Abstract
The annual incidence of mild traumatic brain injury (MTBI) is 3.8 million in the USA with 10–15% experiencing persistent morbidity beyond one year. Chronic traumatic encephalopathy (CTE), a neurodegenerative disease characterized by accumulation of hyperphosphorylated tau, can occur with repetitive MTBI. Risk factors for CTE are challenging to identify because injury mechanisms of MTBI are heterogeneous, clinical manifestations and management vary, and CTE is a postmortem diagnosis, making prospective studies difficult. There is growing interest in the genetic influence on head trauma and development of CTE. Apolipoprotein epsilon 4 (APOE-ε4) associates with many neurologic diseases, and consensus on the ε4 allele as a risk factor is lacking. This review investigates the influence of APOE-ε4 on MTBI and CTE. A comprehensive PubMed literature search (1966 to 12 June 2018) identified 24 unique reports on the topic (19 MTBI studies: 8 athletic, 5 military, 6 population-based; 5 CTE studies: 4 athletic and military, 1 leucotomy group). APOE-ε4 genotype is found to associate with outcomes in 4/8 athletic reports, 3/5 military reports, and 5/6 population-based reports following MTBI. Evidence on the association between APOE-ε4 and CTE from case series is equivocal. Refining modalities to aid CTE diagnosis in larger samples is needed in MTBI.
Keywords: apolipoprotein E, chronic traumatic encephalopathy, concussion, genetic risk factors, mild traumatic brain injury, neurodegenerative disorders
1. Introduction
Mild traumatic brain injury (MTBI) accounts for 70–90% of all traumatic brain injury (TBI), with an estimated 10–15% of MTBI patients reporting persistent cognitive and/or neuropsychiatric deficits at one year post-injury and beyond [1,2,3]. Of particular interest are patients subject to repetitive head trauma in the military or contact sports, contributing to the risk of chronic traumatic encephalopathy (CTE). First coined by New Jersey pathologist Harrison Martland in boxers as “punch-drunk syndrome” and “dementia pugilistica” in subsequent case reports [4,5], this collection of clinical symptoms was termed CTE by British neurologist Critchley in 1949 [6]. In 1973, Corsellis further clarified the diagnosis [7].
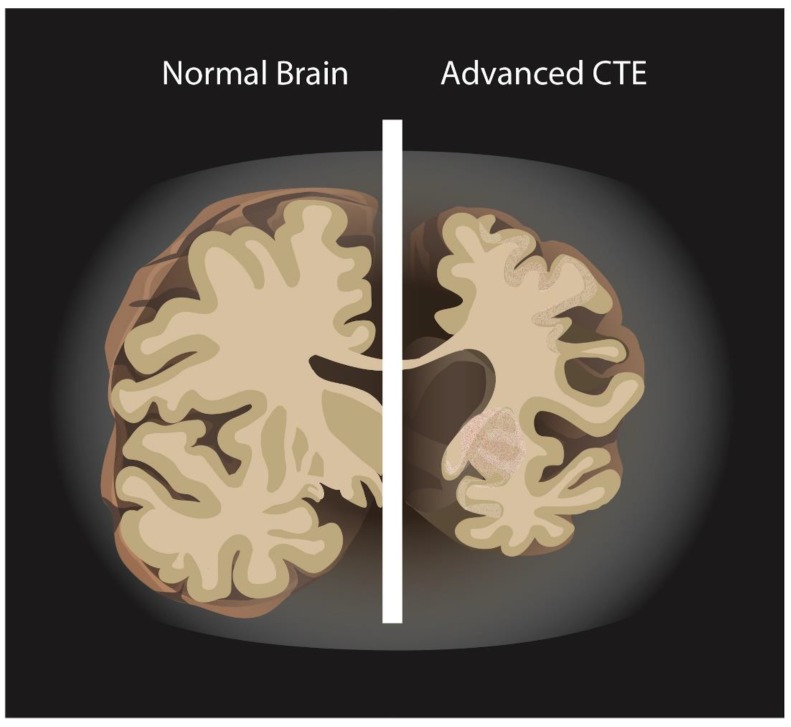
The National Institute of Neurological Disorders and Stroke (NINDS) defined CTE in 2015 as the abnormal and irregular accumulation of hyperphosphorylated tau (p-tau) in neurons and astroglia around small blood vessels in the cortical sulci [8]. Gross pathology also includes decreased brain weight, enlarged lateral and third ventricles, thinned corpus callosum, fenestrated cavum septum pellucidum and cerebellar tonsillar scarring/loss (Figure 1) [7,9,10]. With repetitive concussions, a progressive spectrum of behavioral, cognitive, and/or motor deficits can manifest 8–10 years [9]. Symptoms include irritability, impulsivity, aggression, depression, short-term memory loss, and suicidal risk; advanced stages are dementia, speech and gait disturbances, and parkinsonism that may overlap with tauopathies such as Alzheimer’s disease and frontotemporal dementia. The diagnosis of CTE through postmortem neuropathology makes understanding of its incidence difficult [11,12,13,14].
Figure 1.
Normal brain vs. Chronic traumatic encephalopathy (CTE).
There is considerable interest in genetic predispositions that may influence MTBI recovery, since not all patients with repetitive brain trauma will develop CTE [15,16]. The ability to identify individuals early on who are at risk takes precedence. Allelic variants of the apolipoprotein E (APOE) gene may be predictors for impaired recovery after MTBI [17,18]. As the predominant lipid transporter in the brain, APOE has three molecular isoforms: APOE epsilon 2 (ε2), APOE epsilon 3 (ε3), APOE epsilon 4 (ε4). The six genotypes (ε2/ε2, ε3/ε3, ε4/ε4, ε2/ε3, ε2/ε4, ε3/ε4) vary in their capacity to maintain synaptic function, facilitate neuronal repair, and modulate inflammation following injury [19,20]. Transgenic mice with APOE-ε4 experience greater excitotoxicity, edema, and ischemia with head trauma [19,21,22]. APOE-ε4 has been shown to be a strong genetic risk factor for amyloid pathology (e.g., β-amyloid deposition, subsequent neuroinflammation and microglia activation) in Alzheimer’s disease [23,24,25,26]; however its association with tauopathies—the typical pathological hallmark of CTE—is less clear. Recent studies show that APOE-ε4 may associate with cerebrospinal fluid (CSF) levels of tau and p-tau [23,27,28], as well as possible associations and/or interactions between APOE and tauopathies in the setting of β-amyloid deposition.
Evidence in human cohorts has been equivocal, some having reported unfavorable outcome associated with APOE-ε4 [29,30,31,32,33,34], and others finding no association [35,36,37]. Chamelian et al. observed no association in patients with mild and moderate TBI [36], but in a large cohort of mild, moderate, and severe TBI, Teasdale et al. found worse recovery in children and young adults [37]. Thus, the clinical significance of APOE-ε4 with respect to neuronal repair and synaptic plasticity deserves further study with specific TBI subpopulations. The challenges of investigating APOE genotypes in patients suffering repetitive MTBI and risk developing CTE include the heterogeneity of injury mechanisms, confounding demographics and comorbidities, and the lack of large-scale prospective studies. Towards this goal, we comprehensively review and evaluate the evidence to date on the association of APOE-ε4 carriers with functional outcomes after MTBI and the diagnosis of CTE.
2. Methods
Study Selection
A comprehensive literature search was conducted using the National Library of Medicine PubMed database for all studies published on the association of APOE genotypes with MTBI and/or CTE. Articles published in English through 12 June 2018 were candidates for inclusion using the following search criteria: ((chronic traumatic encephalopathy [title/abstract/MeSH terms] or mild traumatic brain injury [title/abstract/MeSH Terms] or concussion [title/abstract/MeSH Terms]) and apolipoprotein [title/abstract/MeSH Terms]). Two study authors (H.D., A.O.) independently evaluated each article and its accompanying references for scientific merit, with focus on APOE allele status in adult patients who experienced MTBI and/or developed CTE, and reached consensus regarding the inclusion of each reference into the current review. Any disagreements were adjudicated independently by the senior author (J.K.Y.). Informed consent was not applicable to this study as it involves no active human subjects.
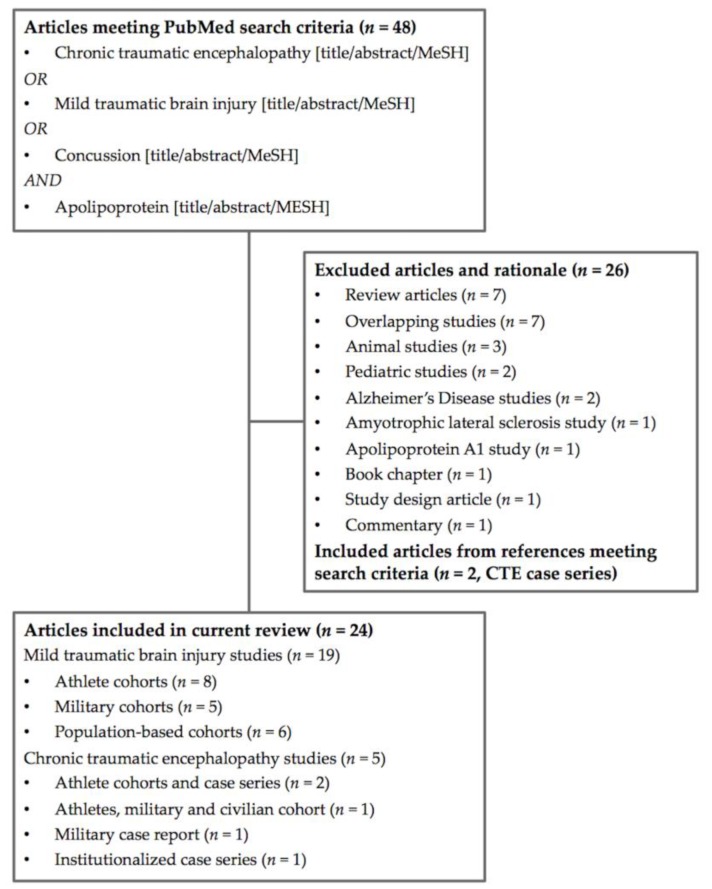
Of the 48 unique articles identified, 26 were removed due to the lack of applicability to the current review (seven review papers, seven overlapping studies, three animal studies, two pediatric studies, two studies on Alzheimer’s disease, one on amyotrophic lateral sclerosis, one on apolipoprotein A1, one on study design, one book chapter, and one commentary) (Figure 2). Two articles from the accompanying references on CTE case series, were included [15,38].
Figure 2.
Flowchart of included studies.
A final total of 24 articles, of which 19 studies were on MTBI (eight athletic (four prospective, four retrospective), five military (all retrospective), six population-based (all prospective)) and five studies were on CTE (three sports-related and military case series, one military case report, one institutionalized case series) were deemed fit for inclusion in the current review (Table 1).
Table 1.
