Abstract
OBJECTIVES
(1) Compare family decision-makers’ perceptions of quality of communication with nursing home (NH) staff (nurses and social workers) and clinicians (physicians and other advanced practitioners) for persons with advanced dementia; (2) determine the extent to which characteristics of NH residents and family decision-makers are associated with those perceptions.
DESIGN
Secondary analysis of baseline data from a cluster randomized trial of the Goals of Care intervention.
SETTING
Twenty-two NHs in North Carolina.
PARTICIPANTS
Family decision-makers of NH residents with advanced dementia (N=302).
MEASUREMENTS
During the baseline interviews, family decision-makers rated the quality of general communication and communication specific to end-of-life care using the Quality of Communication Questionnaire (QoC). QoC item scores ranged 0 – 10, with higher scores indicating better quality of communication. Linear models were used to compare QoC by NH provider type, and to test for associations of QoC with resident and family characteristics.
RESULTS
Family decision-makers rated the QoC with NH staff higher than NH clinicians, including average overall QoC scores [5.5 (1.7) vs. 3.7 (3.0), p<0.001], general communication subscale scores [8.4 (1.7) vs. 5.6 (4.3), p<0.001], and end-of-life communication subscale scores [3.0 (2.3) vs. 2.0 (2.5), p<0.001]. Low scores reflected failure to communicate about many aspects of care, particularly end-of-life care. QoC scores were higher with later stage dementia, but were not associated with the age, gender, race, relationship to the resident, or educational attainment of family decision-makers.
CONCLUSION
Although family decision-makers for persons with advanced dementia rated quality communication with NH staff higher than that with clinicians, they reported poor quality end-of-life communication for both staff and clinicians. Clinicians simply did not perform many communication behaviors that contribute to high quality end-of-life communication. These omissions suggest opportunities to clarify and improve interdisciplinary roles in end-of-life communication for residents with advanced dementia.
Keywords: Nursing Homes, Communication, Dementia, End of Life
INTRODUCTION
Improving communication about care of older adults with advanced dementia is a high priority, especially in nursing homes (NH) where 70% of older Americans with dementia spend their final months of life.1 The final phase of dementia is marked by worsening symptom distress and frequent medical complications such as infections, injurious falls and dehydration.2 Thus, communication about goals of care and end-of-life treatment decisions is essential to promote the quality of life and quality of dying for this vulnerable population.3–6 Routine communication among family decision-makers and NH staff (nurses and social workers) and NH clinicians (physicians and other advanced practitioners) may be helpful to prepare families for end-of-life treatment decisions and to guide treatment at the time of an acute illness.7
The interdisciplinary nature of communication in NHs is a fundamental challenge to delivering effective, resident and family-centered care.8–10 Families typically interact with nurses and social workers, but rarely meet with physicians or other advanced practice clinicians who actually write orders about treatment.11–13 Prior studies suggest that NH staff and clinicians do not routinely communicate about goals of care with family decision-makers, leaving them uninformed about treatment options and unprepared for their roles as decision-makers.14–16 With the exception of the CASCADE Study, which described limited family participation in end of life conversations for residents with dementia at the end of life,2 prior studies have largely been retrospective assessments after death, rather than assessments of communication during the course of advanced dementia.
Addressing this gap in research, we conducted a secondary analysis of baseline data from the Goals of Care study, a clinical trial testing a decision aid intervention to improve goals of care communication for persons with advanced dementia.17 The purpose of this analysis was to describe current quality of communication between family decision-makers for persons with advanced dementia and NH staff and clinicians. Earlier studies suggest characteristics of residents (e.g., dementia stage) and family decision-makers (e.g., race) may influence end of life communication;18–21 thus, we examined the extent that characteristics of NH residents and decision makers were associated with their perceived quality of communication. The specific objectives were: (1) to describe family perceptions of quality of communication with NH staff and NH staff clinicians in general and specific to end-of-life care for persons with advanced dementia in NHs, and (2) to determine the extent to which the characteristics of residents and family decision-makers are associated with those perceptions.
