0378-8741(02)00059-4. [DOI] [PubMed] [Google Scholar]
- 116.Keter L.K., Mutiso P.C. Ethnobotanical studies of medicinal plants used by traditional health practitioners in the management of diabetes in lower eastern province, Kenya. J. Ethnopharmacol. 2012;139:74–80. doi: 10.1016/j.jep.2011.10.014. [DOI] [PubMed] [Google Scholar]
- 117.Tahraoui A., El-Hilaly J., Israili Z., Lyoussi B. Ethnopharmacological survey of plants used in the traditional treatment of hypertension and diabetes in South-Eastern Morocco (Errachidia province) J. Ethnopharmacol. 2007;110:105–117. doi: 10.1016/j.jep.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 118.Frei B., Baltisberger M., Sticher O., Heinrich M. Medical ethnobotany of the zapotecs of the isthmus-sierra (Oaxaca, Mexico): Documentation and assessment of indigenous uses. J. Ethnopharmacol. 1998;62:149–165. doi: 10.1016/S0378-8741(98)00051-8. [DOI] [PubMed] [Google Scholar]
- 119.Babb D.A., Pemba L., Seatlanyane P., Charalambous S., Churchyard G.J., Grant A.D. Use of traditional medicine by HIV-infected individuals in south africa in the era of antiretroviral therapy. Psychol. Health Med. 2007;12:314–320. doi: 10.1080/13548500600621511. [DOI] [PubMed] [Google Scholar]
- 120.Salehi B., Anil Kumar N.V., Şener B., Sharifi-Rad M., Kılıç M., Mahady G.B., Vlaisavljevic S., Iriti M., Kobarfard F., Setzer W.N., et al. Medicinal plants used in the treatment of human immunodeficiency virus. Int. J. Mol. Sci. 2018;19:1459. doi: 10.3390/ijms19051459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Scherrer A.M., Motti R., Weckerle C.S. Traditional plant use in the areas of monte vesole and ascea, cilento national park (Campania, Southern Italy) J. Ethnopharmacol. 2005;97:129–143. doi: 10.1016/j.jep.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 122.Cheikhyoussef A., Shapi M., Matengu K., Ashekele H.M. Ethnobotanical study of indigenous knowledge on medicinal plant use by traditional healers in oshikoto region, Namibia. J. Ethnobiol. Ethnomed. 2011;7:10. doi: 10.1186/1746-4269-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Gemedo-Dalle T., Maass B.L., Isselstein J. Plant biodiversity and ethnobotany of borana pastoralists in Southern Oromia, Ethiopia. Econ. Bot. 2005;59:43–65. doi: 10.1663/0013-0001(2005)059[0043:PBAEOB]2.0.CO;2. [DOI] [Google Scholar]
- 124.Abdolshahi A., Naybandi-Atashi S., Heydari-Majd M., Salehi B., Kobarfard F., Ayatollahi S.A., Ata A., Tabanelli G., Sharifi-Rad M., Montanari C., et al. Antibacterial activity of some Lamiaceae species against Staphylococcus aureus in yoghurt-based drink (Doogh) Cell. Mol. Biol. (Noisy-le-Grand, France) 2018;64:71–77. doi: 10.14715/cmb/2018.64.8.11. [DOI] [PubMed] [Google Scholar]
- 125.Mishra A.P., Sharifi-Rad M., Shariati M.A., Mabkhot Y.N., Al-Showiman S.S., Rauf A., Salehi B., Župunski M., Sharifi-Rad M., Gusain P., et al. Bioactive compounds and health benefits of edible Rumex species—A review. Cell. Mol. Biol. (Noisy-le-Grand, France) 2018;64:27–34. doi: 10.14715/cmb/2018.64.8.5. [DOI] [PubMed] [Google Scholar]
- 126.Marvdashti L.M., Abdolshahi A., Hedayati S., Sharifi-Rad M., Iriti M., Salehi B., Sharifi-Rad J. Pullulan gum production from low-quality fig syrup using Aureobasidium pullulans. Cell. Mol. Biol. 2018;64:22–26. doi: 10.14715/cmb/2018.64.8.4. [DOI] [PubMed] [Google Scholar]
- 127.Mishra A.P., Saklani S., Salehi B., Parcha V., Sharifi-Rad M., Milella L., Iriti M., Sharifi-Rad J., Srivastava M. Satyrium nepalense, a high altitude medicinal orchid of indian himalayan region: Chemical profile and biological activities of tuber extracts. Cell. Mol. Biol. (Noisy-le-Grand, France) 2018;64:35–43. doi: 10.14715/cmb/2018.64.8.6. [DOI] [PubMed] [Google Scholar]
- 128.Sharifi-Rad J., Tayeboon G.S., Niknam F., Sharifi-Rad M., Mohajeri M., Salehi B., Iriti M., Sharifi-Rad M. Veronica persica Poir. Extract—Antibacterial, antifungal and scolicidal activities, and inhibitory potential on Acetylcholinesterase, Tyrosinase, Lipoxygenase and Xanthine oxidase. Cell. Mol. Biol. (Noisy-le-Grand, France) 2018;64:50–56. doi: 10.14715/cmb/2018.64.8.8. [DOI] [PubMed] [Google Scholar]
- 129.Sharifi-Rad M., Fokou P., Sharopov F., Martorell M., Ademiluyi A., Rajkovic J., Salehi B., Martins N., Iriti M., Sharifi-Rad J. Antiulcer agents: From plant extracts to phytochemicals in healing promotion. Molecules. 2018;23:1751. doi: 10.3390/molecules23071751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Sharifi-Rad M., Varoni E.M., Salehi B., Sharifi-Rad J., Matthews K.R., Ayatollahi S.A., Kobarfard F., Ibrahim S.A., Mnayer D., Zakaria Z.A. Plants of the genus Zingiber as a source of bioactive phytochemicals: From tradition to pharmacy. Molecules. 2017;22:2145. doi: 10.3390/molecules22122145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Sharifi-Rad M., Ozcelik B., Altın G., Daşkaya-Dikmen C., Martorell M., Ramírez-Alarcón K., Alarcón-Zapata P., Morais-Braga M.F.B., Carneiro J.N.P., Alves Borges Leal A.L., et al. Salvia spp. Plants-from farm to food applications and phytopharmacotherapy. Trends Food Sci. Technol. 2018;80:242–263. doi: 10.1016/j.tifs.2018.08.008. [DOI] [Google Scholar]
- 132.Salehi B., Valussi M., Jugran A.K., Martorell M., Ramírez-Alarcón K., Stojanović-Radić Z.Z., Antolak H., Kręgiel D., Mileski K.S., Sharifi-Rad M., et al. Nepeta species: From farm to food applications and phytotherapy. Trends Food Sci. Technol. 2018;80:104–122. doi: 10.1016/j.tifs.2018.07.030. [DOI] [Google Scholar]
- 133.Sánchez-Machado D.I., López-Cervantes J., Sendón R., Sanches-Silva A. Aloe vera: Ancient knowledge with new frontiers. Trends Food Sci. Technol. 2017;61:94–102. doi: 10.1016/j.tifs.2016.12.005. [DOI] [Google Scholar]
- 134.Mulaudzi R., Ndhlala A., Kulkarni M., Finnie J., Van Staden J. Antimicrobial properties and phenolic contents of medicinal plants used by the venda people for conditions related to venereal diseases. J. Ethnopharmacol. 2011;135:330–337. doi: 10.1016/j.jep.2011.03.022. [DOI] [PubMed] [Google Scholar]
- 135.Baruah A., Bordoloi M., Baruah H.P.D. Aloe vera: A multipurpose industrial crop. Ind. Crops Prod. 2016;94:951–963. doi: 10.1016/j.indcrop.2016.08.034. [DOI] [Google Scholar]
- 136.Ferro V.A., Bradbury F., Cameron P., Shakir E., Rahman S.R., Stimson W.H. In vitro susceptibilities of shigella flexneri and streptococcus pyogenes to inner gel of Aloe barbadensis miller. Antimicrob. Agents Chemother. 2003;47:1137–1139. doi: 10.1128/AAC.47.3.1137-1139.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Johnson D.B., Shringi B., Patidar D.K., Chalichem N.S.S., Javvadi A.K. Screening of antimicrobial activity of alcoholic & aqueous extract of some indigenous plants. Indo-Global J. Pharm. Sci. 2011;1:186–193. [Google Scholar]