Summary of included studies and findings for APOE allelic variants.
| Search Criteria [Title/Abstract/MeSH Terms]: (Chronic Traumatic Encephalopathy or Mild Traumatic Brain Injury or Concussion) and Apolipoprotein E | ||||||
|---|---|---|---|---|---|---|
| MTBI in Athlete Cohorts (8 Studies) | ||||||
| Author and Year | Study Type | N | Sex; Age | Description | Outcome Measures | Results |
| Cochrane et al., 2018 | MTBI, prospective, athletes | 250 collegiate athletes (95 football, 58 baseball/softball, 67 soccer, 18 basketball, 2 cross-country/track and field) | 184 male, 66 female; 19.0 ± 1.3 years old | APOE-ε2 carriers (n = 28), APOE-ε3 carriers (n = 128), APOE-ε4 carriers (n = 68), 24% self-reported a history of prior concussion. | Self-reported history of concussions and neurocognitive performance from Immediate Post-concussion Assessment and Cognitive Testing (ImPACT). | Apo-ε4 carriers had significantly slower reaction time (p = 0.002) as measured by the ImPACT. |
| Kristman et al., 2008 | MTBI, prospective, athletes | 318 collegiate athletes (43 football, 26 field hockey, 32 basketball, 23 ice hockey, 45 lacrosse, 49 rugby, 53 soccer, 47 volleyball) | 164 male, 154 female, mean age 20.5 ± 2.4 years (range 17–31) | 79 (24.8%) APOE-ε4(+) athletes | Concussions in athletes were diagnosed by the sport-medicine team and verified by a sport-medicine physician. | In the proportional hazards model, presence of the APOE-ε4 was not significantly associated with concussion (p = 0.68). |
| Merritt et al., 2016 | MTBI, prospective, athletes | 42 collegiate athletes (sports not defined) | 35 male, 7 female; subjects with mild concussions (14.3% LOC); ε4 carriers aged 19.9 ± 1.4 years, noncarriers aged 20.0 ± 1.6 years | 15 (35.7%) APOE-ε4(+) athletes, and 27 (64.3%) APOE-ε4(−) athletes | Team physicians determined TBI and concussed athletes were referred for neuropsychological testing post-injury. The Post-Concussion Symptom Scale was used to evaluate self-report symptoms. Physical and cognitive symptom clusters were each dichotomized into “symptoms present” versus “symptoms absent” groups | ε4-carriers associated with “symptoms present” group; ε4(+) athletes more likely to endorse physical symptoms than ε4(−) athletes (odds ratio (OR) = 5.25 (1.33–20.76); p = 0.015)). For cognitive symptoms, ε4-carriers associated with “symptoms present” group; ε4(+) athletes more likely to endorse cognitive symptoms than ε4(−) athletes, (OR = 4.75 (1.23–18.41), p = 0.020) |
| Merritt et al., 2018 | MTBI, prospective, athletes | 57 collegiate athletes (16 football, 11 basketball, 8 lacrosse, 7 rugby, 7 hockey, 4 soccer, 2 wresting, 2 other). | 44 males, 13 females; ε4 carriers 20.3 ± 1.4 years old, ε4 noncarriers 20.3 ± 1.4 years old | 20 athletes (35.1%) APOE-ε4(+); 37 athletes (64.9%) APOE-ε4(−) | Neurocognitive test battery including learning and memory, attention, processing speed, and executive functions: Brief Visuospatial Memory Test, Hopkins Verbal Learning Test; Symbol-Digit Modalities Test; Vigil Continuous Performance Test; Digit Span Test from the WAIS-III; Trail-Making Test; Penn State University Cancellation Test; Stroop Color-Word Test; ImPACT. | No significant differences were seen between athletes with and without the APOE-ε4 allele when examining mean neurocognitive scores (all p > 0.05). However, ε4(+) subjects were more likely to show a greater number of impaired neurocognitive scores post-injury compared to ε4(−) athletes (p < 0.05). More ε4+ athletes (40.0%; 8 of 20) fell in the impaired group compared with ε4- athletes (16.2%; 6 of 37; p = 0.046). APOE-ε4(+) athletes demonstrated greater neurocognitive variability than athletes without APOE-ε4 (p < 0.05). |
| Abrahams et al., 2017 | MTBI retrospective, athletes (rugby) | 288 rugby athletes (121 high school, 116 club, 51 professional) | Males; controls younger than concussed group (19.2 ± 3.5 years vs. 20.5 ± 4.4 years; p = 0.008) | The concussed group (N = 160) reported 1.9 ± 1.0 prior concussions (45%: 1; 34.4%: 2; 8.8%: 3; 11.9%: 4 concussions) | Self-reported duration of symptoms (<1 week versus ≥1 week) | APOE-ε4 isoforms did not differ significantly between concussion and control groups. APOE-ε4 isoform frequency distribution did not differ significantly between duration of symptoms groups |
| Casson et al., 2014 | Chronic brain damage, retrospective cross-sectional, athletes | 45 retired National Football League (NFL) players | 45 males; 45.6 ± 8.9 years old (range, 30–60 years) | Athletes reported 6.9 ± 6.2 concussions (maximum 25) throughout their careers | MMSE, dysarthria, pyramidal system dysfunction, extrapyramidal system dysfunction, cerebellar dysfunction, depression, PHQ9, ImPACT. susceptibility weighted imaging (SWI) and diffusion tensor imaging (DTI) evaluation for brain injuries | APOE-ε4 allele present in 38% of players, a larger number than expected in the general male population (23–26%). No association of the APOE-ε4 genotype with anatomical magnetic resonance imaging (MRI), clinical neurologic, depression, or neuropsychological test results |
| Esopenko et al., 2017 | MTBI, retrospective, alumni athletes | 33 retired National Hockey League (NHL) players | 53 males; alumni athletes 54.3 ± 10.4 years old, controls 53.4 ± 10.2 years old, | Concussions in athletes were 4.8 ± 2.7; in controls were 0.6 ± 0.8; 9 alumni and 4 controls were ε4(+); 1 ε4/ε4, 2 ε2/ε4, rest were ε2/ε3 or ε3/ε3 | Self-reported history of concussion, cognitive function and questionnaires on psychosocial/psychiatric function | ε4-carriers associated with increased psychiatric complaints (p = 0.009) but not objective cognitive performance. Executive function associated with number of concussions after accounting for confounders (β = −0.55 and −0.39, p = 0.005 and p = 0.039 for concussion and age, respectively) |
| Tierney et al., 2010 | MTBI, retrospective, athletes | 196 collegiate athletes (163 football; 33 soccer) | 163 male football and 33 female soccer athletes, age was 19.7 ± 1.5 years old | 48 (24.5%) with 1 concussion, 9/48 (4.6%) with >1 concussions. ε2 and ε4 present in 35 (17.7%) and 62 (31.9%) athletes. | Self-reported history of concussions. | No association between ε4 and ε2 carriers and history of concussion. Significant association (OR = 9.8; p = 0.05) between carrying APOE rare alleles and prior concussions. |
| MTBI in Military Cohorts (5 Studies) | ||||||
| Author | Study Type | N | Sex; Age | Description | Outcome Measures | Results |
| Dretsch et al., 2017 | MTBI, retrospective, active-duty military | 458 military members from two brigade combat teams preparing to deploy to Iraq and Afghanistan | 430 male, 28 female; age was 26.0 ± 7.0 years | History of concussion in 36.5%, with 10.7% having 3+ concussions. 38% (162/430) of men with 1+ concussions, vs. 18% (5/28) of women | Self-reported history of concussions | APOE not associated with risk for concussions. Of ε3/ε4 or ε4/ε4 soldiers, 44.1% (41/93) had a history of one or more prior concussions compared with 34.5% (126/365) of the comparison group (OR = 1.50; p = 0.087) |
| Emmerich et al., 2016 | MTBI, retrospective, active-duty military | 120 demographically matched soldiers with prior deployment to Iraq or Afghanistan (21 with TBI, 34 with posttraumatic stress disorder (PTSD); 13 with TBI + PTSD; 52 controls) | 120 males; TBI subjects’ age was 25.9 ± 1.4 years, PTSD subjects’ age was 26.4 ± 1.3 years, TBI + PTSD subjects’ age was 29.9 ± 1.6 years old; control subjects’ age was 26.7 ± 1.0 years | 85 APOE-ε4(−) (control n = 37, TBI n = 16, PTSD n = 24, TBI + PTSD n = 8); APOE-ε4(+) n = 35 (control n = 15, TBI = 5, PTSD = 10, TBI + PTSD n = 5) | Self-reported history of TBI, including military-associated injury and all other traumas; alcohol use; medical history; prior deployments; current medications; PTSD symptoms; and depression. Blood samples for lipidomic analysis. | ε4(+) subjects exhibited higher plasma phospholipids levels than their ε4(−) counterparts within diagnostic groups. ε4 noncarriers showed decreased saturated fatty acids (SFA)- and monounsaturated fatty acids (MUFA)-containing phosphatidylethanolamine (PE) species for TBI, PTSD, and TBI+PTSD groups, compared with controls. ε4 carriers showed no significant differences between TBI and PTSD groups for SFA- and MUFA. Interaction between ε4-carriers and diagnosis of TBI+PTSD on MUFA-containing lysophosphatidylcholine (LPC) and lysophosphatidylethanolamide (LPE) species. |
| Han et al., 2009 | Mild to moderate TBI, retrospective, active-duty military | 53 military personnel | 42 male, 4 female; Mean age of APOE-ε4(+) was 22.6 ± 3.8 years, mean age of APOE-ε4(−) was 25.2 ± 6.1 years | 16 APOE-ε4(+), 30 APOE-ε4(−) | Job change (reduction in duties for any reason e.g., medical hold, rehabilitation or assignment to light/limited duties (n = 24), reduction due to TBI (n = 3), referral to Medical Board (n = 3), or administrative separation (n = 1)), using neuropsychological assessments | In ε4-carriers, job status was determined by a long-delay free recall on the CVLT-II. If the percent change between long-delay free recall and short-delay free recall (defined as ((long-delay free recall raw score) minus (short-delay free recall raw score))/(short-delay free recall raw score)) >3.55%, subjects correctly predicted as no change in work status (85.7% accuracy). If the percentage change was <3.55%, subjects were correctly predicted to have a change in their job status with 88.9% accuracy |
| Hayes et al., 2017 | MTBI, retrospective, veterans | 160 veterans of OEF/OIF and/or New Dawn | 149 male, 11 female; non-MTBI aged 32.9 ± 8.9 years, MTBI aged 30.6 ± 8.1 years | 55 with no MTBI, 105 with MTBI. ε4(+): 10/55 with no MTBI, 27/105 with MTBI | Linear models examined the main effect of APOE (ε4-carriers, n = 37; non-ε4 carriers, n = 123) and MTBI × APOE interaction factor on cortical thickness. | No main effect of APOE on cortical thickness; no MTBI/APOE interaction. |
| Nielsen et al., 2018 | MTBI, retrospective, veterans | 87 veterans with or without MTBI | Demographics not published | 47 veterans with MTBI and 40 controls | Hierarchical linear regression to evaluate the association between DNA methylation, MTBI, and APOE genotype with plasma APOE, controlling for age, sex, population structure, depression and PTSD | Plasma APOE associated with PTSD severity (p = 0.013). Higher APOE levels in ε3/ε3 compared to ε4 carriers (p = 0.031). Plasma APOE was associated with DNA methylation at CpG sites −877 (p = 0.021), and −775 (p = 0.014). The interaction factor ε4 × PTSD was associated with DNA methylation at CpG −675 (p = 0.009) |
| MTBI in Population-Based Cohorts (6 Studies) | ||||||
