Abstract
(1) Background: South Korea ranked worst in sleep duration compared to other countries, but there are no clear healthcare programs to guarantee sufficient sleep. Studies are needed to suggest evidence and arouse public awareness of the negative effects of abnormal sleep duration. In this study, we investigated the relationship between biological age (BA) and sleep duration. (2) Methods: We used data from the Korea National Health and Nutrition Examination Surveys (KNHANES V-VI; 2010–2015, which is an annually cross-sectional study including 29,309 participants). We performed multiple linear regression to investigate the associations between sleep duration and differences in BA and chronological age (CA). (3) Results: A total of 14.22% of respondents had short sleep duration (less than 6 h per day) and 7.10% of respondents had long sleep duration (more than 8 h per day). People with long sleep duration had a positive correlation with difference between BA and CA (>8 h per day, β = 1.308, p-value = 0.0001; ref = 6~8 h per day, normal). Short sleep duration had an inverse trend with the difference, although the result was not statically significant. Associations were greater in vulnerable populations, such as low income, obese, or people with chronic diseases. (4) Conclusions: Excess sleep duration that is greater than the normal range was associated with increased BA. In particular, such relationships that are related to worsening BA were greater in patients with low income, obesity, and chronic diseases. Based on our findings, healthcare professionals should also consider the negative effects of excess sleep, not only insufficient sleep. Alternatives for controlling optimal sleep duration should be reviewed, especially with vulnerable populations.
Keywords: biological age, sleep duration, self-management, metabolism
1. Introduction
Sleep plays a major role in daily life by assisting physical and mental recovery. Deficiencies in sleep quality or duration can contribute to several health problems, including heart disease, hypertension, diabetes mellitus, and stroke [1,2,3,4,5]. Sleep is an essential factor for health, and its importance is now well-established. South Korea has experienced rapid social and economic developments since the late 20th century, and most people now have busy daily lives [6]. As a result, South Koreans have sleep difficulties. The Organization for Economic Cooperation and Development (OECD) reported that South Korea ranked in the worst level for sleep duration when compared to other countries (South Korea: 469 min per day, 18th/18; United States: 518 min, 2nd/18; UK: 503 min, 11th/18; and, OECD average: 502 min per day) [7].
Some programs and policies have been introduced to improve the quality and quantity of sleep. Nevertheless, problems that are related to sleep remain. Patients diagnosed with sleep disorders have exponentially increased, according to a report of the Health Insurance Review and Assessment Service (HIRA); 287,835 patients had sleep disorders in 2010, which increased to 494,915 patients with sleep disorders in 2016 [8]. Reflecting this situation, nap cafés that operate during lunchtime and target office workers have become popular in South Korea [9]. However, some studies suggest that excess sleep duration can also cause negative health outcomes. Optimal sleep duration, rather than merely increased sleep duration, is suggested as a key factor in managing sleep health [10,11].
To solve the emerging health problems that are related to sleep, increased public attention and healthcare resources are key factors. Thus far, few alternatives have been introduced due to the social atmosphere and limited awareness of sleep problems. In addition, other than programs for management of sleep apnea, there are no clear healthcare programs to promote sufficient sleep duration [12]. Thus, evidence is needed to arouse public awareness of the negative effects of abnormal sleep duration. Further information would be helpful for establishing optimal alternatives to abnormal sleep duration in South Korea.
In this study, we will investigate the relationship of sleep duration and biological age (BA). With aging, chronological age (CA) could no longer reflect physiological function, general health, or overall decline, because an individual’s health status depends on different self-management behaviors and characteristics [13,14]. Thus, an index that can substitute CA to evaluate whether actual health status is needed. BA, which is estimated by measuring health status biomarkers, has been used to estimate physiological function, overall health status, and aging. BA is a useful index that enables subjects to understand their health status and emphasizes the importance of a healthy lifestyle; it has attracted increasing attention since 2000, and many factors, such as socioeconomic status, nutrition, physical activity, and biochemical/hormonal mechanism that affect BA are now known [15,16,17,18]. However, sleep is a major part of daily life that was not assessed as a factor that could affect BA. To investigate the relationship between sleep duration and BA, we study the negative effects of abnormal sleep duration, including worsening BA and cardiovascular diseases.
2. Materials and Methods
2.1. Study Population
We used data from two Korea National Health and Nutrition Examination Surveys (KNHANES V and VI; 2010–2015). The KNHANES is a cross-sectional study conducted annually by the Korean Centers for Disease Control (KCDC) using a stratified, multistage, cluster sampling design. The surveys include three questionnaires: Health Interview Survey, Health Examination, and Nutrition Survey. All of the participants were interviewed by trained personnel during the health examination. In this study, respondents who did not provide data that would have enabled BA calculation and those <20 years of age were excluded, as were subjects who did not report their sleep duration. We ultimately included 29,309 eligible participants.
