Abstract
Hyperthermia is a cancer treatment where tumor tissue is heated to around 40 °C. Hyperthermia shows both cancer cell cytotoxicity and immune response stimulation via immune cell activation. Immunogenic responses encompass the innate and adaptive immune systems, involving the activation of macrophages, natural killer cells, dendritic cells, and T cells. Moreover, hyperthermia is commonly used in combination with different treatment modalities, such as radiotherapy and chemotherapy, for better clinical outcomes. In this review, we will focus on hyperthermia-induced immunogenic effects and molecular events to improve radiotherapy efficacy. The beneficial potential of integrating radiotherapy with hyperthermia is also discussed.
Keywords: hyperthermia, immunotherapy, radiotherapy, combination therapy
1. Current State of Radiotherapy and Immunotherapy
Radiotherapy is a widely used, well-established anti-tumor treatment that has shown significant clinical outcomes. Utilizing ionizing radiation, radiotherapy generates excessive oxidative stress and induces DNA damage, such as single or double DNA strand breaks, and tumor cell deaths [1]. As radiation can penetrate the body, and can be accurately limited to the depth of interest, radiotherapy is a non-invasive and spatially specific strategy compared to other anti-tumor therapies [2]. However, some tumor cells can be radioresistant, showing resistance to radiation-induced oxidative stress and DNA damage-induced cell death through various intracellular pathways [3,4]. Although increased radiation dose is more likely to induce tumor cell deaths, an excessively high radiation dose can induce damage in adjacent normal tissue and related side effects. For this reason, several radiosensitization strategies have been developed for better therapeutic efficacy. Mostly, combinations of radiosensitizing chemotherapy and radiotherapy are used, providing better post-therapy outcomes [5]. In addition, immunotherapy, which elevates systemic immunity against tumor cells, has shown radiosensitizing effects and better therapeutic outcomes [6]. However, radioresistance has not been fully overcome, and current studies focus on novel strategies for enhancing therapeutic efficacy.
Immunotherapy enhances the immune cells’ ability to recognize and target tumor cells, leading to their elimination. The advantages of immunotherapy include high anti-tumor specificity and minimal side effects by utilizing the patient’s own immune system [7]. Current immunotherapies focus on suppressing tumor cell evasion using antibodies that inhibit immune checkpoint molecules, including cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4), programmed death 1 (PD-1), and programmed death-ligand 1 (PD-L1) [8]. Antibodies specific for these molecules are called immune checkpoint blockades, and include anti-CTLA-4 (ipilimumab) and anti-PD-1 (nivolumab and pembrolizumab) antibodies, which are United States Food and Drug Administration (FDA) approved for clinical treatment with significant therapeutic outcomes [8]. Furthermore, current studies covering the radiosensitization effect of immunotherapy suggest the potential of combining immunotherapy and radiotherapy [9]. However, the biggest obstacle in immunotherapy application is the relatively low efficacy, and difficulty in achieving tumor cell-specific immunogenicity, compared to other anti-tumor therapies [10]. Although immune checkpoint blockade antibodies should directly bind to the tumor cell surface for its effect, recent studies suggested that the limitation of immunotherapy is the inefficient delivery to tumor sites [11]. This was also supported by other studies that suggested a novel immune checkpointblockade delivery system, through conjugation with nanoparticles and homing molecules, for efficient delivery. However, the therapeutic significance was still low, and current immunotherapies need further modification for clinically meaningful immunogenic effects.
To better induce immunity against tumor cells, immunogenic therapeutic adjuvants were suggested, some of which showed significantly increased therapeutic efficacy with low normal tissue damage [12]. Recent studies also applied these immunogenic adjuvants to tumor cell sensitization against therapies. For example, platinum-based chemotherapies including cisplatin, carboplatin, and oxaliplatin are widely used as anti-tumor treatments, and show immunogenic effects through cell death induction and the release of death-associated molecular patterns, which activate pro-inflammatory signaling pathways [13]. Similarly, the immunogenic effects of other cytotoxic chemicals also supported this phenomenon [14,15]. However, these chemicals also showed cytotoxicity to normal tissues and induced severe side effects, which slows their clinical application [16,17]. Recently, immunogenic biological derivatives were suggested as an immunogenic approach with fewer side effects. Biological derivatives, such as peptides, glycosides, and natural products, have shown significant immunogenicity through immune cell activation and tumor cell deaths [18,19,20]. Although these studies supported the crucial role and promising potential of immunogenic anti-tumor therapies, neither these adjuvants nor immunotherapy could fulfill the demanding therapeutic efficacy and tumor cell-specific delivery, leaving them as major obstacles to overcome.
Alternatively, hyperthermia was recently suggested as an immunogenic treatment with spatial specificity and high efficacy [21]. And the modification of temperature and treatment duration can control the biological effects of hyperthermia treatment [22]. Furthermore, increased immunity by hyperthermia resulted in tumor cell sensitization against radiotherapy [23]. Although the significant anti-tumor effects of hyperthermia combined with radiotherapy were recently reported, a clinical protocol for the best outcome has not been devised yet. This suggested the need for a deeper understanding of the immunogenic effects of hyperthermia as an anti-tumor adjuvant for clinical applications with better outcomes. In this review, we summarize the current studies on the hyperthermia-induced immunogenicity, and the underlying molecular mechanisms for combining hyperthermia and radiotherapy. In addition, we also provide promising clinical significance for applying hyperthermia as an adjuvant to overcome radioresistance and enhance therapeutic efficacy.
2. The Immunogenic Effect of Hyperthermia
Hyperthermia treatment involves increasing the target site temperature to induce thermic stress, with an average temperature around 40 °C (39–43 °C, dependent on therapeutic strategies). In previous studies, hyperthermia was typically reported to modulate local pro-inflammatory responses, immune activation, cell death, and microenvironmental changes in the target sites, which were mostly mediated by specific chaperone proteins called heat shock proteins (Hsps) [24]. Highamounts of Hsps are expressed upon environmental stress, including heat shock, oxidative stress, and chemical stress [25]. Hsps prevent and reverse heat-induced protein misfolding, and recover heat-induced cellular damages through chaperone activity. In addition, some Hsps are extracellularly exposed and function as signaling molecules to induce a heat shock response in adjacent cells. Transcriptional heat shock response is mediated by the heat shock transcription factor (HSF) via the “chaperone titration model” [26]. In this model, HSF is bound to Hsp70 and Hsp90 in the cytosol in non-stressed circumstances. Upon heat shock, Hsp70 and Hsp90 dissociate from HSF to act as chaperones. The free HSFs form trimer and move to the nucleus where they have transcription factor activity. As responses after hyperthermia treatment are also mediated by Hsps and HSF, understanding of Hsp and HSF molecular mechanisms can explain the biological role of hyperthermia.
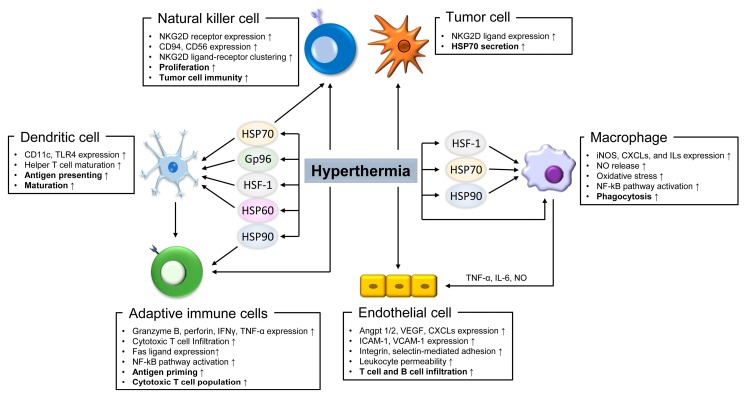
Among the various biological effects of hyperthermia, the immunogenic regulation of cancer progression has been widely studied, and showed promising outcomes through increasing therapeutic efficacy [27,28]. The immunogenicity of hyperthermia has been classically known. Upon infection, adjacent innate immune cells sense pathogen-associated molecular patterns such as lipopolysaccharide and exogenous nucleotides, and secrete cytokines, including interleukin (IL) -1, IL-6, and tumor necrosis factor α (TNF-α). These cytokines circulate in the blood, stimulate the hypothalamus, and activate the COX-2- or RANKL-PGE2 signaling pathways to produce a fever [29,30]. Accordingly, a fever increases systemic temperature and induces pro-inflammatory signaling in the immune cells. Herein, we have summarized the effects of hyperthermia and heat shock responsive factors on enhancing immune cell immunogenicity, which supports the involvement of hyperthermia in increasing the efficacy of anti-tumor therapy (Figure 1).
Figure 1.
Hyperthermia-induced immunogenicity in immune cells. Diagram summarizes the effects of hyperthermia and heat shock proteins (Hsps) in immune response enhancement in macrophage, dendritic cell, natural killer cell, endothelial cell, adaptive immune cells, and tumor cell. VEGF: vascular endothelial growth factor; iNOS: inducible nitric oxide (NO) synthase; CXCLs: chemokine (C-C motif) ligands; ICAM-1: intracellular adhesion molecule 1; VCAM-1: vascular cell adhesion molecule 1; TNF-α: tumor necrosis factor α; NKG2D: natural killer lectin-like receptor gene 2D. HSP: heat shock proteins; TLR: toll-like receptor; ILs: interleukins. The arrows indicate the upregulation effect by hyperthermia.
2.1. Innate Immune Cells
In an immune response, innate immune cells respond to the fever first, which increases their activity. Previous studies suggested that hyperthermia activates macrophages through Hsp-mediated mechanisms, as well as the immunogenic effects of hyperthermia. It was reported that heat shock increased the expression of inducible nitric oxide (NO) synthase (iNOS), chemokine (C-C motif) ligands (CXCLs), and IL and NO release, which activate the functions of macrophages [31,32]. In addition, heat shock enhanced the nuclear factor kappa beta (NF-κB) signaling pathway through induction of IκBα degradation [33]. These effects were also validated by studies showing that heat shock increased macrophage phagocytic activity [34,35,36]. Upon heat stress, HSF1 induces the genes involved in macrophage activation, as well as Hsp expression [37,38]. Various Hsps are involved in the regulation of macrophage activation, which also supports the role of hyperthermia. Specifically, Hsp70 was reportedly related to heat shock-induced macrophage activation, iNOS expression, NF-κB signaling activation, and enhanced phagocytosis [36,39,40,41,42]. Studies on Hsp90 inhibition suggested that Hsp90 controls macrophage activation, NADPH oxidase (NOX) expression, oxidative stress, NF-κB signaling activation, and phagocytosis [36,43,44,45]. Although some studies reported the macrophage inactivation effect of Hsp90 inhibition, the Hsp90 inhibitors used in these studies also reportedly increased Hsp70 expression, causing complex molecular events to occur [43,44,46]. Moreover, Hsp23, Hsp27, and Hsp40, were also involved in macrophage activation, which supports the important role of hyperthermia [36,47,48,49]. Conversely, some studies reported the heat shock-induced inactivation and decreased survival of macrophages [50,51,52]. These studies showed that prolonged and strong heat shock could result in immune response defects and tissue damage, suggesting the importance of hyperthermia intensity and duration.
Dendritic cells (DCs) are a type of innate immune cell which presents antigens to adaptive immune cells to create immunity. The antigen presentation by DCs is significant in generation of immunity against tumor cells. In previous studies, both intense and mild heat shock induced DC maturation and inflammatory signaling activation [53,54]. Other studies also supported that heat shock induced mature CD11c+ DCs through HSF1-, Hsp70-, and toll-like receptor (TLR)-dependent manners [55,56,57,58]. Previous studies also suggested the extraordinary role of Hsp70 in DC activation. Hsp70 is secreted by adherent tumor cells upon heat shock reaction and acts as a DC antigen, which increases immunity against tumor cells through TLR4 in DCs [59,60]. This role of Hsp70 was reported in glioblastoma, hepatocarcinoma, and melanoma cells, and in some clinical studies [61,62,63,64,65]. DCs also reportedly expressed Hsp90 at high temperature, and showed accelerated maturation [66]. The activating role of hyperthermia through Hsp90 was validated in DCs via specific Hsp90 inhibition interfering with the DCs-mediated CD4+ T cell maturation [67,68]. Similar to Hsp70, Hsp90 was also reported to increase immunogenicity against tumor cells by forming complexes of tumor antigen peptide to donor cells [69,70,71,72]. Furthermore, studies about the involvement of Hsp60, gp96 (a member of the Hsp90 family), and Hsc73 in DC activation, supported the hyperthermia-induced immunogenicity of DCs [73,74,75,76,77,78]. These studies show that hyperthermia increases the proliferation, maturation, and antigen presentation of DCs, which may lead to adaptive immune response activation.
