Abstract
Background
Alcohol consumption has become one of the most common cancer risk factors after smoking. Nowadays, estimation of the burden of disease attributable to alcohol has become standard in documenting the impact of health problems, but it has been rarely performed in Indonesia. The aim of this study was to estimate treatment cost of cancer related to alcohol consumption among the Indonesian population.
Methods
This research design was descriptive with a prevalence-based approach using secondary data. Proportions of cancers were calculated using an alcohol-attributable fractions (AAF) formula. Treatment costs for eight types of cancer were assessed according to average treatment cost per patient from the national universal health coverage database for 2016.
Result
The top three AAFs for males were cancers of the pharynx, esophagus and larynx (17.5%, 15.3% and 7.98%, respectively), while in females they were cancers of the esophagus, pharynx and stomach (2.15%; 1.39%; 0.83%). Among the eight types of cancer studied, the highest incidence in males was noted for liver cancer (132 cases) while colorectal cancer was the most common among females (31 cases). Treatment cost for cancers related to alcohol consumption were highest for colorectak cancer followed by laryngeal and liver cancer (116,083, 98,325 and 93,253 USD, respectively.
Conclusion
The expenditure for treatment of cancers related to alcohol consumption accounts for about 1.71% of total cancer treatment cost. Since cancers related to alcohol consumption can be considered having an economic impact in Indonesia, it becomes important for the government to control alcohol consumption so that related healthcare expenditure can be minimized.
Keywords: Alcohol, cancer, treatment cost, Indonesia
Introduction
Alcohol consumption is one of the addictive behaviors which became major contributors to the global burden of morbidity and premature death (Global Burden of Disease Cancer Collaboration, 2017). Impact of alcohol on cancer have been increased from 4% to about 25% of the diseases burden worldwide (Gowing et al., 2015). Based on WHO Global Status Report on Alcohol 2014, cancer became one of the major causes of morbidity and mortality throughout the world, with about 14 million new cases and 8.2 million death-related cancer (Bosque-Prous et al., 2017). In 2015, cancer caused over 8.7 million deaths globally and was the second leading cause of death behind cardiovascular diseases (Global Burden of Disease Cancer Collaboration, 2017). A meta-analysis study done by Bagnardi et al showed there was association of cancers and level of alcohol drinking, which was represented by relative risk of cancer with intake of levels of alcohol, ranged from 1.14 to 8.32 (Bagnardi et al., 2015).
Cancer is considered as the most significant contributors of health care spending in the United States; as well treatment of cancer requires substantial funds (Chang et al., 2004). Health care spending in Europe during 1995-2014 was increasing continuously; it was estimated to be €35.7 billion in 1995 which increased to €83.2 billion in 2014 (Jönsson et al., 2016) Alcohol prevalence as well as economic burden of alcohol remains higher in Asian countries like Thailand, Taiwan, and China (Nganthavee, 2007; Liang et al., 2010; Thavorncharoensap et al., 2010; Hung et al., 2016).
According to WHO, the prevalence of alcohol consumption among the Indonesian population was about 7.1% (World Health Organization, 2014a). Over the past few decades, alcohol prevalence substantially higher in Indonesian adult men and also in women (Ministry of Health, 2013). Research on the burden of diseases especially cancers related to alcohol is not yet done in developing countries like Indonesia. Therefore, the aim of this study was to estimate the burden of cancer and treatment cost related to alcohol consumption among Indonesia population at the national level.
Materials and Methods
This research was secondary data study by using estimation prevalence-based with detail of diseases (Pérez-Ríos and Montes, 2008). Calculation of treatment cost based on concept of cost of illness by using governmental perspective. Direct estimates of morbidity cannot be made because there is a lack of longitudinal studies on the differential morbidity of alcohol drinkers, light, moderate, and heavy drinker, necessary to provide RR estimates for alcohol-related diseases. Original method proposed by Peto et al., (1992) requires incidence rates in those who did not expose risk factor, which are not available in Indonesia.
