Abstract
The physical environment affects how work is done in operating rooms (OR). The circulating nurse (CN), in particular, requires access to and interacts with materials, equipment, and technology more than other OR team members. Naturalistic study of CN behavior is therefore valuable in assessing how OR space and physical configuration influences work patterns and disruptions. This study evaluated the CNs’ work patterns and flow disruptions (FD) by analyzing 25 surgeries across three different ORs. The OR layouts were divided into transitional and functional zones, and the work of CNs was categorized into patient, equipment, material, and information tasks. The results reveal that information tasks involve less movement than other types of work, while across all ORs, CNs were more likely to be involved in layout and environmental hazard FDs when involved in patient, material, or equipment-related tasks compared to information tasks. Different CN work patterns and flow disruptions between ORs suggest a link between OR layout and a CN’s work. Future studies should examine how specific layout elements influence outcomes.
Keywords: operating room, operating room layout, spatial zones, nurse tasks, flow disruptions
1. INTRODUCTION
Operating rooms (OR) are dynamic work systems whose functioning involves complex interactions between surgical team members, patient characteristics, surgery type, tasks that need to be performed, equipment and technology used as well as the physical environment in which the work is performed. This is also a high-risk patient care environment. In industrialized countries, 3% to 16% of inpatients experience major surgical complications, with mortality between 0.4% to 0.8% (Anderson, Davis, Hanna, & Vincent, 2013). Problems with teamwork, communication, equipment design, or tasks have often been associated with these adverse outcomes (Gawande, Zinner, Studdert, & Brennan, 2003; Greenberg et al., 2007).
The study by Karsh et al. (2006) on a human factors engineering paradigm for improving patient safety suggests that in order to improve patient and staff safety in healthcare settings, there needs to be a better understanding of how the work system impacts the healthcare professional. They argue that healthcare systems which support healthcare providers’ performance and reduce hazards will result in improvements in patient safety outcomes (Karsh, Holden, Alper, & Or, 2006).
The surgical process is complex, dynamic, and requires coordination between surgical team members throughout the surgery. The circulating nurse (CN) plays a key role in anticipating and supporting the needs of other team members (Simmons, Graves, & Flynn, 2009), such as the scrub nurse, the surgeon, and the anesthesiologist (Ritchie, 2009). Also, the CN plays a key role in protecting and maintaining patient safety (Alfredsdottir & Bjornsdottir, 2007) throughout different phases of the surgery by ensuring that the surgical protocols are in place when staff is handling the surgical tools in the preparation phase and providing the necessary care in the intra-operative phase (Spry, 2009; Yang et al., 2012). Thus, the CN’s work is deeply impacted by all the components that make up the work system. The CN works outside the sterile field, acting as the link between sterile and non-sterile, supplying equipment, materials, and information to the surgeons and scrub nurse at the operating table, and accessing other resources in the surgical suite beyond the OR (Kang, Massey, & Gillespie, 2015). They require access to appropriate storage and information systems; must have space to prepare or hold information and items; must maintain sterility; and must avoid knocking or bumping into other people or equipment in the often crowded OR. Thus, the locations of equipment, materials, the OR team, and communication devices can impact the performance of the CN, especially once the operation is underway. Configuration of zones designated to perform such activities can influence the CN’s ease of access to areas they constantly travel to as well as travel distances and time spent on performing their activities.
Distraction, interruptions, and layout issues are frequent occurrences during most surgical procedures (Palmer et al., 2013). One study of cardiac operations found an average of 100 flow disruptions (FD) during a cardiac procedure (Palmer et al., 2013). In another study, Wheelock et al. (2015) found that intense equipment distractions were correlated with higher stress levels for scrub nurses. Additionally, an analysis of 731 reported medication errors in ORs showed that distractions and interruptions were associated with 48% of surgical errors (Beyea, Hicks, & Becker, 2003). These FDs can be attributed to various factors including communication breakdowns, environmental hazards, equipment malfunctions, and the layout of the OR (Palmer et al., 2013). The CN is the most ambulatory surgical team member and potentially impacted by and involved in a range of flow disruptions. However, no studies have explored how flow disruptions may impact the work of the CN.