METHODS
The original study
The original Goals of Care study was a cluster randomized trial testing whether a video decision aid and structured care planning discussion improved the quality of communication, decision-making, and palliative care for NH residents with advanced dementia.17 The study examined the impact of the Goals of Care decision aid intervention over 9 months on the primary outcome of quality of communication by NH staff, and on secondary outcomes such as palliative care domains in plans of care, completing Medical Orders for Scope of Treatment, and hospitalization. The study was conducted in 22 NHs in North Carolina. Trained research staff recruited dyads of older adults with advanced dementia and their family decision-makers between April 2012 and September 2014. Dyads were eligible if the NH resident was 65 years old or older, diagnosed with severe to very advanced dementia confirmed by primary NH nurses as stage 5–7 on the Global Deterioration Scale,22 and if the family decision-maker spoke English. All data for this analysis were collected by research staff in face-to-face interviews with the family decision-maker. Study procedures were approved by the University of North Carolina Institutional Review Board.
Data source for the secondary analysis
We used baseline data collected by in-person interviews with family decision-makers for NH residents with advanced dementia. Baseline data included demographic characteristics of family decision-makers and the resident with advanced dementia, and family decision-makers’ perceptions of the quality of communication with NH staff and with NH clinicians. Characteristics of NHs were obtained from a brief written survey completed by a member of the clinical leadership in each NH at the start of study enrollment.
Perceptions of quality of communication
Family decision-makers’ perceptions of quality of communication in general and specific to end-of-life care were measured using the previously validated Quality of Communication Questionnaire (QoC).23 This instrument measured two dimensions of the quality of communication: (1) general communication behaviors, defined as ‘how’ healthcare professionals provide support and communicate with patients and families (6 items), and (2) end-of-life communication, defined as ‘what’ professionals communicate about dying and care at the end of life (7 items).23 Each item was scored from 0 (“worst”) to 10 (“best”), and items do not specify a look-back time period. The QoC also included a response option of “didn’t do” for each item, which was scored as 0 in analysis.23 The overall QoC score and each subscale score was the sum of the item scores divided by the number of items. Because of the distinct roles in care and communication, family decision-makers were asked to give separate ratings of the quality of communication for NH staff (nurses and social workers) and NH clinicians (physicians, nurse practitioners or physician assistants).
Statistical Analyses
Descriptive statistics (e.g., means, standard deviations, frequencies) were used to summarize QoC scores and characteristics of family decision-makers. The normality assumption of the QoC scores was ensured by Shapiro’s test. Scores for individual QoC items by NH staff and clinicians were described by calculating the percentage of family caregivers who chose the “didn’t do” response for individual items. QoC scores with staff were compared to clinicians for the overall scale, and for general and end-of-life communication subscales. We tested the difference for statistical significance via a two-sided t-test for a coefficient in the linear model using an indicator variable for the role (staff and clinician) in the NH. We also used a linear model to determine the extent that quality of communication was associated with (1) age, gender, race, stage 5–7 on the Global Deterioration Scale, nursing home length of stay of NH residents and (2) characteristics of age, gender, race, relationship to the resident, or educational attainment of family decision-makers. All comparisons and associations were adjusted for the latent clustering effects of NH via adding a random intercept in the linear model. Analyses were implemented using SAS 9.3 (Cary, NC). In analyses with single comparisons, a p-value smaller than 0.05 was considered statistically significant; in analyses with multiple comparisons, to reduce the risk of Type-I errors, differences were considered statistically significant when the p-value was smaller than 0.025 (=0.05/2).
RESULTS
Sample characteristics
Family decision-makers (N=302) had an average age of 62.9 years, 67.6% were female, 86.7% were white, and 78.8% were the resident’s child or spouse of the resident’s child (Table 1). They made decisions for NH residents with an average age of 86.5 years, whose dementia severity ranged from GDS 5 (24%) to GDS 7 (26%) and average length of stay in the NH was 758.8 days. Participating NH sites had an average of 122 beds, 55% were operated for-profit, 50% had corporate (vs. private) ownership, and 73% had at least a part-time advanced practice clinician in addition to physician staffing.
