Abstract
Objective
Examine readmission patterns over 90-day episodes of care in persons discharged from hospitals to post-acute settings.
Design
Retrospective cohort study.
Setting
Acute care hospitals.
Participants
Medicare fee-for-service enrollees (N=686,877) discharged from hospitals to post-acute care in 2013–2014. The cohort included beneficiaries >65 years of age hospitalized for stroke, joint replacement, or hip fracture and who survived for 90 days following discharge.
Measurements
90-day unplanned readmissions.
Results
The cohort included 127,680 individuals with stroke, 442,195 undergoing joint replacement, and 117,002 with hip fracture. Thirty-day readmission rates ranged from 3.1% for knee replacement patients discharged to home health agencies (HHA) to 14.4% for hemorrhagic stroke patients discharged to skilled nursing facilities (SNF). Ninety-day readmission rates ranged from 5.0% for knee replacement patients discharged to HHA to 26.1% for hemorrhagic stroke patients discharged to SNF. Differences in readmission rates decreased between stroke sub-conditions (hemorrhagic and ischemic) and increased between joint replacement sub-conditions (knee, elective hip, and non-elective hip) from 30 to 90 days across all initial post-acute discharge settings.
Conclusions
We observed clear patterns in readmissions over 90-day episodes of care across post-acute discharge settings and sub-conditions. Our findings suggest that patients with hemorrhagic stroke may be more vulnerable than those with ischemic over the first 30 days after hospital discharge. For patients receiving non-elective joint replacements, readmission prevention efforts should start immediately after discharge and continue, or even increase, over the 90-day episode of care.
Keywords: quality of care, health services research, healthcare reform, outcomes research
INTRODUCTION
Value-based payment reforms have redefined “episodes of care”.1–4 Under episode-based payment models, provider responsibility no longer ends at patient discharge. Medicare is testing the feasibility of bundling payments for 90-day episodes of care for selected conditions, such as lower extremity joint replacements.4 This expanded view of episodes of care aligns with patient needs and priorities. Recovery from an illness or injury frequently requires care across multiple providers.1, 2 Episode-based payment models are intended to encourage coordination and integration across acute- and post-acute providers and facilities.4
Following hospitalization, approximately 42% of Medicare fee-for-service beneficiaries receive post-acute care through skilled nursing facilities (SNF, 21%), inpatient rehabilitation facilities (IRF, 4%), or home health agencies (HHA, 17%).5, 6 The goal of post-acute care is to help patients further recuperate after hospitalization.5 These services are initially more costly,5 but based on the premise that post-acute services will improve long-term outcomes. This premise is the topic of ongoing investigation and debate.7, 8
The purpose of this study was to examine hospital readmission patterns over 90 days in persons discharged from acute hospitals to post-acute settings. We studied records for Medicare beneficiaries hospitalized for stroke, lower extremity joint replacement, or hip/femur fracture. We were specifically interested in these patient populations because they are 1) included in episode-based payment models9 and 2) commonly referred to post-acute care.10 Stroke, lower extremity joint replacement, and hip/femur fracture are common conditions treated in the SNF, IRF, and HHA post-acute settings, and subsequently may be impacted by episode-based payment models.10 Referral patterns, patient severity, and patient outcomes will be important to monitor as new payment models are implemented. Our findings provide baseline information on readmissions. Readmissions are an established quality measure, represent an undesirable outcome for patients and providers,11,12,13,14 and contribute to rising healthcare costs.5 We stratified our primary conditions of stroke, joint replacement, and hip/femur fracture into sub-conditions (e.g., ischemic vs. hemorrhagic stroke). A secondary objective was to determine whether differences in readmission rates between sub-conditions were stable or changed between 30 and 90 days.
METHODS
Data Sources
We used 2012–2014 100% Medicare Provider Analysis and Review (MedPAR), Beneficiary Summary, and Home Health claims files. The MedPAR files include finalized claims for Medicare fee-for-service beneficiaries’ inpatient stays in acute care hospitals, SNFs, and IRFs. Beneficiary Summary files contain information on individuals’ sociodemographic characteristics, monthly enrollment (i.e., fee-for-service or Medicare Advantage), and mortality. The Home Health claims files include claims for home health services. We linked the files using unique, encrypted beneficiary identification numbers. We obtained the Medicare files after establishing a Data Use Agreement with the Centers for Medicare and Medicaid Services (CMS). The study was approved by our University Institutional Review Board.