2.2. Variables
The BA that was used in this study was calculated with object for estimating risk of metabolism. First, correlation analysis between CA and metabolism diagnostic parameters, including waist circumstance, systolic blood pressure, diastolic blood pressure, fasting blood sugar level, triglycerides, and high-density lipoprotein cholesterol was performed. Systolic blood pressure and diastolic blood pressure were converted into mean arterial blood pressure for the exclusion of redundancy and application of both parameters. After then, principal component analysis (PCA) was conducted for age and the five metabolism diagnostic parameters. The factor with the highest eigenvalue was decided as the principle component, and BA score was calculated using the first principal component obtained. Regression analysis was performed while using the PCA variables as dependent variables and the five metabolism biomarkers as independent variables. The formula developed after this process for estimation of BA by sex is as follows [19,20,21]:
| BA in males = −76.0965 + 0.541 × (waist circumstance) + 0.271 × (mean blood pressure) + 0.213 × (fasting blood glucose level) + 0.059 × (triglyceride level) − 0.312 × (high-density lipoprotein cholesterol level) + 0.850 × (age) | (1) |
| BA in females = −66.530 + 0.484 × (waist circumstance) + 0.328 × (mean blood pressure) + 0.303 × (fasting blood glucose level) + 0.080 × (triglyceride level) − 0.282 × (high-density lipoproteins cholesterol level) + 0.601 × (age) | (2) |
These parameters that are related to metabolism, including waist circumstance, mean blood pressure, fasting blood glucose level, triglyceride level, and high-density lipoprotein cholesterol level in calculating BA were measured through health examination on survey date. Then, we calculated the difference between BA and CA (BA-CA) to evaluate the actual health status of each individual with reference to BA. If the difference was positive when subtracting CA from BA, the individual was considered to have a worse health status when compared to similar age groups. Thus, the difference was considered an outcome variable in this study.
The primary variable of interest was sleep duration which collected based on question about “How many hours do you usually sleep?” in Health Interview Survey. It was categorized as follows: (1) less than 6 h per day (low), (2) 6~8 h per day (normal), or (3) more than 9 h per day (high). We also included other covariates in this study. Based on the previous studies, the risk of metabolism that related to BA in this study were differed by characteristics of study population, including general and socioeconomic status. Therefore, we included general characteristics, such as sex, age, educational level, marital status, economic activity, and household income for controlling the difference due to socioeconomic status [22]. Subjects were grouped by age as follows: <30 years, 30–39 years, 40–49 years, 50–59 years, and ≥60 years. Marital status was defined as follows: married, divorced/separated/bereaved, and single. Also, the prevalence of metabolism, including five parameters, were correlated with increasing BMI [23]. Subjects were grouped by BMI as follows: BMI < 23 kg/m2, underweight or normal; BMI = 23–25, overweight; and BMI > 25, obese [24,25]. By the aspects of healthy behaviors, physical activity was closely associated with metabolism, and the alcohol intake or smoking had positive association with increasing risk [26,27]. Aerobic exercise habits was defined as whether people take a moderate exercise more than 150 min a week or a high-strength exercise more than 75 min a week. High-risk drinking was defined as consumption of more than seven (males) or five (females) drinks on a single occasion at least twice a week. On the other perspectives, stress is also risk factors in chronic symptoms, including metabolism [28]. Stress awareness was defined as people who responded as “frequently” for the question about “How many perceived stress in daily life?” Hypertension, dyslipidemia, and diabetes mellitus were included due to close associations with diagnosis of metabolism [29].
2.3. Statistical Analysis
We first examined the frequencies and percentages of the study population to suggest the distribution of the study population by each categorical variable. Next, we performed t-tests and analysis of variance (ANOVA) to identify relationships between independent variables, BA, and BA difference (BA-CA). Finally, we performed multiple linear regression to investigate the association between sleep duration and difference (BA-CA) after adjusting for covariates. In addition, we performed subgroup analyses by household income, BMI, and diagnosis of chronic diseases (hypertension, dyslipidemia, or diabetes mellitus). We applied a sampling weight to each participant in order to generalize the data. SAS version 9.4 (Cary, NC) was used for all of the analyses. Data used in this study was collected after approving by the KCDC Institutional Review Board, and all of the participants provided written informed consent (2010-02CON-21-C, 2011-02CON-06-C, 2012-01-EXP-01-2C, 2013-07CON-03-4C, and 2014-12EXP-03-5C). In addition, all data was anonymized to avoid identifying the individual.
3. Results
A total of 29,309 respondents participated in this study. Table 1 shows the distribution of the study population by each independent variable, including sleep duration. Among the study population, 14.22% of respondents had short sleep duration (less than 6 h per day) and 7.10% had long sleep duration (more than 8 h per day).
Table 1.