Table 1.
Characteristics of Family Decision-makers and Residents (2012–2014)
| Family Decision-makers (N=302) | |
|---|---|
|
| |
| Age | 62.9 (10.6) |
|
| |
| Female gender | 204 (67.6%) |
|
| |
| Race | |
| African American | 38 (12.6%) |
| Caucasian | 261 (86.7%) |
| Other | 2 (0.7%) |
|
| |
| Relationship to patient | |
| Spouse | 40 (13.2%) |
| Son/in-law | 77 (25.5%) |
| Daughter/in-law | 161 (53.3%) |
| Other | 24 (8.0%) |
|
| |
| Education | |
| Less than high school | 3 (1.0%) |
| High school graduate | 44 (14.6%) |
| Some college/vocational school | 72 (23.9%) |
| College graduate | 102 (33.9%) |
| Advanced degree | 80 (26.6%) |
|
| |
| Residents (N=302) | |
|
| |
| Age | 86.5 (7.2) |
|
| |
| Female Gender | 246 (81.5%) |
|
| |
| Race | |
| African American | 39 (13.0%) |
| Caucasian | 257 (85.4%) |
| Other | 5 (1.6%) |
|
| |
| Dementia stage (Global Deterioration Score) | |
| 5 Moderate dementia | 74 (24.5%) |
| 6 Moderately severe dementia | 152 (50.3%) |
| 7 Severe dementia | 76 (25.2%) |
|
| |
| Nursing home length of stay | 758.8 (839.3) |
Family decision-makers’ perceptions of QoC with NH staff and clinicians
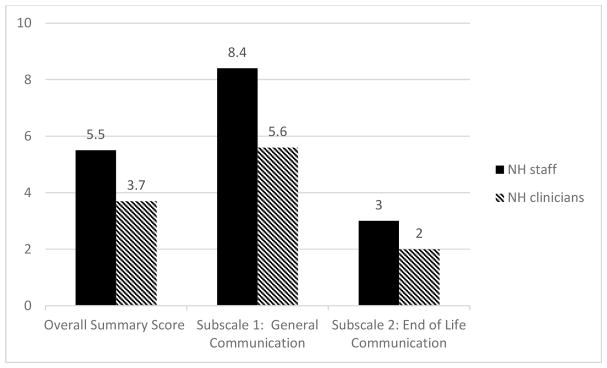
Family decision-makers rated the QoC with NH staff higher than NH clinicians, including overall QoC scores [5.5 (1.7) vs. 3.7 (3.0), p<0.001], general communication subscale scores [8.4 (1.7) vs. 5.6 (4.3), p<0.001], end of life communication subscale scores [3.0 (2.3) vs. 2.0 (2.5), p<0.001] (Figure 1). For both staff and clinicians, family decision-makers rated the quality of general communication as better than end-of-life communication.
Figure 1.
Quality of Communication with Family Decision-makers (N=302)
Communication behaviors performed by NH staff and clinicians
Family decision-maker responses to the 13 individual items in QoC Questionnaire are shown in Table 2, and demonstrate how often NH clinicians omitted specific communication behaviors. NH staff omissions of items in the general communication subscale were uncommon (0.7–3.6%). However, one third of family decision-makers indicated that NH clinicians “didn’t do this” for 5 of 6 general communication behaviors; for example, “Caring about (RESIDENT) as a person” (34.7% didn’t do) and “Giving you full attention” (33.7% didn’t do).
Table 2.