Patient Population
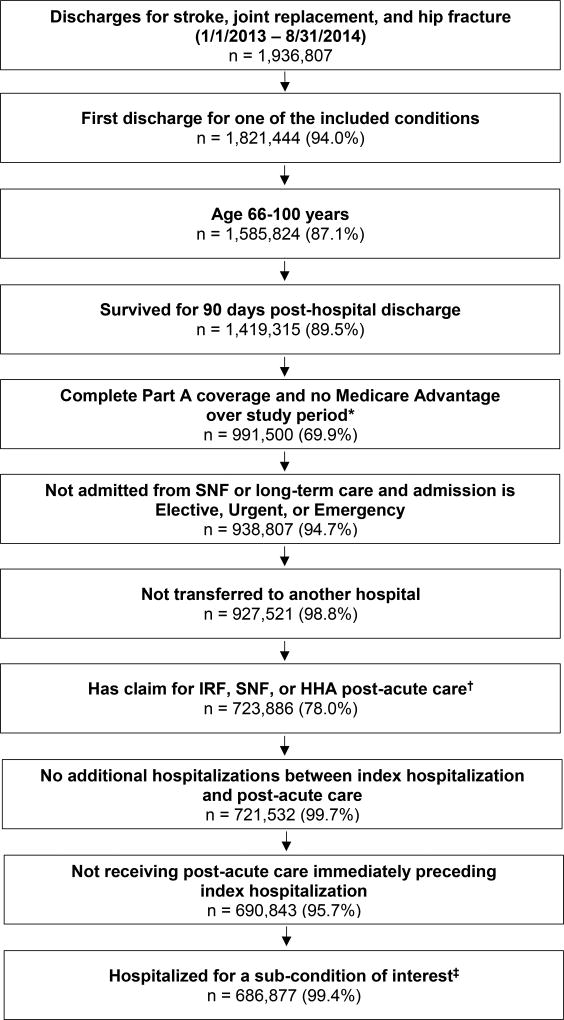
Cohort selection is presented in Figure 1. We used MedPAR files to identify patients hospitalized for stroke (Medicare Severity Diagnosis Related Groups (MS-DRGs) 61–66), joint replacement (MS-DRGs 469, 470), or hip fracture (MS-DRGs 480, 481, 482) from 1/1/2013 to 8/31/2014 (N=1,936,807).4, 9 If patients were hospitalized multiple times for the same condition over the study period, we used their first discharge, which we defined as their index hospitalization. We stratified discharges into sub-conditions of interest. Discharges for stroke were categorized as hemorrhagic or ischemic stroke; joint replacements were categorized as elective hip replacement, non-elective hip replacement, or knee replacement;15 and hip fractures were categorized as femur neck fracture, femur fracture, or hip/femur procedure with complication. ICD-9 diagnostic and procedure codes for the sub-conditions are included in Appendix 1.
Figure 1.
Flow chart presenting number of eligible cases remaining at each step during cohort selection. Values in parentheses are the percentage of the previous step remaining. Abbreviations: SNF, skilled nursing facility; IRF, inpatient rehabilitation facility; HHA, home health agency.
* ‘Study period’ refers to the one-year prior to the index hospitalization through the 90 days post-discharge for each index hospitalization.
† Has a claim for IRF services starting within 3 days of index hospitalization discharge, a SNF claim starting within 8 days, or a HHA claim starting within 10 days.
‡ Sub-conditions of interest for stroke were hemorrhagic and ischemic strokes; for joint replacements were elective hip, non-elective hip, and knee replacements; and for hip fractures were femur neck fractures, femur fractures, and hip/femur procedures with complication.
Individuals under 66 years of age were excluded from analyses to ensure we had a full year of Medicare claims for a one-year look-back for comorbidities and prior hospitalizations. Similarly, the cohort was restricted to those who had complete Part A coverage and were not in Medicare Advantage at any point during the year prior to hospitalization or the 90 days following discharge. We excluded individuals who did not survive for 90 days following hospital discharge and those transferred to another hospital at discharge. We also excluded patients admitted to the hospital from long-term care nursing homes, as these individuals represent a distinct patient population. Nursing home residents typically return to long-term care and experience different care trajectories with significantly higher readmission rates than community-dwelling older adults.16–18 Additionally, we excluded individuals admitted to the hospital from post-acute care settings because these patients were involved in ongoing episodes of care, rather than starting episodes of care.
We were interested in patients receiving post-acute care following hospitalization, so we excluded those who did not have a claim for IRF services starting within 3 days of index hospitalization discharge, a SNF claim starting within 8 days, or a HHA claim starting within 10 days. The designated time frames were based on the specified admission assessment windows in the three settings.19, 20 Patients who had a post-acute claim starting within the designated time frame, but had an intervening hospital stay (i.e., between index hospitalization and post-acute care) were also excluded. We did not include patients discharged to long-term acute care hospitals in the analyses. These patients make up less than 1% of the post-acute population21 and often have different diagnostic conditions and higher levels of severity than patients referred to SNF, IRF or HHA services.5 We used claims in MedPAR files to verify post-acute care in IRFs and SNFs, and in Home Health claims files to verify post-acute services through HHAs. The final cohort included 686,877 Medicare beneficiaries (Figure 1).