The purpose of this study was to examine the difference in movement patterns of the CN and disruptions to the CN’s workflow while performing different types of tasks in three OR environments. This study sought to explore the locations in which work was done, the transitions required, and distances travelled between different locations, as a function of the tasks, surgery, and OR layout. This study uses the interrelationship between the factors within the work systems as the basis for the approach. This analysis was done within a systems-framework by analyzing tasks and the environment while controlling for the person-role. The tools and technology as well as the organizational factors were relatively consistent across the surgeries as they were all within the same organization with similar equipment in each OR. The research team also examined the flow disruptions experienced during these tasks; their classification; how they signified deeper systems problems; and how they related to surgeries, tasks, and OR layout. This is one of the first studies to use an evidence-based approach to explore the interaction between OR layout and task requirements.
2. METHODS
2.1. Design and Setting
Observation of the OR has been extremely valuable for understanding behavior, performance, and safety from the “work as done” perspective, revealing a range of systems-related issues with surgical delivery that were largely ignored beforehand. Observational methods are also valuable for architects to allow for an understanding of workflow in a given layout and provide insight into how work is supported or limited by the room layout design (Persson, Dalholm, & Johansson, 2014). This study used a prospective observational research design utilizing a convenience sample of pre-recorded videos from three different ORs in a major 700-bed academic hospital system in the southeast of the United States. Three ORs were selected due to the differences in their size and the type of surgeries scheduled. A convenience sample of videos was collected, in the order the surgeries were performed, based first on obtaining informed consent from all staff involved in the selected ORs, and then on the requirements for set up configuration of the video capture system. This resulted in an unequal number of surgeries from each OR and some variability in the types of surgeries observed. Video observations were chosen over direct observations so that more detailed data could be documented about the CN behavior and the specific tasks, which would not be possible if the coding was done in real time. The OR doors served as the boundary for the physical space within this analysis, which meant that the behavior of the CN when outside the OR was not included in the analysis.
OR A (690ft2/64.1m2) was located in a modern building and was used for general adult surgeries. ORs B (390ft2/32.2m2) and C (463ft2/43.0m2) were located in an older building and were primarily used for pediatric surgery. The type and duration of the surgeries included in this study are presented in Table 1. On average the surgery duration was 86.3 (SD = 52.0) minutes. Observations included 13 surgeries in OR A, four in OR C, and eight in OR B. This study was approved by the [organization’s name omitted for review] Institutional Review Board (IRB) (study ID: Pro00048787).
Table 1.
Specific surgeries included in the analysis for each OR.