- 138.Luiz C., da Rocha Neto A.C., Franco P.O., Di Piero R.M. Emulsions of essential oils and Aloe polysaccharides: Antimicrobial activity and resistance inducer potential against Xanthomonas fragariae. Trop. Plant Pathol. 2017;42:370–381. doi: 10.1007/s40858-017-0153-5. [DOI] [Google Scholar]
- 139.Alemdar S., Agaoglu S. Investigation of in vitro antimicrobial activity of Aloe vera juice. J. Anim. Vet. Adv. 2009;8:99–102. [Google Scholar]
- 140.Dharajiya D., Pagi N., Jasani H., Patel P. Antimicrobial activity and phytochemical screening of Aloe vera (Aloe barbadensis Miller) Int. J. Curr. Microbiol. App. Sci. 2017;6:2152–2162. [Google Scholar]
- 141.Chen W., Van Wyk B.-E., Vermaak I., Viljoen A.M. Cape aloes—A review of the phytochemistry, pharmacology and commercialisation of Aloe ferox. Phytochem. Lett. 2012;5:1–12. doi: 10.1016/j.phytol.2011.09.001. [DOI] [Google Scholar]
- 142.Abakar H.O.M., Bakhiet S.E., Abadi R.S.M. Antimicrobial activity and minimum inhibitory concentration of Aloe vera sap and leaves using different extracts. J. Pharmacogn. Phytochem. 2017;6:298–303. [Google Scholar]
- 143.Jain I., Jain P., Bisht D., Sharma A., Srivastava B., Gupta N. Comparative evaluation of antibacterial efficacy of six indian plant extracts against streptococcus mutans. J. Clin. Diagn. Res. 2015;9:ZC50. doi: 10.7860/JCDR/2015/11526.5599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Martínez-Romero D., Alburquerque N., Valverde J., Guillén F., Castillo S., Valero D., Serrano M. Postharvest sweet cherry quality and safety maintenance by Aloe vera treatment: A new edible coating. Postharvest Biol. Technol. 2006;39:93–100. doi: 10.1016/j.postharvbio.2005.09.006. [DOI] [Google Scholar]
- 145.Wang H.H., Chung J.G., Ho C.C., Wu L.T., Chang S.H. Aloe-emodin effects on arylamine n-acetyltransferase activity in the bacterium helicobacter pylori. Planta Med. 1998;64:176–178. doi: 10.1055/s-2006-957399. [DOI] [PubMed] [Google Scholar]
- 146.Cellini L., Di Bartolomeo S., Di Campli E., Genovese S., Locatelli M., Di Giulio M. In vitro activity of a loe vera inner gel against h elicobacter pylori strains. Lett. Appl. Microbiol. 2014;59:43–48. doi: 10.1111/lam.12241. [DOI] [PubMed] [Google Scholar]
- 147.Kargaran M., Moradabadi A.R., Arjomandzadegan M., Hosseini H., Habibi G., Tayeboon M., Karami H., Akbari A. Effects of the aqueous extract of Aloe vera on the morphological and physiological properties of E. coli. Iran. Red Crescent Med. J. 2017;19 doi: 10.5812/ircmj.23896. [DOI] [Google Scholar]
- 148.Das S., Mishra B., Gill K., Ashraf M.S., Singh A.K., Sinha M., Sharma S., Xess I., Dalal K., Singh T.P. Isolation and characterization of novel protein with anti-fungal and anti-inflammatory properties from Aloe vera leaf gel. Int. J. Biol. Macromol. 2011;48:38–43. doi: 10.1016/j.ijbiomac.2010.09.010. [DOI] [PubMed] [Google Scholar]
- 149.Radi M., Firouzi E., Akhavan H., Amiri S. Effect of gelatin-based edible coatings incorporated with Aloe vera and black and green tea extracts on the shelf life of fresh-cut oranges. J. Food Qual. 2017;2017:10. doi: 10.1155/2017/9764650. [DOI] [Google Scholar]
- 150.Chen C.P., Wang B.J., Weng Y.M. Physiochemical and antimicrobial properties of edible aloe/gelatin composite films. Int. J. Food Sci. Technol. 2010;45:1050–1055. doi: 10.1111/j.1365-2621.2010.02235.x. [DOI] [Google Scholar]
- 151.Benítez S., Achaerandio I., Sepulcre F., Pujolà M. Aloe vera based edible coatings improve the quality of minimally processed ‘hayward’kiwifruit. Postharvest Biol. Technol. 2013;81:29–36. doi: 10.1016/j.postharvbio.2013.02.009. [DOI] [Google Scholar]
- 152.Benítez S., Achaerandio I., Pujolà M., Sepulcre F. Aloe vera as an alternative to traditional edible coatings used in fresh-cut fruits: A case of study with kiwifruit slices. LWT-Food Sci. Technol. 2015;61:184–193. doi: 10.1016/j.lwt.2014.11.036. [DOI] [Google Scholar]
- 153.Sogvar O.B., Saba M.K., Emamifar A. Aloe vera and ascorbic acid coatings maintain postharvest quality and reduce microbial load of strawberry fruit. Postharvest Biol. Technol. 2016;114:29–35. doi: 10.1016/j.postharvbio.2015.11.019. [DOI] [Google Scholar]
- 154.Saks Y., Barkai-Golan R. Aloe vera gel activity against plant pathogenic fungi. Postharvest Biol. Technol. 1995;6:159–165. doi: 10.1016/0925-5214(94)00051-S. [DOI] [Google Scholar]
- 155.De Rodrýguez D.J., Hernández-Castillo D., Rodrýguez-Garcýa R., Angulo-Sánchez J. Antifungal activity in vitro of Aloe vera pulp and liquid fraction against plant pathogenic fungi. Ind. Crops Prod. 2005;21:81–87. doi: 10.1016/j.indcrop.2004.01.002. [DOI] [Google Scholar]
- 156.Castillo S., Navarro D., Zapata P., Guillén F., Valero D., Serrano M., Martínez-Romero D. Antifungal efficacy of Aloe vera in vitro and its use as a preharvest treatment to maintain postharvest table grape quality. Postharvest Biol. Technol. 2010;57:183–188. doi: 10.1016/j.postharvbio.2010.04.006. [DOI] [Google Scholar]
- 157.Ortega-Toro R., Collazo-Bigliardi S., Roselló J., Santamarina P., Chiralt A. Antifungal starch-based edible films containing Aloe vera. Food Hydrocoll. 2017;72:1–10. doi: 10.1016/j.foodhyd.2017.05.023. [DOI] [Google Scholar]
- 158.Navarro D., Díaz-Mula H.M., Guillén F., Zapata P.J., Castillo S., Serrano M., Valero D., Martínez-Romero D. Reduction of nectarine decay caused by rhizopus stolonifer, botrytis cinerea and penicillium digitatum with Aloe vera gel alone or with the addition of thymol. Int. J. Food Microbiol. 2011;151:241–246. doi: 10.1016/j.ijfoodmicro.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 159.Vieira J.M., Flores-López M.L., de Rodríguez D.J., Sousa M.C., Vicente A.A., Martins J.T. Effect of chitosan—Aloe vera coating on postharvest quality of blueberry (Vaccinium corymbosum) fruit. Postharvest Biol. Technol. 2016;116:88–97. doi: 10.1016/j.postharvbio.2016.01.011. [DOI] [Google Scholar]
- 160.Zapata P., Navarro D., Guillén F., Castillo S., Martínez-Romero D., Valero D., Serrano M. Characterisation of gels from different aloe spp. As antifungal treatment: Potential crops for industrial applications. Ind. Crops Prod. 2013;42:223–230. doi: 10.1016/j.indcrop.2012.06.002. [DOI] [Google Scholar]
- 161.Nidiry E.S.J., Ganeshan G., Lokesha A. Antifungal activity of some extractives and constituents of Aloe vera. Res. J. Med. Plant. 2011;5:196–200. [Google Scholar]
- 162.Martínez-Romero D., Castillo S., Guillén F., Díaz-Mula H.M., Zapata P.J., Valero D., Serrano M. Aloe vera gel coating maintains quality and safety of ready-to-eat pomegranate arils. Postharvest Biol. Technol. 2013;86:107–112. doi: 10.1016/j.postharvbio.2013.06.022. [DOI] [Google Scholar]