Natural killer (NK) cells, the most effective cells involved in tumor growth and recurrence inhibition, were reportedly activated by hyperthermia through enhanced cytotoxicity and recruitment to tumor sites in vivo [79,80,81]. Increased NK cell cytotoxicity was dependent on thermal stimulation-induced clustering of natural killer lectin-like receptor gene 2D (NKG2D) ligand-receptors on tumor and NK cells. This clustering was mediated by hyperthermia-induced Hsp70 expression, which led to NKG2D ligand expression in various types of cancer cells, including colon, lung, cervical, and skin cancer [82,83,84]. Hsp70 could also stimulate NK cell proliferation and activity through the expression of NKG2D, CD94, and CD56 in NK cell membranes [85,86,87]. These studies suggested that hyperthermia increased NK cell immunity through dual stimulation of tumor and NK cells. Hsp90 was studied as another mediator in the induction of NK cell activation using Hsp90 inhibitors [88,89]. Moreover, Hsp72, gp96, and HSF-1 were also reportedly involved in the enhancement of NK cell activity [90,91,92]. In summary, hyperthermia can increase NK cell immunity against tumor cells by activating NK cells, and increasing tumor cell recognition by NK cells.
2.2. Immune Cell Infiltration.
After activation of innate immune cells, naïve leukocytes and lymphocytes are attracted, and infiltrate into the tissue from blood or lymph to interact with antigen-presenting cells. Previous studies have suggested that hyperthermia may help immune cell infiltration through increased endothelial cell activation and permeability. In mild hyperthermia treatment, endothelial cells showed increased expression of angiopoietin (Angpt) 1 and 2, which stimulated vasculogenesis and immune cell infiltration [93]. Although the role of vascular endothelial growth factor (VEGF) in regulating vessel permeability is controversial, hyperthermia was reported to induce VEGF expression in endothelial cells [93,94,95]. We interpreted that hyperthermia enhanced immune cell infiltration through an overall induction of vascular network formation. The roles of Hsps in endothelial cell activation also supported the significant involvement of hyperthermia. Hsp70 expressed post-hyperthermia treatment could move to the extracellular environment [96]. Increased extracellular Hsp70 stimulated normal macrophages to secrete the cytokines TNF-α, IL-6, and NO, which enhanced endothelial wall activation and permeability [97,98,99,100]. These cytokines induced the expression of chemokines including CXCL1, CXCL2, and CXCL10, and adhesion molecules including intracellular adhesion molecule 1 (ICAM-1) and vascular cell adhesion molecule 1 (VCAM-1) in endothelial cells, which modulate the interaction with infiltrating immune cells [101,102,103]. A study examining the role of hyperthermia in increasing endothelial cell adhesion to immune cells directly supported these events [104]. Endothelial cell activation in the central nerve system played a major role in fever generation during pro-inflammatory situations, and hyperthermic immunogenicity could be maintained through endothelial cell activation [105,106]. Hyperthermia also increased the integrin- and selectin-mediated adhesion of lymphocytes to the endothelium [107,108]. Endothelial cell activation and increased immune cell recruitment result in the formation of anti-tumoral microenvironments. This was observed in a previous study where hyperthermia increased the number of infiltrating T and B cells in in vitro and tumor xenograft models [109].
2.3. Adaptive Immune Cells
Cytotoxic T cell activation upon hyperthermia has been supported by previous studies, which provided evidence for the hyperthermia-induced immunogenicity of adaptive immunity. One study reported that hyperthermia treatment induced the expression of granzyme B, perforin, and interferon γ (IFNγ), and increased the cytotoxic activity of cytotoxic T cells [110]. Furthermore, the study suggested that mild hyperthermia (39 °C) showed the best immunogenic effects compared with hyperthermia at other temperatures (~41 °C). This supported the importance of modifying hyperthermia treatment strategies for the best effects. Previous studies reported that hyperthermia induced lymphocyte migration from circulation to the peripheral lymph nodes, local tissue, and even tumor sites in in vivo mouse models [111,112]. Heat shock responsive proteins were also involved in regulating T cell immunity upon hyperthermia. Hyperthermia-induced HSF directly promoted Fas ligand expression and immunity against Fas-bearing target cells both in vitro and in vivo [113,114]. In the context of Hsp, Hsp70 acted as self-epitopes and activated T cells through the induction of CD69 and cytokines, including IFNγ and TNF-α [115]. Hsp90 and Hsp27 also reportedly acted as antigens to induce immunity against myeloma cells, and increased active antigen-specific cytotoxic T cells [116]. Enhancement of hyperthermia-induced Hsp-specific immunity is crucial in tumor progression regulation because tumor cells naturally showed high Hsp expression. The role of Hsps in regulation of signaling pathways was also reported. Hsp90 was involved in TNF-α expression, NF-κB signaling pathway activation, and the pro-inflammatory signaling pathway in cytotoxic T cells [117]. Gp96 showed cross-protective roles in cytotoxic T cells, and had increased activity against tumor cells [118,119]. Gp96 also induced antigen-specific T cell activation through changing the regulatory T cell/cytotoxic T cell ratio by reducing the regulatory T cell population [120]. Gp96 and Hsp80 bound to CD91 on antigen presenting cells, and mediated the priming of antigen presenting cells to T helper cells [121]. Similarly, Hsp110 and gp170 formed complexes with antigens and enhanced antigen presentation to T cells [122]. These studies showed that hyperthermia treatment increased immunogenicity through regulation of cytotoxic T cell population and activity.
Although a few studies suggested the effects of hyperthermia on B cell activation, hyperthermia was also involved in B cell activation. Hyperthermia treatment induced B cells to express TLR9 through activation of the extracellular signal-regulated kinase (ERK) and NF-κB signaling pathways, which activated B cell-mediated immune responses [123]. Hyperthermia-induced HSF1 promoted B cell proliferation and activation [124,125]. Hsp90 increased total B cell proliferation, and activated their antigen presentation via B cell-antigen complex formation [126,127]. Hsp60 protected B cells from apoptosis and increased their survival through the TLR4 signaling pathway [128]. Apg-2, a member of the Hsp110 family, induced the proliferation of, and reduced the oxidative stress in B cells [129]. Taken together, these studies supported that the hyperthermia-induced immunogenic effect could be mediated by adaptive immune cell activation.
3. Molecular Mechanisms of Immunogenicity by Hyperthermia
Attempts to combine radiotherapy and hyperthermia for tumor cell radiosensitization were reported in the 1980s and 1990s [130,131]. However, utilizing hyperthermia for radiosensitization was not widely used due to the difficulty of achieving delicate target site temperature regulation with past hyperthermia technologies, and ignorance of the adequate temperature for hyperthermia treatment [132]. Before the 2000s, hyperthermia treatment was delivered through invasive intraluminal- and interstitial-hyperthermia [133,134]. Invasive hyperthermia treatments were less safe because of the need to penetrate a heating node into the target site. As the hyperthermia technology and equipment developed, various types of non-invasive hyperthermia treatment methods and according outcomes were suggested in recent studies [135]. In recent decades, hyperthermia was delivered through radiofrequency-, microwave-, and electromagnetic-capacitive hyperthermia, with highly sensitive temperature control capacity [136,137,138]. The safety of non-invasive hyperthermia treatment was proven in recent studies [139,140]. Moreover, the immunogenic treatment, which increased the radiation therapy efficacy, suggests the possible application of hyperthermia for radiosensitization, and this hyperthermia-induced radiosensitization was validated by many studies [141,142,143,144]. Focusing on the immunogenicity of hyperthermia, we summarized the current studies examining the molecular events that occur during the combination of hyperthermia treatment and radiotherapy, to understand the radiosensitization effects of hyperthermia (Table 1).
Table 1.
Signaling pathway and proteins induced by combination of hyperthermia radiotherapy.
| Signaling Pathway | Protein | Reference |
|---|---|---|
| DNA repair | DNA-PK | [135,139,147] |
| γH2AX | [139,144] | |
| MRE11 | [140,141,142,143] | |
| Rad50 | [143] | |
| NBS1 | [143] | |
| Rad51 | [145] | |
| BRCA2 | [146] | |
| Ku70 | [147] | |
| Cell cycle/Apoptosis | p53 | [149,157] |
| Cyclin-B1 | [151] | |
| HMGB1 | [152,156] | |
| Bax/Bcl-2 | [157,158,159] | |
| NF-κB | [160] | |
| Akt | [161] | |
| Heat shock response | Hsp90 | [155] |
| Hsp70 | [156,167] | |
| Hsp72 | [164,168] |
3.1. DNA Repair
Radiation generates DNA damage through strong oxidative stress, which induces single or double strand DNA breaks. DNA damage is sensed by DNA damage response proteins, including DNA-dependent protein kinase (DNA-PK), γH2AX, MRE11, and ataxia telangiectasia mutated (ATM), which cause either DNA repair or apoptosis depending on the damage severity. Increased radiation-induced tumor cell apoptosis could activate adjacent immune cells by providing an immunogenic microenvironment [145]. A previous study suggested that DNA-PK activity was inhibited by hyperthermia, and maintained pro-apoptotic signaling by combining hyperthermia and radiation therapies in a hepatoma cell line [142]. This effect of hyperthermia was confirmed by studies that showed hyperthermia-induced γH2AX foci increase, and steady DNA damage responses were mediated by DNA-PK [146]. Hyperthermia-induced inhibition of MRE11, another DNA damage response protein, was also reported to induce radiosensitization, which was correlated with MRE11 expression [147,148]. Hyperthermia also induced MRE11 translocation toward the cytoplasm, and inhibited complex formation with Rad50 and NBS1, which increased the number of unrepaired DNA breaks and caused pro-apoptotic signaling pathway activation [149,150]. Additionally, other DNA repair proteins, including H2AX, Rad51, breast cancer gene 2 (BRCA2), and Ku70, were inhibited by hyperthermia and shown to have roles in hyperthermia-induced radiosensitization [151,152,153,154]. Furthermore, one study even suggested the possible application of hyperthermia for sensitizing tumor cells against genotoxic chemotherapy [155]. From these studies, we can conclude that combining hyperthermia and radiotherapy enhances the genomic instability of tumor cells.
3.2. Cell Cycle Arrest and Apoptosis
Sustained hyperthermia-induced DNA damage, due to inhibited DNA repair, induced the pro-apoptotic signaling pathway [156]. P53 was crucially involved in mediating the signaling to late DNA damage responses, even when combining hyperthermia and radiotherapy [157]. One of the late DNA damage responses, cell cycle progression, was inhibited. Hyperthermia enhanced radiation-induced cell cycle arrest in the G2 and M phases through intracellular accumulation of cyclin B1, which caused tumor cell apoptosis [158,159]. Other studies also suggested that combining hyperthermia and radiotherapy resulted in increased radiosensitive G2 phase cells and high motility group box protein B1 (HMGB1) release, acting as a danger signal, which further stimulated immune responses [160,161]. Studies examining the roles of Hsp70 and Hsp90 expression in cell cycle arrest during combination therapy, suggested the direct involvement of hyperthermia [162,163]. As another late DNA damage response, hyperthermia-induced p53 activated pro-apoptotic signaling proteins and caspases, which sensitized tumor cells to radiotherapy in in vitro and in vivo models [164,165]. Pro-apoptotic signaling activation also occurred by Bax/Bcl-2 ratio regulation via transcriptional regulation [166]. Moreover, hyperthermia could reduce the radiation-induced activation of survival pathways, including the NF-κB signaling pathway through IκB kinase inhibition, and the AKT-S6K pathway [167,168]. As the targeting of the NF-κB and PI3K-AKT-mTOR signaling pathways has been crucial to overcoming tumor cell radioresistance, hyperthermia also may sensitize tumor cells by mediating survival signaling inhibition [169,170].
3.3. Heat Shock Response
As the general regulator of hyperthermic stimulation, Hsps were upregulated and acted as signaling molecules and transcription factors upon heat shock. We found that some studies describing the role of Hsps in hyperthermia-induced radiosensitization suggested Hsps as the mediator of molecular events. Hyperthermia-induced Hsp72 expression increased the radio- and chemo-sensitivity of prostate cancer cells through the suppression of survival, MAPK, and NK-κB pathways [171]. This effect of combination therapy was also validated in an in vivo mouse prostate cancer model [172]. Hyperthermia also increased extracellular Hsps during tumor necrosis, which induced immunity against tumor cells [173]. However, some studies reported the roles of Hsp70 in radioresistance and Hsp72 in etoposide-induced apoptosis resistance [174,175]. This discrepancy suggested that hyperthermia-induced radiosensitization was partially dependent on Hsp expression. Taken together, these studies insisted that the underlying molecular mechanisms that mediate hyperthermia-induced radiosensitization are still elusive. Further molecular studies will be a key to the therapeutic optimization of hyperthermia as a radiosensitizing strategy.