Family Decision-makers’ Report of Quality of Communication (N= 302) (2012–2014)
| Subscales and Items | Staff communication | Clinician communication | p-value | ||
|---|---|---|---|---|---|
| Mean score | Didn’t do (%) | Mean score | Didn’t do (%) | ||
| Overall Quality of Communication score (0–10) | 5.5 | - | 3.7 | - | <0.001 |
| General Communication Subscale score (0–10)a | 8.4 | - | 5.6 | - | <0.001 |
| Using words you understand | 2 (0.7%) | 101 (33.8%) | |||
| Looking you in the eye | 6 (2.0%) | 126 (42.1%) | |||
| Answering all questions about (RESIDENT’s) illness | 11 (3.6%) | 99 (33.1%) | |||
| Listening to what you have to say | 4 (1.3%) | 101 (33.9%) | |||
| Caring about (RESIDENT) as a person | 2 (0.7%) | 105 (35.2%) | |||
| Giving you his or her full attention | 5 (1.7%) | 102 (34.1%) | |||
| End of Life Communication Subscale score (0–10) | 3.0 | - | 2.0 | - | <0.001 |
| Discussing your feelings about (RESIDENT) getting sicker | 175 (58.1%) | 209 (69.9%) | |||
| Talking to you about the details concerning the possibility that RESIDENT might get sicker | 190 (63.1%) | 216 (72.2%) | |||
| Talking to you about how long (RESDIENT) might live. | 270 (89.7%) | 251 (84.0%) | |||
| Talking about what (RESIDENT’S) dying might be like. | 278 (92.4%) | 267 (89.3%) | |||
| Involving you in the decisions about the treatments that (RESIDENT) would want. | 81 (26.9%) | 151 (50.5%) | |||
| Asking about the things in life that were important to (RESIDENT). | 104 (34.4%) | 201 (67.2%) | |||
| Asking about (RESIDENT’S) spiritual or religious beliefs. | 173 (57.3%) | 245 (81.9%) | |||
Quality of Communication Questionnaire scores and subscale scores range from 0–10, with higher scores indicating better quality communication.
Families reported that end-of-life communication behaviors were frequently omitted by both NH staff and clinicians. For six of seven items describing elements of end-of-life communication, most family decision-makers reported that NH clinicians did not do the following: “Talking about how long the (RESIDENT) has to live” (83.1% omitted) and “Talking about what dying (for RESIDENT) might be like (88.4% omitted). Similarly, at least half of decision-makers indicated NH staff “didn’t do” five of seven elements of end-of-life communication; for example, “Talking about your feelings of (RESIDENT) getting sicker” (57.9% omitted) and “Talking about details if (RESIDENT) got sicker” (62.9% omitted).
Associations between QoC and the characteristics of NH residents and family decision-makers
Family decision-maker perceptions of the overall quality of communication with NH clinicians were significantly higher for residents with Global Deterioration Scale scores of 7 vs. 5 [4.0 (2.8) vs. (3.2 (3.0), p<0.007]. No significant association was identified between QoC score with NH clinicians and other resident characteristics, including age, gender, race, Global Deterioration Scale scores of 6 vs. 5, and nursing home length of stay; moreover, no statistically significant association was identified between QoC with NH staff and NH resident characteristics. Finally, no association was identified between overall QoC scores with NH staff or NH clinicians and the characteristics of family decision-makers, including age, gender, race, educational attainment, and relationship to the resident.
DISCUSSION
Patient- and family-centered communication about care at the end-of-life improves the quality of life and quality of dying for individuals with serious illness.24–27 Therefore, achieving high quality communication between health care providers and family decision-makers is an essential element of care for NH residents with advanced dementia. As reported by 302 family decision-makers for persons with advanced dementia enrolled in the Goals of Care clinical trial, the quality of communication was poor, largely due to omission of many important elements of end-of-life communication.17 Furthermore, family decision-makers described distinctly better quality of communication with NH staff than with the NH clinicians who write most treatment orders affecting overall medical care and end-of-life care.
