Abstract
Introduction
Shisha (waterpipe) smoking is becoming a very prevalent form of tobacco consumption in the Middle east and use is growing over the world. Smoking-related malignancies have a high genome-wide burden of mutations, including examples in the gene encoding p53.
Aims
To investigate alterations in p53 immunohistochemical expression in the normal, pre-malignant, malignant oral mucosa in relation to Shisha smoking habits.
Materials and Methods
A total of 105 paraffin embedded tissue sections of OSCCs (52 smokers,53 non-smokers), 96 of premalignant lesions (48 smokers,48 non-smokers) and 60 normal oral mucosa. Some 30 patients with a history of Shisha smoking daily for more than 5 years were also investigated for mutant expression of p53. Tissue samples were considered positive for p53 staining when any positive cells of epithelial origin could be detected.
Results
The majority (74.3%) of oral squamous cell carcinomas showed positive staining for p53 expression (83.1% and 65.5% with Shisha smokers and non-smokers, respectively). In the 96 premalignant lesions, about 23% from non-smokers and 41.7% from smokers showed p53 positivity. In normal epithelium, P53 positive cells were noted in 6.6% of non-smokers and 16.6% of smokers. Positive correlations with Shisha smoking were evident for the following groups: WDOSCC, MDOSCC, mild dysplasia G1, moderate dysplasia G2 and in normal mucosa using Student’s t- test, P value<0.05.
Conclusion
These results strongly suggest that p53 mutations are associated with Shisha smoking in OSCC, pre-malignant lesions and normal mucosa of the oral cavity.
Keywords: Shisha, malignancy, oral mucosa, p53
Introduction
Shisha is a smoking tool also known as Narghile, Hubble bubble, water pipe and hookah in various cultures and countries. It is a device for smoking tobacco in which the vapor passes through water before inhalation to the lungs through the upper respiratory tracts (Sameer et al., 2012). The source of this device belongs to the Eastern Mediterranean region and is now gaining popularity all around the world (Brockman et al., 2012). In the recent two decades, Shisha smoking habits are wildly spread especially by the youth mainly university and college students and also high school children (Neergaard et al., 2007).
Many public health officials considered Shisha as a global threat and given the status of an epidemic. Shisha smoke contains over 4800 different chemicals out of which 69 are carcinogens and several others are tumor promoters (Aslam et al., 2014). Shisha smoking, compared to cigarette smoking, can result in more smoke exposure and greater levels of carbon monoxide (CO) (La Fauci et al., 2012). Although this bad oral habit had is implicated in many types of carcinogenesis in the Middle East (Kadhum et al., 2015), still,1 it’s pathological direct effects unclear.
Shisha poses three sources of danger: First; from tobacco smoke inhalation, Second; from charcoal smoke inhalation, and Third; from infection through the shared use of Shisha tubes. People are familiar with the risks of tobacco smoking, but in case of Shisha, we have other effects such as charcoal smoke, new smoking environments and second-hand smoke which can cause infections (Ramachandra and Yaldrum, 2015).
P53 (the tumor suppressor protein) was first discovered in a complex with the simian virus 40 (SV40) large T-antigen (Lane and Crawford, 1979). It is involved in apoptosis, suppressing of the cell cycle, senescence, differentiation and DNA repair (Acha-Sagredo et al., 2009). Alterations of p53 expression have been reported to be an early event in the development of many carcinomas and its detection may be considered as a biomarker for these early stages of carcinogenesis (Partridge et al., 2007).
An abnormal p53 expression is considered as a predictive of the transformation process of many types of epithelial dysplasia to cancer (Kaye, 2015; Cuevas Gonzalez et al., 2016) especially OSCC which is a tumor type accounting for more than 90% of head and neck malignancies (Zaid et al., 2016)
The aim of the current study was to determine the status of the tumour suppressor gene p53 expression in a group of patients who had a long-term of attending Shisha smoking habit and have more chances to develop oral epithelial dysplasia OED or oral cancers OC (Morse et al., 2007) and in tissue samples of OSCC and Oral dysplasia patients.