The alcohol consumption prevalence
The prevalence of drinkers in Indonesia was obtained from the WHO Global Status Report on Alcohol and Health 2014. The report contained data on the prevalence of alcohol use, heavy drinker status among the Indonesia population for > 15 years of age was 4.9% among male and 0.3% among the female (World Health Organization, 2014a).
Relative risk
Relative risk (RR) was calculated as per meta-analysis study associated with alcohol use and risk of cancer (Bagnardi et al., 2015). In our study RR was calculated for heavy intake of alcohol consumption adjusted with the available prevalence of data on alcohol consumption.
Determination of cancer related to alcohol consumption
The study included risks of 8 types of cancer like cancer of oral cavity, pharynx, esophagus, stomach, colorectum, liver, pancreas, larynx and lung with alcohol consumption. The data obtained was adjusted to the data available with BPJS 2016 (Indonesian Universal Health Coverage (BPJS), 2016) and RR from the meta-analysis study and alcohol-attributable fraction was calculated.
Incidence number of cancers
Incidence number of eight types of cancers was retrieved through secondary data from BPJS 2016 (Indonesian Universal Health Coverage (BPJS), 2016).
Estimation alcohol-attributable fractions (AAFs) and morbidity
AAFs represent the proportion of morbidity due to alcohol with the following formula:
AAF
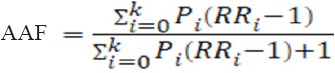
where:
i = exposure category with the initial exposure or no exposure (i = 0);
RRi = the relative risk exposure at the level i compared with no consumption;
Pi = the prevalence or incidence of exposure category (Rehm et al., 2009).
Then, incidence number or morbidity of cancer related to alcohol consumption (AAI) can be calculated by the formula:
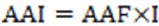
Where:
AAF = alcohol-attributable fraction of cancers;
I = morbidity (incidence number) of type of cancers.
Calculation treatment cost of cancer related to alcohol consumption
The direct costs of all cancers treatment for this study was obtained from the data of the National BPJS 2016. Treatment cost of cancers related to alcohol consumption was calculated by multiplying AAI with the treatment cost of cancer per patient.
Sensitivity analysis
One-way sensitivity analysis has done in an effort to identify the variables that potentially lead to significant changes in the results of the study. Variation of prevalence of alcohol consumption and relatives risk had assessed using one-way sensitivity analysis.
Results
In the study, highest AAFs among males were seen for cancer of pharynx (17.50%) followed by cancer of esophagus and larynx and among females it was seen for cancer of esophagus (2.15%) followed by cancer of pharynx and stomach (Table 1).
Table 1.
The Proportion of Eight Types of Cancer Related to Alcohol Consumption on Alcohol-Attributable Fractions (AAFs)
| No. | Cancer code | ICD-10 | RR* | AAFs (%) | ||
|---|---|---|---|---|---|---|
| Male | Female | Male | Female | |||
| 1 | Colorectum | C 18-21 | 1.53 | 3.23 | 2.53 | 0.66 |
| 2 | Esophageal | C 15 | 4.69 | 8.32 | 15.31 | 2.15 |
| 3 | Larynx | C 32 | 2.77 | 1.55 | 7.98 | 0.16 |
| 4 | Liver | C 22 | 1.59 | 1.24 | 2.81 | 0.07 |
| 5 | Pharynx | C 00-14 | 5.33 | 5.7 | 17.5 | 1.39 |
| 6 | Pancreas | C 25 | 1.16 | 1.17 | 0.78 | 0.05 |
| 7 | Lung | C 33-34 | 1.14 | 1.2 | 0.68 | 0.06 |
| 8 | Stomach | C 16 | 1.2 | 3.8 | 0.97 | 0.83 |
RRs were obtained from Bagnardi (Bagnardi V et al., 2015)
In the study, highest AAM among males were seen for liver cancer (215 cases) followed by colorectal cancer and cancer of larynx (132 and 104 cases) respectively and among females it was seen for cancer of colorectum (31cases) followed by cancer of stomach, lung and esophagus (5, 3, and 3) respectively (Table 2).