This study is the first to use the QoC, a valid and reliable instrument, to evaluate quality of communication in NHs. Prior studies with the instrument did not describe QoC with NH staff. However, similar to earlier studies using the QoC in hospitals and outpatient clinics,23,28,29 family decision-makers in NHs rated the quality of end-of-life communication worse than general communication. Further, the mean score of family decision-maker perceptions of QoC with NH clinicians on the end of life subscale was 2.0 (range= 0–10). This is substantially lower than subscale scores in studies conducted with hospital and clinic settings, where end of life subscale scores ranged from 5.3 – 6.0.28,29 This finding adds to other evidence of the compelling need to improve end-of-life communication in NHs; for example, the CASCADE Study of advanced dementia, which found that only 38% of family decision-makers remembered communication about residents’ treatment options at the end-of-life.2,14 Our findings suggest that both NH staff and clinicians need support and training to raise end-of-life topics, and to prepare family for their roles as decision-makers. For example, the question of when to initiate end of life conversations with family decision-makers may be complicated by clinicians’ need to establish rapport and develop trust with families before discussing at the end of life care and expectations. Indeed, our finding that QoC with NH clinicians was associated with more advanced dementia stage of NH residents suggests clinicians may not begin these conversations with families until dementia is in an advanced stage. Further, the relatively low QoC scores with the most advanced stage of dementia indicates that there is room to improve end-of-life communication even then.
Our study results have implications for the design of interventions to improve end-of-life care for dementia. Although we assessed family decision-maker perceptions of QoC with NH staff and clinicians separately, teamwork in NHs is essential for optimal resident care and dementia care. NH clinicians rely on staff to conduct most communication with families, and to create care plans for residents.30 Our results showed that family decision-makers’ ratings on quality of communication by NH clinicians were poor, largely due to lack of many elements of communication behaviors with family decision-makers. NH physicians in particular have been described as “missing in action,” and their role is structured such that they simply never have the opportunity to meet with family.31 Undefined role structure and the lack of payment incentives are partial explanations for limitations in the quality of communication observed in this study. Thus, interventions to improve end-of-life communication in this setting should consider structuring new opportunities for families and clinicians to meet and finalize treatment decisions, while providing training and support for staff who do most of this communication.
Our findings should be considered in light of several strengths and limitations. Strengths include large sample size, diverse NH settings, and prospective data collection, reflecting the family experience of communication during NH care for persons with advanced dementia. The study also is the first to use QoC Questionnaire to assess quality of communication for NH dementia care. This instrument has been previously validated and widely used in studies of intensive care communication, allowing comparisons to prior studies of communication in other populations with serious illness.23,28,29,32 The study also has several limitations. First, all study NHs were located in North Carolina, which potentially limits the generalizability of the study findings. Second, while 20% of the enrolled NH residents in the Goals of Care study died in the subsequent 9 months, NH staff and clinicians may have felt it premature to raise end-of-life concerns with some family decision-makers. Optimal timing of these discussions in dementia care is difficult, given the challenges of predicting death in this disease.33 Third, it is possible that NH staff and clinicians did provide certain information about care at the end of life but the family member did not recall or absorb the information; it is also possible that NH staff or clinicians discussed end of life care with a family member other than the one who participated in the research, although the research participant was the legally authorized surrogate; thus some gaps in communication may be attributable to causes other than staff or clinician behavior. Fourth, family decision-makers rated the quality of communication with two groups – NH staff and NH clinicians – categories that combined disciplines including staff (nurses and social workers) and clinicians (physicians and advanced practice clinicians). It is possible that important variations in communication between disciplines were not identified.