3.4. Abscopal Effect
Radiation-induced immunogenicity displays the abscopal effect, a phenomenon in which local radiotherapy at a distance from a tumor site suppressed tumor growth and progression. Although the precise mechanism of the abscopal effect is not fully understood, it may be mediated by immune system activation [176,177]. Current studies support that hyperthermia-induced immunogenicity could enhance the therapeutic efficacy of radiotherapy through the abscopal effect. It was reported that magnet-mediated hyperthermia could improve abscopal antitumor effects, and stimulate significant endogenous immune responses in sarcoma-bearing rats, by improving the CD4+/CD8+ T cell ratio [178]. And it was also reported that combining intratumoral DC injection and modulated electro-hyperthermia, exerted a strong abscopal effect against distant non-treated tumors [179]. These reports showed that hyperthermia can exaggerate the radiation-induced abscopal cytotoxicity of tumor cells and enhance radiotherapy efficacy through immunogenic effects, which could be applied to combination therapy in the future.
4. Clinical Significance of the Immunogenic Effect of Hyperthermia
Based on the high potential shown when combining immunogenic hyperthermia and radiotherapy as an anti-tumor treatment, this combination therapy has been used in clinical research to enhance therapeutic efficacy. Current research reports that hyperthermia sensitized various tumor cells, which gave better outcomes in cancer patients. In this review, we summarized current studies on therapeutic strategies used to gain a deeper understanding of the clinical application of hyperthermia and radiation combination therapy. We noticed that the differing treatment schedules between studies determined the clinical radiosensitization effect of hyperthermia. In cervical cancer patients, only concurrent delivery of hyperthermia and radiotherapy showed significantly improved outcomes with negligible adjacent normal tissue damage [180]. In the same study, the radiosensitization effect diminished over time post-treatment, with the effect being significantly reduced 30 min after hyperthermia treatment. The effects of simultaneous hyperthermia treatment (a less than 30-min interval) were reported in superficial, breast, and cervical cancers [181,182,183,184]. Moreover, one study also suggested the suppression of lung cancer metastasis by concurrently combining hyperthermia and radiotherapy [185]. In contrast, another study suggested hyperthermia treatment 1–3 h after radiotherapy, and observed a high rate of complete response [186]. Cervical cancer patients treated with hyperthermia 1–4 h after radiotherapy also showed an improved complete response rate and three-year overall survival [187]. Conversely, some studies reported the effects of hyperthermia which was not concurrently combined with radiotherapy. Hyperthermia treatment twice per week and radiotherapy treatment five times per week increased complete response, but not the overall survival [188]. Another study that used hyperthermia as an irregular, non-scheduled additional treatment showed no beneficial effect on the suppression of locally advanced non-small-cell lung cancer [189]. One study emphasized that the delivery strategy of hyperthermia upon radiotherapy determined the therapeutic efficacy enhancement, which was supported by another study performed in various superficial cancer patients [181]. Research showed that the radiosensitization effect of hyperthermia was maximized when the therapies were concurrently administered. Although clinical research supported better outcomes with therapies combined with hyperthermia, some studies suggested the need to discover the underlying molecular mechanisms for better validation of hyperthermic effects [190]. Therefore, unveiling the biological factors involved in hyperthermia-induced radiosensitization could lead the way to a better understanding of the therapy.
The potential of hyperthermia immunogenicity was also validated via combining with other anti-tumor therapies. In gastrointestinal, and head and neck cancer patients, hyperthermia induced chemosensitivity to certain drugs, including cisplatin and cetuximab, with promising outcomes [186,190]. Triple combination therapy with hyperthermia, radiotherapy, and chemotherapy was performed in a previous study that suggested better recurrence-free and overall survival rates [191]. The hyperthermia-induced chemosensitization effect was also shown in previous studies. This combination therapy could be performed through regional hyperthermia or heated anti-tumor drug infusion. This combination therapy significantly improved overall survival and progression-free survival in some types of cancer [192,193]. A study supported the combination of hyperthermia and chemotherapy induced immunogenicity through providing clinical results [194]. Furthermore, the immunogenicity of hyperthermia treatment improved immunotherapeutic efficacy in some clinical research. Head and neck cancer, and breast cancer patients treated with hyperthermia and immunotherapy showed significantly improved survival outcomes [195,196]. Although only a small amount of clinical research into the combination of hyperthermia and immunotherapy has been performed, this combination therapy is believed to be promising. Taken together, the immunogenic effects of hyperthermia treatment could also sensitize the tumor cells against other anti-tumor therapies. However, more investigation into combination therapy is required to achieve therapeutic utilization.
5. Conclusions
Enhancing therapeutic efficacy has been widely studied for many anti-tumor therapies. In this review, we focused on hyperthermia and its immunogenic effects to sensitize tumor cells against radiotherapy. Studies showed that hyperthermia-induced radiosensitization could occur through enhancing immunogenicity against tumor cells, and that sensitization was clinically significant. As hyperthermia-induced molecular events remain partially unknown, and combination therapy cannot completely eliminate the tumor, further studies are needed to optimize the strategies of combination therapies. Furthermore, we discussed the clinical significance of hyperthermia in combination with chemotherapy and immunotherapy, which suggests the promising potential of optimized combination therapy as an anti-tumor strategy.
To develop hyperthermia treatment as an optimal combination therapy with radiotherapy, we suggest devising optimized hyperthermia treatment protocols considering the immunogenic effects of hyperthermia needed. Although clinical studies showed the schedule of combination therapy dominantly determined the therapeutic outcomes, research into the best schedule design is scarce. Combining other anti-tumor therapies with hyperthermia and radiotherapy is also expected to improve clinical outcomes. Moreover, basic research to understand the elusive molecular events upon hyperthermia can help investigations.
Although the potential of immunogenic treatment in therapeutic sensitization has been suggested, the difficulty in the delivery of immunogenic stimulators, including chemical compounds and immune checkpoint blockades, and low efficacy, slowed clinical success. We suggested hyperthermia treatment as an alternative immunogenic treatment with better delivery and spatial selectivity. Furthermore, hyperthermia treatment elevated heat shock response proteins, which exerted immunogenic effects and marked thermally stimulated sites. Therefore, hyperthermia treatment can compensate for the weak parts of other therapies, and further advances in hyperthermia technology can be used for technical improvement of therapeutic delivery systems. Taken together, we anticipate that further basic, clinical, and technological research into combining hyperthermia and radiotherapy will show a new path to complete tumor control.
Abbreviations
| Angpt | angiopoietin; |
| ATM | ataxia telangiectasia mutated |
| BRCA | breast cancer gene |
| CTLA-4 | cytotoxic T-lymphocyte-associated protein 4 |
| CXCL | chemokine (C-C motif) ligand |
| DC | dendritic cell |
| DNA-PK | DNA-dependent protein kinase |
| FDA | Food and Drug Administration |
| HMGB1 | high motility group box protein B1 |
| HSF | heat shock transcription factor |
| Hsp | heat shock protein |
| ICAM | intracellular adhesion molecule |
| IFNγ | interferon gamma |
| iNOS | inducible nitric oxide synthase |
| NF-κB | nuclear factor kappa beta |
| NK | natural killer |
| NKG2D | natural killer lectin-like receptor gene 2D |
| NO | nitric oxide |
| PD-1 | programmed death 1 |
| PD-L1 | programmed death-ligand 1 |
| TLR | toll-like receptor |
| TNF-α | tumor necrosis factor α |
| VCAM | vascular cell adhesion molecule |
| VEGF | vascular endothelial growth factor |
Author Contributions
S.L. prepared the manuscript draft. B.S., G.P., H.K. (Hyunwoo Kim), H.K. (Hyunkoo Kang), and J.J. edited and reviewed. H.Y. and B.Y. conceptualized and supervised.
Funding
This study was supported by a grant of the Basic Science Research Program through NRF grant (2017R1D1A1B03028769 to B.Y. and 2016R1D1A1B03931405 to H.Y.), Republic of Korea.
Conflicts of Interest
The authors declared that there is no interest to disclose.
References
- 1.Santivasi W.L., Xia F. Ionizing radiation-induced DNA damage, response, and repair. Antioxid. Redox Signal. 2014;21:251–259. doi: 10.1089/ars.2013.5668. [DOI] [PubMed] [Google Scholar]
- 2.Lim K., Small W., Jr., Portelance L., Creutzberg C., Jurgenliemk-Schulz I.M., Mundt A., Mell L.K., Mayr N., Viswanathan A., Jhingran A., et al. Consensus guidelines for delineation of clinical target volume for intensity-modulated pelvic radiotherapy for the definitive treatment of cervix cancer. Int. J. Radiat. Oncol. Biol. Phys. 2011;79:348–355. doi: 10.1016/j.ijrobp.2009.10.075. [DOI] [PubMed] [Google Scholar]
- 3.Bao S., Wu Q., McLendon R.E., Hao Y., Shi Q., Hjelmeland A.B., Dewhirst M.W., Bigner D.D., Rich J.N. Glioma stem cells promote radioresistance by preferential activation of the DNA damage response. Nature. 2006;444:756–760. doi: 10.1038/nature05236. [DOI] [PubMed] [Google Scholar]
- 4.Diehn M., Cho R.W., Lobo N.A., Kalisky T., Dorie M.J., Kulp A.N., Qian D., Lam J.S., Ailles L.E., Wong M., et al. Association of reactive oxygen species levels and radioresistance in cancer stem cells. Nature. 2009;458:780–783. doi: 10.1038/nature07733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Boer S.M., Powell M.E., Mileshkin L., Katsaros D., Bessette P., Haie-Meder C., Ottevanger P.B., Ledermann J.A., Khaw P., Colombo A., et al. Toxicity and quality of life after adjuvant chemoradiotherapy versus radiotherapy alone for women with high-risk endometrial cancer (PORTEC-3): An open-label, multicentre, randomised, phase 3 trial. Lancet Oncol. 2016;17:1114–1126. doi: 10.1016/S1470-2045(16)30120-6. [DOI] [PubMed] [Google Scholar]
- 6.Sharabi A.B., Lim M., DeWeese T.L., Drake C.G. Radiation and checkpoint blockade immunotherapy: Radiosensitisation and potential mechanisms of synergy. Lancet Oncol. 2015;16:e498–e509. doi: 10.1016/S1470-2045(15)00007-8. [DOI] [PubMed] [Google Scholar]