- 163.Bill M., Sivakumar D., Korsten L., Thompson A.K. The efficacy of combined application of edible coatings and thyme oil in inducing resistance components in Avocado (Persea americana mill.) against anthracnose during post-harvest storage. Crop Prot. 2014;64:159–167. doi: 10.1016/j.cropro.2014.06.015. [DOI] [Google Scholar]
- 164.Sitara U., Hassan N., Naseem J. Antifungal activity of Aloe vera gel against plant pathogenic fungi. Pak. J. Bot. 2011;43:2231–2233. [Google Scholar]
- 165.Hassanpour H. Effect of Aloe vera gel coating on antioxidant capacity, antioxidant enzyme activities and decay in Raspberry fruit. LWT-Food Sci. Technol. 2015;60:495–501. doi: 10.1016/j.lwt.2014.07.049. [DOI] [Google Scholar]
- 166.Marpudi S.L., Abirami L., Srividya N. Enhancement of storage life and quality maintenance of papaya fruits using Aloe vera based antimicrobial coating. Indian J. Biotechnol. 2011;10:83–89. [Google Scholar]
- 167.Valverde J.M., Valero D., Martínez-Romero D., Guillén F., Castillo S., Serrano M. Novel edible coating based on Aloe vera gel to maintain table grape quality and safety. J. Agric. Food. Chem. 2005;53:7807–7813. doi: 10.1021/jf050962v. [DOI] [PubMed] [Google Scholar]
- 168.Adetunji C., Fawole O., Arowora K., Nwaubani S., Ajayi E., Oloke J., Majolagbe O., Ogundele B., Aina J., Adetunji J. Effects of edible coatings from Aloe vera gel on quality and postharvest physiology of Ananas comosus L. Fruit during ambient storage. Global J. Sci. Front. Res. Biotech Gene. 2012;12:39–43. [Google Scholar]
- 169.Chauhan O., Nanjappa C., Ashok N., Ravi N., Roopa N., Raju P. Shellac and Aloe vera gel based surface coating for shelf life extension of tomatoes. J. Food Sci. Technol. 2015;52:1200–1205. doi: 10.1007/s13197-013-1035-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Afolayan A., Grierson D., Kambizi L., Madamombe I., Masika P., Jäger A. In vitro antifungal activity of some South African medicinal plants. S. Afr. J. Bot. 2002;68:72–76. doi: 10.1016/S0254-6299(16)30458-6. [DOI] [Google Scholar]
- 171.Subramanian S., Kumar D.S., Arulselvan P., Senthilkumar G. In vitro antibacterial and antifungal activities of ethanolic extract of Aloe vera leaf gel. J. Plant Sci. 2006;1:348–355. [Google Scholar]
- 172.Rosca-Casian O., Parvu M., Vlase L., Tamas M. Antifungal activity of Aloe vera leaves. Fitoterapia. 2007;78:219–222. doi: 10.1016/j.fitote.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 173.Olaleye M., Bello-Michael C. Comparative antimicrobial activities of Aloe vera gel and leaf. Afr. J. Biotechnol. 2005;4:1413–1414. [Google Scholar]
- 174.Hashemi S.A., Madani S.A., Abediankenari S. The review on properties of Aloe vera in healing of cutaneous wounds. BioMed. Res. Int. 2015;2015 doi: 10.1155/2015/714216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Tarameshloo M., Norouzian M., Zarein-Dolab S., Dadpay M., Mohsenifar J., Gazor R. Aloe vera gel and thyroid hormone cream may improve wound healing in wistar rats. Anat. Cell Biol. 2012;45:170–177. doi: 10.5115/acb.2012.45.3.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Liu C., Leung M., Koon J., Zhu L., Hui Y., Yu B., Fung K. Macrophage activation by polysaccharide biological response modifier isolated from Aloe vera L. Var. Chinensis (HAW.) berg. Int. Immunopharmacol. 2006;6:1634–1641. doi: 10.1016/j.intimp.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 177.Davis R.H. Biological activity of Aloe vera. Sofw J. 1993;119:646. [Google Scholar]
- 178.Tizard I., Carpenter R., McAnalley B., Kemp M. The biological activities of mannans and related complex carbohydrates. Mol. Biother. 1989;1:290–296. [PubMed] [Google Scholar]
- 179.Subramanian S., Kumar D.S., Arulselvan P. Wound healing potential of Aloe vera leaf gel studied in experimental rabbits. Asian J. Biochem. 2006;1:178–185. [Google Scholar]
- 180.Liu L., Chen X., Wu B., Jiang Q. Influence of aloe polysaccharide on proliferation and hyaluronic acid and hydroxyproline secretion of human fibroblasts in vitro. J. Chin. Integr. Med. 2010;8:256–262. doi: 10.3736/jcim20100310. [DOI] [PubMed] [Google Scholar]
- 181.Feily A., Namazi M. Aloe vera in dermatology: A brief review. Giornale Italiano di Dermatologia e Venereologia: Organo Ufficiale, Societa Italiana di Dermatologia e Sifilografia. 2009;144:85–91. [PubMed] [Google Scholar]
- 182.Tizard I., Busbee D., Maxwell B., Kemp M. Effects of acemannan, a complex carbohydrate, on wound-healing in young and aged rats. Wounds-A Compend. Clin. Res. Pract. 1994;6:201–209. [Google Scholar]
- 183.Reynolds T., Dweck A. Aloe vera leaf gel: A review update. J. Ethnopharmacol. 1999;68:3–37. doi: 10.1016/S0378-8741(99)00085-9. [DOI] [PubMed] [Google Scholar]
- 184.Choi S.W., Son B.W., Son Y.S., Park Y.I., Lee S.K., Chung M.H. The wound-healing effect of a glycoprotein fraction isolated from Aloe vera. Brit. J. Dermatol. 2001;145:535–545. doi: 10.1046/j.1365-2133.2001.04410.x. [DOI] [PubMed] [Google Scholar]
- 185.Yao H., Chen Y., Li S., Huang L., Chen W., Lin X. Promotion proliferation effect of a polysaccharide from aloe barbadensis miller on human fibroblasts in vitro. Int. J. Biol. Macromol. 2009;45:152–156. doi: 10.1016/j.ijbiomac.2009.04.013. [DOI] [PubMed] [Google Scholar]
- 186.Rajput S.S., Soni K.K., Saxena R. Pharmacology and phytochemistry of saponin isolated from Aloe vera for wound healing activity. Asian J. Chem. 2009;21:1029–1032. [Google Scholar]
- 187.Ray A., Aswatha S.M. An analysis of the influence of growth periods on physical appearance, and acemannan and elemental distribution of Aloe vera L. Gel. Ind. Crops Prod. 2013;48:36–42. doi: 10.1016/j.indcrop.2013.03.024. [DOI] [Google Scholar]
- 188.Carien B., Alvaro V., Josias H. Modulation of drug efflux by aloe materials: An in vitro investigation across rat intestinal tissue. Pharmacogn. Mag. 2013;9:S44. doi: 10.4103/0973-1296.117864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Ishii Y., Tanizawa H., Takino Y. Studies of aloe. V. Mechanism of cathartic effect. (4) Biol. Pharm. Bull. 1994;17:651–653. doi: 10.1248/bpb.17.651. [DOI] [PubMed] [Google Scholar]
- 190.Joseph B., Raj S.J. Pharmacognostic and phytochemical properties of Aloe vera linn an overview. Int. J. Pharm. Sci. Rev. Res. 2010;4:106–110. [Google Scholar]
- 191.Yagi T., Yamauchi K. Synergistic effects of anthraquinones of the purgative activity of rhein anthrone in mice. J. Pharm. Pharmacol. 1999;51:93–95. [PubMed] [Google Scholar]
- 192.Sahu P.K., Giri D.D., Singh R., Pandey P., Gupta S., Shrivastava A.K., Kumar A., Pandey K.D. Therapeutic and medicinal uses of Aloe vera: A review. Pharmacol. Pharm. 2013;4:599. doi: 10.4236/pp.2013.48086. [DOI] [Google Scholar]
- 193.Steenkamp V., Stewart M. Medicinal applications and toxicological activities of aloe. Products. Pharm. Biol. 2007;45:411–420. doi: 10.1080/13880200701215307. [DOI] [Google Scholar]