CONCLUSION/RELEVANCE
For future research, frequent omissions in communication behaviors suggest opportunities to improve the quality of communication. First, NH staff are positioned to perform many elements of general communication better than NH clinicians, and as a result family decision-makers have relatively positive experiences with general communication with staff. Because staff see decision-makers more frequently, they have opportunities to develop trusting relationships and explain daily changes in health. Thus, structural changes to facilitate communication opportunities between families and NH staff may be effective to improve family understanding of advanced dementia and daily care. Second, both NH staff and clinicians omitted key elements of end-of-life communication; thus, additional training and communication tools are needed for all members of the interdisciplinary team. In the parent study for this analysis, the Goals of Care decision aid followed by a semi-structured care plan meeting with staff was effective to improve family ratings of overall and end-of-life quality of communication with staff.17 A potentially useful implication for research is to determine complementary staff and clinician communication roles on interdisciplinary teams, which would increase the ability of NH staff and clinicians to collaborate and to stage end-of-life communication with decision-makers. For example, NH staff might focus on initial communication to assess how families understand and accept deteriorating health due to advanced dementia; then they might facilitate meetings between families and NH clinicians to promote understanding of prognosis, key decisions and treatment options. Advance care planning interventions address some of these gaps in communication;34,35 however, future studies are needed to test the efficacy of tailoring these interventions for family decision-makers facing advanced dementia care.
Acknowledgments
Funding Sources:
This work was supported by the National Institutes of Health/National Institute on Aging (R01AG037483-05). Mark Toles’ contributions were supported by the National Institutes of Health/National Center for Advancing Translational Sciences (Grant 1KL2TR001109).
Footnotes
CONFLICT OF INTEREST DISCLOSURES:
| Elements of Financial/Personal Conflicts | *MT | MKS | FCL | LCH | ||||
|---|---|---|---|---|---|---|---|---|
| Y | N | Y | N | Y | N | Y | N | |
| Employment or Affiliation | X | X | X | X | ||||
| Grants/Funds | X | X | X | X | ||||
| Honoraria | X | X | X | X | ||||
| Speaker Forum | X | X | X | X | ||||
| Consultant | X | X | X | X | ||||
| Stocks | X | X | X | X | ||||
| Royalties | X | X | X | X | ||||
| Expert Testimony | X | X | X | X | ||||
| Board Member | X | X | X | X | ||||
| Patents | X | X | X | X | ||||
| Personal Relationship | X | X | X | X | ||||
AUTHOR CONTRIBUTIONS: All persons who contributed significantly to this work are listed below.
MT - Study concept and design, analysis and interpretation of data, and preparation of manuscript.
MKS - Study concept and design, analysis and interpretation of data, and preparation of manuscript.
FCL – Analysis and interpretation of data, and preparation of manuscript.
LCH - Study concept and design, analysis and interpretation of data, and preparation of manuscript.
SPONSOR’S ROLE: The sponsor did not have a role in the design, methods, subject recruitment, data collection, analysis or preparation of manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mitchell SL, Teno JM, Miller SC, Mor V. A national study of the location of death for older persons with dementia. J Am Geriatr Soc. 2005;53(2):299–305. doi: 10.1111/j.1532-5415.2005.53118.x. [DOI] [PubMed] [Google Scholar]
- 2.Mitchell SL, Teno JM, Kiely DK, et al. The clinical course of advanced dementia. N Engl J Med. 2009;361(16):1529–1538. doi: 10.1056/NEJMoa0902234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Institute of Medicine. Dying in America: Improving quality and honoring individual preferences near the end of life. Washington, DC: The National Academies Press; 2015. [PubMed] [Google Scholar]