| Surgery # | Surgery Duration (min) | Operating Room | Specific Surgery |
|---|---|---|---|
| 1 | 116 | A | Laparoscopic Gastric Bypass |
| 2 | 129 | A | Laparoscopic Gastric Bypass |
| 3 | 108 | A | Laparoscopic Cholecystectomy |
| 4 | 143 | A | Open Inguinal Hernia Repair |
| 5 | 72 | A | Laparoscopic Band Removal |
| 6 | 54 | A | Laparoscopic Cholecystectomy |
| 7 | 181 | A | Laparoscopic Band Removal & Lap. Gastric Bypass |
| 8 | 57 | A | Laparoscopic Cholecystectomy |
| 9 | 154 | A | Gastrostomy Tube Replacement |
| 10 | 77 | A | Laparoscopic Cholecystectomy |
| 11 | 95 | A | Laparoscopic Cholecystectomy |
| 12 | 87 | A | Esophagogastroduodenoscopy |
| 13 | 93 | A | Exploratory Laparotomy |
| 14 | 59 | C | Pediatric Esophageal Dilation |
| 15 | 64 | C | Pediatric Broviac Catheter Insertion |
| 16 | 77 | C | Pediatric Gastrocutaneous Fistula Closure |
| 17 | 244 | C | Pediatric T E Fistula Repair, Thoracic approach |
| 18 | 34 | B | Pediatric Bronchoscopy/Laryngoscopy |
| 19 | 30 | B | Pediatric Myringotomy with Tube Placement |
| 20 | 33 | B | Pediatric Laryngoscopy with Foreign Body Removal/Bronchoscopy |
| 21 | 40 | B | Pediatric Bronchoscopy/Laryngoscopy/Nasal Sinus Endoscopy |
| 22 | 70 | B | Pediatric Tonsillectomy & Pediatric Adenotonsillectomy/Bronchoscopy/Laryngoscopy |
| 23 | 70 | B | Pediatric Tonsillectomy & Adenotonsillectomy/Myringotomy with Tube Placement |
| 24 | 30 | B | Pediatric Myringotomy with Tube Placement |
| 25 | 42 | B | Pediatric Tonsillectomy |
2.2. Video Analysis
Video and audio recordings of surgeries were captured using a portable observation lab comprising of four video cameras deployed in the four corners of the OR and two wireless audio receivers located centrally in the OR. The video cameras were wired to a single computer and video and audio feeds were coordinated using Noldus Observer XT 12 software, allowing high resolution and simultaneous review from multiple angles. Cameras were set up on the morning of recording and monitored throughout the day of capture by a research assistant. For each surgery, the recordings were initiated before patient entry and ended after the patient exit from the OR. Each operation was given a unique identifier (see Figure 1).
Figure 1.
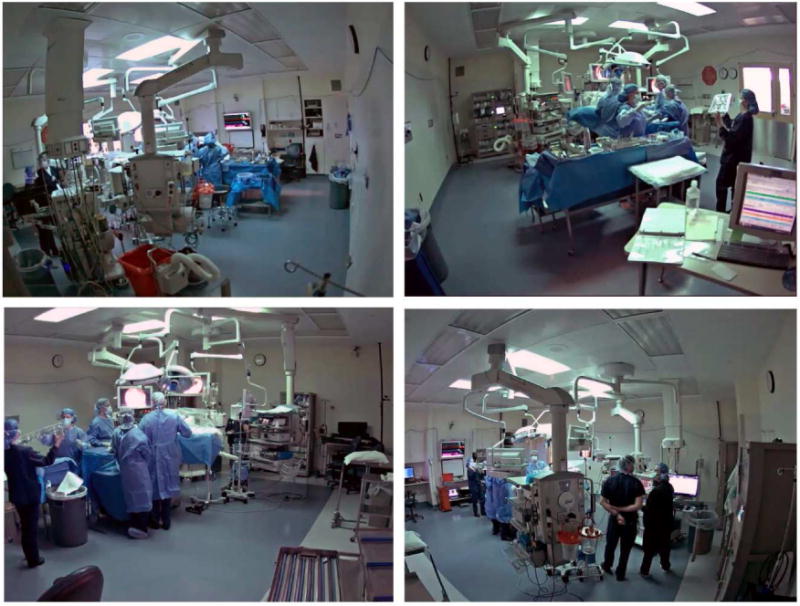
Operating room field captured by cameras in four corners of the room.
The videos were content analyzed using Noldus Observer XT 12 software, which allowed for event-based coding of the staff’s locations and activities. Two graduate students were trained to code the videos. Coding consistency was encouraged by (i) in-person observation of the surgical procedures by all coders, (ii) understanding and discussing the coding schemes, (iii) multiple pilot coding sessions to resolve any consistency issues and refinement of codes, and (iv) testing for inter-rater reliability. Clinical team members including two anesthesiologists and a nurse provided oversight for the coding process and helped to clarify any issues that came up during the coding process. To resolve any conflicts between coders, discussion sessions were held after pilot sessions to address disagreements in coding and to refine the protocol to address uncertainties that may cause inconsistency between coders. Coders were encouraged to use the playback feature of Noldus as needed to code activities correctly.