- 194.Wintola O.A., Sunmonu T.O., Afolayan A.J. The effect of aloe ferox mill. In the treatment of loperamide-induced constipation in wistar rats. BMC Gastroenterol. 2010;10:95. doi: 10.1186/1471-230X-10-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Chihara T., Shimpo K., Beppu H., Yamamoto N., Kaneko T., Wakamatsu K., Sonoda S. Effects of aloe-emodin and emodin on proliferation of the MKN45 human gastric cancer cell line. Asian Pac. J. Cancer Prev. 2015;16:3887–3891. doi: 10.7314/APJCP.2015.16.9.3887. [DOI] [PubMed] [Google Scholar]
- 196.Qin H., Zhu M., Du T., She Q., Yang J., Zhu X., Wei L., Zhang J. Effects of aloe-emodin on proliferation and migration of human gastric cancer cell line BGC-823. Acta Anat. Sin. 2010;41:909–911. [Google Scholar]
- 197.Steinmeyer J. Pharmacological basis for the therapy of pain and inflammation with nonsteroidal anti-inflammatory drugs. Arthritis Res. Ther. 2000;2:379. doi: 10.1186/ar116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Amoo S.O., Aremu A.O., Van Staden J. Unraveling the medicinal potential of South African aloe species. J. Ethnopharmacol. 2014;153:19–41. doi: 10.1016/j.jep.2014.01.036. [DOI] [PubMed] [Google Scholar]
- 199.Li R.W., Lin G.D., Leach D.N., Waterman P.G., Myers S.P. Inhibition of coxs and 5-LOX and activation of ppars by australian clematis species (Ranunculaceae) J. Ethnopharmacol. 2006;104:138–143. doi: 10.1016/j.jep.2005.08.061. [DOI] [PubMed] [Google Scholar]
- 200.Park M.-Y., Kwon H.-J., Sung M.-K. Evaluation of aloin and aloe-emodin as anti-inflammatory agents in aloe by using murine macrophages. Biosci. Biotechnol. Biochem. 2009;73:828–832. doi: 10.1271/bbb.80714. [DOI] [PubMed] [Google Scholar]
- 201.Im S.-A., Oh S.-T., Song S., Kim M.-R., Kim D.-S., Woo S.-S., Jo T.H., Park Y.I., Lee C.-K. Identification of optimal molecular size of modified Aloe polysaccharides with maximum immunomodulatory activity. Int. Immunopharmacol. 2005;5:271–279. doi: 10.1016/j.intimp.2004.09.031. [DOI] [PubMed] [Google Scholar]
- 202.Lindsey K., Jäger A., Viljoen A., van Wyk B.-E. Cyclooxygenase inhibitory activity of aloe species. S. Afr. J. Bot. 2002;68:47–50. doi: 10.1016/S0254-6299(16)30453-7. [DOI] [Google Scholar]
- 203.Arosio B., Gagliano N., Fusaro L.M.P., Parmeggiani L., Tagliabue J., Galetti P., De Castri D., Moscheni C., Annoni G. Aloe-emodin quinone pretreatment reduces acute liver injury induced by carbon tetrachloride. Pharmacol. Toxicol. 2000;87:229–233. doi: 10.1034/j.1600-0773.2000.d01-79.x. [DOI] [PubMed] [Google Scholar]
- 204.Duansak D., Somboonwong J., Patumraj S. Effects of Aloe vera on leukocyte adhesion and TNF-α and IL-6 levels in burn wounded rats. Clin. Hemorheol. Microcirc. 2003;29:239–246. [PubMed] [Google Scholar]
- 205.Liu Z., Ge X., Lu Y., Dong S., Zhao Y., Zeng M. Effects of chitosan molecular weight and degree of deacetylation on the properties of gelatine-based films. Food Hydrocoll. 2012;26:311–317. doi: 10.1016/j.foodhyd.2011.06.008. [DOI] [Google Scholar]
- 206.Esua M.F., Rauwald J.-W. Novel bioactive maloyl glucans from Aloe vera gel: Isolation, structure elucidation and in vitro bioassays. Carbohydr. Res. 2006;341:355–364. doi: 10.1016/j.carres.2005.11.022. [DOI] [PubMed] [Google Scholar]
- 207.Che Q.-M., Akao T., Hattori M., Kobashi K., Namba T. Isolation of a human intestinal bacterium capable of transforming barbaloin to aloe-emodin anthrone1. Planta Med. 1991;57:15–19. doi: 10.1055/s-2006-960007. [DOI] [PubMed] [Google Scholar]
- 208.Hanley D., Solomon W., Saffran B., Davis R. The evaluation of natural substances in the treatment of adjuvant arthritis. J. Am. Podiat. Assoc. 1982;72:275. doi: 10.7547/87507315-72-6-275. [DOI] [PubMed] [Google Scholar]
- 209.Kumar M., Rakesh S., Nagpal R., Hemalatha R., Ramakrishna A., Sudarshan V., Ramagoni R., Shujauddin M., Verma V., Kumar A. Probiotic lactobacillus rhamnosus gg and Aloe vera gel improve lipid profiles in hypercholesterolemic rats. Nutrition. 2013;29:574–579. doi: 10.1016/j.nut.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 210.Etim O.E., Farombi E.O., Usoh I.F., Akpan E.J. The protective effect of Aloe vera juice on lindane induced hepatotoxicity and genotoxicity. Pak. J. Pharm. Sci. 2006;19:333–337. [PubMed] [Google Scholar]
- 211.Singab A.N.B., El-Hefnawy H.M., Esmat A., Gad H.A., Nazeam J.A. A systemic review on aloe arborescens pharmacological profile: Biological activities and pilot clinical trials. Phytother. Res. 2015;29:1858–1867. doi: 10.1002/ptr.5483. [DOI] [PubMed] [Google Scholar]
- 212.Saini D.K., Saini M.R. Evaluation of radioprotective efficacy and possible mechanism of action of aloe gel. Environ. Toxicol. Pharmacol. 2011;31:427–435. doi: 10.1016/j.etap.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 213.Jones K., Hughes J., Hong M., Jia Q., Orndorff S. Modulation of melanogenesis by aloesin: A competitive inhibitor of tyrosinase. Pigm. Cell Res. 2002;15:335–340. doi: 10.1034/j.1600-0749.2002.02014.x. [DOI] [PubMed] [Google Scholar]
- 214.Jia Q., Farrow T.M. 7-Hydroxy Chromones as Potent Antioxidants. 6,884,783. U.S. Patent. 2005 Apr 26;
- 215.Frum Y., Viljoen A. In vitro 5-lipoxygenase and anti-oxidant activities of south african medicinal plants commonly used topically for skin diseases. Skin Pharmacol. Physiol. 2006;19:329–335. doi: 10.1159/000095253. [DOI] [PubMed] [Google Scholar]
- 216.Sazhina N., Lapshin P., Zagoskina N., Misin V. Comparative study of antioxidant properties of extracts of various aloe species. Russ. J. Bioorganic Chem. 2016;42:735–740. doi: 10.1134/S106816201607013X. [DOI] [Google Scholar]
- 217.Kang M.-C., Kim S.Y., Kim Y.T., Kim E.-A., Lee S.-H., Ko S.-C., Wijesinghe W., Samarakoon K.W., Kim Y.-S., Cho J.H. In vitro and in vivo antioxidant activities of polysaccharide purified from Aloe vera (Aloe barbadensis) gel. Carbohydr. Polym. 2014;99:365–371. doi: 10.1016/j.carbpol.2013.07.091. [DOI] [PubMed] [Google Scholar]
- 218.Nwajo H. Antioxidant activity of the exudate from aloe barbadensis leaves in diabetic rats. Biokemistri. 2006;18:2. doi: 10.4314/biokem.v18i2.56395. [DOI] [Google Scholar]
- 219.Habeeb F., Shakir E., Bradbury F., Cameron P., Taravati M.R., Drummond A.J., Gray A.I., Ferro V.A. Screening methods used to determine the anti-microbial properties of Aloe vera inner gel. Methods. 2007;42:315–320. doi: 10.1016/j.ymeth.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 220.Grace O., Simmonds M., Smith G., Van Wyk A. Therapeutic uses of Aloe L. (Asphodelaceae) in Southern Africa. J. Ethnopharmacol. 2008;119:604–614. doi: 10.1016/j.jep.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 221.Kambiz L., Afolayan A. Extracts from aloe ferox and withania somnifera inhibit candida albicans and neisseria gonorrhoea. Afr. J. Biotechnol. 2008;7 doi: 10.4314/ajb.v7i1.58301. [DOI] [Google Scholar]