| Author | Study Type | N | Sex; Age | Description | Outcome Measures | Results |
| Lee et al., 2017 | MTBI, prospective, population-based | 189 patients from emergency departments (ED) of three hospitals | 76 male, 113 female; Mean age of ε4(+) was 42.2 ± 14.7 years and ε4(−) was 40.1 ± 15.2 years | 35 ε4(+), 154 ε4(−) | 1st week post-mTBI and 6th week post-mTBI) sleep assessments, using the Pittsburgh Sleep Quality Index (PSQI) | No difference in PSQI at baseline and week 6 between ε4-carriers and noncarriers. Both ε4 carriers and noncarriers exhibited improvement in overall PSQI scores between baseline and week 6 follow-up (carrier: baseline 8.3 ± 3.9, 6th week: 7.4 ± 4.9, p = 0.05; noncarrier: baseline 8.5 ± 4.4, 6th week: 8.1 ± 3.8, p = 0.03) |
| Liberman et al., 2002 | MTBI, prospective, population-based | 87 adult patients presenting with mild or moderate TBI to a shock trauma center | 48 males, 32 females; <30 years of age (n = 25), 30–49 years old (n = 28) and ≥50 years old (n = 27) | 18 ε4(+), 62 ε4(−) | 13 neuropsychological tests administered twice at 3 and 6 weeks post-injury | 90% with MTBI; 18 (22.5%) ε4-carriers, who had lower scores on 12 of 13 neuropsychological outcomes at visit 1 compared to noncarriers, 2 were significant (grooved pegboard test, p = 0.005; paced auditory serial addition task 2.8-s trial, p = 0.004). At visit 2, ε4(+) had lower adjusted mean scores on 11/13 neuropsychological outcomes, though none were statistically significant. |
| Muller et al., 2009 | MTBI, prospective, population-based | 59 patients with MTBI | 47 male, 12 female; Mean age 35.1 years (range 18–74) | 13 APOE-ε4(+), 46 APOE-ε4(−) | GCS in ED, head computed tomography (CT) and MRI, neurophysiological assessments at baseline and 6-months. Serum S100B was measured. | GCS < 15, TBI on CT/MRI, and serum S-100B > 0.14 μg/L predicted impaired cognitive performance at baseline and 6-months while APOE did not. APOE-ε4 genotype was the only independent factor significantly predicting less improvement from baseline to 6-months. |
| Sundstrom et al., 2007 | MTBI, prospective, population-based | 31 MTBI patients and 62 matched controls | 18 male, 13 female; Mean age 55.2 ± 13.6 years | APOE-ε4 present in 38.7% of MTBI subjects and controls | Self-reported pre and postinjury fatigue, anxiety, depression and sleep disturbance was compared within-group and between groups | In MTBI, fatigue was more commonly reported among ε4 carriers (58%) than noncarriers (32%). MTBI ε4-carriers were more often fatigued than controls with ε4 (58% vs. 17%, p = 0.02). No significant between-group differences between MTBI and controls without ε4 |
| Yang et al., 2015 | MTBI, prospective, population-based | 21 MTBI patients without dementia, 6 MTBI patients with dementia, and 10 controls without MTBI | 15 male, 22 female; (controls: 2 M, 8 F, aged 50.6 ± 6.8 years; MTBI without dementia: 9 M, 12 F, aged 53.7 ± 7.9 years; MTBI with dementia: 4 M, 2 F; aged 60.0 ± 7.5 years) | ε4 carriers: 5 of 21 MTBI without dementia, 4 of 6 MTBI with dementia, 1 of 10 controls | MMSE, amyloid-PET | ε4 frequency high in MTBI patients with dementia (p = 0.049). Linear regression between APOE-ε4 and average amyloid standardized uptake value ratio (SUVR) showed significant correlation for all subjects (p < 0.05) |
| Yue et al., 2017 | MTBI, prospective, population-based | 114 MTBI patients | 76 male, 38 female; aged 49.6 ± 13.6 for ε4(+); aged 39.7 ± 16.5 years for noncarriers | 79 ε4(−), 35 ε4(+) | 6-month verbal memory using the CVLT-II, including Short-Delay Free Recall (SDFR), Short-Delayed Cued Recall (SDCR), Long-Delay Free Recall (LDFR), and Long-Delay Cued Recall (LDCR). | ε4-carriers associated with long-delay verbal memory deficits (LDFR: B = −1.17 points, 95% CI (−2.33, −0.01), p = 0.049; LDCR: B = −1.58 (−2.63, −0.52), p = 0.004), and a marginal decrease on SDCR (B = −1.02 (−2.05, 0.00), p = 0.050). CT pathology was the strongest predictor of decreased verbal memory. |
| CTE in Athlete and Military Cohorts (4 Studies) | ||||||
| Author | Study Type | N | Sex; Age | Description | Outcome Measures | Results |
| Stern et al., 2013 | CTE, retrospective, athletes | 36 athletes (29 football (22 pro, 4 college, 3 high school), 3 hockey, 1 wrestling, 3 boxing (1 pro, 2 amateur)) with neuropathologically confirmed CTE | All male; aged 56.8 ± 21.9 years (range 17–98) | APOE-ε4 genotype distribution was 3% ε2/ε3, 63% ε3/ε3, 26% ε3/ε4, and 9% ε4/ε4 | Next-of-kin interviewed for neuropsychiatric, social/occupational histories, dementia, depression, changes in cognition, behavior, mood, motor function, and ADLs | Proportions of APOE genotypes (i.e., ε4/ε4, ε4 carriers, and ε4 noncarriers) in this CTE sample were significantly different from those found in an age-matched normative sample (p < 0.05). Primary difference between this CTE sample and population norms was a greater proportion of ε4/ε4 in this sample (p < 0.05). More ε4/ε4 in the cognition group than expected (p < 0.05). Relative proportions of APOE in the 10 subjects with dementia did not differ significantly from those seen in Alzheimer’s (p > 0.05) |
| Mckee et al., 2013 | CTE, retrospective, athletes, military veterans, and civilians | 80 athletes (22 veterans), 3 military veterans, 1 civilian with history of falls, 1 civilian with history of self-injurious head banging behavior; 18 age- and sex-matched controls | 84 males, 1 female; Mean age of 54.2 ± 23.3 years (age range 14–98) | Of all subjects, including controls, 21 were carriers of Apo-ε4, 5 were homozygous for Apo-ε4 | Post-mortem brains of subjects with histories of repetitive MTBI were analyzed for evidence of CTE. Hyperphosphorylated tau pathology ranged in severity from focal pathology in the frontal lobe to a more global tauopathy, allowing for a progressive staging of pathology in these subjects. APOE genotyping was performed | In the 68 subjects diagnosed with CTE, the proportion of carrying at least one APOE-ε4 allele was not significantly different than that observed in the general population (p = 0.334) |
| Omalu et al., 2011 | CTE, case series, athlete | 14 pro athletes (8 football, 4 wrestling, 1 boxing, 1 mixed martial arts, 3 high school football) | Subjects male; age range 16–52 years | ε3/ε3 in 6 athletes (60%), ε3/ε4 in 2 athletes (20%), ε2/ε3 in 1 athlete (10%), ε2/ε4 (10%) in 1 athlete. 9 of the pro athletes (90%) with at least 1 ε3 allele. 7 of 10 pro athletes with known APOE genotype had CTE (70%). For the 3 deceased high school football players, the APOE genotype in 1 case could not be determined (blood samples were not available), and the genotypes in the other 2 were ε3/ε3 and ε3/ε3 | Histochemical and immunohistochemical brain tissue analysis for CTE changes and apolipoprotein E genotyping | Three pro athletes carried APOE-ε4, two of which (ε3/ε4 genotype) were positive for CTE, and the remaining (ε2/ε4 genotype) negative for CTE |
| Omalu et al., 2011 | CTE, case report, military | Case report of a military individual | 27-year-old male | The APOE genotype was ε3/ε4 | Histochemical and immunohistochemical brain tissue analysis for CTE changes | Autopsy, as well as gross and histomorphological examination of this brain revealed CTE changes similar to those observed in USA athletes |
| CTE in an Institutionalized Cohort (1 Study) | ||||||
| Author | Study Type | N | Sex; Age | Description | Outcome Measures | Results |
| Shively et al., 2017 | Leucotomy, case series, institutionalized | 5 institutionalized patients with schizophrenia and history of surgical leucotomy, with post-diagnosis survival of >40 years | 2 male, 3 female; Ages were 67, 70, 77, 87, and 89 years | Three of 5 are APOE-ε4 carriers, with the other 2 having ε3/ε3 genotype | Immunohistochemistry for abnormally hyperphosphorylated tau, beta-amyloid, antigen CD68; H&E stains on tissue sections for general morphology/structure | The three ε4-carriers showed scattered β-amyloid plaques in the overlying gray matter, which were not seen in the two ε3/ε3 patients |
APOE: apolipoprotein E gene; CI: confidence interval; CT: computed tomography; LOC: loss of consciousness; MMSE: Mini Mental State Exam; OEF: Operation Enduring Freedom; OIF: Operation Iraqi Freedom; TBI: traumatic brain injury.
3. Results
3.1. Mild Traumatic Brain Injury in Athletes
Eight studies evaluated associations between APOE genotype and MTBI in athletes of various competitive levels (Table 1). While four studies did not note an association between APOE-ε4 carriers and MTBI outcomes, four others reported otherwise. Kristman et al., 2008, a prospective cohort of 318 various collegiate athletes (25% possessing APOE-ε4 allele), recorded 28 athletes experiencing concussions, with no association demonstrated between concussion incidence and ε4 [39]. In Tierney et al., 2010, a cross-sectional study of 229 football and female soccer college players (32% with ε4 allele), 48 athletes had prior documented concussion, which did not associate with APOE-ε4 [40]. Similarly, in 45 retired NFL players (38% having APOE-ε4 allele) with mean age of 46 years, a 7-year career span, and average number of seven concussions, pathologic neuroimaging findings and neuropsychological impairment did not vary with the genotype [41]. Lastly, a case-control analysis of 128 non-concussed controls and 160 previously concussed rugby players (average of two concussions per player) at all competitive levels did not detect differences in allele frequency between the groups, nor did self-report post-concussive symptoms differ in duration for concussed players [42].
Four investigations found an association with APOE-ε4 and neuropsychological outcomes following sports-related MTBI. In a prospective cohort of 42 college athletes (36% possessing ε4 allele), Merritt et al., 2016 measured post-concussive symptoms by using the Post-Concussion Symptom Scale (PCSS) within 10 days of MTBI [43]. The PCSS is a 22-item self-reporting measure showing ε4-positive athletes endorsing higher likelihood of physical and cognitive symptoms, with an odds ratio (OR) of 5.25 and 4.75 respectively. A group of 57 collegiate athletes on various teams (35% with ε4 allele) underwent a comprehensive neurocognitive battery across domains of learning, memory, attention, processing speed, executive functioning 14 days postinjury [44]. While mean neurocognitive scores did not differ between allelic groups, ε4-positive athletes exhibited a greater proportion of impaired neurocognitive scores and high-performance variability, which the authors attributed to less efficient and other nonspecific influences of the APOE-ε4 allele on cognitive processing.