General characteristics of study population.
| Variables | N | % |
|---|---|---|
| Sleep duration | ||
| <6 | 4652 | 14.22 |
| 6~8 | 22,602 | 78.68 |
| >8 | 2055 | 7.10 |
| Sex | ||
| Male | 12,529 | 49.44 |
| Female | 16,780 | 50.56 |
| Age (years) | ||
| <30 | 3120 | 17.40 |
| 30~39 | 5209 | 20.31 |
| 40~49 | 5534 | 22.41 |
| 50~59 | 6028 | 20.03 |
| 60≤ | 9418 | 19.86 |
| Educational level | ||
| Under high school graduation | 18,158 | 55.65 |
| Bachelor’s degree | 9899 | 39.83 |
| Master’s degree or above | 1252 | 4.52 |
| Marital status | ||
| Married | 22,027 | 70.62 |
| Marriage problems | 3599 | 9.61 |
| Single | 3683 | 19.78 |
| Economic activity | ||
| Unemployed | 11,644 | 34.89 |
| Employed | 17,665 | 65.11 |
| Household income | ||
| Low | 5307 | 14.41 |
| Mid-low | 7524 | 26.04 |
| Mid-high | 8126 | 29.80 |
| High | 8352 | 29.75 |
| BMI | ||
| <23 | 12,807 | 44.21 |
| 23–25 | 6984 | 23.27 |
| >25 | 9518 | 32.52 |
| Aerobic exercise habits | ||
| Yes | 8304 | 31.40 |
| No | 21,005 | 68.60 |
| Smoking status | ||
| Smoker | 5722 | 24.42 |
| Ex-smoker | 6000 | 20.18 |
| Non-smoker | 17,587 | 55.40 |
| Alcohol intake | ||
| Less than twice a week | 26,273 | 86.94 |
| More than twice a week | 3036 | 13.06 |
| Stress awareness | ||
| Low | 21,916 | 73.32 |
| High | 7393 | 26.68 |
| Hypertension | ||
| Diagnosed | 6558 | 16.80 |
| None | 22,751 | 83.20 |
| Dyslipidemia | ||
| Diagnosed | 3720 | 9.92 |
| None | 25,589 | 90.08 |
| Diabetes Mellitus | ||
| Diagnosed | 2447 | 6.36 |
| None | 26,862 | 93.64 |
| Survey year | ||
| 2010 | 4921 | 13.92 |
| 2011 | 5568 | 18.01 |
| 2012 | 5162 | 17.75 |
| 2013 | 4751 | 17.02 |
| 2014 | 4352 | 16.24 |
| 2015 | 4555 | 17.06 |
| Total | 29,309 | 100.00 |
Table 2 shows the mean and standard deviation of BA and difference (BA-CA) for each categorical variable. Overall, the average BA was 49.75 years and the difference was 4.00 years. People with short sleep duration had higher BA than other groups. People with long sleep duration had a higher BA-CA difference (p-value < 0.0001). Higher BMI was associated with higher BA and BA-CA difference (p-value < 0.0001). Health behavior indicators of aerobic exercise, smoking, and alcohol also generally had positive trends with higher BA and BA-CA difference. Diagnosis of a chronic disease, such as hypertension, dyslipidemia, or diabetes mellitus showed a similar trend to BA and BA-CA difference.
Table 2.
The averages of biological age (BA) and its differences with chronological age (CA) in study population.
| Variables | BA | Difference (BA-CA) | ||||
|---|---|---|---|---|---|---|
| Mean | SD | p-Value | Mean | SD | p-Value | |
| Sleep duration | ||||||
| <6 | 61.53 | 21.12 | <0.0001 | 4.29 | 14.88 | <0.0001 |
| 6~8 | 52.94 | 21.23 | 3.75 | 14.14 | ||
| >8 | 54.62 | 24.74 | 4.62 | 14.63 | ||
| Sex | ||||||
| Male | 54.52 | 21.32 | <0.0001 | 3.62 | 14.68 | <0.0001 |
| Female | 54.35 | 21.98 | 4.10 | 14.00 | ||
| Age (years) | ||||||
| ~30 | 24.60 | 12.59 | <0.0001 | 0.34 | 11.80 | <0.0001 |
| 30~39 | 38.19 | 14.04 | 3.24 | 13.70 | ||
| 40~49 | 49.21 | 15.48 | 4.86 | 15.12 | ||
| 50~59 | 60.47 | 15.20 | 6.08 | 14.95 | <0.0001 | |