- 7.Martin-Liberal J., Ochoa de Olza M., Hierro C., Gros A., Rodon J., Tabernero J. The expanding role of immunotherapy. Cancer Treat. Rev. 2017;54:74–86. doi: 10.1016/j.ctrv.2017.01.008. [DOI] [PubMed] [Google Scholar]
- 8.Topalian S.L., Drake C.G., Pardoll D.M. Immune checkpoint blockade: A common denominator approach to cancer therapy. Cancer Cell. 2015;27:450–461. doi: 10.1016/j.ccell.2015.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Formenti S.C., Demaria S. Combining radiotherapy and cancer immunotherapy: A paradigm shift. J. Natl. Cancer Inst. 2013;105:256–265. doi: 10.1093/jnci/djs629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shi H., Qi X., Ma B., Cao Y., Wang L., Sun L., Niu H. The status, limitation and improvement of adoptive cellular immunotherapy in advanced urologic malignancies. Chin. J. Cancer Res. 2015;27:128–137. doi: 10.3978/j.issn.1000-9604.2014.12.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fan Y., Moon J.J. Nanoparticle Drug Delivery Systems Designed to Improve Cancer Vaccines and Immunotherapy. Vaccines. 2015;3:662–685. doi: 10.3390/vaccines3030662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pilones K.A., Vanpouille-Box C., Demaria S. Combination of radiotherapy and immune checkpoint inhibitors. Semin. Radiat. Oncol. 2015;25:28–33. doi: 10.1016/j.semradonc.2014.07.004. [DOI] [PubMed] [Google Scholar]
- 13.Hato S.V., Khong A., de Vries I.J., Lesterhuis W.J. Molecular pathways: The immunogenic effects of platinum-based chemotherapeutics. Clin. Cancer Res. 2014;20:2831–2837. doi: 10.1158/1078-0432.CCR-13-3141. [DOI] [PubMed] [Google Scholar]
- 14.Garg A.D., Krysko D.V., Verfaillie T., Kaczmarek A., Ferreira G.B., Marysael T., Rubio N., Firczuk M., Mathieu C., Roebroek A.J., et al. A novel pathway combining calreticulin exposure and ATP secretion in immunogenic cancer cell death. EMBO J. 2012;31:1062–1079. doi: 10.1038/emboj.2011.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Workenhe S.T., Pol J.G., Lichty B.D., Cummings D.T., Mossman K.L. Combining oncolytic HSV-1 with immunogenic cell death-inducing drug mitoxantrone breaks cancer immune tolerance and improves therapeutic efficacy. Cancer Immunol. Res. 2013;1:309–319. doi: 10.1158/2326-6066.CIR-13-0059-T. [DOI] [PubMed] [Google Scholar]
- 16.Florea A.M., Busselberg D. Cisplatin as an anti-tumor drug: Cellular mechanisms of activity, drug resistance and induced side effects. Cancers. 2011;3:1351–1371. doi: 10.3390/cancers3011351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cassidy J., Misset J.L. Oxaliplatin-related side effects: Characteristics and management. Semin. Oncol. 2002;29:11–20. doi: 10.1053/sonc.2002.35524. [DOI] [PubMed] [Google Scholar]
- 18.Sun W., Wei X., Niu A., Ma X., Li J.J., Gao D. Enhanced anti-colon cancer immune responses with modified eEF2-derived peptides. Cancer Lett. 2015;369:112–123. doi: 10.1016/j.canlet.2015.08.002. [DOI] [PubMed] [Google Scholar]
- 19.Menger L., Vacchelli E., Adjemian S., Martins I., Ma Y., Shen S., Yamazaki T., Sukkurwala A.Q., Michaud M., Mignot G., et al. Cardiac glycosides exert anticancer effects by inducing immunogenic cell death. Sci. Transl. Med. 2012;4:143ra99. doi: 10.1126/scitranslmed.3003807. [DOI] [PubMed] [Google Scholar]
- 20.Chen H.M., Wang P.H., Chen S.S., Wen C.C., Chen Y.H., Yang W.C., Yang N.S. Shikonin induces immunogenic cell death in tumor cells and enhances dendritic cell-based cancer vaccine. Cancer Immunol. Immunother. 2012;61:1989–2002. doi: 10.1007/s00262-012-1258-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mace T.A., Zhong L., Kokolus K.M., Repasky E.A. Effector CD8+ T cell IFN-gamma production and cytotoxicity are enhanced by mild hyperthermia. Int. J. Hyperth. 2012;28:9–18. doi: 10.3109/02656736.2011.616182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang H.G., Mehta K., Cohen P., Guha C. Hyperthermia on immune regulation: A temperature’s story. Cancer Lett. 2008;271:191–204. doi: 10.1016/j.canlet.2008.05.026. [DOI] [PubMed] [Google Scholar]
- 23.Schildkopf P., Frey B., Mantel F., Ott O.J., Weiss E.M., Sieber R., Janko C., Sauer R., Fietkau R., Gaipl U.S. Application of hyperthermia in addition to ionizing irradiation fosters necrotic cell death and HMGB1 release of colorectal tumor cells. Biochem. Biophys. Res. Commun. 2010;391:1014–1020. doi: 10.1016/j.bbrc.2009.12.008. [DOI] [PubMed] [Google Scholar]
- 24.Kasdorf E., Perlman J.M. Hyperthermia, inflammation, and perinatal brain injury. Pediatr. Neurol. 2013;49:8–14. doi: 10.1016/j.pediatrneurol.2012.12.026. [DOI] [PubMed] [Google Scholar]
- 25.Singh I.S., Hasday J.D. Fever, hyperthermia and the heat shock response. Int. J. Hyperth. 2013;29:423–435. doi: 10.3109/02656736.2013.808766. [DOI] [PubMed] [Google Scholar]
- 26.Richter K., Haslbeck M., Buchner J. The heat shock response: Life on the verge of death. Mol. Cell. 2010;40:253–266. doi: 10.1016/j.molcel.2010.10.006. [DOI] [PubMed] [Google Scholar]
- 27.Frey B., Weiss E.M., Rubner Y., Wunderlich R., Ott O.J., Sauer R., Fietkau R., Gaipl U.S. Old and new facts about hyperthermia-induced modulations of the immune system. Int. J. hyperth. 2012;28:528–542. doi: 10.3109/02656736.2012.677933. [DOI] [PubMed] [Google Scholar]
- 28.Falk M.H., Issels R.D. Hyperthermia in oncology. Int. J. Hyperth. 2001;17:1–18. doi: 10.1080/02656730150201552. [DOI] [PubMed] [Google Scholar]
- 29.Evans S.S., Repasky E.A., Fisher D.T. Fever and the thermal regulation of immunity: The immune system feels the heat. Nat. Rev. Immunol. 2015;15:335–349. doi: 10.1038/nri3843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roth J., Blatteis C.M. Mechanisms of fever production and lysis: Lessons from experimental LPS fever. Compr. Physiol. 2014;4:1563–1604. doi: 10.1002/cphy.c130033. [DOI] [PubMed] [Google Scholar]
- 31.Slawinska A., Hsieh J.C., Schmidt C.J., Lamont S.J. Heat stress and lipopolysaccharide stimulation of chicken macrophage-like cell line activates expression of distinct sets of genes. PLoS ONE. 2016;11:e0164575. doi: 10.1371/journal.pone.0164575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goldring C.E., Reveneau S., Chantome A., Pance A., Fleury C., Hume D.A., Sester D., Mignotte B., Jeannin J.F. Heat shock enhances transcriptional activation of the murine-inducible nitric oxide synthase gene. FASEB J. 2000;14:2393–2395. doi: 10.1096/fj.98-0509fje. [DOI] [PubMed] [Google Scholar]
- 33.Shanley T.P., Ryan M.A., Eaves-Pyles T., Wong H.R. Heat shock inhibits phosphorylation of I-κBα. Shock. 2000;14:447–450. doi: 10.1097/00024382-200014040-00005. [DOI] [PubMed] [Google Scholar]
- 34.Vega V.L., Charles W., Crotty Alexander L.E. Rescuing of deficient killing and phagocytic activities of macrophages derived from non-obese diabetic mice by treatment with geldanamycin or heat shock: Potential clinical implications. Cell Stress Chaperones. 2011;16:573–581. doi: 10.1007/s12192-011-0268-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vega V.L., De Maio A. Increase in phagocytosis after geldanamycin treatment or heat shock: Role of heat shock proteins. J. Immunol. 2005;175:5280–5287. doi: 10.4049/jimmunol.175.8.5280. [DOI] [PubMed] [Google Scholar]
- 36.Miller L., Qureshi M.A. Induction of heat-shock proteins and phagocytic function of chicken macrophage following in vitro heat exposure. Vet. Immunol. Immunopathol. 1992;30:179–191. doi: 10.1016/0165-2427(92)90137-F. [DOI] [PubMed] [Google Scholar]
- 37.Zhang H., Zhang L., Yu F., Liu Y., Liang Q., Deng G., Chen G., Liu M., Xiao X. HSF1 is a transcriptional activator of IL-10 gene expression in RAW264.7 macrophages. Inflammation. 2012;35:1558–1566. doi: 10.1007/s10753-012-9471-4. [DOI] [PubMed] [Google Scholar]
- 38.Moore K.W., de Waal Malefyt R., Coffman R.L., O′Garra A. Interleukin-10 and the interleukin-10 receptor. Ann. Rev. Immunol. 2001;19:683–765. doi: 10.1146/annurev.immunol.19.1.683. [DOI] [PubMed] [Google Scholar]
- 39.Kovalchin J.T., Wang R., Wagh M.S., Azoulay J., Sanders M., Chandawarkar R.Y. In vivo delivery of heat shock protein 70 accelerates wound healing by up-regulating macrophage-mediated phagocytosis. Wound Repair Regen. 2006;14:129–137. doi: 10.1111/j.1743-6109.2006.00102.x. [DOI] [PubMed] [Google Scholar]
- 40.Antonova O.Y., Yurinskaya M.M., Funikov S.Y., Evgen’ev M.B., Vinokurov M.G. Exogenous heat shock protein HSP70 modulates lipopolysaccharide-induced macrophage activation. Dokl. Biochem. Biophys. 2013;452:320–324. doi: 10.1134/S0012496613050141. [DOI] [PubMed] [Google Scholar]
- 41.Zhang L., Liu Q., Yuan X., Wang T., Luo S., Lei H., Xia Y. Requirement of heat shock protein 70 for inducible nitric oxide synthase induction. Cell Signal. 2013;25:1310–1317. doi: 10.1016/j.cellsig.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 42.Scholer C.M., Marques C.V., da Silva G.S., Heck T.G., de Oliveira Junior L.P., Homem de Bittencourt P.I., Jr. Modulation of rat monocyte/macrophage innate functions by increasing intensities of swimming exercise is associated with heat shock protein status. Mol. Cell. Biochem. 2016;421:111–125. doi: 10.1007/s11010-016-2791-1. [DOI] [PubMed] [Google Scholar]
- 43.Madrigal-Matute J., Lopez-Franco O., Blanco-Colio L.M., Munoz-Garcia B., Ramos-Mozo P., Ortega L., Egido J., Martin-Ventura J.L. Heat shock protein 90 inhibitors attenuate inflammatory responses in atherosclerosis. Cardiovasc. Res. 2010;86:330–337. doi: 10.1093/cvr/cvq046. [DOI] [PubMed] [Google Scholar]
- 44.Chen F., Yu Y., Qian J., Wang Y., Cheng B., Dimitropoulou C., Patel V., Chadli A., Rudic R.D., Stepp D.W., et al. Opposing actions of heat shock protein 90 and 70 regulate nicotinamide adenine dinucleotide phosphate oxidase stability and reactive oxygen species production. Arterioscler. Thromb. Vasc. Biol. 2012;32:2989–2999. doi: 10.1161/ATVBAHA.112.300361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Basu S., Matsutake T. Heat shock protein-antigen presenting cell interactions. Methods. 2004;32:38–41. doi: 10.1016/S1046-2023(03)00189-0. [DOI] [PubMed] [Google Scholar]
- 46.Luo S., Wang T., Qin H., Lei H., Xia Y. Obligatory role of heat shock protein 90 in iNOS induction. Am. J. Physiol. Cell Physiol. 2011;301:C227–C233. doi: 10.1152/ajpcell.00493.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Raizman J.E., Chen Y.X., Seibert T., Hibbert B., Cuerrier C.M., Salari S., Zhao X., Hu T., Shi C., Ma X., et al. Heat shock protein-27 attenuates foam cell formation and atherogenesis by down-regulating scavenger receptor-A expression via NF-κB signaling. Biochim. Biophys. Acta. 2013;1831:1721–1728. doi: 10.1016/j.bbalip.2013.07.015. [DOI] [PubMed] [Google Scholar]
- 48.Li S.S., Xu X.T., Liu W., Xu Z.P., Zhang W.W., Li Y., Dong X.X., Yang X.W., Liu F., Wang Y.Z., et al. Effects of Schistosoma japonicum heat-shock protein 40 on macrophage activation. Zhongguo Xue Xi Chong Bing Fang Zhi Za Zhi. 2012;24:137–141. [PubMed] [Google Scholar]
- 49.Liu J., Hong S., Feng Z., Xin Y., Wang Q., Fu J., Zhang C., Li G., Luo L., Yin Z. Regulation of lipopolysaccharide-induced inflammatory response by heat shock protein 27 in THP-1 cells. Cell. Immunol. 2010;264:127–134. doi: 10.1016/j.cellimm.2010.05.011. [DOI] [PubMed] [Google Scholar]