Table 2.
Number of Mortality (NOM) and Alcohol-Attributable Morbidity (AAM) of Eight Types of Cancer Related to Alcohol Consumption in Indonesia 2016
| No | Cancers | ICD-10 | NOM | AAM | |||
|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Total | |||
| 1 | Colorectum | C 18-21 | 5,204 | 4,636 | 132 | 31 | 163 |
| 2 | Esophagus | C 15 | 288 | 145 | 44 | 3 | 47 |
| 3 | Larynx | C 32 | 1,305 | 314 | 104 | 1 | 105 |
| 4 | Liver | C 22 | 7,649 | 3,358 | 215 | 2 | 217 |
| 5 | Pharynx | C 00-14 | 144 | 93 | 25 | 1 | 26 |
| 6 | Pancreas | C 25 | 1,013 | 899 | 8 | N/A | 8 |
| 7 | Lung | C 33-34 | 7,879 | 4,220 | 54 | 3 | 56 |
| 8 | Stomach | C 16 | 441 | 648 | 4 | 5 | 10 |
| Total | 23.923 | 14.313 | 586 | 47 | 632 | ||
| % of eight types of cancer | 2.45% | 0.33% | 1.65% | ||||
NOM, Number of mortality; AAM, Alcohol-attributable mortality; N/A, not available
Among the treatment cost, the total cost of cancer-related to alcohol consumption was highest among males (3, 88,952.19 USD) as compared to females (27,275.15 USD). Treatment costs among the 8 types of cancer-related to alcohol consumption among males were cancer of larynx which topped the list with 98.107.12 USD followed by colorectal and liver cancer (95,170.89 and 92,305.23 USD) respectively and among the females were colorectal cancer (20,912.48 USD) topped the list, followed by lung and esophageal cancer (1,839.08 and 1,494.34 USD) respectively. Overall, the highest total treatment cost of cancer-related to alcohol consumption especially in heavy level intake of alcohol was seen for colorectal cancer (116,083.37 USD) followed by cancer of larynx and liver (98,324.93 and 93,253.29 USD) respectively.
One-way sensitivity used by changing prevalence of alcohol consumption and relative risk of eight types of cancer related to alcohol consumption. Table 4 show prevalence changes by decreasing prevalence about 1%, 3% and 5% then, also increasing prevalence about 5%, 10%, and 20%.
Table 3.
Total Treatment Cost of Eight Types of Cancer Related to Alcohol Consumption in Indonesia 2016
| Cancer | ICD-10 code | Male | Female | Total of treatment cost (USD) | ||
|---|---|---|---|---|---|---|
| AAM | Treatment cost (USD) | AAM | Treatment cost (USD) | |||
| Colorectum | C 18-21 | 132 | 95,170.89 | 31 | 20,912.48 | 116,083.37 |
| Esophageal | C 15 | 44 | 42,326.26 | 3 | 1,494.34 | 43,820.60 |
| Larynx | C 32 | 104 | 98,107.12 | 1 | 217.81 | 98,324.93 |
| Liver | C 22 | 215 | 92,305.23 | 2 | 948.06 | 93,253.29 |
| Pharynx | C 00-14 | 25 | 10,830.10 | 1 | 203.59 | 11,033.69 |
| Pancreas | C 25 | 8 | 5,613.22 | N/A | N/A | 5,613.22 |
| Lung | C 33-34 | 54 | 42,997.76 | 3 | 1,839.08 | 44,836.84 |
| Stomach | C 16 | 4 | 1,601.61 | 5 | 1,340.67 | 2,942.28 |
| Total | 586 | 388,952.19 | 47 | 27,275.15 | 416,227.34 | |
N/A, not available; 1 USD, IDR 13,369 (based on http:/www.bi.go.id/moneter/informasi-kurs/transaksi-bi/Default.aspx per December 31st, 2016);
Table 4.