- 222.Bisi-Johnson M.A., Obi C.L., Hattori T., Oshima Y., Li S., Kambizi L., Eloff J.N., Vasaikar S.D. Evaluation of the antibacterial and anticancer activities of some South African medicinal plants. BMC Complement. Altern. Med. 2011;11:14. doi: 10.1186/1472-6882-11-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Luseba D., Elgorashi E., Ntloedibe D., Van Staden J. Antibacterial, anti-inflammatory and mutagenic effects of some medicinal plants used in south africa for the treatment of wounds and retained placenta in livestock. S. Afr. J. Bot. 2007;73:378–383. doi: 10.1016/j.sajb.2007.03.003. [DOI] [Google Scholar]
- 224.Cowan M.M. Plant products as antimicrobial agents. Clin. Microbiol. Rev. 1999;12:564–582. doi: 10.1128/cmr.12.4.564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.El-Shemy H., Aboul-Soud M., Nassr-Allah A., Aboul-Enein K., Kabash A., Yagi A. Antitumor properties and modulation of antioxidant enzymes’ activity by Aloe vera leaf active principles isolated via supercritical carbon dioxide extraction. Curr. Med. Chem. 2010;17:129–138. doi: 10.2174/092986710790112620. [DOI] [PubMed] [Google Scholar]
- 226.Sharifi-Rad J., Salehi B., Stojanović-Radić Z.Z., Fokou P.V.T., Sharifi-Rad M., Mahady G.B., Sharifi-Rad M., Masjedi M.R., Lawal T.O., Ayatollahi S.A., et al. Medicinal plants used in the treatment of tuberculosis—Ethnobotanical and ethnopharmacological approaches. Biotechnol. Adv. 2017 doi: 10.1016/j.biotechadv.2017.07.001. [DOI] [PubMed] [Google Scholar]
- 227.Tan Z., Li F., Xing J. Separation and purification of aloe anthraquinones using PEG/salt aqueous two-phase system. Sep. Sci. Technol. 2011;46:1503–1510. doi: 10.1080/01496395.2011.563766. [DOI] [Google Scholar]
- 228.Sharma A., GAUTAM S. An overview on medicinal properties of Aloe vera: Antibacterial & antifungal aspects. Int. J. Pharma Bio Sci. 2013;4:694–705. [Google Scholar]
- 229.Schmidt J.M., Greenspoon J.S. Aloe vera dermal wound gel is associated with a delay in wound healing. Obstet. Gynecol. 1991;78:115–117. [PubMed] [Google Scholar]
- 230.Soeda M. Studies on anti-bacterial and anti-fungal activities of cape aloe. Nippon Saikingaku Zasshi. 1966;21:609–614. doi: 10.3412/jsb.21.609. [DOI] [PubMed] [Google Scholar]
- 231.Li S.-W., Yang T.-C., Lai C.-C., Huang S.-H., Liao J.-M., Wan L., Lin Y.-J., Lin C.-W. Antiviral activity of aloe-emodin against influenza a virus via galectin-3 up-regulation. Eur. J. Pharmacol. 2014;738:125–132. doi: 10.1016/j.ejphar.2014.05.028. [DOI] [PubMed] [Google Scholar]
- 232.Olatunya O.S., Olatunya A.M., Anyabolu H.C., Adejuyigbe E.A., Oyelami O.A. Preliminary trial of Aloe vera gruel on hiv infection. J. Altern. Complement. Med. 2012;18:850–853. doi: 10.1089/acm.2010.0735. [DOI] [PubMed] [Google Scholar]
- 233.Sydiskis R., Owen D., Lohr J., Rosler K., Blomster R. Inactivation of enveloped viruses by anthraquinones extracted from plants. Antimicrob. Agents Chemother. 1991;35:2463–2466. doi: 10.1128/AAC.35.12.2463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Hamiza O., Rehman M., Khan R., Tahir M., Khan A., Lateef A., Sultana S. Chemopreventive effects of aloin against 1,2-dimethylhydrazine-induced preneoplastic lesions in the colon of wistar rats. Hum. Exp. Toxicol. 2014;33:148–163. doi: 10.1177/0960327113493307. [DOI] [PubMed] [Google Scholar]
- 235.Pan Q., Pan H., Lou H., Xu Y., Tian L. Inhibition of the angiogenesis and growth of aloin in human colorectal cancer in vitro and in vivo. Cancer Cell Int. 2013;13:69. doi: 10.1186/1475-2867-13-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Masaldan S., Iyer V.V. Exploration of effects of emodin in selected cancer cell lines: Enhanced growth inhibition by ascorbic acid and regulation of LRP1 and AR under hypoxia-like conditions. J. Appl. Toxicol. 2014;34:95–104. doi: 10.1002/jat.2838. [DOI] [PubMed] [Google Scholar]
- 237.Lin M.L., Lu Y.C., Su H.L., Lin H.T., Lee C.C., Kang S.E., Lai T.C., Chung J.G., Chen S.S. Destabilization of carp mRNAs by aloe-emodin contributes to caspase-8-mediated p53-independent apoptosis of human carcinoma cells. J. Cell. Biochem. 2011;112:1176–1191. doi: 10.1002/jcb.23031. [DOI] [PubMed] [Google Scholar]
- 238.Muto A., Hori M., Sasaki Y., Saitoh A., Yasuda I., Maekawa T., Uchida T., Asakura K., Nakazato T., Kaneda T. Emodin has a cytotoxic activity against human multiple myeloma as a janus-activated kinase 2 inhibitor. Mol. Cancer Therapeut. 2007;6:987–994. doi: 10.1158/1535-7163.MCT-06-0605. [DOI] [PubMed] [Google Scholar]
- 239.Lin S.-Y., Lai W.-W., Ho C.-C., Yu F.-S., Chen G.-W., Yang J.-S., Liu K.-C., Lin M.-L., Wu P.-P., Fan M.-J. Emodin induces apoptosis of human tongue squamous cancer SCC-4 cells through reactive oxygen species and mitochondria-dependent pathways. Anticancer Res. 2009;29:327–335. [PubMed] [Google Scholar]
- 240.LIN C.-C., KAO S.-T., CHEN G.-W., CHUNG J.-G. Berberine decreased n-acetylation of 2-aminofluorene through inhibition of n-acetyltransferase gene expression in human leukemia Hl-60 cells. Anticancer Res. 2005;25:4149–4155. [PubMed] [Google Scholar]
- 241.Lin J.-G., Chen G.-W., Li T.-M., Chouh S.-T., Tan T.-W., Chung J.-G. Aloe-emodin induces apoptosis in T24 human bladder cancer cells through the p53 dependent apoptotic pathway. J. Urol. 2006;175:343–347. doi: 10.1016/S0022-5347(05)00005-4. [DOI] [PubMed] [Google Scholar]
- 242.Jackson T., Verrier J., Kochanek P. Anthraquinone-2-sulfonic acid (AQ2S) is a Novel neurotherapeutic agent. Cell Death Dis. 2014;4:e451. doi: 10.1038/cddis.2012.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Sharifi-Rad J., Sharifi-Rad M., Salehi B., Iriti M., Roointan A., Mnayer D., Soltani-Nejad A., Afshari A. In vitro and in vivo assessment of free radical scavenging and antioxidant activities of Veronica persica Poir. Cell. Mol. Biol. (Noisy-le-Grand, France) 2018;64:57–64. doi: 10.14715/cmb/2018.64.8.9. [DOI] [PubMed] [Google Scholar]
- 244.Yagi A., Kabash A., Mizuno K., Moustafa S., Khalifa T., Tsuji H. Radical scavenging glycoprotein inhibiting cyclooxygenase-2 and thromboxane A2 synthase from Aloe vera gel. Planta Med. 2003;69:269–271. doi: 10.1055/s-2003-38481. [DOI] [PubMed] [Google Scholar]
- 245.Kim H.S., Lee B.M. Inhibition of benzo[a]pyrene-DNA adduct formation by Aloe barbadensis miller. Carcinogenesis. 1997;18:771–776. doi: 10.1093/carcin/18.4.771. [DOI] [PubMed] [Google Scholar]
- 246.Kim H.S., Kacew S., Lee B.M. In vitro chemopreventive effects of plant polysaccharides (Aloe barbadensis miller, Lentinus edodes, Ganoderma lucidum and Coriolus versicolor) Carcinogenesis. 1999;20:1637–1640. doi: 10.1093/carcin/20.8.1637. [DOI] [PubMed] [Google Scholar]