- 50.Wang Y., Li C., Wang X., Zhang J., Chang Z. Heat shock response inhibits IL-18 expression through the JNK pathway in murine peritoneal macrophages. Biochem. Biophys. Res. Commun. 2002;296:742–748. doi: 10.1016/S0006-291X(02)00930-0. [DOI] [PubMed] [Google Scholar]
- 51.Schell M.T., Spitzer A.L., Johnson J.A., Lee D., Harris H.W. Heat shock inhibits NF-kB activation in a dose- and time-dependent manner. J. Surg. Res. 2005;129:90–93. doi: 10.1016/j.jss.2005.05.025. [DOI] [PubMed] [Google Scholar]
- 52.Prestes-Carneiro L.E., Shio M.T., Fernandes P.D., Jancar S. Cross-regulation of iNOS and COX-2 by its products in murine macrophages under stress conditions. Cell. Physiol. Biochem. 2007;20:283–292. doi: 10.1159/000107514. [DOI] [PubMed] [Google Scholar]
- 53.Matsumoto K., Yamamoto N., Hagiwara S., Saito M., Furue H., Shigetomi T., Narita Y., Mitsudo K., Tohnai I., Kobayashi T., et al. Optimization of hyperthermia and dendritic cell immunotherapy for squamous cell carcinoma. Oncol. Rep. 2011;25:1525–1532. doi: 10.3892/or.2011.1232. [DOI] [PubMed] [Google Scholar]
- 54.Knippertz I., Stein M.F., Dorrie J., Schaft N., Muller I., Deinzer A., Steinkasserer A., Nettelbeck D.M. Mild hyperthermia enhances human monocyte-derived dendritic cell functions and offers potential for applications in vaccination strategies. Int. J. Hyperth. 2011;27:591–603. doi: 10.3109/02656736.2011.589234. [DOI] [PubMed] [Google Scholar]
- 55.Zhao W., An H., Zhou J., Xu H., Yu Y., Cao X. Hyperthermia differentially regulates TLR4 and TLR2-mediated innate immune response. Immunol. Lett. 2007;108:137–142. doi: 10.1016/j.imlet.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 56.Zheng H., Benjamin I.J., Basu S., Li Z. Heat shock factor 1-independent activation of dendritic cells by heat shock: Implication for the uncoupling of heat-mediated immunoregulation from the heat shock response. Eur. J. Immunol. 2003;33:1754–1762. doi: 10.1002/eji.200323687. [DOI] [PubMed] [Google Scholar]
- 57.DeFillipo A.M., Dai J., Li Z. Heat shock-induced dendritic cell maturation is coupled by transient aggregation of ubiquitinated proteins independently of heat shock factor 1 or inducible heat shock protein 70. Mol. Immunol. 2004;41:785–792. doi: 10.1016/j.molimm.2004.04.016. [DOI] [PubMed] [Google Scholar]
- 58.Redzovic A., Gulic T., Laskarin G., Eminovic S., Haller H., Rukavina D. Heat-Shock Proteins 70 Induce Pro-inflammatory maturation program in decidual CD1a+ dendritic cells. Am. J. Reprod. Immunol. 2015;74:38–53. doi: 10.1111/aji.12374. [DOI] [PubMed] [Google Scholar]
- 59.Meng F.D., Sui C.G., Tian X., Li Y., Yang C.M., Ma P., Liu Y.P., Jiang Y.H. Heat-shock protein 70 as a tumor antigen for in vitro dendritic cell pulsing in renal cell carcinoma cases. Asian Pac. J. Cancer Prev. 2014;15:8947–8950. doi: 10.7314/APJCP.2014.15.20.8947. [DOI] [PubMed] [Google Scholar]
- 60.Fang H., Ang B., Xu X., Huang X., Wu Y., Sun Y., Wang W., Li N., Cao X., Wan T. TLR4 is essential for dendritic cell activation and anti-tumor T-cell response enhancement by DAMPs released from chemically stressed cancer cells. Cell. Mol. Immunol. 2014;11:150–159. doi: 10.1038/cmi.2013.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Etminan N., Peters C., Lakbir D., Bunemann E., Borger V., Sabel M.C., Hanggi D., Steiger H.J., Stummer W., Sorg R.V. Heat-shock protein 70-dependent dendritic cell activation by 5-aminolevulinic acid-mediated photodynamic treatment of human glioblastoma spheroids in vitro. Br. J. Cancer. 2011;105:961–969. doi: 10.1038/bjc.2011.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gao J., Luo S.M., Peng M.L., Deng T. Enhanced immunity against hepatoma induced by dendritic cells pulsed with Hsp70-H22 peptide complexes and CD40L. J. Cancer Res. Clin. Oncol. 2012;138:917–926. doi: 10.1007/s00432-012-1166-6. [DOI] [PubMed] [Google Scholar]
- 63.Knudsen S., Schardt A., Buhl T., Boeckmann L., Schon M.P., Neumann C., Haenssle H.A. Enhanced T-cell activation by immature dendritic cells loaded with HSP70-expressing heat-killed melanoma cells. Exp. Dermatol. 2010;19:108–116. doi: 10.1111/j.1600-0625.2009.00962.x. [DOI] [PubMed] [Google Scholar]
- 64.Jie X., Hua L., Jiang W., Feng F., Feng G., Hua Z. Clinical application of a dendritic cell vaccine raised against heat-shocked glioblastoma. Cell Biochem. Biophys. 2012;62:91–99. doi: 10.1007/s12013-011-9265-6. [DOI] [PubMed] [Google Scholar]
- 65.Weng D., Calderwood S.K., Gong J. Preparation of a heat-shock protein 70-based vaccine from DC-tumor fusion cells. Methods Mol. Biol. 2011;787:255–265. doi: 10.1007/978-1-61779-295-3_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Basu S., Srivastava P.K. Fever-like temperature induces maturation of dendritic cells through induction of hsp90. Int. Immunol. 2003;15:1053–1061. doi: 10.1093/intimm/dxg104. [DOI] [PubMed] [Google Scholar]
- 67.Trojandt S., Reske-Kunz A.B., Bros M. Geldanamycin-mediated inhibition of heat shock protein 90 partially activates dendritic cells, but interferes with their full maturation, accompanied by impaired upregulation of RelB. J. Exp. Clin. Cancer Res. 2014;33:16. doi: 10.1186/1756-9966-33-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Byrd C.A., Bornmann W., Erdjument-Bromage H., Tempst P., Pavletich N., Rosen N., Nathan C.F., Ding A. Heat shock protein 90 mediates macrophage activation by Taxol and bacterial lipopolysaccharide. Proc. Natl. Acad. Sci. USA. 1999;96:5645–5650. doi: 10.1073/pnas.96.10.5645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tanaka T., Okuya K., Kutomi G., Takaya A., Kajiwara T., Kanaseki T., Tsukahara T., Hirohashi Y., Torigoe T., Hirata K., et al. Heat shock protein 90 targets a chaperoned peptide to the static early endosome for efficient cross-presentation by human dendritic cells. Cancer Sci. 2015;106:18–24. doi: 10.1111/cas.12570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Murshid A., Gong J., Calderwood S.K. Heat shock protein 90 mediates efficient antigen cross presentation through the scavenger receptor expressed by endothelial cells-I. J. Immunol. 2010;185:2903–2917. doi: 10.4049/jimmunol.0903635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ichiyanagi T., Imai T., Kajiwara C., Mizukami S., Nakai A., Nakayama T., Udono H. Essential role of endogenous heat shock protein 90 of dendritic cells in antigen cross-presentation. J. Immunol. 2010;185:2693–2700. doi: 10.4049/jimmunol.1000821. [DOI] [PubMed] [Google Scholar]
- 72.Imai T., Kato Y., Kajiwara C., Mizukami S., Ishige I., Ichiyanagi T., Hikida M., Wang J.Y., Udono H. Heat shock protein 90 (HSP90) contributes to cytosolic translocation of extracellular antigen for cross-presentation by dendritic cells. Proc. Natl. Acad. Sci. USA. 2011;108:16363–16368. doi: 10.1073/pnas.1108372108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Korba V.D., Heil C.G., Jr. Eight years of fertility control with norgestrel-ethinyl estradiol (Ovral): An updated clinical review. Fertil. Steril. 1975;26:973–981. doi: 10.1016/S0015-0282(16)41410-X. [DOI] [PubMed] [Google Scholar]
- 74.Kol A., Bourcier T., Lichtman A.H., Libby P. Chlamydial and human heat shock protein 60s activate human vascular endothelium, smooth muscle cells, and macrophages. J. Clin. Investig. 1999;103:571–577. doi: 10.1172/JCI5310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Radosevic-Stasic B., Jakovac H., Grebic D., Trobonjaca Z., Mrakovcic-Sutic I., Cuk M. Heat shock protein Gp96 as potential regulator of morphostasis after partial hepatectomy in mice. Curr. Aging Sci. 2012;5:254–262. doi: 10.2174/1874609811205030013. [DOI] [PubMed] [Google Scholar]
- 76.Tamura Y., Torigoe T., Kukita K., Saito K., Okuya K., Kutomi G., Hirata K., Sato N. Heat-shock proteins as endogenous ligands building a bridge between innate and adaptive immunity. Immunotherapy. 2012;4:841–852. doi: 10.2217/imt.12.75. [DOI] [PubMed] [Google Scholar]
- 77.Thery C., Regnault A., Garin J., Wolfers J., Zitvogel L., Ricciardi-Castagnoli P., Raposo G., Amigorena S. Molecular characterization of dendritic cell-derived exosomes. Selective accumulation of the heat shock protein hsc73. J. Cell Biol. 1999;147:599–610. doi: 10.1083/jcb.147.3.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Liu A., Ming J.Y., Fiskesund R., Ninio E., Karabina S.A., Bergmark C., Frostegard A.G., Frostegard J. Induction of dendritic cell-mediated T-cell activation by modified but not native low-density lipoprotein in humans and inhibition by annexin a5: Involvement of heat shock proteins. Arterioscler. Thromb. Vasc. Biol. 2015;35:197–205. doi: 10.1161/ATVBAHA.114.304342. [DOI] [PubMed] [Google Scholar]
- 79.Smyth M.J., Thia K.Y., Street S.E., Cretney E., Trapani J.A., Taniguchi M., Kawano T., Pelikan S.B., Crowe N.Y., Godfrey D.I. Differential tumor surveillance by natural killer (NK) and NKT cells. J. Exp. Med. 2000;191:661–668. doi: 10.1084/jem.191.4.661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ostberg J.R., Dayanc B.E., Yuan M., Oflazoglu E., Repasky E.A. Enhancement of natural killer (NK) cell cytotoxicity by fever-range thermal stress is dependent on NKG2D function and is associated with plasma membrane NKG2D clustering and increased expression of MICA on target cells. J. Leukoc. Biol. 2007;82:1322–1331. doi: 10.1189/jlb.1106699. [DOI] [PubMed] [Google Scholar]
- 81.Farjadian S., Norouzian M., Younesi V., Ebrahimpour A., Lotfi R. Hyperthermia increases natural killer cell cytotoxicity against SW-872 liposarcoma cell line. Iran.J. Immunol. 2013;10:93–102. [PubMed] [Google Scholar]
- 82.Bae J.H., Kim J.Y., Kim M.J., Chang S.H., Park Y.S., Son C.H., Park S.J., Chung J.S., Lee E.Y., Kim S.H., et al. Quercetin enhances susceptibility to NK cell-mediated lysis of tumor cells through induction of NKG2D ligands and suppression of HSP70. J. Immunother. 2010;33:391–401. doi: 10.1097/CJI.0b013e3181d32f22. [DOI] [PubMed] [Google Scholar]
- 83.Galazka G., Jurewicz A., Domowicz M., Cannella B., Raine C.S., Selmaj K. HINT1 peptide/Hsp70 complex induces NK-cell-dependent immunoregulation in a model of autoimmune demyelination. Eur. J. Immunol. 2014;44:3026–3044. doi: 10.1002/eji.201444694. [DOI] [PubMed] [Google Scholar]
- 84.Kim J.Y., Son Y.O., Park S.W., Bae J.H., Chung J.S., Kim H.H., Chung B.S., Kim S.H., Kang C.D. Increase of NKG2D ligands and sensitivity to NK cell-mediated cytotoxicity of tumor cells by heat shock and ionizing radiation. Exp. Mol. Med. 2006;38:474–484. doi: 10.1038/emm.2006.56. [DOI] [PubMed] [Google Scholar]
- 85.Multhoff G., Mizzen L., Winchester C.C., Milner C.M., Wenk S., Eissner G., Kampinga H.H., Laumbacher B., Johnson J. Heat shock protein 70 (Hsp70) stimulates proliferation and cytolytic activity of natural killer cells. Exp. Hematol. 1999;27:1627–1636. doi: 10.1016/S0301-472X(99)00104-6. [DOI] [PubMed] [Google Scholar]