Hospital Readmissions
The outcome was unplanned readmissions within 90 days of hospital discharge. To identify readmissions, we used the specifications from the 30-day unplanned hospital readmission measure endorsed by the National Quality Forum,22 but extended the observation window from 30 to 90 days. Readmissions were considered a dichotomous outcome (yes/no). For patients with multiple unplanned readmissions over the 90-day observation window, the timing of the first readmission was used in calculating 90-day rates and in plotting time to event analyses (see Data Analysis below).
We extracted information on patients’ age, sex, race/ethnicity (Non-Hispanic White, Non-Hispanic Black, Hispanic, Other), disability entitlement (disability as the original reason for Medicare entitlement, yes/no), and dual eligibility (eligible for Medicare and Medicaid, yes/no) from the Beneficiary Summary files. We used MedPAR hospital claims over the year prior to index hospitalization to determine number of stays (count). Claims for the index hospitalization were used to determine length of stay (days) and intensive care or critical care unit utilization (days). We estimated CMS hierarchical condition categories (HCC) risk scores from the secondary diagnoses of the index hospitalization claim and patients’ sociodemographic information (age, sex, disability entitlement, and dual eligibility).23 The CMS-HCC risk adjustment models are used in the Medicare Advantage plans to predict a patient’s relative risk of future health care expenditures.24
Data Analysis
We calculated summary statistics for patients discharged to each post-acute care setting stratified by sub-conditions. We then calculated observed 30- and 90-day readmission rates for each post-acute care setting stratified by sub-conditions. We also performed time to event analyses using product limit estimators and generated plots of unplanned readmission rates over 90-day episodes of care for each post-acute care/sub-condition combination. To address our secondary objective, we used log-rank tests to determine if there were differences in 30- and 90-day readmission rates between sub-conditions. Lastly, we used Cox Proportional Hazard models to examine changes in the magnitude of the differences in readmission rates between sub-conditions over time. Analyses were performed using SAS version 9.4 (Cary, NC).
RESULTS
Cohort Characteristics
The cohort included 127,680 individuals hospitalized for stroke, 442,195 individuals hospitalized for joint replacement, and 117,002 individuals hospitalized for hip/femur fracture. Distributions across sub-conditions within the post-acute care discharge settings are presented in Table 1. Patient characteristics stratified by post-acute discharge settings and sub-conditions are presented in Appendix 2.
Table 1.
30- and 90-day unplanned hospital readmission rates by post-acute discharge setting for patients with stroke, lower extremity joint replacement, and hip facture
| Discharge location |
Condition | Sub-Condition | N | Readmission, % | |
|---|---|---|---|---|---|
| 30-day | 90-day | ||||
| HHA | Stroke | Hemorrhagic | 2,628 | 11.4 | 19.6 |
| Ischemic | 27,628 | 8.8 | 18.2 | ||
|
| |||||
| Joint replacement | Hip, elective | 58,659 | 3.3 | 5.4 | |
| Hip, non-elective | 5,434 | 6.7 | 11.7 | ||
| Knee | 124,890 | 3.1 | 5.0 | ||
|
| |||||
| Hip fracture | Femur neck | 6,825 | 5.7 | 11.6 | |
| Femur | 966 | 5.8 | 13.4 | ||
| Complications* | 471 | 6.2 | 13.2 | ||
|
| |||||
| IRF | Stroke | Hemorrhagic | 5,704 | 12.6 | 23.4 |
| Ischemic | 45,386 | 10.2 | 21.4 | ||
|
| |||||
| Joint replacement | Hip, elective | 9,648 | 6.4 | 10.6 | |
| Hip, non-elective | 16,506 | 9.3 | 18.0 | ||
| Knee | 18,671 | 6.0 | 10.1 | ||
|
| |||||
| Hip fracture | Femur neck | 23,168 | 8.1 | 16.6 | |
| Femur | 2,499 | 6.6 | 15.2 | ||
| Complications* | 420 | 8.3 | 16.4 | ||
|
| |||||
| SNF | Stroke | Hemorrhagic | 5,439 | 14.4 | 26.1 |
| Ischemic | 40,895 | 11.5 | 23.8 | ||
|
| |||||
| Joint replacement | Hip, elective | 50,108 | 5.9 | 9.7 | |
| Hip, non-elective | 46,837 | 10.1 | 19.4 | ||
| Knee | 111,442 | 5.2 | 8.7 | ||
|
| |||||
| Hip fracture | Femur neck | 71,535 | 9.3 | 18.7 | |
| Femur | 9,312 | 9.2 | 18.2 | ||
| Complications* | 1,806 | 9.8 | 18.7 | ||
Abbreviations: HHA, home health agency; IRF, inpatient rehabilitation facility; SNF, skilled nursing facility.