- 4.Kaldjian LC, Curtis AE, Shinkunas LA, Cannon KT. Goals of care toward the end of life: a structured literature review. Am J Hosp Palliat Care. 2008;25(6):501–511. doi: 10.1177/1049909108328256. [DOI] [PubMed] [Google Scholar]
- 5.Rosemond C, Hanson LC, Zimmerman S. Goals of Care or Goals of Trust? How Family Members Perceive Goals for Dying Nursing Home Residents. J Palliat Med. 2017;20(4):360–365. doi: 10.1089/jpm.2016.0271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300(14):1665–1673. doi: 10.1001/jama.300.14.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lopez RP, Mitchell SL, Givens JL. Preventing Burdensome Transitions of Nursing Home Residents with Advanced Dementia: It’s More than Advance Directives. J Palliat Med. 2017 doi: 10.1089/jpm.2017.0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson RA, Toles MP, Corazzini K, et al. Local interaction strategies and capacity for better care in nursing homes: a multiple case study. BMC Health Serv Res. 2014;14:244. doi: 10.1186/1472-6963-14-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Colon-Emeric CS, Lekan-Rutledge D, Utley-Smith Q, et al. Connection, regulation, and care plan innovation: A case study of four nursing homes. Health Care Manage Rev. 2006;31(4):337–346. doi: 10.1097/00004010-200610000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nazir A, Unroe K, Tegeler M, et al. Systematic review of interdisciplinary interventions in nursing homes. J Am Med Dir Assoc. 2013;14(7):471–478. doi: 10.1016/j.jamda.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 11.Biola H, Sloane PD, Williams CS, et al. Physician communication with family caregivers of long-term care residents at the end of life. J Am Geriatr Soc. 2007;55(6):846–856. doi: 10.1111/j.1532-5415.2007.01179.x. [DOI] [PubMed] [Google Scholar]
- 12.Jones K, Birchley G, Huxtable R, et al. End of life care: A scoping review of experiences of Advance Care Planning for people with dementia. Dementia (London, England) 2016 doi: 10.1177/1471301216676121. [DOI] [PubMed] [Google Scholar]
- 13.Towsley GL, Hirschman KB, Madden C. Conversations about End of Life: Perspectives of Nursing Home Residents, Family, and Staff. J Palliat Med. 2015;18(5):421–428. doi: 10.1089/jpm.2014.0316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Givens JL, Kiely DK, Carey K, Mitchell SL. Healthcare proxies of nursing home residents with advanced dementia: decisions they confront and their satisfaction with decision-making. J Am Geriatr Soc. 2009;57(7):1149–1155. doi: 10.1111/j.1532-5415.2009.02304.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Givens JL, Spinella S, Ankuda CK, et al. Healthcare Proxy Awareness of Suspected Infections in Nursing Home Residents with Advanced Dementia. J Am Geriatr Soc. 2015;63(6):1084–1090. doi: 10.1111/jgs.13435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Teno JM, Mitchell SL, Kuo SK, et al. Decision-making and outcomes of feeding tube insertion: a five-state study. J Am Geriatr Soc. 2011;59(5):881–886. doi: 10.1111/j.1532-5415.2011.03385.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hanson LC, Zimmerman S, Song MK, et al. Effect of the Goals of Care Intervention for Advanced Dementia: A Randomized Clinical Trial. JAMA Intern Med. 2017;177(1):24–31. doi: 10.1001/jamainternmed.2016.7031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eneanya ND, Wenger JB, Waite K, et al. Racial Disparities in End-of-Life Communication and Preferences among Chronic Kidney Disease Patients. Am J Nephrol. 2016;44(1):46–53. doi: 10.1159/000447097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sanders JJ, Robinson MT, Block SD. Factors Impacting Advance Care Planning among African Americans: Results of a Systematic Integrated Review. Journal of palliative medicine. 2016;19(2):202–227. doi: 10.1089/jpm.2015.0325. [DOI] [PubMed] [Google Scholar]
- 20.LoPresti MA, Dement F, Gold HT. End-of-Life Care for People With Cancer From Ethnic Minority Groups: A Systematic Review. Am J Hosp Palliat Care. 2016;33(3):291–305. doi: 10.1177/1049909114565658. [DOI] [PubMed] [Google Scholar]