Data Changes Due to Prevalance Alternative
| Prevalence | AAF (%) | AAM (%) | Total treatment cost (%) | |||
|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | |
| Deccreased 1% | -0.9 | -1 | -1 | -1 | -0.9 | -1 |
| Decreased 3% | -2.6 | -3 | -2.9 | -3 | -2.8 | -3 |
| Decreased 5% | -4.4 | -4.9 | -4.8 | -5 | -4.7 | -5 |
| Increased 5% | 4.3 | 4.9 | 4.7 | 5 | 4.7 | 5 |
| Increased 10% | 8.6 | 9.8 | 9.5 | 9.9 | 9.4 | 9.9 |
| Increased 20% | 17 | 19.7 | 18.8 | 19.8 | 18.7 | 19.8 |
Discussion
Our study was the first study done in Indonesia to estimate the treatment cost of cancers related to alcohol consumption. Our study described the burden of cancer-related to alcohol consumption and would become a baseline study for the government to have control measures related to alcohol consumption so as to reduce the harmful effects of alcohol consumption. Alcohol was responsible for 1.65% of all cancer cases and treatment cost of cancer-related to alcohol consumption was seen highest in colorectum cancer followed by larynx and liver cancer in USD (116,083, 98,325 and 93,253) respectively.
Prevalence of cancers both in male and female has similarity on three top cancer, there were cancer of lung, liver, and colorectum. When compared to Globocan data 2012, estimated prevalence number of cancers on three top places in Indonesia also occupied by cancer of lung in first place (16.3% of total incidence of cancer in Indonesia) then followed by cancer of colorectum (12.8%), and liver (8.4%) (World Health Organization, 2014b).
Eight types of cancer in Indonesia both in male and female majority occurred in elderly population. Based on WHO data, life expectancy of the Indonesia population that is surviving at older ages in 2015 was about 67 years for male and 71 years for female. Age significantly increases the risk of cancer. In elderly people, other lifestyle that associated risks will also accumulated. The risk factors for the most common cancers have a long time to impact and increase the risk of disease in older people. A study explained that the incidence of most cancers increases with age, rising more rapidly beginning in midlife (45-64 years) (Whiteman and Wilson, 2016). Based on previous research, mechanism of the increase in cancer risk with age was related to dose-duration effect of carcinogenic exposures (Scoccianti et al., 2015).
AAFs was aimed to estimate the proportion of each cancer cases related to alcohol consumption. The highest AAFs in male is 17.50% can be interpreted that the proportion of pharynx cancer related to alcohol consumption is about 17.50% then followed by esophageal cancer (15.18%) and larynx cancer (7.91%). Then, for female, the highest AAFs is 2.15% can be interpreted that the proportion of esophageal cancer related to alcohol consumption is about 2.15%, then followed by pharynx cancer (1.39%) and stomach cancer (0.83%). From here, it can be showed that AAFs value in female smaller than male because the prevalence of heavy drinker in female is less than male.
Morbidity of eight types of cancer related to alcohol in male was higher than female, it was about 586 cases in male (2.45% of total incidence of eight types of cancer) and 47 cases (0.33% of total incidence of eight types of cancer). This was in accordance with prevalence of alcohol consumption higher in male than female. Overall, liver cancer have highest AAM that showed number of case of liver cancer due to alcohol consumption, it was about 217 cases (1.98% of total incidence of liver cancer), then followed by colorectum cancer (163 cases), and larynx cancer (105 cases). These trend was also happened in China, a study by Liang et al., (2010), showed that liver cancer was the main alcohol-related cancer, contributing more than 60% of alcohol-related cancer with total incidence number of liver cancer due to alcohol consumption. Among Korean women, the AAF for colorectal cancer incidence was the highest (4.2%) and about 0.5% (464 cancer cases) of incident cancers were attributable to alcohol consumption (Park et al., 2014). Based on research by Chang et al. (2017) examined about the association between alcohol and cancer in Asian people has been stating that ALDH2 polymorphism (ALDH2*2 allele) was responsible and play a role in causing cancer related to alcohol (Chang et al., 2017). López-Lázaro (2016) also explained there was a local mechanism of alcohol causing cancer. Ethanol that presenting in alcoholic beverages can causes a local cytotoxic effect in cells lining until cell death happened when the ethanol was passing the epithelial tissues such as in oral cavity, pharynx and esophagus.