The “Complications” sub-condition includes patients undergoing hip/femur fracture procedures with complications
Hospital Readmissions
Condition-specific 30- and 90-day readmission rates by post-acute discharge setting are presented in Table 1. For patients with stroke, 30-day readmission rates ranged from 8.8% in HHAs (ischemic) to 14.4% in SNFs (hemorrhagic) and 90-day rates ranged from 18.2% in HHAs (ischemic) to 26.1% in SNFs (hemorrhagic). For patients with lower extremity joint replacement, 30-day readmission rates ranged from 3.1% in HHAs (knee) to 10.1% in SNFs (non-elective hip) and 90-day rates from 5.0% in HHAs, (knee) to 19.4% in SNFs, (non-elective hip). For patients with hip/femur fracture, 30-day readmission rates ranged from 5.7% in HHAs (femur neck) to 9.8% in SNFs (hip/femur procedure with complications) and 90-day rates ranged from 11.6% in HHAs (femur neck) to 18.7% in SNFs (femur neck and hip/femur procedure with complications).
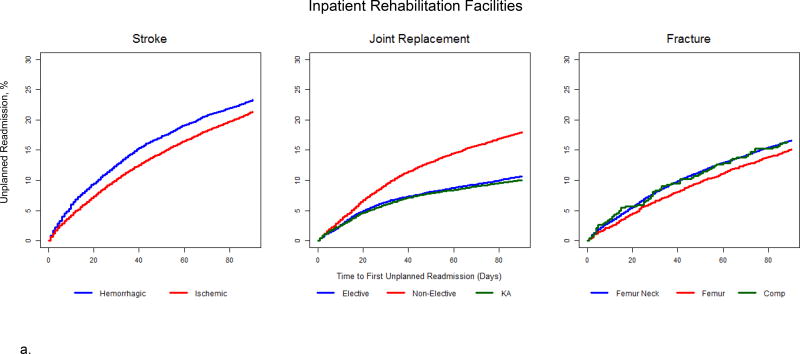
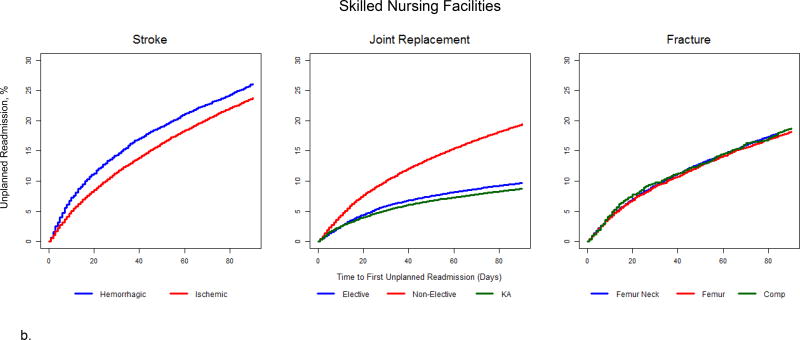
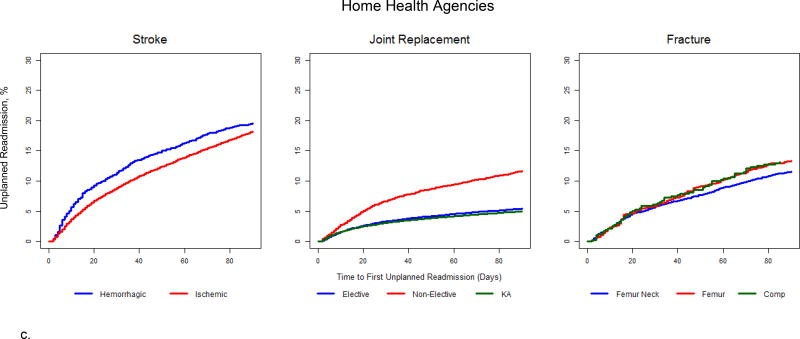
Patterns of readmission rates over time were consistent across post-acute discharge settings (Table 1 and Figure 2). Among patients with stroke, those who experienced a hemorrhagic stroke had higher 30- and 90-day readmission rates than those who had an ischemic stroke. Among patients with lower extremity joint replacement, those undergoing non-elective hip replacements had higher 30- and 90-day readmission rates than those undergoing elective procedures (hip or knee replacement). Among patients with hip/femur fractures, readmission rates at 30 and 90 days were similar across the sub-conditions.