| 60+ | 72.47 | 14.50 | 3.47 | 14.16 | ||
| Educational level | ||||||
| Under high school graduation | 62.04 | 19.51 | <0.0001 | 4.92 | 14.91 | <0.0001 |
| Bachelor’s degree | 41.28 | 19.15 | 2.12 | 13.04 | ||
| Master’s degree or above | 47.87 | 18.86 | 3.05 | 13.23 | ||
| Marital status | ||||||
| Married | 56.23 | 19.22 | <0.0001 | 4.24 | 14.20 | 0.0159 |
| Marriage problems | 69.68 | 19.00 | 5.06 | 15.73 | ||
| Single | 28.68 | 16.62 | 0.69 | 12.88 | ||
| Economic activity | ||||||
| Unemployed | 58.16 | 23.09 | <0.0001 | 3.78 | 14.01 | 0.5913 |
| Employed | 51.96 | 20.37 | 3.97 | 14.48 | ||
| Household income | ||||||
| Low | 67.76 | 19.80 | <0.0001 | 4.32 | 15.00 | 0.0051 |
| Mid-low | 55.26 | 22.14 | 4.47 | 15.07 | ||
| Mid-high | 50.28 | 20.48 | 3.91 | 13.75 | ||
| High | 49.23 | 19.93 | 3.09 | 13.60 | ||
| BMI | ||||||
| <23 | 44.65 | 20.08 | <0.0001 | −3.28 | 11.04 | <0.0001 |
| 23–25 | 57.30 | 19.49 | 4.46 | 12.30 | ||
| >25 | 65.45 | 19.32 | 13.14 | 14.11 | ||
| Aerobic exercise habits | ||||||
| Yes | 51.39 | 21.47 | <0.0001 | 3.06 | 14.06 | <0.0001 |
| No | 55.62 | 21.68 | 4.22 | 14.37 | ||
| Smoking status | ||||||
| Smoker | 51.85 | 21.38 | <0.0001 | 5.21 | 15.85 | <0.0001 |
| Ex-smoker | 58.51 | 20.23 | 3.51 | 13.97 | ||
| Non-smoker | 53.86 | 22.10 | 3.60 | 13.84 | ||
| Alcohol intake | ||||||
| Less than twice a week | 54.61 | 21.59 | <0.0001 | 3.41 | 13.82 | <0.0001 |
| More than twice a week | 52.82 | 22.61 | 8.05 | 17.33 | ||
| Stress awareness | ||||||
| Low | 55.24 | 21.49 | 0.0827 | 3.63 | 13.97 | 0.0044 |
| High | 52.00 | 22.15 | 4.67 | 15.20 | ||
| Hypertension | ||||||
| Diagnosed | 72.75 | 15.80 | <0.0001 | 8.47 | 14.82 | <0.0001 |
| None | 49.14 | 20.25 | 2.58 | 13.86 | ||
| Dyslipidemia | ||||||
| Diagnosed | 69.89 | 17.03 | 0.073 | 8.80 | 15.93 | <0.0001 |
| None | 52.17 | 21.39 | 3.18 | 13.90 | ||
| Diabetes Mellitus | ||||||
| Diagnosed | 80.33 | 18.51 | <0.0001 | 16.45 | 18.62 | <0.0001 |
| None | 52.06 | 20.40 | 2.75 | 13.26 | ||
| Survey year | ||||||
| 2010 | 57.28 | 20.04 | <0.0001 | 5.01 | 14.01 | <0.0001 |
| 2011 | 54.01 | 22.27 | 3.47 | 14.59 | ||
| 2012 | 54.42 | 21.90 | 3.61 | 14.27 | ||
| 2013 | 52.16 | 21.74 | 3.57 | 14.22 | ||
| 2014 | 53.15 | 21.45 | 3.23 | 14.05 | ||
| 2015 | 55.41 | 22.32 | 4.50 | 14.50 | ||
| Total | 49.75 | 0.22 | 4.00 | 0.12 | ||
Table 3 shows the results of linear regression analysis for BA-CA difference to investigate the association with sleep duration. People with long sleep duration had a positive correlation with the difference between BA and CA (>8 h per day, β = 1.308, p-value = 0.0001; ref = 6~8 h per day, normal). Short sleep duration had an inverse trend with BA-CA difference, although the results were not statically significant. Females or those in the 40~49 age group had higher BA-CA differences than other groups. On the aspects of health behavior, people with no aerobic exercise, smoking, and alcohol had higher BA-CA differences. Higher stress in daily life was associated with higher BA-CA differences. The diagnosis of chronic diseases, such as hypertension, dyslipidemia, or diabetes mellitus had a positive correlation with higher BA-CA difference.
Table 3.