- 247.Buenz E.J. Aloin induces apoptosis in jurkat cells. Toxicol. Vitro. 2008;22:422–429. doi: 10.1016/j.tiv.2007.10.013. [DOI] [PubMed] [Google Scholar]
- 248.Song X., Xu A., Bi Z. Effect of aloin on inducible nitric oxide synthase and nuclear factor Kappa B synthesis of hacat cells irradiated by Ultraviolet B. Chin. J. Dermatol. 2005;38:565–568. [Google Scholar]
- 249.Grimaudo S., Tolomeo M., Gancitano R., Dalessandro N., Aiello E. Effects of highly purified anthraquinoid compounds from Aloe vera on sensitive and multidrug resistant leukemia cells. Oncol. Rep. 1997;4:341–343. doi: 10.3892/or.4.2.341. [DOI] [PubMed] [Google Scholar]
- 250.Kabbash A., El-Soud K., Zalat E., Shoeib N., Yagi A. Supercritical carbon dioxide extraction of aloe emodin and barbaloin from Aloe vera L. Leaves and their in-vitro cytotoxic activity. Saudi Pharm. J. 2008;16:75–81. [Google Scholar]
- 251.Lee K.H., Hong H.S., Lee C.H., Kim C.H. Induction of apoptosis in human leukaemic cell lines k562, hl60 and u937 by diethylhexylphthalate isolated from Aloe vera linne. J. Pharm. Pharmacol. 2000;52:1037–1041. doi: 10.1211/0022357001774778. [DOI] [PubMed] [Google Scholar]
- 252.Lee K.H., Kim J.H., Lim D.S., Kim C.H. Anti-leukaemic and anti-mutagenic effects of di (2-ethylhexyl) phthalate isolated from Aloe vera linne. J. Pharm. Pharmacol. 2000;52:593–598. doi: 10.1211/0022357001774246. [DOI] [PubMed] [Google Scholar]
- 253.Li T.-D., Gu J.-Y., Luo Y., Li J.-G. The antitumor active components from Aloe vera var. Chinesis Berg. Lishizhen Med. Mater. Med. Res. 2009;10:7. [Google Scholar]
- 254.Womble D., Helderman J.H. Enhancement of allo-resposiveness of human lymphocytes by acemannan (Carrisyntm) Int. J. Immunopharmacol. 1988;10:967–974. doi: 10.1016/0192-0561(88)90043-4. [DOI] [PubMed] [Google Scholar]
- 255.Kumar R., Sharma B., Tomar N.R., Roy P., Gupta A.K., Kumar A. In vivo evalution of hypoglycemic activity of Aloe spp. And identification of its mode of action on glut-4 gene expression in vitro. Appl. Biochem. Biotechnol. 2011;164:1246–1256. doi: 10.1007/s12010-011-9210-6. [DOI] [PubMed] [Google Scholar]
- 256.Rajasekaran S., Sivagnanam K., Subramanian S. Modulatory effects of Aloe vera leaf gel extract on oxidative stress in rats treated with streptozotocin. J. Pharm. Pharmacol. 2005;57:241–246. doi: 10.1211/0022357055416. [DOI] [PubMed] [Google Scholar]
- 257.Ghannam N., Kingston M., Al-Meshaal I.A., Tariq M., Parman N.S., Woodhouse N. The antidiabetic activity of aloes: Preliminary clinical and experimental observations. Horm. Res. Paediatr. 1986;24:288–294. doi: 10.1159/000180569. [DOI] [PubMed] [Google Scholar]
- 258.Franz G. Polysaccharides in pharmacy: Current applications and future concepts. Planta Med. 1989;55:493–497. doi: 10.1055/s-2006-962078. [DOI] [PubMed] [Google Scholar]
- 259.Anand S., Muthusamy V., Sujatha S., Sangeetha K., Raja R.B., Sudhagar S., Devi N.P., Lakshmi B. Aloe emodin glycosides stimulates glucose transport and glycogen storage through PI3K dependent mechanism in l6 myotubes and inhibits adipocyte differentiation in 3T3L1 adipocytes. FEBS Lett. 2010;584:3170–3178. doi: 10.1016/j.febslet.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 260.Jain N., Vijayaraghavan R., Pant S.C., Lomash V., Ali M. Aloe vera gel alleviates cardiotoxicity in streptozocin-induced diabetes in rats. J. Pharm. Pharmacol. 2010;62:115–123. doi: 10.1211/jpp.62.01.0013. [DOI] [PubMed] [Google Scholar]
- 261.Dana N., Javanmard S.H., Asgary S., Asnaashari H., Abdian N. The effect of Aloe vera leaf gel on fatty streak formation in hypercholesterolemic rabbits. J. Res. Med. Sci. 2012;17:439. [PMC free article] [PubMed] [Google Scholar]
- 262.Dhingra D., Lamba D., Kumar R., Nath P., Gauttam S. Antihyperlipidemic activity of Aloe succotrina in rats: Possibly mediated by inhibition of hmg-coa reductase. ISRN Pharmacol. 2014;2014 doi: 10.1155/2014/243575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Maharjan R., Nagar P.S., Nampoothiri L. Effect of Aloe barbadensis mill. Formulation on letrozole induced polycystic ovarian syndrome rat model. J. Ayurveda Integr. Med. 2010;1:273. doi: 10.4103/0975-9476.74090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Desai B.N., Maharjan R.H., Nampoothiri L.P. Aloe barbadensis mill. Formulation restores lipid profile to normal in a letrozole-induced polycystic ovarian syndrome rat model. Pharmacogn. Res. 2012;4:109. doi: 10.4103/0974-8490.94736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Bhalla A., Chauhan U. Identification of antihyperlipidemic components in Aloe vera through reverse phase HPlC. J. Biol. Sci. Med. 2015;1:21–27. [Google Scholar]
- 266.Babaee N., Zabihi E., Mohseni S., Moghadamnia A.A. Evaluation of the therapeutic effects of Aloe vera gel on minor recurrent aphthous stomatitis. Dental Res. J. 2012;9:381. [PMC free article] [PubMed] [Google Scholar]
- 267.Suvitayavat W., Sumrongkit C., Thirawarapan S., Bunyapraphatsara N. Effects of aloe preparation on the histamine-induced gastric secretion in rats. J. Ethnopharmacol. 2004;90:239–247. doi: 10.1016/j.jep.2003.09.044. [DOI] [PubMed] [Google Scholar]
- 268.Yusuf S., Agunu A., Diana M. The effect of Aloe vera A. Berger (Liliaceae) on gastric acid secretion and acute gastric mucosal injury in rats. J. Ethnopharmacol. 2004;93:33–37. doi: 10.1016/j.jep.2004.03.027. [DOI] [PubMed] [Google Scholar]
- 269.Eamlamnam K., Patumraj S., Visedopas N., Thong-Ngam D. Effects of Aloe vera and sucralfate on gastric microcirculatory changes, cytokine levels and gastric ulcer healing in rats. World J. Gastroenterol. 2006;12:2034. doi: 10.3748/wjg.v12.i13.2034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Ernst E. Adverse effects of herbal drugs in dermatology. Brit. J. Dermatol. 2000;143:923–929. doi: 10.1046/j.1365-2133.2000.03822.x. [DOI] [PubMed] [Google Scholar]
- 271.Sorrell J.M., Caplan A.I. Fibroblasts—A diverse population at the center of it all. Int. Rev. Cell Mol. Biol. 2009;276:161–214. doi: 10.1016/S1937-6448(09)76004-6. [DOI] [PubMed] [Google Scholar]
- 272.Sorrell J.M., Caplan A.I. Fibroblast heterogeneity: More than skin deep. J. Cell Sci. 2004;117:667–675. doi: 10.1242/jcs.01005. [DOI] [PubMed] [Google Scholar]
- 273.Liu X., Wu H., Byrne M., Krane S., Jaenisch R. Type iii collagen is crucial for collagen I fibrillogenesis and for normal cardiovascular development. Proc. Natl. Acad. Sci. USA. 1997;94:1852–1856. doi: 10.1073/pnas.94.5.1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Ali S.A., Galgut J.M., Choudhary R.K. On the novel action of melanolysis by a leaf extract of Aloe vera and its active ingredient aloin, potent skin depigmenting agents. Planta Med. 2012;78:767–771. doi: 10.1055/s-0031-1298406. [DOI] [PubMed] [Google Scholar]