Figure 2.
Unadjusted unplanned readmission rates over 90-day episodes of care for patients discharged to post-acute care (a. Inpatient Rehabilitation Facilities, b. Skilled Nursing Facilities, c. Home Health Agencies) following hospitalization for stroke, lower extremity joint replacement, or hip or femur fracture. Labels: Elective, elective hip replacement; Non-elective, non-elective hip replacement; KA, knee arthroplasty; Comp, hip fracture with complications.
a. Patients discharged to Inpatient Rehabilitation Facilities. *Log rank tests for 30- and 90-day unplanned readmissions were 33.16 (p<0.0001) and 15.58 (p<0.0001) for stroke, 153.19 (p<0.0001) and 543.87 (p<0.0001) for joint replacement, and 6.51 (p=0.0387) and 3.94 (p=0.1396) for fracture.
b. Patients discharged to Skilled Nursing Facilities. *Log rank tests for 30- and 90-day unplanned readmissions were 40.01 (p<0.0001) and 18.06 (p<0.0001) for stroke, 1367.07 (p<0.0001) and 3959.17 (p<0.0001) for joint replacement, and 0.62 (p=0.7331) and 1.38 (p=0.5017) for fracture, respectively.
c. Patients discharged with Home Health Agency services. *Log rank tests for 30- and 90-day unplanned readmissions were 19.91 (p<0.0001) and 4.44 (p=0.0350) for stroke, 217.50 (p<0.0001) and 476.52 (p<0.0001) for joint replacement, and 0.14 (p=0.9335) and 3.12 (p=0.2102) for fracture, respectively.
The magnitude of the differences in readmission rates between sub-conditions decreased from 30 to 90 days for patients with stroke (p<0.0001) and increased for patients with lower extremity joint replacement (p<0.0001). No differences were observed from 30 to 90 days among hip fracture sub-conditions. These patterns were observed for all three post-acute discharge settings. At 30 days, the readmission rates for patients with hemorrhagic stroke were 2.4% (IRF), 2.6% (HHA), and 2.9% (SNF) higher than the readmission rates for patients with ischemic stroke. At 90 days, the differences were reduced to 2.0% (IRF), 1.4% (HHA), and 2.3% (SNF). At 30 days, the readmission rates for patients undergoing non-elective hip replacement procedures were 3.3% (IRF), 3.6% (HHA), and 4.9% (SNF) higher than the readmission rates for patients undergoing knee replacement procedures. At 90 days, the magnitude of the differences had increased to 7.9% (IRF), 6.7% (HHA), and 10.7% (SNF). No differences in readmission rates were observed from 30 to 90 days between elective hip and knee procedures.
DISCUSSION
We present patterns in unplanned readmission rates over 90-day episodes of care for patients with stroke and lower extremity orthopedic conditions who received post-acute care in 2013–2014. This information is relevant to the pending changes in service delivery and payment models.5, 25 CMS is testing 90-day episode-based payment models for joint replacement and hip fracture.4 Additionally joint replacement, hip fracture and stroke are conditions included in the CMS Bundled Payments for Care Improvement initiative, a voluntary episode-based payment program.9 Our findings can serve as a baseline for examining readmissions over 90-day episodes that include post-acute care. Monitoring changes as reforms are implemented is an important area for future research.
We stratified readmission rates by sub-condition and initial post-acute setting. This builds on previous work and provides additional insight. Ninety-day readmission rates of 6% among patients undergoing knee replacement procedures,26 7% among patients undergoing hip replacement,27 and 26% among patients with stroke28 have been reported. Our findings provide a more in-depth look and demonstrate that rates vary within each condition category across sub-conditions and post-acute settings. This information allows for more targeted readmission prevention strategies.
We observed clear patterns in readmissions over 90 days across discharge settings. Patients with hemorrhagic stroke had higher readmission rates than those with ischemic stroke at all time points, and patients undergoing non-elective lower extremity joint replacement procedures had higher rates than those undergoing elective procedures.
The differences in readmission rates between sub-conditions decreased over time post-discharge for patients with stroke and increased for patients with joint replacement. This has implications for episode-based care delivery. For patients with stroke, efforts to prevent readmissions may be especially beneficial for patients with hemorrhagic stroke over the first 30 days after hospital discharge, but later in the episode it will be equally important to target patients with ischemic stroke. For patients receiving non-elective joint replacements our results indicate that readmission prevention efforts should start immediately after discharge and continue, or even increase, over the course of the episode of care. For patients with hip or femur fracture, readmission rates were similar across sub-conditions at all time points, implying no difference in risk over time. The strength of the sub-condition patterns we observed is supported by the consistency across post-acute SNF, IRF, and HHA discharge settings.