The results of multiple linear regression analysis for the association between sleep duration and differences in biological age (BA) with chronological age (CA).
| Variables | Differences | ||
|---|---|---|---|
| β | SE | p-Value | |
| Sleep duration | |||
| <6 | −0.376 | 0.239 | 0.1158 |
| 6~8 | Ref | - | - |
| >8 | 1.308 | 0.343 | 0.0001 |
| Sex | |||
| Male | −3.521 | 0.234 | <0.0001 |
| Female | Ref | - | - |
| Age (years) | |||
| ~30 | 4.039 | 0.453 | <0.0001 |
| 30~39 | 4.989 | 0.324 | <0.0001 |
| 40~49 | 5.462 | 0.312 | <0.0001 |
| 50~59 | 4.522 | 0.272 | <0.0001 |
| 60+ | Ref | - | - |
| Educational level | |||
| Under high school graduation | 0.440 | 0.384 | 0.2528 |
| Bachelor’s degree | −0.393 | 0.370 | 0.2881 |
| Master’s degree or above | Ref | - | - |
| Marital status | |||
| Married | Ref | - | - |
| Marriage problems | −0.137 | 0.349 | 0.6958 |
| Single | −0.383 | 0.373 | 0.3054 |
| Economic activity | |||
| Unemployed | Ref | - | - |
| Employed | −0.319 | 0.179 | 0.0745 |
| Household income | |||
| Low | 0.363 | 0.319 | 0.2555 |
| Mid-low | 0.528 | 0.257 | 0.0401 |
| Mid-high | 0.421 | 0.223 | 0.0600 |
| High | Ref | - | - |
| BMI | |||
| <23 | Ref | - | - |
| 23–25 | 7.794 | 0.215 | <0.0001 |
| >25 | 16.539 | 0.217 | <0.0001 |
| Aerobic exercise habits | |||
| Yes | −1.363 | 0.194 | <0.0001 |
| No | Ref | - | - |
| Smoking status | |||
| Smoker | Ref | - | - |
| Ex-smoker | −1.620 | 0.276 | <0.0001 |
| Non-smoker | −2.122 | 0.280 | <0.0001 |
| Alcohol intake | |||
| Less than twice a week | Ref | - | - |
| More than twice a week | 3.257 | 0.403 | <0.0001 |
| Stress awareness | |||
| Low | Ref | - | - |
| High | 0.738 | 0.213 | 0.0006 |
| Hypertension | |||
| Diagnosed | 2.470 | 0.274 | <0.0001 |
| None | Ref | - | - |
| Dyslipidemia | |||
| Diagnosed | 1.464 | 0.330 | <0.0001 |
| None | Ref | - | - |
| Diabetes Mellitus | |||
| Diagnosed | 12.879 | 0.476 | <0.0001 |
| None | Ref | - | - |
| Survey year | |||
| 2010 | −0.077 | 0.321 | 0.8091 |
| 2011 | −1.208 | 0.314 | 00.0001 |
| 2012 | −0.962 | 0.347 | 0.0057 |
| 2013 | −1.281 | 0.318 | <0.0001 |
| 2014 | −0.438 | 0.306 | 0.1527 |
| 2015 | Ref | - | - |
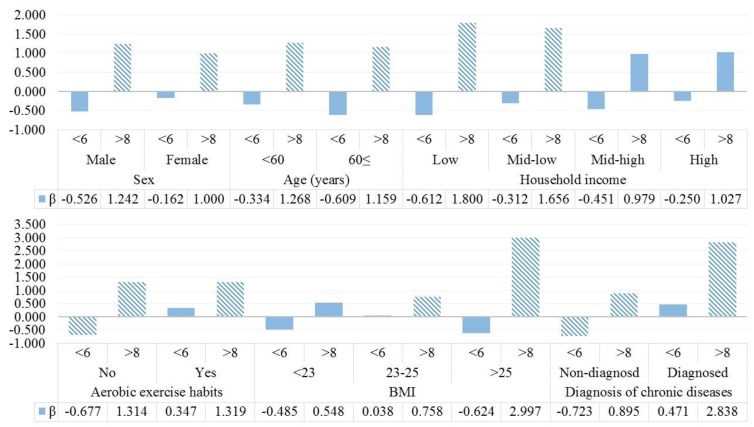
We also performed sub-group analysis for linear regression analysis between sleep duration and BA-CA differences to investigate BA-CA differences, according to household income, BMI, and diagnosis of chronic diseases. The results are shown in Figure 1. Larger differences between BA and CA with longer sleep duration were more prevalent in lower income groups than others. However, there were no statistically significant results in the short sleep group (less than 6 h per day). In the results by BMI or diagnosis of chronic diseases, the increases in BA with long sleep duration were more frequent in obese groups or people with the diagnosis of chronic diseases.
Figure 1.
The results of sub-group analysis for the association between sleep duration and difference in biological age (BA) with chronological (CA) according to household income, BMI, and diagnosis of chronic diseases. Hatched bars show the statistically significant results.
4. Discussion
Rapid socioeconomic development in South Korea has resulted in conflicting outcomes. Life is more convenient than in the past, but to survive under competition, most people experience worse mental health and stress than in the past. In particular, sleep duration is one major recent problem. Although sleep occupies about half of daily life, problems that are related to sleep have not been majorly addressed so far, and sleep alternatives are not sufficient [12]. The continuously poor management of sleep duration in South Korea must be addressed in near the future, and optimal management of sleep duration will play a major key role in sleep medicine [10]. This study focused on sleep duration and investigated the association between sleep duration and BA by considering the outcomes that can cause worsened sleep.