Materials and Methods
105 paraffin embedded tissue sections of oral squamous cell carcinomas (OSCC), 96 sections of Epithelial premalignant lesions (leukoplakia and lichen planus) all those patients were shisha smokers at least 3 times per week at the last 5 years before they were diagnosed with the lesion, and 60 normal oral mucosa from the sites of 3rd molars extraction, 30 patients of them had attended Shish smoking at least 3 times per week for more than 5 years, classified as in Tale1, were immunohistochemically stained with a Mouse Monoclonal antibody for the presence of p53 (Prediluted, MMab, Do 7, IgG2b/K, BIO-sb). First the paraffin blocks were cut in 4 microns thicknesses and embedded on positive charged slides Bio SB Hydrophilic Plus Slides (BSB 7028), then dried by air for 2 hours at 58° C, after that Deparaffinized, dehydrated and rehydrated, then subjected to heat epitope retrieval using ImmunoDNA Retriever with Citrate (BSB 0020-BSB 0023). Then heated using a steamer by placing the slides in a pre-warmed staining dish containing the ImmunoDNA Retriever with Citrate in a Steamer, covered and steamed for 30-60 minutes. After heat treatment, the slides were transferred to ImmunoDNA Retriever with Citrate to room temperature and let stand for 15-20 minutes. The antibody was incubated at ambient temperature. Slides were washed with IHC wash buffer then treated with Peroxidase/AP Blocker for 5 min, Primary Antibody 45 min, Substrate-Chromogen 7 min and finally with hematoxylin.
Tissue samples were considered positive for p53 staining when only one positive cell of epithelial origin could be detected in the sample. In the p53 positive tissue specimens, cell counts of the positive cells in five different areas of the slide, in defined size and standardized location, were performed to quantify the p53 expression.
Mutations of p53 gene lead the p53 protein to be stabilized and extend it’s half-life, so it becomes detectable by immunohistological staining techniques (Porter et al., 2016). Detection of p53 by immunohistology might be caused by the stabilization of the protein due to the presence of mutation or result from promotion driven mechanisms that lead to increased p53 at the steady state in a cell cycle checkpoint response mechanism (Girod et al., 1994).
Table 1.
The Distribution of the Study Samples
| Tissues source | Smokers | Non-Smokers | Total | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| OSCC | 52 | 49.50 | 53 | 51.50 | 105 |
| WDOSCC | 22 | 20.90 | 23 | 21.90 | 45 |
| MDOSCC | 15 | 14.20 | 15 | 14.20 | 30 |
| PDOSCC | 15 | 14.20 | 15 | 14.20 | 30 |
| Premalignant Lesions | 48 | 50 | 48 | 50 | 96 |
| Hyperplastic lesions G0 | 12 | 12.50 | 12 | 12.50 | 24 |
| Mild dysplasia G1 | 12 | 12.50 | 12 | 12.50 | 24 |
| Moderate dysplasia G2 | 12 | 12.50 | 12 | 12.50 | 24 |
| Severe dysplasia G3 | 12 | 12.50 | 12 | 12.50 | 24 |
| Normal mucosa | 30 | 50 | 30 | 50 | 60 |
Results
P53 positivity was seen in man samples, it was mainly located at the basal and parabasal layers of normal and premalignant mucosa, while it was more scattered in the malignant mucosa especially with the poorly differentiated cases, Figures (1, 2 and 3). Shisha smoking was associated with an increase in the number of uniformly distributed proliferating cells, and also with focally p53-positive mucosa.
Figure 1.
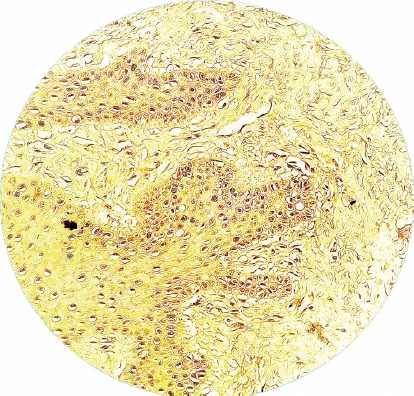
P53 Expression of Normal Mucosa in Smoker Normal Mucosa
Figure 2.
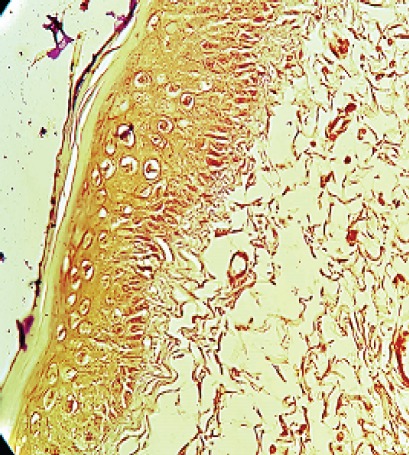
P53 Expression of Leukoplakia in Non- Smoker Sample
Figure 3.