Our findings suggest that interventions to reduce readmission rates over 90 day episodes of care may need to be targeted to specific patient populations and post-acute settings. These interventions may also need to extend beyond the window immediately surrounding hospital discharge. Current prevention strategies primarily focus on the discharge process and follow-up within the first 14 days;29–31 however, positive outcomes have been observed with programs extending 30 or more days post-hospital discharge,32, 33 as well as with interventions targeting post-acute care discharge.34 Timing, duration, and delivery of readmission reduction programs in the context of episode-based payments will be a priority area for future research.
Strengths of our study are that we examined readmissions over extended episodes of care in a national cohort stratified by post-acute discharge setting and diagnostic impairment group. We also studied unplanned readmissions as defined by CMS.22 Prior research on readmissions has usually focused on overall or condition-specific all cause readmission and often excluded patients discharged to post-acute care.35–39
Limitations
Limitations associated with our study include the following. The completeness and coding accuracy of administrative and billing data cannot be consistently verified. Our analyses are restricted to the patient characteristics available in the claims files, and information regarding the severity of primary and comorbid conditions is limited. Social determinants such as education, financial status and social support are not directly measured in the Medicare files and this may affect readmission risk. We used Medicare fee-for-service files to identify our cohorts. We did not have access to information for persons enrolled in Medicare supplemental or Medicare Advantage plans. We included only patients who were discharged from acute hospitals to post-acute settings from specific impairment groups. Our findings do not apply to the larger Medicare population or to persons with conditions not represented in our sample. We did not risk adjust our analyses. Risk adjustment to determine readmission benchmarks or to make comparisons among facilities was not consistent with the purpose of our study. The absence of risk adjustment means that it is not appropriate to compare outcomes across the different post-acute care settings. Observed (unadjusted) rates also play a valuable role in informing care delivery. These are the actual rates of patients experiencing an undesirable outcome and, from the provider and payer perspectives, represent resource utilization over episodes of care. We believe this is important information given the pending changes in service delivery and payment models.5, 25 Finally, while the future status of broad Affordable Care Act objectives and programs is uncertain, considerable momentum and support have developed for changes that appear to be improving patient outcomes and reducing costs.1, 40
CONCLUSIONS
As we move toward the implementation of bundled payments and provider-accountability for extended episodes of care, it is important to understand how clinical and patient-centered quality measures perform for specific patient populations. We observed clear condition-specific patterns in 90-day readmissions across post-acute discharge settings. Differences in readmission rates between stroke types decreased over time, differences in readmission rates between joint replacement groups increased over time, and no meaningful differences in readmission rates between hip fracture groups were noted over time. This information may be useful in targeting interventions as health systems, providers, patients, and caregivers adapt to the new episode-based healthcare delivery and payment models.
Supplementary Material
Acknowledgments
The study was supported by the National Institutes of Health (R01AG33134; K05CA134923; R01HD069443; K12HD055929; K01HD086290; U54GM104941; P2CHD065702, and P30AG024832); the Agency for Healthcare Research and Quality (R24HS22134); and the Foundation for Physical Therapy's Center of Excellence in Physical Therapy Health Services and Health Policy Research and Training Grant.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no conflicts of interest to report.
References
- 1.Burwell SM. Setting value-based payment goals--HHS efforts to improve U.S. health care. N Engl J Med. 2015;372(10):897–899. doi: 10.1056/NEJMp1500445. [DOI] [PubMed] [Google Scholar]
- 2.The Lewin Group. [Accessed July 5, 2017];CMS Bundled Payments for Care Improvement (BPCI) Initiative Models 2–4: Year 1 Evaluation & Monitoring Annual Report. https://innovation.cms.gov/Files/reports/BPCI-EvalRpt1.pdf.