- 275.Wu X., Yin S., Zhong J., Ding W., Wan J., Xie Z. Mushroom tyrosinase inhibitors from Aloe barbadensis miller. Fitoterapia. 2012;83:1706–1711. doi: 10.1016/j.fitote.2012.09.028. [DOI] [PubMed] [Google Scholar]
- 276.Ro J.Y., Lee B.C., Kim J.Y., Chung Y.J., Chung M.H., Lee S.K., Jo T.H., Kim K.H., Park Y.I. Inhibitory mechanism of aloe single component (Alprogen) on mediator release in guinea pig lung mast cells activated with specific antigen-antibody reactions. J. Pharmacol. Exp. Ther. 2000;292:114–121. [PubMed] [Google Scholar]
- 277.Sharifi-Rad J., Ayatollahi S.A., Varoni E.M., Salehi B., Kobarfard F., Sharifi-Rad M., Iriti M., Sharifi-Rad M. Chemical composition and functional properties of essential oils from Nepeta schiraziana boiss. Farmacia. 2017;65:802–812. [Google Scholar]
- 278.Halliwell B., Gutteridge J.M. Free Radicals in Biology and Medicine. Oxford University Press; New York, NY, USA: 2015. [Google Scholar]
- 279.Zhang X.-F., Xie L., Liu Y., Xiang J.-F., Tang Y.-L. Binding of the bioactive component Aloe dihydroisocoumarin with human serum albumin. J. Mol. Struct. 2008;891:87–92. doi: 10.1016/j.molstruc.2008.03.005. [DOI] [Google Scholar]
- 280.Zhang X.-F., Wang H.-M., Song Y.-L., Nie L.-H., Wang L.-F., Liu B., Shen P.-P., Liu Y. Isolation, structure elucidation, antioxidative and immunomodulatory properties of two novel dihydrocoumarins from Aloe vera. Bioorg. Med. Chem. Lett. 2006;16:949–953. doi: 10.1016/j.bmcl.2005.10.096. [DOI] [PubMed] [Google Scholar]
- 281.López A., de Tangil M.S., Vega-Orellana O., Ramírez A.S., Rico M. Phenolic constituents, antioxidant and preliminary antimycoplasmic activities of leaf skin and flowers of Aloe vera (L.) Burm. f. (syn. A. Barbadensis Mill.) from the Canary islands (Spain) Molecules. 2013;18:4942–4954. doi: 10.3390/molecules18054942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Botes L., Van der Westhuizen F.H., Loots D.T. Phytochemical contents and antioxidant capacities of two aloe greatheadii var. Davyana extracts. Molecules. 2008;13:2169–2180. doi: 10.3390/molecules13092169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Asamenew G., Bisrat D., Mazumder A., Asres K. In vitro antimicrobial and antioxidant activities of anthrone and chromone from the latex of aloe harlana reynolds. Phytother. Res. 2011;25:1756–1760. doi: 10.1002/ptr.3482. [DOI] [PubMed] [Google Scholar]
- 284.Yoo E.A., Kim S.D., Lee W.M., Park H.J., Kim S.K., Cho J.Y., Min W., Rhee M.H. Evaluation of antioxidant, antinociceptive, and anti-inflammatory activities of ethanol extracts from aloe saponaria haw. Phytother. Res. 2008;22:1389–1395. doi: 10.1002/ptr.2514. [DOI] [PubMed] [Google Scholar]
- 285.Cardarelli M., Rouphael Y., Pellizzoni M., Colla G., Lucini L. Profile of bioactive secondary metabolites and antioxidant capacity of leaf exudates from eighteen aloe species. Ind. Crops Prod. 2017;108:44–51. doi: 10.1016/j.indcrop.2017.06.017. [DOI] [Google Scholar]
- 286.Silva M.A., Trevisan G., Hoffmeister C., Rossato M.F., Boligon A.A., Walker C.I.B., Klafke J.Z., Oliveira S.M., Silva C.R., Athayde M.L. Anti-inflammatory and antioxidant effects of aloe saponaria haw in a model of uvb-induced paw sunburn in rats. J. Photochem. Photobiol. B Biol. 2014;133:47–54. doi: 10.1016/j.jphotobiol.2014.02.019. [DOI] [PubMed] [Google Scholar]
- 287.Zandi K., Zadeh M.A., Sartavi K., Rastian Z. Antiviral activity of Aloe vera against herpes simplex virus type 2: An in vitro study. Afr. J. Biotechnol. 2007;6:1770–1773. [Google Scholar]
- 288.Visuthikosol V., Chowchuen B., Sukwanarat Y., Sriurairatana S., Boonpucknavig V. Effect of Aloe vera gel to healing of burn wound a clinical and histologic study. J. Med. Assoc. Thai. 1995;78:403–409. [PubMed] [Google Scholar]
- 289.Kemp M., Kahlon J., Chinnah A., Carpenter R., McAnalley B., McDaniel H., Shannon W. In-vitro evaluation of the antiviral effects of acemannan on the replication and pathogenesis of HIV-1 and other enveloped viruses: Modification of the processing of glycoprotein precursors. Antivir. Res. 1990;13:83. [Google Scholar]
- 290.Azghani A.O., Williams I., Holiday D.B., Johnson A.R. A beta-linked mannan inhibits adherence of pseudomonas aeruginosa to human lung epithelial cells. Glycobiology. 1995;5:39–44. doi: 10.1093/glycob/5.1.39. [DOI] [PubMed] [Google Scholar]
- 291.Waihenya R., Mtambo M., Nkwengulila G. Evaluation of the efficacy of the crude extract of aloe secundiflora in chickens experimentally infected with newcastle disease virus. J. Ethnopharmacol. 2002;79:299–304. doi: 10.1016/S0378-8741(01)00370-1. [DOI] [PubMed] [Google Scholar]
- 292.Kambizi L., Goosen B., Taylor M., Afolayan A. Anti-viral effects of aqueous extracts of aloe ferox and withania somnifera on herpes simplex virus type 1 in cell culture. S. Afr. J. Sci. 2007;103:359–360. [Google Scholar]
- 293.Zofou D., Kuete V., Titanji V.P. Medicinal Plant Research in Africa. Elsevier; Amsterdam, The Netherlands: 2013. Antimalarial and other antiprotozoal products from african medicinal plants; pp. 661–709. [Google Scholar]
- 294.Van Zyl R., Viljoen A., Jäger A. In vitro activity of aloe extracts against plasmodium falciparum. S. Afr. J. Bot. 2002;68:106–110. doi: 10.1016/S0254-6299(16)30465-3. [DOI] [Google Scholar]
- 295.Clarkson C., Maharaj V.J., Crouch N.R., Grace O.M., Pillay P., Matsabisa M.G., Bhagwandin N., Smith P.J., Folb P.I. In vitro antiplasmodial activity of medicinal plants native to or naturalised in South Africa. J. Ethnopharmacol. 2004;92:177–191. doi: 10.1016/j.jep.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 296.Maphosa V., Masika P.J., Bizimenyera E.S., Eloff J. In-vitro anthelminthic activity of crude aqueous extracts of Aloe ferox, leonotis leonurus and elephantorrhiza elephantina against haemonchus contortus. Trop. Anim. Health Prod. 2010;42:301–307. doi: 10.1007/s11250-009-9421-9. [DOI] [PubMed] [Google Scholar]
- 297.Nićiforović A., Adžić M., Zarić B., Radojčić M. Adjuvant antiproliferative and cytotoxic effect of aloin in irradiated HELAS3 cells. Russ. J. Phys. Chem. A. 2007;81:1463–1466. doi: 10.1134/S0036024407090221. [DOI] [Google Scholar]
- 298.Niciforovic A., Adzic M., Spasic S.D., Radojcic M.B. Antitumor effects of a natural anthracycline analog (Aloin) involve altered activity of antioxidant enzymes in HELAS3 cells. Cancer Biol. Ther. 2007;6:1211–1216. doi: 10.4161/cbt.6.8.4383. [DOI] [PubMed] [Google Scholar]
- 299.Van Wyk B.-E. The potential of south african plants in the development of new medicinal products. S. Afr. J. Bot. 2011;77:812–829. doi: 10.1016/j.sajb.2011.08.011. [DOI] [Google Scholar]