Esopenko et al., 2017, consisting of 38 retired professional hockey players (28% with ε4) and 20 age-matched controls, found that psychiatric complaints in retired athletes were associated with possession of the ε4 allele [45]. In a cross-sectional analysis of 250 collegiate athletes (27% with ε4 allele, 24% with self-reported MTBI history) from various sports, baseline cognitive status were measured by Immediate Post-concussion Assessment and Cognitive Testing (ImPACT) [46]. The authors did not detect differences in concussion susceptibility attributable to APOE; however, the baseline reaction times of ε4 carriers were slower compared to other allele groups.
3.2. Mild Traumatic Brain Injury in Military Cohorts
Four of the five studies with active-duty personnel or veterans found no clear association between APOE-ε4, MTBI susceptibility and/or outcome measures (Table 1). In Dretsch et al., 2017, a retrospective cohort of 458 active-duty soldiers preparing for deployment (mean age 26 years old, 22% with ε4 allele), 36% self-reported prior history of concussion, APOE alleles did not associate with having a history of MTBI [47]. In a retrospective study of 160 veterans (mean age 33 years old, 23% with ε4 allele, 53% with military-related lifetime MTBI), Hayes et al., 2017 reported that while MTBI resulted in reduced cortical thickness measured on magnetic resonance imaging (MRI), the APOE loci did not interact with MTBI to affect cortical thickness [48].
Han et al., 2009 analyzed whether APOE genotype may contribute to change in job status, i.e., reduced duties following mild to moderate TBI in 46 active-duty members (35% with ε4 allele) [49]. Notably, the authors observed that a change in free delay recall on the California Verbal Learning Test-Second Edition (CVLT-II) predicted job status change only in ε4-positive subjects [49]. Pre-deployment data from 120 active-duty soldiers (mean age 27 years old, 29% with ε4 allele, 18% with MTBI history), Emmerich et al. observed that ε4-carriers with MTBI history were associated with increased levels of phospholipids, in particular lysophosphatidylcholine [50]. The APOE-ε4 protein is less efficient in transporting these lipids, which the authors proposed can exacerbate the effects of injury/disease. Lastly, Nielsen et al., 2018, a cross-sectional study of 47 veterans with MTBI and 40 control veterans, detected lower levels of plasma APOE in both groups carrying the ε4 allele [51]. The authors did not observe an association between APOE genotype and MTBI status, and found instead that the ε4 allele associated with APOE gene promoter methylation and conferred increased susceptibility to combat-related posttraumatic stress disorder (PTSD) [51].
3.3. Mild Traumatic Brain Injury in Population—Based Cohorts
In six prospective population-based studies, an association between APOE-ε4 genotype and MTBI outcome was found in five reports. Liberman et al., 2002 studied a longitudinal series of 72 presenting with mild and 8 with moderate TBI (mean age 41 years old, 23% with ε4 allele) presenting at a trauma center, who were administered neuropsychological testing at 3 and 6 weeks [52]. The first testing showed that ε4-carriers had lower scores on 12 of the 13 tests, of which two were significant- grooved pegboard and paced auditory serial addition task; scores remained lower on 11 of 13 tests by 6 weeks although none were significant, which the authors attributed to slowed recovery with ε4 following TBI [52]. In a prospective matched cohort in Sweden analyzed post-injury symptoms of 31 MTBI subjects (mean age 55 years, 39% with ε4 allele, mean follow-up 20 months) and 62 controls [53]. APOE-ε4 carriers with MTBI experienced more fatigue than noncarriers with MTBI (58% vs. 32%) and ε4 carrier controls (58% vs. 17%), whereas there was no difference in fatigue level between MTBI ε4 noncarriers and controls.
A prospective study in Norway included 59 MTBI patients (mean age 35 years, 22% with ε4 allele) who received a battery of neuropsychological tests during hospitalization and at 6 months. APOE genotype was not found to be a predictor of impairment at either time point; however ε4-positive patients, as with positive computed tomography (CT) findings, associated with reduced improvement in performance at 6 months [54]. In Yue et al., 2017, a prospective cohort of 114 MTBI patients (mean age 43 years, 28% with ε4 allele), verbal memory evaluation using the CVLT-II at 6 months post-injury revealed impaired long-delay free and cued recall for ε4 carriers, along with marginally decreased short-delay cued recall [55]. Yang et al., 2015, a retrospective cohort of 27 individuals with MTBI (mean age 54 years for those without dementia, 60 years with dementia, MTBI history 6 years ago, 30% with ε4 allele) and 10 age-matched controls, found the highest APOE-ε4 frequency in subjects with MTBI history plus development of dementia (0.250 vs. 0.143 for MTBI without dementia vs. 0.050 for controls) [56]. The authors suggested that APOE genotype can be one of many contributing factors to amyloid accumulation.
In 189 patients with MTBI (19% with ε4 allele, mean age 42 years for carriers, 40 years for noncarriers) evaluated at weeks 1 and 6 post-injury, Lee et al., 2017, using the Pittsburgh Sleep Quality Index (PSQI) did not show a difference in recovery of sleep disturbance by APOE status [57].
3.4. Chronic Traumatic Encephalopathy in Athletes and Veterans
This review examined evidence of APOE-ε4 genotype associating with CTE development, which is a postmortem pathologic diagnosis limited to case series and reports to date. Evidence on sports-related development of CTE encompassed three case series from McKee et al., Omalu et al., and Stern et al., involving athletes and veterans, the majority of whom were also athletes. In a cohort of 85 subjects with history of repetitive MTBI, 65 cases had confirmed CTE with available APOE genotyping (64 athletes and 21 veterans, mean age 60 years old, 29% with ε4 allele, 63% with CTE as sole diagnosis) [15]. The authors did not find the proportion of CTE patients with ε4 allele to be greater than the general population. The brains of 17 subjects (14 former professional athletes in football, wrestling, boxing, and martial arts; three high school football players) were examined after unexpected deaths by Omalu et al., 2011, and the causes of death were as follows: six, five, and three professional athletes died of accidental drug abuse related causes, suicide, and natural causes, respectively; three high school players died from acute accidental trauma while playing football [58]. The mean age was 36 years, and CTE was identified in 11 athletes (10 of 14 professional, 1 of 3 high school) with mean age of 41 years; APOE genotyping was available for 12 of 17 athletes and three of these subjects (25%) were determined to possess ε4 allele [58]. Two of 7 CTE-positive professional athletes were ε4-positive (29%), while none of the high school players had any evidence of CTE.
Stern et al., 2013 examined the brains of 36 former athletes with confirmed CTE (29 football players, 3 hockey players, 3 boxers, 1 wrestler; mean age 57 years; leading causes of death are systemic, suicide, overdose, and dementia-related; 35% with ε4 allele) and interviewed the next-of-kin for clinical symptomatology [38]. Ten of 36 subjects also had dementia and stage IV CTE based on severity of p-tau pathology [15]. Although authors did not observe a difference between the APOE genotypes of CTE subjects with dementia from those seen in patients with Alzheimer’s disease, notably they found a greater proportion of ε4 homozygotes in CTE patients than expected in a normal, age-matched population [38]. Two clinical subtypes of CTE were reported: one early in the course of the disease manifesting as behavior/mood impairments, and the other exhibiting cognitive impairment later in life. The authors suggested that APOE-ε4 susceptibility for CTE was largely driven by ε4 homozygotes in the cognitively impaired group [38].
Omalu et al., 2011 published the case report of a 27-year-old Marine Corps Iraqi war veteran, with APOE genotype ε3/ε4. The subject experienced repeated mortar blast exposures on active duty prior to honorable discharge and committed suicide by hanging, with subsequent biopsy demonstrating neuropathologic evidence of CTE [14]. Prior to his death, the subject reported persistent mood symptoms and neuropsychological testing revealed impairments diagnosed as PTSD. The authors concluded that the histochemical and immunohistochemical findings of multifocal, neocortical, and subcortical neurofibrillary tangles and neuritic threads were similar to CTE changes previously observed in athletes [14].
3.5. Chronic Traumatic Encephalopathy in Leucotomy Patients
Shively et al., 2017 studied post-mortem brain tissues of five institutionalized schizophrenic patients (mean age 78 years at death, 60% with ε4 allele) who received bilateral prefrontal leucotomy, i.e., iatrogenic axonal injury, 4 decades prior to death, which could have contributed to the development of CTE [59]. Results were compared to five age-matched schizophrenic patients (60% with ε4 allele) in the same institution who had not undergone leucotomy. Whereas p-tau and β-amyloid were not notable in the nonleucotomized group, all leucotomy cases had patterns of cortical p-tau distribution in adjacent gray matter that was pathognomonic of CTE lesions in addition to the ε4-carriers having scattered β-amyloid plaque formation. The authors concluded that these findings suggested APOE genotype and axonal injury were factors contributing to the development of CTE [59].
4. Discussion
There is growing interest over the past 2 decades to improve understanding and prognostication of long-term outcomes after MTBI, with focus on multidimensional risk factors. MTBI commonly occurs collegiate and professional sports, and morbidity is exacerbated by repeated mild trauma inherent in some sports activities [60,61,62]. Continued efforts to improve triage, monitoring and surveillance of patients presenting to the emergency department with concussive symptoms and during their acute follow-up period is increasingly recognized as critical for reducing morbidity. For military personnel (active-duty or retired), there is a high incidence of blast exposure in the battlefield. A possible link between acute MTBI and chronic impairments in subsets of individuals may relate to different APOE isoforms and their varying levels of protein function in lipid processing and neuroimmunological activation [63,64,65].
Clinical outcome measures across multiple domains are increasingly used to determine whether APOE-ε4 carriers are more susceptible to MTBI, fare worse during recovery, and are more prone to developing CTE through repetitive head trauma. Uncovering specific factors contributing to recovery heterogeneity may have profound implications on the patient suffering from concussion. Genetics may in part play a role to influence acute and chronic responses to trauma. In this review, we evaluate the literature on the strength of association of APOE-ε4 on MTBI and CTE in athletes, military personnel, and the general public, while also discussing the range of clinical measures used by each study.
4.1. Role of APOE in the Central Nervous System
The APOE protein is a well-known endogenous immunomodulatory agent synthesized in response to injury, and functions to modulate lipid transport, cell membrane and synaptic maintenance, mitochondrial energy production, neuronal repair, and synaptogenesis [63]. The APOE gene is located on chromosome 19 and is highly polymorphic, resulting in a range of genotypes. APOE ε2 and ε3 have two and one cysteine residues, respectively, capable of detoxifying cytotoxic products of lipid peroxidation, whereas ε4 has two arginine residues that lack such ability. Differences in the tertiary structure and charge distribution of the APOE-ε4 isoform impair its capability to orchestrate these functions. Evidence in the literature attributes APOE-ε4 with a proinflammatory state and dysregulation of cerebral perfusion [19,20,65,66,67], along with changes in the blood-brain-barrier and cerebral edema in mice models [68]. While the proinflammatory influence can confer an evolutionary survival advantage in populations with high-risk exposure to infectious diseases [64], it is detrimental in a variety of neurological disorders [63]. As a regulator of neuronal repair for deep cerebral structures including the hippocampus, entorhinal complex, parahippocampal gyrus, and basal ganglia, APOE modulates regions that are crucial to memory consolidation and sensitive to damage from blunt head trauma [69,70].