- 86.Xie Y., Bai O., Zhang H., Yuan J., Zong S., Chibbar R., Slattery K., Qureshi M., Wei Y., Deng Y., et al. Membrane-bound HSP70-engineered myeloma cell-derived exosomes stimulate more efficient CD8+ CTL- and NK-mediated antitumour immunity than exosomes released from heat-shocked tumour cells expressing cytoplasmic HSP70. J. Cell. Mol. Med. 2010;14:2655–2666. doi: 10.1111/j.1582-4934.2009.00851.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gross C., Schmidt-Wolf I.G., Nagaraj S., Gastpar R., Ellwart J., Kunz-Schughart L.A., Multhoff G. Heat shock protein 70-reactivity is associated with increased cell surface density of CD94/CD56 on primary natural killer cells. Cell Stress Chaperones. 2003;8:348–360. doi: 10.1379/1466-1268(2003)008<0348:HSPRIA>2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bae J., Munshi A., Li C., Samur M., Prabhala R., Mitsiades C., Anderson K.C., Munshi N.C. Heat shock protein 90 is critical for regulation of phenotype and functional activity of human T lymphocytes and NK cells. J. Immunol. 2013;190:1360–1371. doi: 10.4049/jimmunol.1200593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Huyan T., Li Q., Dong D.D., Yang H., Zhang J., Huang Q.S., Yin D.C., Shang P. Heat shock protein 90 inhibitors induce functional inhibition of human natural killer cells in a dose-dependent manner. Immunopharmacol. Immunotoxicol. 2016;38:77–86. doi: 10.3109/08923973.2015.1119159. [DOI] [PubMed] [Google Scholar]
- 90.Botzler C., Issels R., Multhoff G. Heat-shock protein 72 cell-surface expression on human lung carcinoma cells in associated with an increased sensitivity to lysis mediated by adherent natural killer cells. Cancer Immunol. Immunother. 1996;43:226–230. doi: 10.1007/s002620050326. [DOI] [PubMed] [Google Scholar]
- 91.Newman R.G., Dee M.J., Malek T.R., Podack E.R., Levy R.B. Heat shock protein vaccination and directed IL-2 therapy amplify tumor immunity rapidly following bone marrow transplantation in mice. Blood. 2014;123:3045–3055. doi: 10.1182/blood-2013-08-520775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Dayanc B.E., Bansal S., Gure A.O., Gollnick S.O., Repasky E.A. Enhanced sensitivity of colon tumour cells to natural killer cell cytotoxicity after mild thermal stress is regulated through HSF1-mediated expression of MICA. Int. J. Hyperth. 2013;29:480–490. doi: 10.3109/02656736.2013.821526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Li M., Fuchs S., Bose T., Schmidt H., Hofmann A., Tonak M., Unger R., Kirkpatrick C.J. Mild heat stress enhances angiogenesis in a co-culture system consisting of primary human osteoblasts and outgrowth endothelial cells. Tissue Eng. Part C Methods. 2014;20:328–339. doi: 10.1089/ten.tec.2013.0087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Martin-Saavedra F.M., Wilson C.G., Voellmy R., Vilaboa N., Franceschi R.T. Spatiotemporal control of vascular endothelial growth factor expression using a heat-shock-activated, rapamycin-dependent gene switch. Hum. Gene Ther. Methods. 2013;24:160–170. doi: 10.1089/hgtb.2013.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hoeppner L.H., Phoenix K.N., Clark K.J., Bhattacharya R., Gong X., Sciuto T.E., Vohra P., Suresh S., Bhattacharya S., Dvorak A.M., et al. Revealing the role of phospholipase Cβ3 in the regulation of VEGF-induced vascular permeability. Blood. 2012;120:2167–2173. doi: 10.1182/blood-2012-03-417824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lee C.T., Repasky E.A. Opposing roles for heat and heat shock proteins in macrophage functions during inflammation: A function of cell activation state? Front. Immunol. 2012;3:140. doi: 10.3389/fimmu.2012.00140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Shevtsov M., Multhoff G. Heat shock protein-peptide and HSP-based immunotherapies for the treatment of cancer. Front. Immunol. 2016;7:171. doi: 10.3389/fimmu.2016.00171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Desreumaux P. Specific targeting of IL-6 signalling pathway: A new way to treat IBD? Gut. 2000;47:465–466. doi: 10.1136/gut.47.4.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Fonseca S.F., Mendonca V.A., Teles M.C., Ribeiro V.G., Tossige-Gomes R., Neves C.D., Rocha-Vieira E., Leite L.H., Soares D.D., Coimbra C.C., et al. Inflammatory cytokines and plasma redox status responses in hypertensive subjects after heat exposure. Braz. J. Med. Biol. Res. 2016;49:e5026. doi: 10.1590/1414-431X20155026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Maruo N., Morita I., Shirao M., Murota S. IL-6 increases endothelial permeability in vitro. Endocrinology. 1992;131:710–714. doi: 10.1210/endo.131.2.1639018. [DOI] [PubMed] [Google Scholar]
- 101.King M.A., Leon L.R., Morse D.A., Clanton T.L. Unique cytokine and chemokine responses to exertional heat stroke in mice. J. Appl. Physiol. 2017;122:296–306. doi: 10.1152/japplphysiol.00667.2016. [DOI] [PubMed] [Google Scholar]
- 102.Wung B.S., Ni C.W., Wang D.L. ICAM-1 induction by TNFα and IL-6 is mediated by distinct pathways via Rac in endothelial cells. J. Biomed. Sci. 2005;12:91–101. doi: 10.1007/s11373-004-8170-z. [DOI] [PubMed] [Google Scholar]
- 103.Harris T.A., Yamakuchi M., Ferlito M., Mendell J.T., Lowenstein C.J. MicroRNA-126 regulates endothelial expression of vascular cell adhesion molecule 1. Proc. Natl. Acad. Sci. USA. 2008;105:1516–1521. doi: 10.1073/pnas.0707493105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Shah A., Unger E., Bain M.D., Bruce R., Bodkin J., Ginnetti J., Wang W.C., Seon B., Stewart C.C., Evans S.S. Cytokine and adhesion molecule expression in primary human endothelial cells stimulated with fever-range hyperthermia. Int. J. Hyperth. 2002;18:534–551. doi: 10.1080/02656730210157843. [DOI] [PubMed] [Google Scholar]
- 105.Eskilsson A., Mirrasekhian E., Dufour S., Schwaninger M., Engblom D., Blomqvist A. Immune-induced fever is mediated by IL-6 receptors on brain endothelial cells coupled to STAT3-dependent induction of brain endothelial prostaglandin synthesis. J. Neurosci. 2014;34:15957–15961. doi: 10.1523/JNEUROSCI.3520-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Engstrom L., Ruud J., Eskilsson A., Larsson A., Mackerlova L., Kugelberg U., Qian H., Vasilache A.M., Larsson P., Engblom D., et al. Lipopolysaccharide-induced fever depends on prostaglandin E2 production specifically in brain endothelial cells. Endocrinology. 2012;153:4849–4861. doi: 10.1210/en.2012-1375. [DOI] [PubMed] [Google Scholar]
- 107.Wang W.C., Goldman L.M., Schleider D.M., Appenheimer M.M., Subjeck J.R., Repasky E.A., Evans S.S. Fever-range hyperthermia enhances L-selectin-dependent adhesion of lymphocytes to vascular endothelium. J. Immunol. 1998;160:961–969. [PubMed] [Google Scholar]
- 108.Evans S.S., Bain M.D., Wang W.C. Fever-range hyperthermia stimulates α4β7 integrin-dependent lymphocyte-endothelial adhesion. Int. J. Hyperth. 2000;16:45–59. doi: 10.1080/026567300285411. [DOI] [PubMed] [Google Scholar]
- 109.Tang L., Wang K. Chronic Inflammation in Skin Malignancies. J. Mol. Signal. 2016;11:2. doi: 10.5334/1750-2187-11-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Takahashi A., Torigoe T., Tamura Y., Kanaseki T., Tsukahara T., Sasaki Y., Kameshima H., Tsuruma T., Hirata K., Tokino T., et al. Heat shock enhances the expression of cytotoxic granule proteins and augments the activities of tumor-associated antigen-specific cytotoxic T lymphocytes. Cell Stress Chaperones. 2012;17:757–763. doi: 10.1007/s12192-012-0348-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Evans S.S., Wang W.C., Bain M.D., Burd R., Ostberg J.R., Repasky E.A. Fever-range hyperthermia dynamically regulates lymphocyte delivery to high endothelial venules. Blood. 2001;97:2727–2733. doi: 10.1182/blood.V97.9.2727. [DOI] [PubMed] [Google Scholar]
- 112.Fisher D.T., Chen Q., Skitzki J.J., Muhitch J.B., Zhou L., Appenheimer M.M., Vardam T.D., Weis E.L., Passanese J., Wang W.C., et al. IL-6 trans-signaling licenses mouse and human tumor microvascular gateways for trafficking of cytotoxic T cells. J. Clin. Investig. 2011;121:3846–3859. doi: 10.1172/JCI44952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bouchier-Hayes L., McBride S., van Geelen C.M., Nance S., Lewis L.K., Pinkoski M.J., Beere H.M. Fas ligand gene expression is directly regulated by stress-inducible heat shock transcription factor-1. Cell Death Differ. 2010;17:1034–1046. doi: 10.1038/cdd.2010.4. [DOI] [PubMed] [Google Scholar]
- 114.Murapa P., Ward M.R., Gandhapudi S.K., Woodward J.G., D’Orazio S.E. Heat shock factor 1 protects mice from rapid death during Listeria monocytogenes infection by regulating expression of tumor necrosis factor α during fever. Infect. Immun. 2011;79:177–184. doi: 10.1128/IAI.00742-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.de Jong H., Koffeman E.C., Meerding J.M., Scholman R.C., Wieten L., de Jager W., Klein M., Otten H., van Wijk F., van der Zee R., et al. T cell recognition of naturally presented epitopes of self-heat shock protein 70. Cell Stress Chaperones. 2014;19:569–578. doi: 10.1007/s12192-013-0484-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Li R., Qian J., Zhang W., Fu W., Du J., Jiang H., Zhang H., Zhang C., Xi H., Yi Q., et al. Human heat shock protein-specific cytotoxic T lymphocytes display potent antitumour immunity in multiple myeloma. Br. J. Haematol. 2014;166:690–701. doi: 10.1111/bjh.12943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Collins C.B., Strassheim D., Aherne C.M., Yeckes A.R., Jedlicka P., de Zoeten E.F. Targeted inhibition of heat shock protein 90 suppresses tumor necrosis factor-α and ameliorates murine intestinal inflammation. Inflamm. Bowel Dis. 2014;20:685–694. doi: 10.1097/01.MIB.0000442839.28664.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ju Y., Fan H., Liu J., Hu J., Li X., Li C., Chen L., Gao Q., Gao G.F., Meng S. Heat shock protein gp96 adjuvant induces T cell responses and cross-protection to a split influenza vaccine. Vaccine. 2014;32:2703–2711. doi: 10.1016/j.vaccine.2014.03.045. [DOI] [PubMed] [Google Scholar]
- 119.Li Y., Song H., Li J., Wang Y., Yan X., Zhao B., Zhang X., Wang S., Chen L., Qiu B., et al. Hansenula polymorpha expressed heat shock protein gp96 exerts potent T cell activation activity as an adjuvant. J. Biotechnol. 2011;151:343–349. doi: 10.1016/j.jbiotec.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 120.Wang S., Qiu L., Liu G., Li Y., Zhang X., Jin W., Gao G.F., Kong X., Meng S. Heat shock protein gp96 enhances humoral and T cell responses, decreases Treg frequency and potentiates the anti-HBV activity in BALB/c and transgenic mice. Vaccine. 2011;29:6342–6351. doi: 10.1016/j.vaccine.2011.05.008. [DOI] [PubMed] [Google Scholar]