Students coded the location of the CN at all points in time during the surgery and the CN’s primary activity into one of four exclusive categories: patient tasks (P), equipment tasks (E), materials and supplies tasks (M), and information tasks (I). Together, these tasks are termed as PEMSI tasks in this study (Khoshkenar et al., 2017). All surgical team members are involved in different PEMSI tasks during the course of the surgery. For example, the CN is extensively involved in all PEMSI tasks. PEMSI categories are linked to the person (role) performing a type of activity and the objects or components of the work system that are the focus of the task. Patient-related tasks include repositioning, transferring, preparing, or anesthetizing patients. Equipment-related tasks are activities related to equipment, such as preparing, monitoring, moving, or cleaning equipment. Materials and supplies tasks are those related to material or supplies; such as using, preparing, or cleaning instruments; gowning; trash disposal; or retrieving supplies from nurse PYXIS station. Information-related tasks refer to activities, such as phone calls, pagers, texts, equipment or instrument handoff, computer work, or paperwork. The subcategories of PEMSI activities were developed succinctly to avoid any overlap of activities and enabling coders to code for only one activity at a time. The number of tasks performed in each zone and the number of zones traveled by the CN while performing a task were both obtained by transforming the coded data.
The quantitative exploration of small deviations from optimal work patterns variously described as glitches (Morgan et al., 2013), non-routine events (Weinger, Slagle, Jain, & Ordonez, 2003), or FD provides an opportunity to evaluate and improve system function (Morgan et al., 2014), reduce errors (Wiegmann, ElBardissi, Dearani, Daly, & Sundt, 2007), and potentially improve outcomes (Catchpole et al., 2014; de Leval, Carthey, Wright, Farewell, & Reason, 2000). FDs, defined as “events that disrupt the natural progression of the task” (Wiegmann et al., 2007), were classified by a third video observer according to an existing classification framework (Palmer et al., 2013). Only the specific FDs that involved the CN were extracted and analyzed at the CN task level. From these data, FDs related to OR layout and environmental hazards were then extracted for additional analysis. Layout FDs were defined as incidents due to connector, equipment, furniture, or fixed structure positioning; inadequate use of space; and impeded visibility. Environmental hazard FDs were defined as incidents where surgical staff are involved with the environment, such as slipping, falling, tripping; interaction with sharp objects and contaminated needles; collision between staff and objects; and excessive reach for accessing patient, objects, or equipment.
The OR layout was divided into zones based on a framework developed by Ahmad et al. (2016) and adapted for this study through 12 preparatory direct observations prior to video data collection. Consensus within the interdisciplinary research team (which included anesthesiologists, nurses, healthcare administrators, human factors engineers, operations managers, and architects) yielded 20 zones. The zones were classified as either transitional (primarily meant for circulation between different parts of the OR) or functional (reflecting specific functions). Functional zone categories included support, supply, door, surgical, and workstation zones. Figure 2 shows the layout of three ORs under study with the designated zones.
Figure 2.

Floor plans of the three operating rooms with assigned zones, Operating Room A (top), Operating room B (middle), and Operating Room C (bottom).
The event-based data extracted from Observer XT 12 were converted into time-based data with the unit of time as seconds, which enabled exploration of frequency and duration of all events and subjects as well as simultaneous comparison of events and activities across the OR. The observers derived measures for each task within each surgery and each OR. The measures were (i) the total number of zones (functional + transitional) travelled through, (ii) the number of transitional zones travelled through, (iii) the total number of FDs occurring, and (iv) the occurrence of environmental hazard and layout-related FDs.
Since it was impractical to capture distances travelled by the CN from the videos, these were estimated using computer-based simulation software called AnyLogic. A model representation of each OR was developed and appropriately scaled to enable the tracking of distance. Staff and equipment would move from one zone to another based on the coded time-based data. Their actual positions within a zone would depend on the available space within that zone at the time the staff or equipment arrived. The model also accounted for path obstructions (of both static and dynamic objects), which allowed a reasonable estimate of the distance travelled to be calculated for each task. For statistical analysis, the distances traveled were then segmented into three categories: no movement, movements less than 10 meters (<10), and movements greater than 10 meters (≥10).