The best evidence linking APOE-ε4 with poor outcomes comes from studies of severe TBI, with patients experiencing worse cognitive and functional impairments, β-amyloid deposition, prolonged coma, as well as a synergistic influence on the risk of developing Alzheimer’s disease [33,71,72,73]. Understanding the role of APOE-ε4 in MTBI has been challenging, as the set of outcome measures to encompass the range of functional, mood, cognitive, and behavioral domains is expansive while focal deficits may be specific to the individual. However, progress has been made regarding the characterization of specific risk factors after MTBI. Likewise, chronic mild head trauma causing dementia pugilistica was first described 1928 in boxers and now studied in an increasing number of sports and military personnel [5]. Chronic traumatic encephalopathy can present after a latent period as a composite syndrome of mood, neuropsychiatric, and cognitive abnormalities [58]. The histomorphologic features of CTE in a football player were first described in Omalu et al., 2006 [74], which the authors further defined in 2011 with additional cases as a distinct cerebral tauopathy of neurofibrillary tangles (NFTs) and neuritic threads (NTs), with or without the presence of amyloid plaques [58]. In contrast to 28% of the population that possesses at least one APOE-ε4 at baseline [18], an estimated 57% of CTE individuals are carriers of the ε4 allele [75]. The potential for genetic predisposition is not entirely clear and challenging to study due to the need for neuropathologic diagnosis on autopsy, which limits sample size.
4.2. Evidence on APOE and Mild Traumatic Brain Injury
Current research on the association between APOE-ε4 and MTBI can be better understood through classifying the outcome measures of interest into four categories and evaluating the strength of findings according to each measure: (i) susceptibility for MTBI based on self-reported history of documented concussion, (ii) neuroimaging implications, (iii) acute to subacute/chronic functional disability, and (iv) test battery for neurocognitive and neuropsychological impairment.
Whether APOE-ε4 confers a genetic predisposition to TBI susceptibility has important ramifications on current standards of primary prevention, particularly for athletes and military personnel who possess the isoform. Four large athletic cohorts spanning several sports and competitive levels, and one study in active-duty soldiers examined self-reported history of concussions identified by sport-medicine professionals [39,40,42,46,47]. These studies consisted primarily of young adult males, for which APOE genotype did not impart increased risk of sustaining a MTBI. The proportion of ε4-carriers in athletes and soldiers ranged from 22–32%, similar to the general population. While the ε4 allele itself did not influence susceptibility, there was a 3-fold risk for subsequent concussions in subjects with prior concussions [39,76]. Future investigations on the possibility of polygenetic risk factors for MTBI will be of interest [40,51].
Intracranial damage from MTBI can be occult using current clinical standards of neuroimaging such as CT and conventional MRI. It is increasingly recognized that while CT-positive pathology indicates worse prognosis, CT-negative imaging is not necessarily a sensitive measure for the absence of intracranial injury. In fact, up to 30% of MTBI patients who are CT-negative can be MRI-positive for intracranial injury, specifically axonal shear and gliding contusions [77]. Yue et al., 2017 found that 25% of MTBI patients had intracranial pathology on initial head CT scan within 24 h of injury, and APOE-ε4 did not accurately predict the presence of acute CT-positive lesions [55]. Casson et al., 2014 conducted extensive MRI studies with susceptibility weighted imaging (SWI) and diffusion tensor imaging (DTI) in a cohort of retired professional football players experiencing a mean total of nineconcussions over their lifespan, 38% of whom were ε4 carriers [41]. While most players (87%) did not have MRI findings of brain injury, 13% had reduced fractional anisotropy values indicative of chronic injury, which correlated with APOE-ε4 carrier status. While APOE-ε4 may not predispose patients to radiographic evidence of TBI after a single injury, axonal injury is a progressive process rather than from a single event [78]. Hence the possibility of APOE-ε4 to confer susceptibility to white matter injury with repetitive MTBI deserves intensive prospective study.
Prior landmark studies by Teasdale et al. in 2005 and Ariza et al. in 2006 examined TBI patients across all injury severities and found APOE-ε4 carriers to have worse symptoms and functional recovery [37,79]. However, our review finds this genetic relationship less clear for MTBI. On one hand, ε4-positive college athletes were more likely to endorse physical and cognitive complaints at 1 week postconcussion [43] and fatigue on long-term follow-up [34]. However, in a large cohort of rugby players, Abrahams et al. did not find a difference in the duration of post-concussive symptoms, possibly in part due to the binary outcome measure of more or less than 1 week of symptoms [42]. It is known that MTBI recovery remains variable within the first few weeks, where intervention, rehabilitation, medical and/or behavioral management may impart greater effects than if instituted months postinjury. Secondary injury and evolving intracranial processes can impact brain physiology and recovery across acute and subacute recovery, where APOE may continue to modulate immune status and neuroinflammation [20,63,64]. On the other hand, a study on sleep disturbance did not find worse outcomes associated with APOE-ε4 [57], and Casson et al., 2014 reported a higher prevalence of depression in retired football players (33% vs. 15–20% in the general population) independent of APOE status [41].
There is an overall movement towards consensus measures across cognitive domains of learning and memory, attention, processing speed, executive function, and others after MTBI [80,81,82]. Results to date among studies have been mixed, both in general and in the context of APOE. Cognitive scores in concussed collegiate athletes (using the Brief Visuospatial Memory Test-Revised) and former athletes (using CogState battery and Cambridge Brain Science) did not differ in any subdomains by APOE genotype, except for ε4-athletes having greater score variability [44] and ε4-alumni self-reporting more psychiatric complaints [45]. When the CVLT-II was used; however, APOE-ε4 carriers suffering MTBI presenting to Level I trauma centers [55] and in the military [49] exhibited worse long-delay verbal memory compared to patients without ε4. Other notable differences include manipulative dexterity in motor function and auditory processing and flexibility at 3 weeks post-injury [52], and a global index incorporating these measures predicted less improvement in ε4 carriers at 6 months [54]. Thus, in contrast to the moderate to severe TBI literature, these studies highlight that after MTBI, specific subdomains of neurobehavioral outcomes, particularly those of memory consolidation, retrieval and processing, may be modulated and/or impacted by APOE-ε4 status.
4.3. Evidence on APOE and Chronic Traumatic Encephalopathy
Given recent developments in the diagnosis and staging of CTE these past two decades, our review shows that the relationship between APOE and CTE is in need for further study [15]. Of 112 total former athletes and veterans confirmed with CTE to date (with the majority being football players) who received APOE genotyping, 30% were ε4 carriers [15,38,58]. Systemic illness, suicide, and drug overdose were the most common causes of death of CTE patients. Along with mood lability and disinhibition, patients begin to exhibit progressive worsening of short-term memory loss, executive dysfunction, and loss of attention and concentration 8–10 years after experiencing repetitive MTBI [9]. Similar to impaired memory processing ε4-carriers suffering MTBI, ε4-individuals-particularly homozygotes-with CTE suffered worse cognitive difficulties (episodic memory, executive function, attention and concentration) prior to death, based on the medical records and blinded interviews conducted with next-of-kin [38].
In theory, because of neurotoxic effects on the mitochondria and cytoskeleton conferred by the dysfunctional APOE-ε4 isoform, elevated risks are present for neurodegeneration through widespread deposition of p-tau following repeated injury [83,84]. In the context of limited patient samples, however, no studies thus far have identified increased susceptibility for developing CTE with the ε4 allele. Findings of CTE rely heavily on former athletes with long careers, and a majority of the veterans with CTE had MTBI exposure through sports. The literature reveals that mean age at death ranged from 41 to 60 years, football was the most common sport, and the average career time was 12 to 15 years. Stages I to IV of CTE correlate with the severity of hyperphosphorylated tau pathology, although with multifocal axonal disruption and loss in deep cortex and white matter regardless of the CTE stage [9]. In the largest study to date [15], mean age and new symptomology for each progressive stage were as follows: 28 years old, headache and loss of attention/concentration; 44 years old, depression/lability and short-term memory loss; 56 years old, cognitive impairment, executive dysfunction, visuospatial abnormality; 77 years old, dementia and profound short-term memory loss.
Research in CTE, a progressive tauopathy with distinctive histologic findings and nonspecific clinical symptoms, through autopsy-based case series is limited by the ascertainment bias of using reports from the next-of-kin of the deceased. Additionally, current literature lacks matched controls with exposure of repetitive MTBI but did not develop CTE. Evidence to date does not have the strength to suggest APOE status as a predictor of developing CTE; however, clinical criteria for diagnosing CTE need to be further established to facilitate prospective cohort studies for validation.
4.4. Limitations and Future Directions
The goal of this investigation was to explore the possibility of APOE-ε4 influence on MTBI and CTE, and studies on other genes which may play similar roles were not included for analysis. Given the relatively small number of studies measuring a variety of outcome types in each patient cohort, no formal grading of the level of evidence or bias was performed, limiting this study to an overview of the diverse approaches underway in understanding the phenotypic manifestation of a possible genetic risk factor in the context of both MTBI and CTE. While the difference in verbal memory attributed to APOE-ε4 is statistically significant, its deleterious impact on recovery and generalizability to the populations at large remain uncertain, in part due to English language limitations inherent to the CVLT-II.
Several hypotheses have been proposed regarding the role of APOE-ε4 in neurodegeneration following head trauma, including but not limited to the deposition and clearance of Aβ peptides and formation of plaques, dysregulation of neuronal signaling, and abnormal phosphorylation of tau to form neurofibrillary tangles. However, the molecular mechanisms of these ε4-mediated detrimental effects remain largely unknown. Presently, CTE is a diagnosis that can only be made with neuropathological analysis from wide sampling of the brain. Whether there is a primary mechanism, such as overactivated extracellular signal-regulated kinase (ERK) or tau phosphorylation causing neuronal death (leading to CTE over time) [85], cannot be extrapolated using post-mortem brain tissue analysis.
The studies examined in the current review are also limited by age. In the athletic cohorts with MTBI, most studies (6 of 8) examined subjects with a mean age of 18–21 years, of which three studies showed decreases in neurocognitive tests in ε4-carriers. Of the five military studies, mean age was generally 20–30 years. The six population-based cohorts with MTBI consisted of an older population with mean age 35 to 55 years, of which ε4-carriers showed associations with decreased neurocognitive test performance, more subjective fatigue, and dementia. As CTE is a post-mortem diagnosis, most cases to date are in the older age range (mean age in 50s). Undoubtedly, age can be a modifier and a confounder of APOE-ε4 effects, and studies have shown age-dependent alterations in CSF beta-amyloid markers for APOE-ε4 carriers vs. noncarriers [86,87], as well as APOE genotype prevalence and associated risk [25,88]. Future studies targeting APOE associations with MTBI outcomes and CTE should accordingly evaluate and control for age.