Treatment cost of eight types of cancer related to alcohol consumption analyzed by calculating the direct treatment cost of eight types of cancer in Indonesia 2016. Total treatment cost of cancer related to alcohol consumption in 2016 was about 416,227.34 USD or 1.71% of total treatment of eight types of cancer. It was about 0.008% of total healthcare expenditure by government in 2016. Our finding was similar with previous research conducted in Thailand. The direct cost on health care was about 5,491.2 million Bath including treatment cost for laryngeal cancer, liver cancer, mouth and oropharynx cancer, esophageal cancer, stomach cancer and other diseases (Thavorncharoensap et al., 2010). Chemotherapy and radiation therapy use were the common largest cost of cancer treatment (Warren et al., 2008).
According to Basic Health Survey report 2013, cancer as a non-communicable diseases (NCDs) has prevalence data less than among other NCDs such as asthma and chronic obstructive pulmonary disease (COPD) (Ministry of Health, 2013). Even cancer prevalence less than others, but cancer classified as catastrophic diseases which has the characteristics of high cost and high risk of death, then actually much cost spent on cancer treatment. Like developing countries, developed countries also explained cancer is among the most significant contributors of healthcare spending, with direct treatment cost in 2002 at 60.9 billion USD (Chang et al., 2004), in 2006 spent healthcare cost about 11% (Bouchery et al., 2011) then in 2014 has increased to 87.7 billion USD (American Cancer Society, 2017). Interventions such as increased excise taxes, educational approaches highlighted the dangers of alcohol use are the most cost-effective intervention to reduce alcohol use (Kelly-Weeder et al., 2011). Then policy initiatives such as imposing punishment and prohibition for inebriation to reduce prevalence of alcohol consumption (Lai et al., 2007).
However, some limitations of the study need to be discussed. This result could be said to be under estimation with real cost because of some factors including the number of participants covered by national insurer was about 70% of total Indonesia population. In addition, not all participants utilize the health services offered by BPJS, for example some cancer patients prefer to use alternative treatment such as traditional medicine rather than formal health care services. Another limitation is relative risk (RR) has been used in this research was not from Indonesia then it could not represented fully of Indonesia’s cancer condition which is affected by demographic differences, and comorbidity disease beside cancer affected by other lifestyles. Our finding could be considered by government to reduce healthcare expenditure of cancer related to alcohol wherefore the prevalence of alcohol consumption has increased in recent years.
Despite these limitations, our results show the importance and the priority to be accorded to reduce the rate of alcohol consumption in the Indonesian population. A reduction in alcohol consumption would decrease the cancer burden and a significant impact is anticipated specifically for healthcare cost related to alcohol consumption.