- 21.Tjia J, Dharmawardene M, Givens JL. Advance Directives among Nursing Home Residents with Mild, Moderate, and Advanced Dementia. Journal of palliative medicine. 2018;21(1):16–21. doi: 10.1089/jpm.2016.0473. [DOI] [PubMed] [Google Scholar]
- 22.Reisberg B, Ferris SH, de Leon MJ, Crook T. The Global Deterioration Scale for assessment of primary degenerative dementia. Am J Psychiatry. 1982;139(9):1136–1139. doi: 10.1176/ajp.139.9.1136. [DOI] [PubMed] [Google Scholar]
- 23.Engelberg R, Downey L, Curtis JR. Psychometric characteristics of a quality of communication questionnaire assessing communication about end-of-life care. J Palliat Med. 2006;9(5):1086–1098. doi: 10.1089/jpm.2006.9.1086. [DOI] [PubMed] [Google Scholar]
- 24.Tulsky JA, Beach MC, Butow PN, et al. A Research Agenda for Communication Between Health Care Professionals and Patients Living With Serious Illness. JAMA Intern Med. 2017;177(9):1361–136. doi: 10.1001/jamainternmed.2017.2005. [DOI] [PubMed] [Google Scholar]
- 25.Fellowes D, Wilkinson S, Moore P. Communication skills training for health care professionals working with cancer patients, their families and/or carers. Cochrane Database of Syst Rev. 2004;(2):Cd003751. doi: 10.1002/14651858.CD003751.pub2. [DOI] [PubMed] [Google Scholar]
- 26.Rao JK, Anderson LA, Inui TS, Frankel RM. Communication interventions make a difference in conversations between physicians and patients: a systematic review of the evidence. Med Care. 2007;45(4):340–349. doi: 10.1097/01.mlr.0000254516.04961.d5. [DOI] [PubMed] [Google Scholar]
- 27.Scheunemann LP, McDevitt M, Carson SS, Hanson LC. Randomized, controlled trials of interventions to improve communication in intensive care: a systematic review. Chest. 2011;139(3):543–554. doi: 10.1378/chest.10-0595. [DOI] [PubMed] [Google Scholar]
- 28.Long AC, Engelberg RA, Downey L, et al. Race, income, and education: associations with patient and family ratings of end-of-life care and communication provided by physicians-in-training. J Palliat Med. 2014;17(4):435–447. doi: 10.1089/jpm.2013.0214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smith-Howell ER, Hickman SE, Meghani SH, et al. End-of-Life Decision Making and Communication of Bereaved Family Members of African Americans with Serious Illness. Journal of Palliat Med. 2016;19(2):174–182. doi: 10.1089/jpm.2015.0314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cagle JG, Unroe KT, Bunting M, et al. Caring for Dying Patients in the Nursing Home: Voices From Frontline Nursing Home Staff. J Pain Symptom Manage. 2017;53(2):198–207. doi: 10.1016/j.jpainsymman.2016.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shield RR, Wetle T, Teno J, et al. Physicians “missing in action”: family perspectives on physician and staffing problems in end-of-life care in the nursing home. J Am Geriatr Soc. 2005;53(10):1651–1657. doi: 10.1111/j.1532-5415.2005.53505.x. [DOI] [PubMed] [Google Scholar]
- 32.Curtis JR, Back AL, Ford DW, et al. Effect of communication skills training for residents and nurse practitioners on quality of communication with patients with serious illness: a randomized trial. JAMA. 2013;310(21):2271–2281. doi: 10.1001/jama.2013.282081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mitchell SL, Miller SC, Teno JM, et al. Prediction of 6-month survival of nursing home residents with advanced dementia using ADEPT vs hospice eligibility guidelines. JAMA. 2010;304(17):1929–1935. doi: 10.1001/jama.2010.1572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brinkman-Stoppelenburg A, Rietjens JA, van der Heide A. The effects of advance care planning on end-of-life care: a systematic review. J Palliat Med. 2014;28(8):1000–1025. doi: 10.1177/0269216314526272. [DOI] [PubMed] [Google Scholar]
- 35.Houben CHM, Spruit MA, Groenen MTJ, et al. Efficacy of advance care planning: a systematic review and meta-analysis. J Am Med Dir Assoc. 2014;15(7):477–489. doi: 10.1016/j.jamda.2014.01.008. [DOI] [PubMed] [Google Scholar]