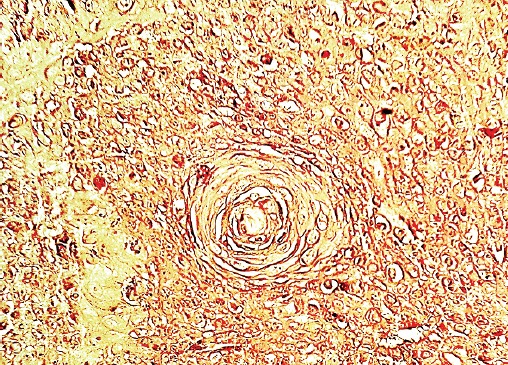
P53 Expression of WDOSCC in Smokers Sample
Of 105 tissue samples of oral squamous cell carcinomas, 78 samples (74.3%) showed a positive staining for p53 expression, 65.5% (n= 34) of non-smokers and 83.1% (n=43) of Shisha smokers. In the 96 patients with premalignant lesions, about 23% (n=10) of the non-smokers and 41.7% (n= 20) of the Shisha smokers showed p53 positivity. In the patients with normal epithelium, P53 positive cells were noticed in 6.6% (n=2) of the non-smokers and 16.6% (n=5) of the smokers. Detailed percentages of each group are located in the Figure 4.
Figure 4.
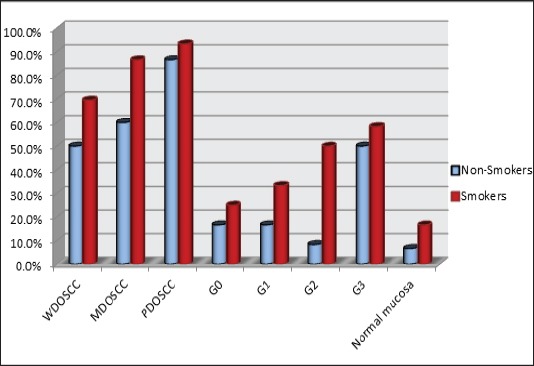
Chart of P53 Expression in the Study Samples
The quantification of p53 expression in the positive tissue samples showed a positive correlation with Shisha Smoking in the following groups: WDOSCC, MDOSCC, Mild dysplasia G1, Moderate dysplasia G2 and in normal mucosa using t-student test, P value<0.05.
Discussion
Shisha smoking is an ancient practice of tobacco use in the Arab world especially in Syria and Lebanon where people of all ages, especially colleges students, are used to smoke Shisha almost daily. And such bad oral habits have many forms including Shisha, and alcohol consumption is estimated to account for approximately 75% of cancers of the oral cavity (Hashibe et al., 2007; Pare and Joly, 2017; Yakin et al., 2017). Actually, there is no sufficient data about the Shisha smoking frequency in Syria and Lebanon. However, it is supposed to be higher than other countries such as the USA where the results demonstrate that approximately 1 in 5 American college students reports past-year Shisha use. Results also suggest that there are a number of established correlates of Shisha smoking, including male gender, Arab ethnicity, cigarette smoking, and the belief that Shisha smoking is less harmful than cigarette smoking (Grekin and Ayna, 2012).
Also, there are many studies revealed that the relationship between smoking and OED was as strong as that for smoking and OC, suggesting that smoking may have its greatest impact on oral carcinogenesis prior to malignant transformation (Morse et al., 2007). The observation that p53 alterations are early events in the tumorigenesis of the oral cavity and the association with smoking have prompted us to investigate for p53 expression also in the normal oral mucosa of Shisha smokers who have no overt precancerous or cancerous lesions and consuming Shisha for at least 5 years.
In the current study as in many other studies worldwide, we found a positive correlation between smoking and P53 positivity in the benign and malignant oral mucosa tissue. The focally p53-positive mucosa in smokers samples might be an indication that Shisha smoking induces early mucosal alterations in the development of OSCC (van Oijen et al., 1999).
Our results are in concordance with Ayan et al who had investigated the p53 expression in heavy smoker’s normal mucosa and detected a Positive immunoreaction for p53 in (20%) of his normal oral tissue samples (Ayan et al., 2000).