References
- 1.Bagnardi V, Rota M, Botteri E, et al. Alcohol consumption and site-specific cancer risk: a comprehensive dose-response meta-analysis. Br J Cancer. 2015;112:580–93. doi: 10.1038/bjc.2014.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bouchery EE, Harwood HJ, Sacks JJ, et al. Economic costs of excessive alcohol consumption in the U.S. Am J Prev Med. 2011;41:516–24. doi: 10.1016/j.amepre.2011.06.045. [DOI] [PubMed] [Google Scholar]
- 3.Chang JS, Hsiao JR, Chen CH. ALDH2 polymorphism and alcohol-related cancers in Asians: a public health perspective. J Biomed Sci. 2017;24:3524–30. doi: 10.1186/s12929-017-0327-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chang SR, Long S, Kutikova L. Estimating the cost of cancer: Results on the basis of claims data analyses for cancer patients diagnosed with seven types of cancer during 1999 to 2000. J Clin Oncol. 2004;22:3524–30. doi: 10.1200/JCO.2004.10.170. [DOI] [PubMed] [Google Scholar]
- 5.Global Burden of Disease Cancer Collaboration. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted fife-years for 32 cancer groups, 1990 to 2015: A systematic analysis for the Global Burden of Disease Study. JAMA Oncol. 2017;3:524–48. doi: 10.1001/jamaoncol.2016.5688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gowing LR, Ali RL, Allsop S, et al. Global statistics on addictive behaviours:2014 status report: Addiction global statistics. Addiction. 2015;110:904–19. doi: 10.1111/add.12899. [DOI] [PubMed] [Google Scholar]
- 7.Hung MC, Lai WW, Chen HHW, et al. Cost effectiveness of cancer treatment in Taiwan. J Formos Med Assoc. 2016;115:509–16. doi: 10.1016/j.jfma.2016.04.002. [DOI] [PubMed] [Google Scholar]
- 8.Jönsson B, Hofmarcher T, Lindgren P, et al. The cost and burden of cancer in the European Union 1995-2014. Eur J Cancer. 2016;66:162–70. doi: 10.1016/j.ejca.2016.06.022. [DOI] [PubMed] [Google Scholar]
- 9.Kelly-Weeder S, Phillips K, Rounseville S. Effectiveness of public health programs for decreasing alcohol consumption. Patient Intell. 2011;29:29–38. doi: 10.2147/PI.S12431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lai T, Habicht J, Reinap M, et al. Costs, health effects and cost-effectiveness of alcohol and tobacco control strategies in Estonia. Health Policy. 2007;84:75–88. doi: 10.1016/j.healthpol.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 11.Liang H, Wang J, Xiao H, et al. Estimation of cancer incidence and mortality attributable to alcohol drinking in China. BMC Public Health. 2010;10:730–5. doi: 10.1186/1471-2458-10-730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.López-Lázaro M. A local mechanism by which alcohol consumption causes cancer. Oral Oncol. 2016;62:149–52. doi: 10.1016/j.oraloncology.2016.10.001. [DOI] [PubMed] [Google Scholar]
- 13.Nganthavee W. The economic burden of smoking-related disease in Thailand: a prevalence-based analysis. J Med Assoc Thai. 2007;90:1925–9. [PubMed] [Google Scholar]
- 14.Park SM, Lu Z, Lee C. Attributable fraction of alcohol consumption on cancer using population-based nationwide cancer incidence and mortality data in the Republic of Korea. BMC Cancer. 2014;14:14420. doi: 10.1186/1471-2407-14-420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pérez-Ríos M, Montes A. Methodologies used to estimate tobacco-attributable mortality: a review. BMC Public Health. 2008;8:8–22. doi: 10.1186/1471-2458-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peto R, Lopez AD, Boreham J, et al. Mortality from tobacco in developed countries: indirect estimation from national vital statistics. Lancet. 1992;339:1268–78. doi: 10.1016/0140-6736(92)91600-d. [DOI] [PubMed] [Google Scholar]
- 17.Rehm J, Mathers C, Popova S, et al. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373:2223–33. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- 18.Scoccianti C, Cecchini M, Anderson AS, et al. European code against cancer 4th Edition: Alcohol drinking and cancer. Cancer Epidemiol. 2015;39:67–74. doi: 10.1016/j.canep.2015.01.007. [DOI] [PubMed] [Google Scholar]
- 19.Thavorncharoensap M, Teerawattananon Y, Yothasamut J, et al. The economic costs of alcohol consumption in Thailand. BMC Public Health. 2010;10:323–7. doi: 10.1186/1471-2458-10-323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Warren Jl, Yabroff KR, Meekins A, et al. Evaluation of trends in the cost of initial cancer treatment. J Natl Cancer Inst. 2008;100:888–97. doi: 10.1093/jnci/djn175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Whiteman DC, Wilson LF. The fractions of cancer attributable to modifiable factors: A global review. Cancer Epidemiol. 2016;44:203–21. doi: 10.1016/j.canep.2016.06.013. [DOI] [PubMed] [Google Scholar]