- 3.Department of Health and Human Services. [Accessed July 5, 2017];Centers for Medicare & Medicaid Services. Federal Register. Medicare Program; Comprehensive Care for Joint Replacement Payment Model for Acute Care Hospitals Furnishing Lower Extremity Joint Replacement Services; Final Rule. https://www.gpo.gov/fdsys/pkg/FR-2015-11-24/pdf/2015-29438.pdf. [PubMed]
- 4.Department of Health and Human Services. [Accessed December 16, 2017];Federal Register. Medicare Program; Advancing Care Coordination Through Episode Payment Models (EPMs); Cardiac Rehabilitation Incentive Payment Model; and Changes to the Comprehensive Care for Joint Replacement Model (CJR); Proposed Rule. https://www.gpo.gov/fdsys/pkg/FR-2016-08-02/pdf/2016-17733.pdf. [PubMed]
- 5.Medicare Payment Advisory Commission. [Accessed July 20, 2016];A Data Book: Health Care Spending and the Medicare Program. 2016 Jun; http://medpac.gov/documents/data-book/june-2016-data-book-health-care-spending-and-the-medicare-program.pdf?sfvrsn=0.
- 6.Krumholz HM, Nuti SV, Downing NS, et al. Mortality, Hospitalizations, and Expenditures for the Medicare Population Aged 65 Years or Older, 1999-2013. JAMA. 2015;314(4):355–365. doi: 10.1001/jama.2015.8035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mallinson T, Deutsch A, Bateman J, et al. Comparison of discharge functional status after rehabilitation in skilled nursing, home health, and medical rehabilitation settings for patients after hip fracture repair. Arch Phys Med Rehabil. 2014;95(2):209–217. doi: 10.1016/j.apmr.2013.05.031. [DOI] [PubMed] [Google Scholar]
- 8.Dejong G. Are we asking the right question about postacute settings of care? Arch Phys Med Rehabil. 2014;95(2):218–221. doi: 10.1016/j.apmr.2013.10.014. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Medicare & Medicaid Services. [Accessed March 15, 2017];Bundled Payments for Care Improvement (BPCI) Initiative: General Information. https://innovation.cms.gov/initiatives/bundled-payments/
- 10.Medicare Payment Advisory Commission. [Accessed July 1, 2017];Report to the Congress: Medicare and Health Care Delivery Systems. 2017 Jun; Available at: http://www.medpac.gov/docs/default-source/reports/jun17_reporttocongress_sec.pdf.
- 11.Kaye KS, Marchaim D, Chen TY, et al. Effect of nosocomial bloodstream infections on mortality, length of stay, and hospital costs in older adults. J Am Geriatr Soc. 2014;62(2):306–311. doi: 10.1111/jgs.12634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Engbers MJ, Blom JW, Cushman M, et al. The contribution of immobility risk factors to the incidence of venous thrombosis in an older population. J Thromb Haemost. 2014;12(3):290–296. doi: 10.1111/jth.12480. [DOI] [PubMed] [Google Scholar]
- 13.Covinsky KE, Palmer RM, Fortinsky RH, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc. 2003;51(4):451–458. doi: 10.1046/j.1532-5415.2003.51152.x. [DOI] [PubMed] [Google Scholar]
- 14.Lum HD, Studenski SA, Degenholtz HB, et al. Early hospital readmission is a predictor of one-year mortality in community-dwelling older Medicare beneficiaries. J Gen Intern Med. 2012;27(11):1467–1474. doi: 10.1007/s11606-012-2116-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation. [Accessed July 18, 2017];Procedure-Specific Readmission Measure Updates and Specifications Report, Hospital-Level 30-day Risk Standardized Readmission Measures, Elective Primary Total Hip Arthroplasty (THA) and/or Total Knee Arthroplasty (TKA)-Version 5.0. 2016 https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html.
- 16.Bogaisky M, Dezieck L. Early hospital readmission of nursing home residents and community-dwelling elderly adults discharged from the geriatrics service of an urban teaching hospital: patterns and risk factors. J Am Geriatr Soc. 2015;63(3):548–552. doi: 10.1111/jgs.13317. [DOI] [PubMed] [Google Scholar]
- 17.Li S, Middleton A, Ottenbacher KJ, et al. Trajectories Over the First Year of Long-Term Care Nursing Home Residence. J Am Med Dir Assoc. 2017 doi: 10.1016/j.jamda.2017.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chan TC, Hung IF, Cheng VC, et al. Is nursing home residence an independent predictor of recurrent hospitalization in older adults? J Am Med Dir Assoc. 2013;14(9):706–707. doi: 10.1016/j.jamda.2013.05.008. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Medicare & Medicaid Services. [Accessed June 16, 2016];The Inpatient Rehabilitation Facility-Patient Assessment Instrument (IRF-PAI) Training Manual. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/InpatientRehabFacPPS/IRFPAI.html.
- 20.Centers for Medicare & Medicaid Services. [Accessed August 8, 2017];Long-Term Care Facility Resident Assessment Instrument 3.0 User's Manual. Version 1.13. 2015 Oct; https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Downloads/MDS-30-RAI-Manual-V113.pdf.