A significantly increased level of micronuclei in Shisha smokers was detected by Setouhy et al who had investigated the oral smears of these patients (El-Setouhy et al., 2008), usually, micronuclei in exfoliated human oral cells is a small intranuclear DNA structure separated from the main nucleus of the basal epithelial layers. Exfoliation of micronuclei in human oral cells is a normal process and the normal frequency is 1–3 per 1,000 cells. Upon exposure to certain carcinogenic stimuli (such as pesticides, radiation), however, the frequency of exfoliation of micronuclei is increased with Shisha smokers and this ensures the effects of this form of smoking on the cell cycle and proliferative activity (Kashyap and Reddy, 2012).
Shisha smoking induces similar amounts of carcinogenesis as does cigarette smoking (Ramachandra and Yaldrum, 2015). Rastam et al., (2010) found that Exposing oral epithelial cells to the continuous Shisha smoking may initiate carcinogenic transformation in these cells.
However, smoking is associated with p53 mutations in OSCC (Brennan et al., 1995) and premalignant lesions as Lazarus et al., (1995) suggested that p53 mutation may be a very early event in oral cavity tumor progression and demonstrated that pre-malignant lesions obtained from non-tobacco users do not exhibit p53 mutations. Furthermore, the expression of p53 above the basal layer in the epithelium is considered as an early stage of oral carcinogenesis and an indicator of a developing carcinoma, even preceding morphological tissue alterations (Cruz et al., 1998).
In conclusion, these results strongly suggest that p53 mutation is associated with Shisha smoking in OSCC, pre-malignant lesions and normal mucosa of the oral cavity. Shisha smokers with had a higher risk for p53 mutation than non-smokers. Rules should be made to restrict this bad habit, especially with young people.
References
- 1.Acha-Sagredo A, Ruesga MT, Rodriguez C, et al. p53 mutation is rare in oral mucosa brushings from patients previously treated for a head and neck squamous cell carcinoma. Oral Oncol. 2009;45:661–4. doi: 10.1016/j.oraloncology.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 2.Aslam HM, Saleem S, German S, et al. Harmful effects of shisha: literature review. Int Arch Med. 2014;7:16. doi: 10.1186/1755-7682-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ayan N, Ayan I, Alatli C, et al. P53 overexpression in normal oral mucosa of heavy smokers. J Exp Clin Cancer Res. 2000;19:525–9. [PubMed] [Google Scholar]
- 4.Brennan JA, Boyle JO, Koch WM, et al. Association between cigarette smoking and mutation of the p53 gene in squamous-cell carcinoma of the head and neck. N Engl J Med. 1995;332:712–7. doi: 10.1056/NEJM199503163321104. [DOI] [PubMed] [Google Scholar]
- 5.Brockman LN, Pumper MA, Christakis DA, et al. Hookah's new popularity among US college students: a pilot study of the characteristics of hookah smokers and their Facebook displays. BMJ Open. 2012;2 doi: 10.1136/bmjopen-2012-001709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cruz IB, Snijders PJ, Meijer CJ, et al. p53 expression above the basal cell layer in oral mucosa is an early event of malignant transformation and has predictive value for developing oral squamous cell carcinoma. J Pathol. 1998;184:360–8. doi: 10.1002/(SICI)1096-9896(199804)184:4<360::AID-PATH1263>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 7.Cuevas Gonzalez JC, Gaitan Cepeda LA, Borges Yanez SA, et al. p53 and p16 in oral epithelial dysplasia and oral squamous cell carcinoma: A study of 208 cases. Indian J Pathol Microbiol. 2016;59:153–8. doi: 10.4103/0377-4929.182037. [DOI] [PubMed] [Google Scholar]
- 8.El-Setouhy M, Loffredo CA, Radwan G, et al. Genotoxic effects of waterpipe smoking on the buccal mucosa cells. Mutat Res. 2008;655:36–40. doi: 10.1016/j.mrgentox.2008.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Girod SC, Kramer C, Knufermann R, et al. p53 expression in the carcinogenesis in the oral mucosa. J Cell Biochem. 1994;56:444–8. doi: 10.1002/jcb.240560404. [DOI] [PubMed] [Google Scholar]