The prevalence of age-related comorbidities in subjects with more severe stages of CTE, along with the presence of other neurological disorders such as motor neuron disease, Alzheimer’s disease, Lewy body disease, and frontotemporal degeneration, limit the generalizability of the studies included in this review. Furthermore, to aid understanding of MTBI exposure leading to CTE, additional history of the TBIs themselves are is needed, e.g., characteristics of each incident, frequency, and the time between subsequent concussions to allow for recovery. To date, of the 5 military studies with MTBI evaluated in the current review, the influence of APOE-ε4 status on outcome after MTBI remains unclear: one study of 458 active-duty subjects showed a trend of increased prior concussions in ε4-carriers, one study of 87 veterans showed interaction between ε4, PTSD and DNA methylation, one study of 120 veterans showed interactions between ε4 status and diagnosis of TBI and PTSD, one study of 53 active-duty subjects showed a relationship between job status and memory performance associated with ε4-carriers, and one study on cortical thickness was negative. Outcomes after military TBI are undoubtedly multifactorial, and future large genetic studies are necessary to delineate whether APOE and other genetic risk factors exist for the military setting. The effects of sports-related, military, and civilian-setting concussions need to be compared in detail to characterize the heterogeneous nature of MTBI. Future prospective investigations will be necessary not only to elucidate the primary mechanisms of APOE in mild head trauma but to understand its relationship with findings in neuroimaging, epigenetics, and biomarkers.
5. Conclusions
In general, presence of the APOE-ε4 allele does not increase the susceptibility for MTBI. Post-injury, the ε4 isoform of this immunomodulatory gene is associated with impaired cognition, most pronounced in the subdomains of memory consolidation, retrieval and processing. This may be in part due to decreased capacity by the ε4 protein to modulate neuronal repair in deep brain structures responsible for memory processing. APOE-ε4 carriers, with repetitive injury, are more likely to sustain white matter injury detectable on neuroimaging in the form of axonal damage. CTE is a progressive neurodegenerative process that manifests approximately a decade after repeated exposure to MTBI and/or concussion. While the proportion of CTE subjects with APOE-ε4 is no greater than the general population, ε4 carriers may exhibit elevated cognitive difficulties during the progression of their disease course. Future prospective studies are needed to validate APOE-ε4 status as a risk factor for impairment after MTBI, and to establish premortem clinical criteria of diagnosing CTE to better understand the role that APOE-ε4 may have early in the disease.
Author Contributions
Conceptualization, H.D., A.O., J.K.Y. Methodology, H.D., J.K.Y.; Validation, H.D., A.O., T.L., J.K.Y.; Formal Analysis, H.D., A.O., J.K.Y.; Investigation, H.D., A.O., P.S.U., E.M.G.-B., C.G.S., C.G.M., N.M., T.L., J.K.Y.; Resources, H.D., J.K.Y.; Data Curation, H.D., A.O., E.M.G.-B., J.K.Y.; Writing—Original Draft Preparation, H.D., A.O., P.S.U., E.M.G.-B., C.G.S., C.G.M., N.M., T.L., J.K.Y.; Writing—Review and Editing, H.D., A.O., P.S.U., E.M.G.-B., C.G.S., C.G.M., N.M., T.L., J.K.Y.; Visualization, H.D., E.M.G.-B., J.K.Y.; Supervision, N.M., T.L., J.K.Y.; Project Administration, H.D., J.K.Y.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Cassidy J.D., Carroll L.J., Peloso P.M., Borg J., von Holst H., Holm L., Kraus J., Coronado V.G., WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury Incidence, risk factors and prevention of mild traumatic brain injury: Results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J. Rehabil. Med. 2004;36:28–60. doi: 10.1080/16501960410023732. [DOI] [PubMed] [Google Scholar]
- 2.Arciniegas D.B., Anderson C.A., Topkoff J., McAllister T.W. Mild traumatic brain injury: A neuropsychiatric approach to diagnosis, evaluation, and treatment. Neuropsychiatr. Dis. Treat. 2005;1:311–327. [PMC free article] [PubMed] [Google Scholar]
- 3.Alexander M.P. Mild traumatic brain injury: Pathophysiology, natural history, and clinical management. Neurology. 1995;45:1253–1260. doi: 10.1212/WNL.45.7.1253. [DOI] [PubMed] [Google Scholar]
- 4.Millspaugh J.A. Dementia pugilistica. US Nav. Med. Bull. 1937;35:297–303. [Google Scholar]
- 5.Martland H.S. Punch Drunk. J. Am. Med. Assoc. 1928;91:1103–1107. doi: 10.1001/jama.1928.02700150029009. [DOI] [Google Scholar]
- 6.Critchley M. Hommage a Clovis Vincent. Maloine; Paris, France: 1949. Punch-drunk syndromes: The chronic traumatic encephalopathy of boxers. [Google Scholar]
- 7.Corsellis J.A.N., Bruton C.J., Freeman-Browne D. The aftermath of boxing. Psychol. Med. 1973;3:270–303. doi: 10.1017/S0033291700049588. [DOI] [PubMed] [Google Scholar]
- 8.McKee A.C., Cairns N.J., Dickson D.W., Folkerth R.D., Dirk Keene C., Litvan I., Perl D.P., Stein T.D., Vonsattel J.P., Stewart W., et al. The first NINDS/NIBIB consensus meeting to define neuropathological criteria for the diagnosis of chronic traumatic encephalopathy. Acta Neuropathol. 2015;131:75–86. doi: 10.1007/s00401-015-1515-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McKee A.C., Cantu R.C., Nowinski C.J., Hedley-Whyte E.T., Gavett B.E., Budson A.E., Santini V.E., Lee H.S., Kubilus C.A., Stern R.A. Chronic traumatic encephalopathy in athletes: Progressive tauopathy after repetitive head injury. J. Neuropathol. Exp. Neurol. 2009;68:709–735. doi: 10.1097/NEN.0b013e3181a9d503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pan J., Connolly I.D., Dangelmajer S., Kintzing J., Ho A.L., Grant G. Sports-related brain injuries: Connecting pathology to diagnosis. Neurosurg. Focus. 2016;40:E14. doi: 10.3171/2016.1.FOCUS15607. [DOI] [PubMed] [Google Scholar]
- 11.Bailes J.E., Cantu R.C. Head injury in athletes. Neurosurgery. 2001;48:26–45. doi: 10.1097/00006123-200101000-00005. discussion 45–46. [DOI] [PubMed] [Google Scholar]
- 12.Macciocchi S.N., Barth J.T., Alves W., Rimel R.W., Jane J.A. Neuropsychological functioning and recovery after mild head injury in collegiate athletes. Neurosurgery. 1996;39:510–514. doi: 10.1227/00006123-199609000-00014. [DOI] [PubMed] [Google Scholar]
- 13.Goldstein L.E., McKee A.C. Response to Comment on “Chronic Traumatic Encephalopathy in Blast-Exposed Military Veterans and a Blast Neurotrauma Mouse Model”. Sci. Transl. Med. 2012;4:157lr5. doi: 10.1126/scitranslmed.3004862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Omalu B., Hammers J.L., Bailes J., Hamilton R.L., Ilyas Kamboh M., Webster G., Fitzsimmons R.P. Chronic traumatic encephalopathy in an Iraqi war veteran with posttraumatic stress disorder who committed suicide. Neurosurg. Focus. 2011;31:E3. doi: 10.3171/2011.9.FOCUS11178. [DOI] [PubMed] [Google Scholar]
- 15.McKee A.C., Stern R.A., Nowinski C.J., Stein T.D., Alvarez V.E., Daneshvar D.H., Lee H.-S., Wojtowicz S.M., Hall G., Baugh C.M., et al. The spectrum of disease in chronic traumatic encephalopathy. Brain. 2013;136:43–64. doi: 10.1093/brain/aws307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bieniek K.F., Ross O.A., Cormier K.A., Walton R.L., Soto-Ortolaza A., Johnston A.E., DeSaro P., Boylan K.B., Graff-Radford N.R., Wszolek Z.K., et al. Chronic traumatic encephalopathy pathology in a neurodegenerative disorders brain bank. Acta Neuropathol. 2015;130:877–889. doi: 10.1007/s00401-015-1502-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Samatovicz R.A. Genetics and brain injury: Apolipoprotein E. J. Head Trauma Rehabil. 2000;15:869–874. doi: 10.1097/00001199-200006000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Graham D.I., Horsburgh K., Nicoll J.A., Teasdale G.M. Apolipoprotein E and the response of the brain to injury. Acta Neurochir. Suppl. 1999;73:89–92. doi: 10.1007/978-3-7091-6391-7_15. [DOI] [PubMed] [Google Scholar]
- 19.Chen Y., Lomnitski L., Michaelson D.M., Shohami E. Motor and cognitive deficits in apolipoprotein E-deficient mice after closed head injury. Neuroscience. 1997;80:1255–1262. doi: 10.1016/S0306-4522(97)00007-9. [DOI] [PubMed] [Google Scholar]
- 20.Vitek M.P., Brown C.M., Colton C.A. APOE genotype-specific differences in the innate immune response. Neurobiol. Aging. 2009;30:1350–1360. doi: 10.1016/j.neurobiolaging.2007.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Horsburgh K., Kelly S., McCulloch J., Higgins G.A., Roses A.D., Nicoll J.A.R. Increased neuronal damage in apolipoprotein E-deficient mice following global ischaemia. Neuroreport. 1999;10:837–841. doi: 10.1097/00001756-199903170-00031. [DOI] [PubMed] [Google Scholar]