- 300.Pecere T., Gazzola M.V., Mucignat C., Parolin C., Dalla Vecchia F., Cavaggioni A., Basso G., Diaspro A., Salvato B., Carli M. Aloe-emodin is a new type of anticancer agent with selective activity against neuroectodermal tumors. Cancer Res. 2000;60:2800–2804. [PubMed] [Google Scholar]
- 301.Capasso F., Borrelli F., Capasso R., Carlo G.D., Izzo A., Pinto L., Mascolo N., Castaldo S., Longo R. Aloe and its therapeutic use. Phytother. Res. 1998;12:S124–S127. doi: 10.1002/(SICI)1099-1573(1998)12:1+<S124::AID-PTR271>3.0.CO;2-X. [DOI] [Google Scholar]
- 302.Pecere T., Sarinella F., Salata C., Gatto B., Bet A., Dalla Vecchia F., Diaspro A., Carli M., Palumbo M., Palù G. Involvement of p53 in specific anti-neuroectodermal tumor activity of aloe-emodin. Int. J. Cancer. 2003;106:836–847. doi: 10.1002/ijc.11312. [DOI] [PubMed] [Google Scholar]
- 303.Yang M.R., Kang C.G., Roh Y.S., Son B.W., Choi H.D., Park Y.I., Lee S.K., Choi S.W., Chung M.K. The glycopeptide, a promoter of thymidine uptake, from Aloe vera. Nat. Prod. Sci. 1998;4:62–67. [Google Scholar]
- 304.Clementi M.E., Tringali G., Triggiani D., Giardina B. Aloe arborescens extract protects IMR-32 cells against alzheimer amyloid beta peptide via inhibition of radical peroxide production. Nat. Prod. Commun. 2015;10:1993–1995. [PubMed] [Google Scholar]
- 305.Tao L., Xie J., Wang Y., Wang S., Wu S., Wang Q., Ding H. Protective effects of aloe-emodin on scopolamine-induced memory impairment in mice and H2O2-induced cytotoxicity in PC12 cells. Bioorg. Med. Chem. Lett. 2014;24:5385–5389. doi: 10.1016/j.bmcl.2014.10.049. [DOI] [PubMed] [Google Scholar]
- 306.Halder S., Mehta A.K., Mediratta P.K. Aloe vera improves memory and reduces depression in mice. Nutr. Neurosci. 2013;16:250–254. doi: 10.1179/1476830512Y.0000000050. [DOI] [PubMed] [Google Scholar]
- 307.Wang Y., Cao L., Du G. Protective effects of Aloe vera extract on mitochondria of neuronal cells and rat brain. China J. Chin. Mater. Med. 2010;35:364–368. doi: 10.4268/cjcmm20100324. [DOI] [PubMed] [Google Scholar]
- 308.Bagewadi H.G., Rathor N. Effect of Aloe vera on animal models of parkinson disease in mice. Int. J. Pharm. Bio. Sci. 2014;5:549–559. [Google Scholar]
- 309.Rathor N., Arora T., Manocha S., Patil A.N., Mediratta P.K., Sharma K.K. Anticonvulsant activity of a loe vera leaf extract in acute and chronic models of epilepsy in mice. J. Pharm. Pharmacol. 2014;66:477–485. doi: 10.1111/jphp.12181. [DOI] [PubMed] [Google Scholar]
- 310.Jin Y.H., Lee S.J., Chung M.H., Park J.H., Park Y.I., Cho T.H., Lee S.K. Aloesin and arbutin inhibit tyrosinase activity in a synergistic manner via a different action mechanism. Arch. Pharm. Res. 1999;22:232. doi: 10.1007/BF02976355. [DOI] [PubMed] [Google Scholar]
- 311.Choi S., Park Y.I., Lee S.K., Kim J.E., Chung M.H. Aloesin inhibits hyperpigmentation induced by UV radiation. Clin. Exp. Dermatol. 2002;27:513–515. doi: 10.1046/j.1365-2230.2002.01120.x. [DOI] [PubMed] [Google Scholar]
- 312.Davis R.H., Rosenthal K.Y., Cesario L.R., Rouw G.A. Processed Aloe vera administered topically inhibits inflammation. J. Am. Podiat. Med. Assoc. 1989;79:395–397. doi: 10.7547/87507315-79-8-395. [DOI] [PubMed] [Google Scholar]
- 313.Jia Y., Zhao G., Jia J. Preliminary evaluation: The effects of Aloe ferox Miller and Aloe arborescens miller on wound healing. J. Ethnopharmacol. 2008;120:181–189. doi: 10.1016/j.jep.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 314.Shahzad M.N., Ahmed N. Effectiveness of Aloe vera gel compared with 1% silver sulphadiazine cream as burn wound dressing in second degree burns. J. Pak. Med. Assoc. 2013;63:225–230. [PubMed] [Google Scholar]
- 315.Khorasani G., Hosseinimehr S.J., Azadbakht M., Zamani A., Mahdavi M.R. Aloe versus silver sulfadiazine creams for second-degree burns: A randomized controlled study. Surg. Today. 2009;39:587–591. doi: 10.1007/s00595-008-3944-y. [DOI] [PubMed] [Google Scholar]
- 316.Tabandeh M.R., Oryan A., Mohammadalipour A. Polysaccharides of Aloe vera induce MMP-3 and TIMP-2 gene expression during the skin wound repair of rat. Int. J. Biol. Macromol. 2014;65:424–430. doi: 10.1016/j.ijbiomac.2014.01.055. [DOI] [PubMed] [Google Scholar]
- 317.Lakhanpal G., Bhalerao S., Sharma S., Patil H. To study the efficacy of different formulations of Aloe vera (spp. Aloe barbadensis) on wound healing in rats. Res. J. Pharm. Biol. Chem. Sci. 2015;6:432–440. [Google Scholar]
- 318.Woźniak A., Paduch R. Aloe vera extract activity on human corneal cells. Pharm. Biol. 2012;50:147–154. doi: 10.3109/13880209.2011.579980. [DOI] [PubMed] [Google Scholar]
- 319.Budai M.M., Varga A., Milesz S., Tőzsér J., Benkő S. Aloe vera downregulates LPS-induced inflammatory cytokine production and expression of NLRP3 inflammasome in human macrophages. Mol. Immunol. 2013;56:471–479. doi: 10.1016/j.molimm.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 320.Shida T., Yagi A., Nishimura H., Nishioka I. Effect of aloe extract on peripheral phagocytosis in adult bronchial asthma. Planta Med. 1985;51:273–275. doi: 10.1055/s-2007-969480. [DOI] [PubMed] [Google Scholar]
- 321.Karaca K., Sharma J., Nordgren R. Nitric oxide production by chicken macrophages activated by acemannan, a complex carbohydrate extracted from Aloe Vera. Int. J. Immunopharmacol. 1995;17:183–188. doi: 10.1016/0192-0561(94)00102-T. [DOI] [PubMed] [Google Scholar]
- 322.Devaraj S., Jialal R., Jialal I., Rockwood J. A pilot randomized placebo controlled trial of 2 Aloe vera supplements in patients with pre-diabetes/metabolic syndrome. Planta Med. 2008;74:SL77. doi: 10.1055/s-0028-1083957. [DOI] [Google Scholar]
- 323.Huseini H.F., Kianbakht S., Hajiaghaee R., Dabaghian F.H. Anti-hyperglycemic and anti-hypercholesterolemic effects of Aloe vera leaf gel in hyperlipidemic type 2 diabetic patients: A randomized double-blind placebo-controlled clinical trial. Planta Med. 2012;78:311–316. doi: 10.1055/s-0031-1280474. [DOI] [PubMed] [Google Scholar]
- 324.Urch D. Aloe vera Nature’s Gift. Blackdown Publications; Bristol, UK: 1999. pp. 7–13. [Google Scholar]
- 325.Oral ulcers remedy gets fda clearance. J. Am. Dent. Assoc. 1994;125:1308–1310. [PubMed] [Google Scholar]
- 326.Chandrahas B., Jayakumar A., Naveen A., Butchibabu K., Reddy P.K., Muralikrishna T. A randomized, double-blind clinical study to assess the antiplaque and antigingivitis efficacy of Aloe vera mouth rinse. J. Indian Soc. Periodontol. 2012;16:543. doi: 10.4103/0972-124X.106905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Grindlay D., Reynolds T. The Aloe vera phenomenon: A review of the properties and modern uses of the leaf parenchyma gel. J. Ethnopharmacol. 1986;16:117–151. doi: 10.1016/0378-8741(86)90085-1. [DOI] [PubMed] [Google Scholar]