Our findings suggest that sleep duration longer than the normal range could cause negative health outcomes. In particular, it was associated with higher BA than CA, similar to previous studies. Short sleep duration could contribute to negative health outcomes, such as obesity, stroke, and other cardiovascular diseases [1,2,3,4,5,11]. However, excessive sleep duration can also worsen individual health outcomes [30]. Related studies showed that excessive sleep duration was associated with depression [31]. In addition, some studies have suggested that excessive sleep is associated with dementia, nervous anxiety, and other chronic diseases [32]. Even worse, sleep duration longer than the normal range could shorten life expectancy [33]. Although some previous findings also suggested negative results with short or excess sleep duration, such studies commonly focused on health outcomes, such as incidence of chronic diseases. Thus, we analyzed the association between sleep based on optimal sleep duration (6~8 h) and BA. In addition, negative health outcomes due to excessive sleep were frequently caused due to loss of sleep quality in the previous findings [34]. However, its association between difference with BA and excessive sleep in this study can be explained as following mechanism. First, the physical activity was would be key role in managing metabolism, but excessive sleep could bring the loss of physical activity. Second, people with lethargy are more likely to vulnerable in controlling self-management, such as sleep duration. On the other hand, deficit of sleep was not associated with difference between CA and BA; it could support the results by excessive sleep. With the emerging importance of self-management, findings related to BA and sleep duration will be helpful in improving individual health. A nationwide health policy with limited resources must be efficiently managed to ensure the proper control of latent risk factors.
Sub-group analysis showed more instances of worsening BA with excess sleep duration in specific groups. Low-income groups were more affected by the relationship between sleep duration and BA, likely because worsening outcomes due to excess sleep duration have a greater impact on those with limited healthcare resources. Results suggest that the presence of other chronic diseases was highly associated with worsening BA and longer sleep duration. Therefore, excess sleep duration has more influence on increased BA in economically or clinically vulnerable populations. Healthcare professionals and policymakers should consider problems that are related to sleep duration and review possible solutions to the problem of sleep duration. Because potential risk factors have greater effects on vulnerable populations, efficient alternatives must be considered.
Our study has some strengths when compared to previous findings. First, BA was used as the outcome variable in this study to evaluate the effect of shortage of or excess sleep duration. Previous studies have demonstrated several findings that are related to sleep duration. Because BA has recently been used as an indicator of health status and aging, we used it to show the effect of shortage of or excess sleep duration on overall health status. Therefore, the results of this study could indicate additional negative problems that are related to sleep. Remedies for this problem should be reviewed to target sleep problems. Second, the data used in this study was nationwide. Therefore, it has strengths related to external validity. The results of this study could be helpful in establishing healthcare alternatives for solving sleep problems in South Korea. Third, our data consisted of both clinical and survey data, allowing for the consideration of several characteristics related to sleep duration.
However, our study has some limitations related to the nature of the data. First, data that was used in this study was collected with a cross-sectional study design. Therefore, there are some problems related to the causal relationship between sleep duration and difference with BA; the excessive sleep could be caused by worsening health status. The results should be interpreted with caution. Second, in this study, based on a self-reporting survey, sleep duration was measured as response for “How many hours do you usually sleep?” This measurement can cause inaccuracies, including recall bias, because it is not objective sleep duration measurements, such as using actigraphy. However, due to the national research, there were limitations in making elaborate research, and the overall results of sleep duration were similar to previous findings. Third, BA was used as an outcome variable in this study. Several types of BA can be used to measure different targeted diseases. We used the BA related to metabolism to investigate worsening effects that are caused by shortage of or excess sleep duration. Thus, the results of this study could be limited in specific health outcomes and might not estimate some symptoms. Fourth, in previous studies, sleep quality was also associated with health outcomes. Due to limited data, this study only focused on sleep duration, not sleep quality. Therefore, the effect of sleep quality was not measured. Finally, the data used in this study was only collected from South Korean. Thus, we could not capture the diversity of ethnic, and our results cannot be generalized in other ethnics.
Despite some limitations in this study, our findings suggest that excess sleep duration has a positive correlation with higher BA, and this association is greater in vulnerable populations, such as those with low income, obesity, or chronic diseases. Therefore, strategies for managing optimal sleep duration in South Korea should be evaluated and compared to those of other OECD countries. To target efficient alternatives, healthcare professionals should focus on economic or clinically vulnerable populations.
5. Conclusions
Excess sleep duration is associated with increased BA. In particular, this relationship of worsened BA was greater in patients who are low income, obese, and have chronic diseases. Based on our findings, healthcare professionals should consider the negative effects of excess sleep, not only sleep shortage. To solve such problems, alternatives to promote optimal sleep duration should be reviewed, particularly in vulnerable populations.