- 22.Buttini M., Orth M., Bellosta S., Akeefe H., Pitas R.E., Wyss-Coray T., Mucke L., Mahley R.W. Expression of human apolipoprotein E3 or E4 in the brains of Apoe−/− mice: Isoform-specific effects on neurodegeneration. J. Neurosci. 1999;19:4867–4880. doi: 10.1523/JNEUROSCI.19-12-04867.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shinohara M., Koga S., Konno T., Nix J., Shinohara M., Aoki N., Das P., Parisi J.E., Petersen R.C., Rosenberry T.L., et al. Distinct spatiotemporal accumulation of N-truncated and full-length amyloid-β42 in Alzheimer’s disease. Brain. 2017;140:3301–3316. doi: 10.1093/brain/awx284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abner E.L., Neltner J.H., Jicha G.A., Patel E., Anderson S.L., Wilcock D.M., Van Eldik L.J., Nelson P.T. Diffuse Amyloid-β Plaques, Neurofibrillary Tangles, and the Impact of APOE in Elderly Persons’ Brains Lacking Neuritic Amyloid Plaques. J. Alzheimers Dis. 2018;64:1307–1324. doi: 10.3233/JAD-180514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heffernan A.L., Chidgey C., Peng P., Masters C.L., Roberts B.R. The Neurobiology and Age-Related Prevalence of the ε4 Allele of Apolipoprotein E in Alzheimer’s Disease Cohorts. J. Mol. Neurosci. 2016;60:316–324. doi: 10.1007/s12031-016-0804-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gonzalez B., Abud E.M., Abud A.M., Poon W.W., Gylys K.H. Tau Spread, Apolipoprotein E, Inflammation, and More: Rapidly Evolving Basic Science in Alzheimer Disease. Neurol. Clin. 2017;35:175–190. doi: 10.1016/j.ncl.2017.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hohman T.J., Dumitrescu L., Barnes L.L., Thambisetty M., Beecham G., Kunkle B., Gifford K.A., Bush W.S., Chibnik L.B., Mukherjee S., et al. Alzheimer’s Disease Genetics Consortium and the Alzheimer’s Disease Neuroimaging Initiative Sex-Specific Association of Apolipoprotein E with Cerebrospinal Fluid Levels of Tau. JAMA Neurol. 2018;75:989–998. doi: 10.1001/jamaneurol.2018.0821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Farfel J.M., Yu L., De Jager P.L., Schneider J.A., Bennett D.A. Association of APOE with tau-tangle pathology with and without β-amyloid. Neurobiol. Aging. 2016;37:19–25. doi: 10.1016/j.neurobiolaging.2015.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alexander S., Kerr M.E., Kim Y., Kamboh M.I., Beers S.R., Conley Y.P. Apolipoprotein E4 allele presence and functional outcome after severe traumatic brain injury. J. Neurotrauma. 2007;24:790–797. doi: 10.1089/neu.2006.0133. [DOI] [PubMed] [Google Scholar]
- 30.Jiang Y., Sun X., Gui L., Xia Y., Tang W., Cao Y., Gu Y. Correlation between APOE-491AA promoter in epsilon4 carriers and clinical deterioration in early stage of traumatic brain injury. J. Neurotrauma. 2007;24:1802–1810. doi: 10.1089/neu.2007.0299. [DOI] [PubMed] [Google Scholar]
- 31.Chiang M.-F., Chang J.G., Hu C.J. Association between apolipoprotein E genotype and outcome of traumatic brain injury. Acta Neurochir. 2003;145:649–653. doi: 10.1007/s00701-003-0069-3. discussion 653–654. [DOI] [PubMed] [Google Scholar]
- 32.Jordan B.D., Relkin N.R., Ravdin L.D., Jacobs A.R., Bennett A., Gandy S. Apolipoprotein E epsilon4 associated with chronic traumatic brain injury in boxing. JAMA. 1997;278:136–140. doi: 10.1001/jama.1997.03550020068040. [DOI] [PubMed] [Google Scholar]
- 33.Friedman G., Froom P., Sazbon L., Grinblatt I., Shochina M., Tsenter J., Babaey S., Yehuda B., Groswasser Z. Apolipoprotein E-epsilon4 genotype predicts a poor outcome in survivors of traumatic brain injury. Neurology. 1999;52:244–248. doi: 10.1212/WNL.52.2.244. [DOI] [PubMed] [Google Scholar]
- 34.Sundstrom A., Marklund P., Nilsson L.G., Cruts M., Adolfsson R., Van Broeckhoven C., Nyberg L. APOE influences on neuropsychological function after mild head injury: Within-person comparisons. Neurology. 2004;62:1963–1966. doi: 10.1212/01.WNL.0000129268.83927.A8. [DOI] [PubMed] [Google Scholar]
- 35.Millar K., Nicoll J.A.R., Thornhill S., Murray G.D., Teasdale G.M. Long term neuropsychological outcome after head injury: Relation to APOE genotype. J. Neurol. Neurosurg. Psychiatry. 2003;74:1047–1052. doi: 10.1136/jnnp.74.8.1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chamelian L., Reis M., Feinstein A. Six-month recovery from mild to moderate Traumatic Brain Injury: The role of APOE-epsilon4 allele. Brain. 2004;127:2621–2628. doi: 10.1093/brain/awh296. [DOI] [PubMed] [Google Scholar]
- 37.Teasdale G.M., Murray G.D., Nicoll J.A.R. The association between APOE epsilon4, age and outcome after head injury: A prospective cohort study. Brain. 2005;128:2556–2561. doi: 10.1093/brain/awh595. [DOI] [PubMed] [Google Scholar]
- 38.Stern R.A., Daneshvar D.H., Baugh C.M., Seichepine D.R., Montenigro P.H., Riley D.O., Fritts N.G., Stamm J.M., Robbins C.A., McHale L., et al. Clinical presentation of chronic traumatic encephalopathy. Neurology. 2013;81:1122–1129. doi: 10.1212/WNL.0b013e3182a55f7f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kristman V.L., Tator C.H., Kreiger N., Richards D., Mainwaring L., Jaglal S., Tomlinson G., Comper P. Does the Apolipoprotein ε4 Allele Predispose Varsity Athletes to Concussion? A Prospective Cohort Study. Clin. J. Sport Med. 2008;18:322–328. doi: 10.1097/JSM.0b013e31817e6f3e. [DOI] [PubMed] [Google Scholar]
- 40.Tierney R.T., Mansell J.L., Higgins M., McDevitt J.K., Toone N., Gaughan J.P., Mishra A., Krynetskiy E. Apolipoprotein E genotype and concussion in college athletes. Clin. J. Sport Med. 2010;20:464–468. doi: 10.1097/JSM.0b013e3181fc0a81. [DOI] [PubMed] [Google Scholar]
- 41.Casson I.R., Viano D.C., Haacke E.M., Kou Z., LeStrange D.G. Is There Chronic Brain Damage in Retired NFL Players? Neuroradiology, Neuropsychology, and Neurology Examinations of 45 Retired Players. Sports Health. 2014;6:384–395. doi: 10.1177/1941738114540270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Abrahams S., Mc Fie S., Patricios J., Suter J., Posthumus M., September A.V. An association between polymorphisms within the APOE gene and concussion aetiology in rugby union players. J. Sci. Med. Sport. 2018;21:117–122. doi: 10.1016/j.jsams.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 43.Merritt V.C., Arnett P.A. Apolipoprotein E (APOE) ε4 Allele Is Associated with Increased Symptom Reporting Following Sports Concussion. J. Int. Neuropsychol. Soc. 2016;22:89–94. doi: 10.1017/S1355617715001022. [DOI] [PubMed] [Google Scholar]
- 44.Merritt V.C., Rabinowitz A.R., Arnett P.A. The Influence of the Apolipoprotein E (APOE) Gene on Subacute Post-Concussion Neurocognitive Performance in College Athletes. Arch. Clin. Neuropsychol. 2018;33:36–46. doi: 10.1093/arclin/acx051. [DOI] [PubMed] [Google Scholar]
- 45.Esopenko C., Chow T.W., Tartaglia M.C., Bacopulos A., Kumar P., Binns M.A., Kennedy J.L., Müller D.J., Levine B. Cognitive and psychosocial function in retired professional hockey players. J. Neurol. Neurosurg. Psychiatry. 2017;88:512–519. doi: 10.1136/jnnp-2016-315260. [DOI] [PubMed] [Google Scholar]
- 46.Cochrane G.D., Sundman M.H., Hall E.E., Kostek M.C., Patel K., Barnes K.P., Ketcham C.J. Genetics Influence Neurocognitive Performance at Baseline but Not Concussion History in Collegiate Student-Athletes. Clin. J. Sport Med. 2017;28:125–129. doi: 10.1097/JSM.0000000000000443. [DOI] [PubMed] [Google Scholar]
- 47.Dretsch M.N., Silverberg N., Gardner A.J., Panenka W.J., Emmerich T., Crynen G., Ait-Ghezala G., Chaytow H., Mathura V., Crawford F.C., et al. Genetics and Other Risk Factors for Past Concussions in Active-Duty Soldiers. J. Neurotrauma. 2017;34:869–875. doi: 10.1089/neu.2016.4480. [DOI] [PubMed] [Google Scholar]
- 48.Hayes J.P., Logue M.W., Sadeh N., Spielberg J.M., Verfaellie M., Hayes S.M., Reagan A., Salat D.H., Wolf E.J., McGlinchey R.E., et al. Mild traumatic brain injury is associated with reduced cortical thickness in those at risk for Alzheimer’s disease. Brain. 2017;140:813–825. doi: 10.1093/brain/aww344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Han S.D., Duke Han S., Suzuki H., Drake A.I., Jak A.J., Houston W.S., Bondi M.W. Clinical, Cognitive, and Genetic Predictors of Change in Job Status Following Traumatic Brain Injury in a Military Population. J. Head Trauma Rehabil. 2009;24:57–64. doi: 10.1097/HTR.0b013e3181957055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Emmerich T., Abdullah L., Crynen G., Dretsch M., Evans J., Ait-Ghezala G., Reed J., Montague H., Chaytow H., Mathura V., et al. Plasma Lipidomic Profiling in a Military Population of Mild Traumatic Brain Injury and Post-Traumatic Stress Disorder with Apolipoprotein E ε4–Dependent Effect. J. Neurotrauma. 2016;33:1331–1348. doi: 10.1089/neu.2015.4061. [DOI] [PubMed] [Google Scholar]
- 51.Nielsen D.A., Spellicy C.J., Harding M.J., Graham D.P. Apolipoprotein E DNA methylation and posttraumatic stress disorder are associated with plasma ApoE level: A preliminary study. Behav. Brain Res. 2018 doi: 10.1016/j.bbr.2018.05.013. [DOI] [PubMed] [Google Scholar]
- 52.Liberman J.N., Stewart W.F., Wesnes K., Troncoso J. Apolipoprotein E epsilon 4 and short-term recovery from predominantly mild brain injury. Neurology. 2002;58:1038–1044. doi: 10.1212/WNL.58.7.1038. [DOI] [PubMed] [Google Scholar]
- 53.Sundström A., Nilsson L.G., Cruts M., Adolfsson R., Van Broeckhoven C., Nyberg L. Fatigue before and after mild traumatic brain injury: Pre–post-injury comparisons in relation to Apolipoprotein E. Brain Inj. 2007;21:1049–1054. doi: 10.1080/02699050701630367. [DOI] [PubMed] [Google Scholar]
- 54.Müller K., Ingebrigtsen T., Wilsgaard T., Wikran G., Fagerheim T., Romner B., Waterloo K. Prediction of time trends in recovery of cognitive function after mild head injury. Neurosurgery. 2009;64:698–704. doi: 10.1227/01.NEU.0000340978.42892.78. discussion 704. [DOI] [PubMed] [Google Scholar]
- 55.Yue J.K., Robinson C.K., Burke J.F., Winkler E.A., Deng H., Cnossen M.C., Lingsma H.F., Ferguson A.R., McAllister T.W., Rosand J., et al. The TRACK-TBI Investigators Apolipoprotein E epsilon 4 (APOE-ε4) genotype is associated with decreased 6-month verbal memory performance after mild traumatic brain injury. Brain Behav. 2017;7:e00791. doi: 10.1002/brb3.791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yang S.T., Hsiao I.T., Hsieh C.J., Chiang Y.H., Yen T.C., Chiu W.T., Lin K.J., Hu C.J. Accumulation of amyloid in cognitive impairment after mild traumatic brain injury. J. Neurol. Sci. 2015;349:99–104. doi: 10.1016/j.jns.2014.12.032. [DOI] [PubMed] [Google Scholar]