- 121.Pawaria S., Binder R.J. CD91-dependent programming of T-helper cell responses following heat shock protein immunization. Nat. Commun. 2011;2:521. doi: 10.1038/ncomms1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Wang X.Y., Yi H., Yu X., Zuo D., Subjeck J.R. Enhancing antigen cross-presentation and T-cell priming by complexing protein antigen to recombinant large heat-shock protein. Methods Mol. Biol. 2011;787:277–287. doi: 10.1007/978-1-61779-295-3_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Chen W., Wang J., An H., Zhou J., Zhang L., Cao X. Heat shock up-regulates TLR9 expression in human B cells through activation of ERK and NF-κB signal pathways. Immunol. Lett. 2005;98:153–159. doi: 10.1016/j.imlet.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 124.Gandhapudi S.K., Murapa P., Threlkeld Z.D., Ward M., Sarge K.D., Snow C., Woodward J.G. Heat shock transcription factor 1 is activated as a consequence of lymphocyte activation and regulates a major proteostasis network in T cells critical for cell division during stress. J. Immunol. 2013;191:4068–4079. doi: 10.4049/jimmunol.1202831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Hardy L., Goodman M., Vasquez A., Chauhan D., Anderson K.C., Voellmy R., Spector N.L. Activation signals regulate heat shock transcription factor 1 in human B lymphocytes. J. Cell. Physiol. 1997;170:235–240. doi: 10.1002/(SICI)1097-4652(199703)170:3<235::AID-JCP3>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 126.Tukaj S., Tiburzy B., Manz R., de Castro Marques A., Orosz A., Ludwig R.J., Zillikens D., Kasperkiewicz M. Immunomodulatory effects of heat shock protein 90 inhibition on humoral immune responses. Exp. Dermatol. 2014;23:585–590. doi: 10.1111/exd.12476. [DOI] [PubMed] [Google Scholar]
- 127.Houlihan J.L., Metzler J.J., Blum J.S. HSP90α and HSP90β isoforms selectively modulate MHC class II antigen presentation in B cells. J. Immunol. 2009;182:7451–7458. doi: 10.4049/jimmunol.0804296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Cohen-Sfady M., Pevsner-Fischer M., Margalit R., Cohen I.R. Heat shock protein 60, via MyD88 innate signaling, protects B cells from apoptosis, spontaneous and induced. J. Immunol. 2009;183:890–896. doi: 10.4049/jimmunol.0804238. [DOI] [PubMed] [Google Scholar]
- 129.Li C., Liu D., Yuan Y., Huang S., Shi M., Tao K., Feng W. Overexpression of Apg-2 increases cell proliferation and protects from oxidative damage in BaF3-BCR/ABL cells. Int. J. Oncol. 2010;36:899–904. doi: 10.3892/ijo_00000568. [DOI] [PubMed] [Google Scholar]
- 130.Overgaard J., Gonzalez Gonzalez D., Hulshof M.C., Arcangeli G., Dahl O., Mella O., Bentzen S.M. Randomised trial of hyperthermia as adjuvant to radiotherapy for recurrent or metastatic malignant melanoma. European Society for Hyperthermic Oncology. Lancet. 1995;345:540–543. doi: 10.1016/S0140-6736(95)90463-8. [DOI] [PubMed] [Google Scholar]
- 131.Kim J.H. Combined hyperthermia and radiation therapy in cancer treatment: Current status. Cancer Investing. 1984;2:69–80. doi: 10.3109/07357908409020289. [DOI] [PubMed] [Google Scholar]
- 132.Datta N.R., Ordonez S.G., Gaipl U.S., Paulides M.M., Crezee H., Gellermann J., Marder D., Puric E., Bodis S. Local hyperthermia combined with radiotherapy and-/or chemotherapy: Recent advances and promises for the future. Cancer Treat. Rev. 2015;41:742–753. doi: 10.1016/j.ctrv.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 133.Zhao Q., Memezawa H., Smith M.L., Siesjo B.K. Hyperthermia complicates middle cerebral artery occlusion induced by an intraluminal filament. Brain Res. 1994;649:253–259. doi: 10.1016/0006-8993(94)91071-5. [DOI] [PubMed] [Google Scholar]
- 134.Gottlieb C.F., Hagmann M.J., Babij T.M., Abitbol A.A., Lewin A.A., Houdek P.V., Schwade J.G. Interstitial microwave hyperthermia applicators having submillimetre diameters. Int. J. Hyperth. 1990;6:707–714. doi: 10.3109/02656739009140966. [DOI] [PubMed] [Google Scholar]
- 135.Van der Zee J., Vujaskovic Z., Kondo M., Sugahara T. The Kadota Fund International Forum 2004--clinical group consensus. Int. J. Hyperth. 2008;24:111–122. doi: 10.1080/02656730801895058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Yahara K., Ohguri T., Yamaguchi S., Imada H., Narisada H., Ota S., Tomura K., Sakagami M., Fujimoto N., Korogi Y. Definitive radiotherapy plus regional hyperthermia for high-risk and very high-risk prostate carcinoma: Thermal parameters correlated with biochemical relapse-free survival. Int. J. Hyperth. 2015;31:600–608. doi: 10.3109/02656736.2015.1062214. [DOI] [PubMed] [Google Scholar]
- 137.Burfeindt M.J., Zastrow E., Hagness S.C., Van Veen B.D., Medow J.E. Microwave beamforming for non-invasive patient-specific hyperthermia treatment of pediatric brain cancer. Phys. Med. Biol. 2011;56:2743–2754. doi: 10.1088/0031-9155/56/9/007. [DOI] [PubMed] [Google Scholar]
- 138.Yu J.I., Park H.C., Oh D., Noh J.M., Jung S.H., Kim H.Y., Shin S.W., Cho S.K., Sinn D.H., Paik Y.H., et al. Combination treatment of trans-arterial chemo-embolisation, radiotherapy and hyperthermia (CERT) for hepatocellular carcinoma with portal vein tumour thrombosis: Interim analysis of prospective phase II trial. Int. J. Hyperth. 2016;32:331–338. doi: 10.3109/02656736.2016.1144895. [DOI] [PubMed] [Google Scholar]
- 139.Botsa E., Poulou L.S., Koutsogiannis I., Ziakas P.D., Koundouraki A., Alexopoulou E., Thanos L. CT-guided radiofrequency tumor ablation in children. Pediatr. Radiol. 2014;44:1421–1425. doi: 10.1007/s00247-014-3008-y. [DOI] [PubMed] [Google Scholar]
- 140.Facciorusso A., Di Maso M., Muscatiello N. Microwave ablation versus radiofrequency ablation for the treatment of hepatocellular carcinoma: A systematic review and meta-analysis. Int. J. Hyperth. 2016;32:339–344. doi: 10.3109/02656736.2015.1127434. [DOI] [PubMed] [Google Scholar]
- 141.Dovedi S.J., Adlard A.L., Lipowska-Bhalla G., McKenna C., Jones S., Cheadle E.J., Stratford I.J., Poon E., Morrow M., Stewart R., et al. Acquired resistance to fractionated radiotherapy can be overcome by concurrent PD-L1 blockade. Cancer Res. 2014;74:5458–5468. doi: 10.1158/0008-5472.CAN-14-1258. [DOI] [PubMed] [Google Scholar]
- 142.Zeng Z.C., Jiang G.L., Wang G.M., Tang Z.Y., Curran W.J., Iliakis G. DNA-PKcs subunits in radiosensitization by hyperthermia on hepatocellular carcinoma hepG2 cell line. World J. Gastroenterol. 2002;8:797–803. doi: 10.3748/wjg.v8.i5.797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Franken N.A., Van Bree C., Veltmaat M.A., Rodermond H.M., Haveman J., Barendsen G.W. Radiosensitization by bromodeoxyuridine and hyperthermia: Analysis of linear and quadratic parameters of radiation survival curves of two human tumor cell lines. J. Radiat. Res. 2001;42:179–190. doi: 10.1269/jrr.42.179. [DOI] [PubMed] [Google Scholar]
- 144.Zolzer F., Streffer C. Quiescence in S-phase and G1 arrest induced by irradiation and/or hyperthermia in six human tumour cell lines of different p53 status. Int. J. Radiat. Biol. 2000;76:717–725. doi: 10.1080/095530000138394. [DOI] [PubMed] [Google Scholar]
- 145.Garg A.D., Dudek A.M., Agostinis P. Cancer immunogenicity, danger signals, and DAMPs: What, when, and how? BioFactors. 2013;39:355–367. doi: 10.1002/biof.1125. [DOI] [PubMed] [Google Scholar]
- 146.Van Oorschot B., Granata G., Di Franco S., Ten Cate R., Rodermond H.M., Todaro M., Medema J.P., Franken N.A. Targeting DNA double strand break repair with hyperthermia and DNA-PKcs inhibition to enhance the effect of radiation treatment. Oncotarget. 2016;7:65504–65513. doi: 10.18632/oncotarget.11798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Xu M., Myerson R.J., Hunt C., Kumar S., Moros E.G., Straube W.L., Roti Roti J.L. Transfection of human tumour cells with Mre11 siRNA and the increase in radiation sensitivity and the reduction in heat-induced radiosensitization. Int. J. Hyperth. 2004;20:157–162. doi: 10.1080/02656730310001625986. [DOI] [PubMed] [Google Scholar]
- 148.Xu M., Myerson R.J., Xia Y., Whitehead T., Moros E.G., Straube W.L., Roti J.L. The effects of 41 degrees C hyperthermia on the DNA repair protein, MRE11, correlate with radiosensitization in four human tumor cell lines. Int. J. Hyperth. 2007;23:343–351. doi: 10.1080/02656730701383007. [DOI] [PubMed] [Google Scholar]
- 149.Gerashchenko B.I., Gooding G., Dynlacht J.R. Hyperthermia alters the interaction of proteins of the Mre11 complex in irradiated cells. Cytometry Part A. 2010;77:940–952. doi: 10.1002/cyto.a.20955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Zhu W.G., Seno J.D., Beck B.D., Dynlacht J.R. Translocation of MRE11 from the nucleus to the cytoplasm as a mechanism of radiosensitization by heat. Radiat. Res. 2001;156:95–102. doi: 10.1667/0033-7587(2001)156[0095:TOMFTN]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 151.Kaneko H., Igarashi K., Kataoka K., Miura M. Heat shock induces phosphorylation of histone H2AX in mammalian cells. Biochem. Biophys. Res. Commun. 2005;328:1101–1106. doi: 10.1016/j.bbrc.2005.01.073. [DOI] [PubMed] [Google Scholar]
- 152.Bergs J.W., Oei A.L., Ten Cate R., Rodermond H.M., Stalpers L.J., Barendsen G.W., Franken N.A. Dynamics of chromosomal aberrations, induction of apoptosis, BRCA2 degradation and sensitization to radiation by hyperthermia. Int. J. Mol. Med. 2016;38:243–250. doi: 10.3892/ijmm.2016.2611. [DOI] [PubMed] [Google Scholar]
- 153.Genet S.C., Fujii Y., Maeda J., Kaneko M., Genet M.D., Miyagawa K., Kato T.A. Hyperthermia inhibits homologous recombination repair and sensitizes cells to ionizing radiation in a time- and temperature-dependent manner. J. Cell. Physiol. 2013;228:1473–1481. doi: 10.1002/jcp.24302. [DOI] [PubMed] [Google Scholar]
- 154.Yin H.L., Suzuki Y., Matsumoto Y., Tomita M., Furusawa Y., Enomoto A., Morita A., Aoki M., Yatagai F., Suzuki T., et al. Radiosensitization by hyperthermia in the chicken B-lymphocyte cell line DT40 and its derivatives lacking nonhomologous end joining and/or homologous recombination pathways of DNA double-strand break repair. Radiat. Res. 2004;162:433–441. doi: 10.1667/RR3239. [DOI] [PubMed] [Google Scholar]
- 155.Blasiak J., Widera K., Pertynski T. Hyperthermia can differentially modulate the repair of doxorubicin-damaged DNA in normal and cancer cells. Acta Biochim. Pol. 2003;50:191–195. [PubMed] [Google Scholar]
- 156.Tomita M. Involvement of DNA-PK and ATM in radiation- and heat-induced DNA damage recognition and apoptotic cell death. J. Radiat. Res. 2010;51:493–501. doi: 10.1269/jrr.10039. [DOI] [PubMed] [Google Scholar]
- 157.Takahashi A., Ota I., Tamamoto T., Asakawa I., Nagata Y., Nakagawa H., Kondo N., Ohnishi K., Furusawa Y., Matsumoto H., et al. p53-dependent hyperthermic enhancement of tumour growth inhibition by X-ray or carbon-ion beam irradiation. Int. J. Hyperth. 2003;19:145–153. doi: 10.1080/02656730210166131. [DOI] [PubMed] [Google Scholar]
- 158.Mackey M.A., Ianzini F. Enhancement of radiation-induced mitotic catastrophe by moderate hyperthermia. Int. J. Radiat. Biol. 2000;76:273–280. doi: 10.1080/095530000138925. [DOI] [PubMed] [Google Scholar]
- 159.Kang J., Kim W., Lee S., Kwon D., Chun J., Son B., Kim E., Lee J.M., Youn H., Youn B. TFAP2C promotes lung tumorigenesis and aggressiveness through miR-183- and miR-33a-mediated cell cycle regulation. Oncogene. 2017;36:1585–1596. doi: 10.1038/onc.2016.328. [DOI] [PubMed] [Google Scholar]
- 160.Schildkopf P., Holmer R., Sieber R., Ott O.J., Janko C., Mantel F., Frey B., Fietkau R., Gaipl U.S. Hyperthermia in combination with X-irradiation induces inflammatory forms of cell death. Autoimmunity. 2009;42:311–313. doi: 10.1080/08916930902832041. [DOI] [PubMed] [Google Scholar]
- 161.Cui Y.H., Liang H.J., Zhang Q.Q., Li S.Q., Li X.R., Huo X.Q., Yang Q.H., Li W.W., Gu J.F., Hua Q.L., et al. Radiosensitivity enhancement by arsenic trioxide in conjunction with hyperthermia in the EC-1 esophageal carcinoma cell line. Asian Pac. J. Cancer Prev. 2012;13:1693–1697. doi: 10.7314/APJCP.2012.13.4.1693. [DOI] [PubMed] [Google Scholar]