- 21.Medicare Payment Advisory Commission (MedPAC) [Accessed July 3, 2017];Medicare post-acute care reforms. 2016 Apr; http://medpac.gov/docs/default-source/congressional-testimony/testimonymedicare-post-acute-care-reforms-energy-and-commerce-.pdf?sfvrsn=0.
- 22.Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation. [Accessed August 10, 2017];All-Cause Hospital-wide Measure Updates and Specifications Report: Hospital-level 30-day Risk-standardized Readmission Measure. Version 5.0. 2016 https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html.
- 23.Centers for Medicare & Medicaid Services. [Accessed November 11, 2015];Model Software/ICD-9-CM Mappings. Version 22 CMS-HCC Risk-Adjustment Model. 2014 https://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/Risk-Adjustors.html.
- 24.Pope GC, Kautter J, Ingber MJ, et al. [Accessed December 19, 2016];Evaluation of the CMS-HCC Risk Adjustment Model. Final Report. 2011 Mar; https://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/Downloads/Evaluation_Risk_Adj_Model_2011.pdf.
- 25. [Accessed September 1, 2016];Improving Medicare Post-Acute Care Transformation Act of 2014, PL 113-185. https://www.govtrack.us/congress/bills/113/hr4994.
- 26.Schairer WW, Vail TP, Bozic KJ. What are the rates and causes of hospital readmission after to1tal knee arthroplasty? Clin Orthop Relat Res. 2014;472(1):181–187. doi: 10.1007/s11999-013-3030-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schairer WW, Sing DC, Vail TP, et al. Causes and frequency of unplanned hospital readmission after total hip arthroplasty. Clin Orthop Relat Res. 2014;472(2):464–470. doi: 10.1007/s11999-013-3121-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Andrews AW, Li D, Freburger JK. Association of Rehabilitation Intensity for Stroke and Risk of Hospital Readmission. Phys Ther. 2015;95(12):1660–1667. doi: 10.2522/ptj.20140610. [DOI] [PubMed] [Google Scholar]
- 29.Condon C, Lycan S, Duncan P, et al. Reducing Readmissions After Stroke With a Structured Nurse Practitioner/Registered Nurse Transitional Stroke Program. Stroke. 2016;47(6):1599–1604. doi: 10.1161/STROKEAHA.115.012524. [DOI] [PubMed] [Google Scholar]
- 30.Nabagiez JP, Shariff MA, Khan MA, et al. Physician assistant home visit program to reduce hospital readmissions. J Thorac Cardiovasc Surg. 2013;145(1):225–231. 233. doi: 10.1016/j.jtcvs.2012.09.047. discussion 232-223. [DOI] [PubMed] [Google Scholar]
- 31.Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Courtney M, Edwards H, Chang A, et al. Fewer emergency readmissions and better quality of life for older adults at risk of hospital readmission: a randomized controlled trial to determine the effectiveness of a 24-week exercise and telephone follow-up program. J Am Geriatr Soc. 2009;57(3):395–402. doi: 10.1111/j.1532-5415.2009.02138.x. [DOI] [PubMed] [Google Scholar]
- 33.Naylor MD, Brooten D, Campbell R, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA. 1999;281(7):613–620. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- 34.Berkowitz RE, Fang Z, Helfand BK, et al. Project ReEngineered Discharge (RED) lowers hospital readmissions of patients discharged from a skilled nursing facility. J Am Med Dir Assoc. 2013;14(10):736–740. doi: 10.1016/j.jamda.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 35.Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355–363. doi: 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vahidy FS, Donnelly JP, McCullough LD, et al. Nationwide Estimates of 30-Day Readmission in Patients With Ischemic Stroke. Stroke. 2017;48(5):1386–1388. doi: 10.1161/STROKEAHA.116.016085. [DOI] [PubMed] [Google Scholar]
- 37.Kurtz SM, Lau EC, Ong KL, et al. Hospital, Patient, and Clinical Factors Influence 30- and 90-Day Readmission After Primary Total Hip Arthroplasty. J Arthroplasty. 2016;31(10):2130–2138. doi: 10.1016/j.arth.2016.03.041. [DOI] [PubMed] [Google Scholar]
- 38.Kurtz SM, Lau EC, Ong KL, et al. Which Hospital and Clinical Factors Drive 30- and 90-Day Readmission After TKA? J Arthroplasty. 2016;31(10):2099–2107. doi: 10.1016/j.arth.2016.03.045. [DOI] [PubMed] [Google Scholar]
- 39.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 40.Navathe AS, Song Z, Emanuel EJ. The Next Generation of Episode-Based Payments. JAMA. 2017;317(23):2371–2372. doi: 10.1001/jama.2017.5902. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.