- 57.Lee H.H., Yeh C.T., Ou J.C., Ma H.P., Chen K.Y., Chang C.F., Lai J.H., Liao K.H., Lin C.M., Lin S.Y., et al. The Association of Apolipoprotein E Allele 4 Polymorphism with the Recovery of Sleep Disturbance after Mild Traumatic Brain Injury. Acta Neurol. Taiwan. 2017;26:13–19. [PubMed] [Google Scholar]
- 58.Omalu B., Bailes J., Hamilton R.L., Kamboh M.I., Hammers J., Case M., Fitzsimmons R. Emerging histomorphologic phenotypes of chronic traumatic encephalopathy in American athletes. Neurosurgery. 2011;69:173–183. doi: 10.1227/NEU.0b013e318212bc7b. discussion 183. [DOI] [PubMed] [Google Scholar]
- 59.Shively S.B., Edgerton S.L., Iacono D., Purohit D.P., Qu B.-X., Haroutunian V., Davis K.L., Diaz-Arrastia R., Perl D.P. Localized cortical chronic traumatic encephalopathy pathology after single, severe axonal injury in human brain. Acta Neuropathol. 2017;133:353–366. doi: 10.1007/s00401-016-1649-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Buzas D., Jacobson N.A., Morawa L.G. Concussions from 9 Youth Organized Sports: Results from NEISS Hospitals Over an 11-Year Time Frame, 2002–2012. Orthop. J. Sports Med. 2014;2 doi: 10.1177/2325967114528460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Baker R.J., Patel D.R. Sports related mild traumatic brain injury in adolescents. Indian J. Pediatr. 2000;67:317–321. doi: 10.1007/BF02820676. [DOI] [PubMed] [Google Scholar]
- 62.Lau B., Lovell M.R., Collins M.W., Pardini J. Neurocognitive and symptom predictors of recovery in high school athletes. Clin. J. Sport Med. 2009;19:216–221. doi: 10.1097/JSM.0b013e31819d6edb. [DOI] [PubMed] [Google Scholar]
- 63.Mahley R.W., Weisgraber K.H., Huang Y. Apolipoprotein E4: A causative factor and therapeutic target in neuropathology, including Alzheimer’s disease. Proc. Natl. Acad. Sci. USA. 2006;103:5644–5651. doi: 10.1073/pnas.0600549103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Finch C.E., Morgan T.E. Systemic inflammation, infection, ApoE alleles, and Alzheimer disease: A position paper. Curr. Alzheimer Res. 2007;4:185–189. doi: 10.2174/156720507780362254. [DOI] [PubMed] [Google Scholar]
- 65.Guo L., LaDu M.J., Van Eldik L.J. A dual role for apolipoprotein e in neuroinflammation: Anti- and pro-inflammatory activity. J. Mol. Neurosci. 2004;23:205–212. doi: 10.1385/JMN:23:3:205. [DOI] [PubMed] [Google Scholar]
- 66.Zlatar Z.Z., Bischoff-Grethe A., Hays C.C., Liu T.T., Meloy M.J., Rissman R.A., Bondi M.W., Wierenga C.E. Higher Brain Perfusion May Not Support Memory Functions in Cognitively Normal Carriers of the ApoE ε4 Allele Compared to Non-Carriers. Front. Aging Neurosci. 2016;8:151. doi: 10.3389/fnagi.2016.00151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kerr M.E., Kraus M., Marion D., Kamboh I. Advances in Experimental Medicine and Biology. Springer Nature International Publishing; New York, NY, USA: 1999. Evaluation of Apolipoprotein E Genotypes on Cerebral Blood Flow and Metabolism Following Traumatic Brain Injury; pp. 117–124. [DOI] [PubMed] [Google Scholar]
- 68.Methia N., André P., Hafezi-Moghadam A., Economopoulos M., Thomas K.L., Wagner D.D. ApoE deficiency compromises the blood brain barrier especially after injury. Mol. Med. 2001;7:810–815. doi: 10.1007/BF03401973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bigler E.D., Johnson S.C., Anderson C.V., Blatter D.D. Traumatic brain injury and memory: The role of hippocampal atrophy. Neuropsychology. 1996;10:333–342. doi: 10.1037/0894-4105.10.3.333. [DOI] [Google Scholar]
- 70.Bigler E.D., Anderson C.V., Blatter D.D., Andersob C.V. Temporal lobe morphology in normal aging and traumatic brain injury. AJNR Am. J. Neuroradiol. 2002;23:255–266. [PMC free article] [PubMed] [Google Scholar]
- 71.Teasdale G.M., Nicoll J.A., Murray G., Fiddes M. Association of apolipoprotein E polymorphism with outcome after head injury. Lancet. 1997;350:1069–1071. doi: 10.1016/S0140-6736(97)04318-3. [DOI] [PubMed] [Google Scholar]
- 72.Crawford F.C., Vanderploeg R.D., Freeman M.J., Singh S., Waisman M., Michaels L., Abdullah L., Warden D., Lipsky R., Salazar A., et al. APOE genotype influences acquisition and recall following traumatic brain injury. Neurology. 2002;58:1115–1118. doi: 10.1212/WNL.58.7.1115. [DOI] [PubMed] [Google Scholar]
- 73.Mayeux R., Ottman R., Maestre G., Ngai C., Tang M.X., Ginsberg H., Chun M., Tycko B., Shelanski M. Synergistic Effects of Traumatic Head Injury and Apolipoprotein-epsilon4 in Patients with Alzheimer’s Disease. Neurology. 1995;45:555–557. doi: 10.1212/WNL.45.3.555. [DOI] [PubMed] [Google Scholar]
- 74.Omalu B.I., DeKosky S.T., Minster R.L., Ilyas Kamboh M., Hamilton R.L., Wecht C.H. Chronic Traumatic Encephalopathy in a National Football League Player. Neurosurgery. 2006;59:1086–1093. doi: 10.1227/01.NEU.0000245601.69451.27. [DOI] [PubMed] [Google Scholar]
- 75.Gavett B.E., Stern R.A., McKee A.C. Chronic traumatic encephalopathy: A potential late effect of sport-related concussive and subconcussive head trauma. Clin. Sports Med. 2011;30:179–188. doi: 10.1016/j.csm.2010.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Schulz M.R., Marshall S.W., Mueller F.O., Yang J., Weaver N.L., Kalsbeek W.D., Bowling J.M. Incidence and risk factors for concussion in high school athletes, North Carolina, 1996–1999. Am. J. Epidemiol. 2004;160:937–944. doi: 10.1093/aje/kwh304. [DOI] [PubMed] [Google Scholar]
- 77.Yuh E.L., Mukherjee P., Lingsma H.F., Yue J.K., Ferguson A.R., Gordon W.A., Valadka A.B., Schnyer D.M., Okonkwo D.O., Maas A.I.R., et al. TRACK-TBI Investigators Magnetic resonance imaging improves 3-month outcome prediction in mild traumatic brain injury. Ann. Neurol. 2013;73:224–235. doi: 10.1002/ana.23783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Büki A., Povlishock J.T. All roads lead to disconnection?—Traumatic axonal injury revisited. Acta Neurochir. 2006;148:181–193. doi: 10.1007/s00701-005-0674-4. discussion 193–194. [DOI] [PubMed] [Google Scholar]
- 79.Ariza M., Pueyo R., Matarín Mdel M., Junqué C., Mataró M., Clemente I., Moral P., Poca M.A., Garnacho A., Sahuquillo J. Influence of APOE polymorphism on cognitive and behavioural outcome in moderate and severe traumatic brain injury. J. Neurol. Neurosurg. Psychiatry. 2006;77:1191–1193. doi: 10.1136/jnnp.2005.085167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hicks R., Giacino J., Harrison-Felix C., Manley G., Valadka A., Wilde E.A. Progress in developing common data elements for traumatic brain injury research: Version two—The end of the beginning. J. Neurotrauma. 2013;30:1852–1861. doi: 10.1089/neu.2013.2938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wilde E.A., Whiteneck G.G., Bogner J., Bushnik T., Cifu D.X., Dikmen S., French L., Giacino J.T., Hart T., Malec J.F., et al. Recommendations for the use of common outcome measures in traumatic brain injury research. Arch. Phys. Med. Rehabil. 2010;91:1650–1660. doi: 10.1016/j.apmr.2010.06.033. [DOI] [PubMed] [Google Scholar]
- 82.Broglio S.P., Kontos A.P., Levin H., Schneider K., Wilde E.A., Cantu R.C., Feddermann-Demont N., Fuller G.W., Gagnon I., Gioia G.A., et al. National Institute of Neurological Disorders and Stroke and Department of Defense Sport-Related Concussion Common Data Elements Version 1.0 Recommendations. J. Neurotrauma. 2018 doi: 10.1089/neu.2018.5643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Geddes J.F., Vowles G.H., Nicoll J.A., Révész T. Neuronal cytoskeletal changes are an early consequence of repetitive head injury. Acta Neuropathol. 1999;98:171–178. doi: 10.1007/s004010051066. [DOI] [PubMed] [Google Scholar]
- 84.Gavett B.E., Stern R.A., Cantu R.C., Nowinski C.J., McKee A.C. Mild traumatic brain injury: A risk factor for neurodegeneration. Alzheimers Res. Ther. 2010;2:18. doi: 10.1186/alzrt42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Harris F.M., Brecht W.J., Xu Q., Mahley R.W., Huang Y. Increased tau phosphorylation in apolipoprotein E4 transgenic mice is associated with activation of extracellular signal-regulated kinase: Modulation by zinc. J. Biol. Chem. 2004;279:44795–44801. doi: 10.1074/jbc.M408127200. [DOI] [PubMed] [Google Scholar]
- 86.Lautner R., Insel P.S., Skillbäck T., Olsson B., Landén M., Frisoni G.B., Herukka S.-K., Hampel H., Wallin A., Minthon L., et al. Preclinical effects of APOE ε4 on cerebrospinal fluid Aβ42 concentrations. Alzheimers Res. Ther. 2017;9:87. doi: 10.1186/s13195-017-0313-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sutphen C.L., Jasielec M.S., Shah A.R., Macy E.M., Xiong C., Vlassenko A.G., Benzinger T.L.S., Stoops E.E.J., Vanderstichele H.M.J., Brix B., et al. Longitudinal Cerebrospinal Fluid Biomarker Changes in Preclinical Alzheimer Disease During Middle Age. JAMA Neurol. 2015;72:1029–1042. doi: 10.1001/jamaneurol.2015.1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Farrer L.A., Cupples L.A., Haines J.L., Hyman B., Kukull W.A., Mayeux R., Myers R.H., Pericak-Vance M.A., Risch N., van Duijn C.M. Effects of age, sex, and ethnicity on the association between apolipoprotein E genotype and Alzheimer disease. A meta-analysis. APOE and Alzheimer Disease Meta Analysis Consortium. JAMA. 1997;278:1349–1356. doi: 10.1001/jama.1997.03550160069041. [DOI] [PubMed] [Google Scholar]