- 162.Milanovic D., Firat E., Grosu A.L., Niedermann G. Increased radiosensitivity and radiothermosensitivity of human pancreatic MIA PaCa-2 and U251 glioblastoma cell lines treated with the novel Hsp90 inhibitor NVP-HSP990. Radiat. Oncol. 2013;8:42. doi: 10.1186/1748-717X-8-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Werthmoller N., Frey B., Ruckert M., Lotter M., Fietkau R., Gaipl U.S. Combination of ionising radiation with hyperthermia increases the immunogenic potential of B16-F10 melanoma cells in vitro and in vivo. Int. J. Hyperth. 2016;32:23–30. doi: 10.3109/02656736.2015.1106011. [DOI] [PubMed] [Google Scholar]
- 164.Liang H., Zhan H.J., Wang B.G., Pan Y., Hao X.S. Change in expression of apoptosis genes after hyperthermia, chemotherapy and radiotherapy in human colon cancer transplanted into nude mice. World J. Gastroenterol. 2007;13:4365–4371. doi: 10.3748/wjg.v13.i32.4365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Nijhuis E.H., Poot A.A., Feijen J., Vermes I. Induction of apoptosis by heat and gamma-radiation in a human lymphoid cell line; role of mitochondrial changes and caspase activation. Int. J. Hyperth. 2006;22:687–698. doi: 10.1080/02656730601045409. [DOI] [PubMed] [Google Scholar]
- 166.Liu W., Kang M., Qin Y., Wei Z., Wang R. Apoptosis-inducing effects of cetuximab combined with radiotherapy and hypothermia on human nasopharyngeal carcinoma CNE cells. Int. J. Clin. Exp. Med. 2015;8:2182–2189. [PMC free article] [PubMed] [Google Scholar]
- 167.Curry H.A., Clemens R.A., Shah S., Bradbury C.M., Botero A., Goswami P., Gius D. Heat shock inhibits radiation-induced activation of NF-κB via inhibition of I-κB kinase. J. Biol. Chem. 1999;274:23061–23067. doi: 10.1074/jbc.274.33.23061. [DOI] [PubMed] [Google Scholar]
- 168.Man J., Shoemake J.D., Ma T., Rizzo A.E., Godley A.R., Wu Q., Mohammadi A.M., Bao S., Rich J.N., Yu J.S. Hyperthermia sensitizes glioma stem-like cells to radiation by inhibiting AKT signaling. Cancer Res. 2015;75:1760–1769. doi: 10.1158/0008-5472.CAN-14-3621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Youn H., Son B., Kim W., Jun S.Y., Lee J.S., Lee J.M., Kang C., Kim J., Youn B. Dissociation of MIF-rpS3 complex and sequential NF-κB activation is involved in IR-induced metastatic conversion of NSCLC. J. Cell. Biochem. 2015;116:2504–2516. doi: 10.1002/jcb.25195. [DOI] [PubMed] [Google Scholar]
- 170.Kang J., Kim W., Kwon T., Youn H., Kim J.S., Youn B. Plasminogen activator inhibitor-1 enhances radioresistance and aggressiveness of non-small cell lung cancer cells. Oncotarget. 2016;7:23961–23974. doi: 10.18632/oncotarget.8208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Gabai V.L., Budagova K.R., Sherman M.Y. Increased expression of the major heat shock protein Hsp72 in human prostate carcinoma cells is dispensable for their viability but confers resistance to a variety of anticancer agents. Oncogene. 2005;24:3328–3338. doi: 10.1038/sj.onc.1208495. [DOI] [PubMed] [Google Scholar]
- 172.Johannsen M., Thiesen B., Gneveckow U., Taymoorian K., Waldofner N., Scholz R., Deger S., Jung K., Loening S.A., Jordan A. Thermotherapy using magnetic nanoparticles combined with external radiation in an orthotopic rat model of prostate cancer. Prostate. 2006;66:97–104. doi: 10.1002/pros.20324. [DOI] [PubMed] [Google Scholar]
- 173.Lin F.C., Hsu C.H., Lin Y.Y. Nano-therapeutic cancer immunotherapy using hyperthermia-induced heat shock proteins: Insights from mathematical modeling. Int. J. Nanomed. 2018;13:3529–3539. doi: 10.2147/IJN.S166000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Brondani Da Rocha A., Regner A., Grivicich I., Pretto Schunemann D., Diel C., Kovaleski G., Brunetto De Farias C., Mondadori E., Almeida L., Braga Filho A., et al. Radioresistance is associated to increased Hsp70 content in human glioblastoma cell lines. Int. J. Oncol. 2004;25:777–785. doi: 10.3892/ijo.25.3.777. [DOI] [PubMed] [Google Scholar]
- 175.Gibbons N.B., Watson R.W., Coffey R.N., Brady H.P., Fitzpatrick J.M. Heat-shock proteins inhibit induction of prostate cancer cell apoptosis. Prostate. 2000;45:58–65. doi: 10.1002/1097-0045(20000915)45:1<58::AID-PROS7>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 176.Postow M.A., Callahan M.K., Barker C.A., Yamada Y., Yuan J., Kitano S., Mu Z., Rasalan T., Adamow M., Ritter E., et al. Immunologic correlates of the abscopal effect in a patient with melanoma. N. Eng. J. Med. 2012;366:925–931. doi: 10.1056/NEJMoa1112824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Demaria S., Ng B., Devitt M.L., Babb J.S., Kawashima N., Liebes L., Formenti S.C. Ionizing radiation inhibition of distant untreated tumors (abscopal effect) is immune mediated. Int. J. Radiat. Oncol. Biol. Phys. 2004;58:862–870. doi: 10.1016/j.ijrobp.2003.09.012. [DOI] [PubMed] [Google Scholar]
- 178.Wang H., Zhang L., Shi Y., Javidiparsijani S., Wang G., Li X., Ouyang W., Zhou J., Zhao L., Wang X., et al. Abscopal antitumor immune effects of magnet-mediated hyperthermia at a high therapeutic temperature on Walker-256 carcinosarcomas in rats. Oncol. Lett. 2014;7:764–770. doi: 10.3892/ol.2014.1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Qin W., Akutsu Y., Andocs G., Suganami A., Hu X., Yusup G., Komatsu-Akimoto A., Hoshino I., Hanari N., Mori M., et al. Modulated electro-hyperthermia enhances dendritic cell therapy through an abscopal effect in mice. Oncol. Rep. 2014;32:2373–2379. doi: 10.3892/or.2014.3500. [DOI] [PubMed] [Google Scholar]
- 180.van Leeuwen C.M., Crezee J., Oei A.L., Franken N.A.P., Stalpers L.J.A., Bel A., Kok H.P. The effect of time interval between radiotherapy and hyperthermia on planned equivalent radiation dose. Int. J. Hyperth. 2018;34:1–9. doi: 10.1080/02656736.2018.1468930. [DOI] [PubMed] [Google Scholar]
- 181.Myerson R.J., Straube W.L., Moros E.G., Emami B.N., Lee H.K., Perez C.A., Taylor M.E. Simultaneous superficial hyperthermia and external radiotherapy: Report of thermal dosimetry and tolerance to treatment. Int. J. Hyperth. 1999;15:251–266. doi: 10.1080/026567399285639. [DOI] [PubMed] [Google Scholar]
- 182.Feyerabend T., Wiedemann G.J., Jager B., Vesely H., Mahlmann B., Richter E. Local hyperthermia, radiation, and chemotherapy in recurrent breast cancer is feasible and effective except for inflammatory disease. Int. J. Radiat. Oncol. Biol. Phys. 2001;49:1317–1325. doi: 10.1016/S0360-3016(00)01514-5. [DOI] [PubMed] [Google Scholar]
- 183.Harima Y., Nagata K., Harima K., Oka A., Ostapenko V.V., Shikata N., Ohnishi T., Tanaka Y. Bax and Bcl-2 protein expression following radiation therapy versus radiation plus thermoradiotherapy in stage IIIB cervical carcinoma. Cancer. 2000;88:132–138. doi: 10.1002/(SICI)1097-0142(20000101)88:1<132::AID-CNCR18>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 184.Harima Y., Nagata K., Harima K., Ostapenko V.V., Tanaka Y., Sawada S. A randomized clinical trial of radiation therapy versus thermoradiotherapy in stage IIIB cervical carcinoma. Int. J. Hyperth. 2001;17:97–105. doi: 10.1080/02656730903092018. [DOI] [PubMed] [Google Scholar]
- 185.Sakurai H., Hayakawa K., Mitsuhashi N., Tamaki Y., Nakayama Y., Kurosaki H., Nasu S., Ishikawa H., Saitoh J.I., Akimoto T., et al. Effect of hyperthermia combined with external radiation therapy in primary non-small cell lung cancer with direct bony invasion. Int. J. Hyperth. 2002;18:472–483. doi: 10.1080/02656730210146917. [DOI] [PubMed] [Google Scholar]
- 186.Verduijn G.M., de Wee E.M., Rijnen Z., Togni P., Hardillo J.A.U., Ten Hove I., Franckena M., van Rhoon G.C., Paulides M.M. Deep hyperthermia with the HYPERcollar system combined with irradiation for advanced head and neck carcinoma—A feasibility study. Int. J. Hyperth. 2018;34:1–8. doi: 10.1080/02656736.2018.1454610. [DOI] [PubMed] [Google Scholar]
- 187.van der Zee J., Gonzalez Gonzalez D., van Rhoon G.C., van Dijk J.D., van Putten W.L., Hart A.A. Comparison of radiotherapy alone with radiotherapy plus hyperthermia in locally advanced pelvic tumours: A prospective, randomised, multicentre trial. Lancet. 2000;355:1119–1125. doi: 10.1016/S0140-6736(00)02059-6. [DOI] [PubMed] [Google Scholar]
- 188.Jones E.L., Oleson J.R., Prosnitz L.R., Samulski T.V., Vujaskovic Z., Yu D., Sanders L.L., Dewhirst M.W. Randomized trial of hyperthermia and radiation for superficial tumors. J. Clin. Oncol. 2005;23:3079–3085. doi: 10.1200/JCO.2005.05.520. [DOI] [PubMed] [Google Scholar]
- 189.Mitsumori M., Zeng Z.F., Oliynychenko P., Park J.H., Choi I.B., Tatsuzaki H., Tanaka Y., Hiraoka M. Regional hyperthermia combined with radiotherapy for locally advanced non-small cell lung cancers: A multi-institutional prospective randomized trial of the International Atomic Energy Agency. Int. J. Clin. Oncol. 2007;12:192–198. doi: 10.1007/s10147-006-0647-5. [DOI] [PubMed] [Google Scholar]
- 190.Takahashi I., Emi Y., Hasuda S., Kakeji Y., Maehara Y., Sugimachi K. Clinical application of hyperthermia combined with anticancer drugs for the treatment of solid tumors. Surgery. 2002;131:S78–S84. doi: 10.1067/msy.2002.119308. [DOI] [PubMed] [Google Scholar]
- 191.Westermann A.M., Jones E.L., Schem B.C., van der Steen-Banasik E.M., Koper P., Mella O., Uitterhoeve A.L., de Wit R., van der Velden J., Burger C., et al. First results of triple-modality treatment combining radiotherapy, chemotherapy, and hyperthermia for the treatment of patients with stage IIB, III, and IVA cervical carcinoma. Cancer. 2005;104:763–770. doi: 10.1002/cncr.21128. [DOI] [PubMed] [Google Scholar]
- 192.Gofrit O.N., Shapiro A., Pode D., Sidi A., Nativ O., Leib Z., Witjes J.A., van der Heijden A.G., Naspro R., Colombo R. Combined local bladder hyperthermia and intravesical chemotherapy for the treatment of high-grade superficial bladder cancer. Urology. 2004;63:466–471. doi: 10.1016/j.urology.2003.10.036. [DOI] [PubMed] [Google Scholar]
- 193.Issels R.D., Lindner L.H., Verweij J., Wust P., Reichardt P., Schem B.C., Abdel-Rahman S., Daugaard S., Salat C., Wendtner C.M., et al. Neo-adjuvant chemotherapy alone or with regional hyperthermia for localised high-risk soft-tissue sarcoma: A randomised phase 3 multicentre study. Lancet Oncol. 2010;11:561–570. doi: 10.1016/S1470-2045(10)70071-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Atanackovic D., Nierhaus A., Neumeier M., Hossfeld D.K., Hegewisch-Becker S. 41.8 degrees C whole body hyperthermia as an adjunct to chemotherapy induces prolonged T cell activation in patients with various malignant diseases. Cancer Immunol. Immunother. 2002;51:603–613. doi: 10.1007/s00262-002-0327-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Takeda T., Takeda H., Tanaka C., Maruhashi S., Takeda T. The effect of immunotherapy and hyperthermia for advanced or recurrent head and neck cancer—74 clinical cases. Gan Kagaku Ryoho. 2014;41:1283–1285. [PubMed] [Google Scholar]
- 196.Takeda T., Takeda T., Kobayashi S., Takeda H. Immunotherapy with hyperthermia for advanced or recurrent breast cancer patients in whom standard therapy showed no effect or was refused. Gan Kagaku Ryoho. 2012;39:1766–1769. [PubMed] [Google Scholar]