- 10.Grekin ER, Ayna D. Waterpipe smoking among college students in the United States: a review of the literature. J Am Coll Health. 2012;60:244–9. doi: 10.1080/07448481.2011.589419. [DOI] [PubMed] [Google Scholar]
- 11.Hashibe M, Brennan P, Benhamou S, et al. Alcohol drinking in never users of tobacco, cigarette smoking in never drinkers, and the risk of head and neck cancer: pooled analysis in the International Head and Neck Cancer Epidemiology Consortium. J Natl Cancer Inst. 2007;99:777–89. doi: 10.1093/jnci/djk179. [DOI] [PubMed] [Google Scholar]
- 12.Kadhum M, Sweidan A, Jaffery AE, et al. A review of the health effects of smoking shisha. Clin Med (Lond) 2015;15:263–6. doi: 10.7861/clinmedicine.15-3-263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kashyap B, Reddy PS. Micronuclei assay of exfoliated oral buccal cells: means to assess the nuclear abnormalities in different diseases. J Cancer Res Ther. 2012;8:184–91. doi: 10.4103/0973-1482.98968. [DOI] [PubMed] [Google Scholar]
- 14.Kaye PV. p53 immunohistochemistry as a biomarker of dysplasia and neoplastic progression in Barrett's oesophagus. Diagn Histopathol. 2015;21:89–98. [Google Scholar]
- 15.La Fauci G, Weiser G, Steiner IP, et al. Carbon monoxide poisoning in narghile (water pipe) tobacco smokers. CJEM. 2012;14:57–9. doi: 10.2310/8000.2011.110431. [DOI] [PubMed] [Google Scholar]
- 16.Lane DP, Crawford LV. T antigen is bound to a host protein in SY40-transformed cells. Nature. 1979;278:261–3. doi: 10.1038/278261a0. [DOI] [PubMed] [Google Scholar]
- 17.Lazarus P, Garewal HS, Sciubba J, et al. A low incidence of p53 mutations in pre-malignant lesions of the oral cavity from non-tobacco users. Int J Cancer. 1995;60:458–63. doi: 10.1002/ijc.2910600406. [DOI] [PubMed] [Google Scholar]
- 18.Morse DE, Psoter WJ, Cleveland D, et al. Smoking and drinking in relation to oral cancer and oral epithelial dysplasia. Cancer Causes Control. 2007;18:919–29. doi: 10.1007/s10552-007-9026-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Neergaard J, Singh P, Job J, et al. Waterpipe smoking and nicotine exposure: a review of the current evidence. Nicotine Tob Res. 2007;9:987–94. doi: 10.1080/14622200701591591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pare A, Joly A. Oral cancer: Risk factors and management. Press Med. 2017;46:320–30. doi: 10.1016/j.lpm.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 21.Partridge M, Costea DE, Huang X. The changing face of p53 in head and neck cancer. Int J Oral Maxillofac Surg. 2007;36:1123–38. doi: 10.1016/j.ijom.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 22.Porter JR, Fisher BE, Batchelor E. p53 pulses diversify target gene expression dynamics in an mRNA half-life-dependent manner and delineate co-regulated target gene subnetworks. Cell Syst. 2016;2:272–82. doi: 10.1016/j.cels.2016.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ramachandra SS, Yaldrum A. Shisha smoking: An emerging trend in Southeast Asian nations. J Public Health Policy. 2015;36:304–17. doi: 10.1057/jphp.2015.16. [DOI] [PubMed] [Google Scholar]
- 24.Rastam S, Li FM, Fouad FM, et al. Water pipe smoking and human oral cancers. Med Hypotheses. 2010;74:457–9. doi: 10.1016/j.mehy.2009.10.013. [DOI] [PubMed] [Google Scholar]
- 25.Sameer ur R, Sadiq MA, Parekh MA, et al. Cross-sectional study identifying forms of tobacco used by Shisha smokers in Pakistan. J Pak Med Assoc. 2012;62:192–5. [PubMed] [Google Scholar]
- 26.van Oijen MG, van de Craats JG, Slootweg PJ. p53 overexpression in oral mucosa in relation to smoking. J Pathol. 1999;187:469–74. doi: 10.1002/(SICI)1096-9896(199903)187:4<469::AID-PATH262>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 27.Yakin M, Gavidi RO, Cox B, et al. Oral cancer risk factors in New Zealand. N Z Med J. 2017;130:30–8. [PubMed] [Google Scholar]
- 28.Zaid KW, Chantiri M, Bassit G. Recombinant human bone morphogenetic protein-2 in development and progression of oral squamous cell carcinoma. Asian Pac J Cancer Prev. 2016;17:927–32. doi: 10.7314/apjcp.2016.17.3.927. [DOI] [PubMed] [Google Scholar]