Author Contributions
Conceptualization, K.-T.H. and D.W.K.; Methodology, D.W.K.; Software, D.W.K.; Validation, K.-T.H., D.W.K. and S.J.K.; Formal Analysis, K.-T.H.; Investigation, D.W.K.; Resources, S.J.K.; Data Curation, S.J.K.; Writing-Original Draft Preparation, K.-T.H.; Writing-Review & Editing, S.J.K.; Visualization, K.-T.H.; Supervision, S.J.K.; Project Administration, D.W.K.; Funding Acquisition, S.J.K.
Funding
This work was supported by the Soonchunhyang University Research Fund.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Knutson K.L., Ryden A.M., Mander B.A., Van Cauter E. Role of sleep duration and quality in the risk and severity of type 2 diabetes mellitus. Arch. Intern. Med. 2006;166:1768–1774. doi: 10.1001/archinte.166.16.1768. [DOI] [PubMed] [Google Scholar]
- 2.Baron K.G., Reid K.J., Kern A.S., Zee P.C. Role of sleep timing in caloric intake and BMI. Obesity. 2011;19:1374–1381. doi: 10.1038/oby.2011.100. [DOI] [PubMed] [Google Scholar]
- 3.Hermida R.C., Ayala D.E., Mojón A., Fernández J.R. Sleep-time blood pressure as a therapeutic target for cardiovascular risk reduction in type 2 diabetes. Am. J. Hypertens. 2012;25:325–334. doi: 10.1038/ajh.2011.231. [DOI] [PubMed] [Google Scholar]
- 4.Bassetti C.L. Sleep and stroke. Semin. Neurol. 2005;25:19–32. doi: 10.1055/s-2005-867073. [DOI] [PubMed] [Google Scholar]
- 5.Patel S.R., Hu F.B. Short sleep duration and weight gain: A systematic review. Obesity. 2008;16:643–653. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kwon S. Thirty years of national health insurance in South Korea: Lessons for achieving universal health care coverage. Health Policy Plan. 2008;24:63–71. doi: 10.1093/heapol/czn037. [DOI] [PubMed] [Google Scholar]
- 7.Organization for Economic Co-operation and Development (OECD) Society at a Glance 2009: OECD Social Indicators. OECD; Paris, France: 2009. [Google Scholar]
- 8.Health Insurance Review and Assessment Service Disease Statistics. [(accessed on 15 July 2018)]; Available online: http://opendata.hira.or.kr/home.do.
- 9.Korea Herald Cafes Tap into the Growing Demand for Resting and Healing Places in Crowded Cities. The Korea Herald. [(accessed on 10 July 2018)]; Available online: http://www.koreaherald.com/view.php?ud=20170427001154.
- 10.Buxton O.M., Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc. Sci. Med. 2010;71:1027–1036. doi: 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- 11.Heslop P., Smith G.D., Metcalfe C., Macleod J., Hart C. Sleep duration and mortality: The effect of short or long sleep duration on cardiovascular and all-cause mortality in working men and women. Sleep Med. 2002;3:305–314. doi: 10.1016/S1389-9457(02)00016-3. [DOI] [PubMed] [Google Scholar]
- 12.Han K.-T., Kim W., Kim S.J., Jang S.-Y., Ju Y.J., Chun S.Y., Lee S.G., Park E.-C. Sleep disorders and risk of hospitalization in patients with mood disorders: Analysis of the National Sample Cohort over 10 years. Psychiatry Res. 2016;245:259–266. doi: 10.1016/j.psychres.2016.08.047. [DOI] [PubMed] [Google Scholar]
- 13.Ingram D.K., Nakamura E., Smucny D., Roth G.S., Lane M.A. Strategy for identifying biomarkers of aging in long-lived species. Exp. Gerontol. 2001;36:1025–1034. doi: 10.1016/S0531-5565(01)00110-3. [DOI] [PubMed] [Google Scholar]
- 14.Finkel D., Whitfield K., McGue M. Genetic and environmental influences on functional age: A twin study. J. Gerontol. Ser. B. 1995;50:P104–P113. doi: 10.1093/geronb/50B.2.P104. [DOI] [PubMed] [Google Scholar]
- 15.Mitnitski A.B., Graham J.E., Mogilner A.J., Rockwood K. Frailty, fitness and late-life mortality in relation to chronological and biological age. BMC Geriatr. 2002;2:1. doi: 10.1186/1471-2318-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fishman L.S. Chronological versus skeletal age, an evaluation of craniofacial growth. Angle Orthod. 1979;49:181–189. doi: 10.1043/0003-3219(1979)049<0181:CVSAAE>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.Twisk J., Kemper H., van Mechelen W. The relationship between physical fitness and physical activity during adolescence and cardiovascular disease risk factors at adult age. The Amsterdam Growth and Health Longitudinal Study. Int. J. Sports Med. 2002;23:8–14. doi: 10.1055/s-2002-28455. [DOI] [PubMed] [Google Scholar]
- 18.Bae C.-Y., Kang Y.G., Kim S., Cho C., Kang H.C., Yu B.Y., Lee S.-W., Cho K.H., Lee D.C., Lee K., et al. Development of models for predicting biological age (BA) with physical, biochemical, and hormonal parameters. Arch. Gerontol. Geriatr. 2008;47:253–265. doi: 10.1016/j.archger.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 19.Kang Y.G., Suh E., Chun H., Kim S.-H., Kim D.K., Bae C.-Y. Models for estimating the metabolic syndrome biological age as the new index for evaluation and management of metabolic syndrome. Clin. Interv. Aging. 2017;12:253–261. doi: 10.2147/CIA.S123316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jia L., Zhang W., Jia R., Zhang H., Chen X. Construction formula of biological age using the principal component analysis. BioMed Res. Int. 2016;2016:8. doi: 10.1155/2016/4697017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kang Y.G., Suh E., Lee J.-W., Kim D.W., Cho K.H., Bae C.-Y. Biological age as a health index for mortality and major age-related disease incidence in Koreans: National health Insurance service–health screening 11-year follow-up study. Clin. Interv. Aging. 2018;13:429–436. doi: 10.2147/CIA.S157014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chichlowska K.L., Rose K.M., Diez-Roux A.V., Golden S.H., McNeill A.M., Heiss G. Individual and Neighborhood Socioeconomic Status Characteristics and Prevalence of Metabolic Syndrome. The Atherosclerosis Risk in Communities (ARIC) Study. Psychosom. Med. 2008;70:986–992. doi: 10.1097/PSY.0b013e318183a491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ervin R.B. Prevalence of metabolic syndrome among adults 20 years of age and over, by sex, age, race and ethnicity, and body mass index: United States. Natl. Health Stat. Rep. 2009;13:1–8. [PubMed] [Google Scholar]
- 24.Anuurad E., Shiwaku K., Nogi A., Kitajima K., Enkhmaa B., Shimono K., Yamane Y. The new BMI criteria for asians by the regional office for the western pacific region of WHO are suitable for screening of overweight to prevent metabolic syndrome in elder Japanese workers. J. Occup. Health. 2003;45:335–343. doi: 10.1539/joh.45.335. [DOI] [PubMed] [Google Scholar]
- 25.WHO Expert Consultation Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 26.Healy G.N., Wijndaele K., Dunstan D.W., Shaw J.E., Salmon J., Zimmet P.Z., Owen N. Objectively Measured Sedentary Time, Physical Activity, and Metabolic Risk: The Australian Diabetes, Obesity and Lifestyle Study (AusDiab) Diabetes Care. 2008;31:369–371. doi: 10.2337/dc07-1795. [DOI] [PubMed] [Google Scholar]
- 27.Park Y.-W., Zhu S., Palaniappan L., Heshka S., Carnethon M.R., Heymsfield S.B. The metabolic syndrome: Prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988–1994. Arch. Intern. Med. 2003;163:427–436. doi: 10.1001/archinte.163.4.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chandola T., Brunner E., Marmot M. Chronic stress at work and the metabolic syndrome: Prospective study. BMJ. 2006;332:521–525. doi: 10.1136/bmj.38693.435301.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alberti K.G.M., Zimmet P., Shaw J. The metabolic syndrome—A new worldwide definition. Lancet. 2005;366:1059–1062. doi: 10.1016/S0140-6736(05)67402-8. [DOI] [PubMed] [Google Scholar]
- 30.Jike M., Itani O., Watanabe N., Buysse D.J., Kaneita Y. Long sleep duration and health outcomes: A systematic review, meta-analysis and meta-regression. Sleep Med. Rev. 2017;39:25–36. doi: 10.1016/j.smrv.2017.06.011. [DOI] [PubMed] [Google Scholar]
- 31.Lippman S., Gardener H., Rundek T., Seixas A., Santiago M., Elkind M., Sacco R., Wright C., Ramos A. Sleep Duration is Associated with Depression in the Northern Manhattan Study (P1. 150) Neurology. 2016;86:1–150. [Google Scholar]
- 32.Benito-León J., Louis E.D., Villarejo-Galende A., Romero J.P., Bermejo-Pareja F. Long sleep duration in elders without dementia increases risk of dementia mortality (NEDICES) Neurology. 2014;83:1530–1537. doi: 10.1212/WNL.0000000000000915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kripke D.F., Garfinkel L., Wingard D.L., Klauber M.R., Marler M.R. Mortality associated with sleep duration and insomnia. Arch. Gen. Psychiatry. 2002;59:131–136. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 34.Grandner M.A., Drummond S.P.A. Who are the long sleepers? Towards an understanding of the mortality relationship. Sleep Med. Rev. 2007;11:341–360. doi: 10.1016/j.smrv.2007.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]