2.3. Statistical Analysis
A set of logistic regressions, including quasi-Poisson regressions, was performed with explanatory variables representing the tasks, the OR, and a covariate for each specific surgery. Stepwise deletion of insignificant variables, in addition to the model deviance, was used to identify the best-fit models. For basic movement around the OR, quasi-Poisson regression models with a log link function and the log of the duration of each task as the offset variable were used to predict the number of all zones and number of transitional zones through which the CN traveled during each task. A quasi-Poisson regression was used, as the variance and the mean of the dependent variables were not equal. For distance travelled, an ordered logistic regression model was used to predict the likelihood of the CNs traveling longer distances during the tasks with two outliers removed from the analysis at the task level. Logistic regression models were also used to predict the occurrences of a CN-involved FD during each of the CN’s tasks across all surgeries. Additionally, task duration was used as an offset to account for the differences in event durations and thus created models that were able to predict event rates per unit time. All data reduction and analyses were conducted in R version 3.3.2 using the GLM function.
3. RESULTS
A convenience sample of 25 surgeries was recorded in the three ORs (13 in OR A, 4 in OR B, and 8 in OR C), yielding 37 hours of observations. Across all surgeries, the CN spent 34 hours performing 1,471 tasks of which 9% (n= 131) were patient related; 23% (n= 341) were equipment related; 33% (n= 482) were material, instruments, and supplies related; and 35% (n= 517) were information related. In terms of time spent on all activities, patient-related tasks accounted for 12% of total activity time (4 hours), equipment and materials-related tasks accounted for 18% (6 hours), and information-related tasks accounted for 53% (18 hours). About 91% of the CN’s activities required traveling through multiple zones within the ORs. On average, each single-zone activity took 35 seconds (95% CI: 28.34, 41.70) to complete, whereas each multiple-zone activity took about 53 seconds (95% CI: 50.52, 55.74).
3.1. Movement within the operating room
Within a single task, on average, the CN travelled through 5.16 (95% CI: 4.93, 5.39) zones. More specifically, during patient-related tasks the CN traveled an average of 5.61 (95% CI: 4.84, 6.38) zones per task. Equipment tasks required movement across an average of 5.40 (95% CI: 4.90, 5.91) zones per task. Materials and supplies tasks required movement across an average of 5.87 (95% CI: 5.44, 6.30) zones per task. Information-related tasks were associated with an average of 4.10 (95% CI: 3.81, 4.40) zones per task. Tasks with no movement accounted for 15% of tasks, 56% of tasks required movement of up to 10 meters, and 29% of tasks required movement of more than 10 meters.
The total number of zones (transitional + functional) that the CN travelled through were explored by OR and task with covariates representing each specific surgery. The quasi-Poisson regression model (Table 2) revealed significant differences between the ORs and tasks, with some surgeries identified as being significantly different from the rest of the surgery sample. CNs in OR C traveled through 19% (exp(0.18)=1.19, 95% CI: 1.06, 1.34) more zones than in OR B or OR A. When the CN was engaged in patient tasks, they traveled through 55% (95%CI: 1.31, 1.84) more zones than when involved with information tasks. Equipment and material tasks were also associated with traveling through 148% (95%CI: 2.17, 2.85) and 246% (95%CI: 3.05, 3.88) more zones than when the CN was engaged in information tasks, respectively. Surgeries 4 (OR A, Open Inguinal Hernia Repair) and 7 (OR A, Laparoscopic Band Removal & Lap. Gastric Bypass) appeared to require significantly less travelling than other surgeries, while surgery 18 (OR B, Pediatric Bronchoscopy/Laryngoscopy) required more movements between zones.
Table 2.
Quasi-Poisson regression model predicting the total (transitional + functional) number of zones that the CN traveled through during each PEMSI task
| Coefficient | Estimate | Std. Error | t-value | p-value | Odds Ratio | 95%CI on Odds Ratio |
|---|---|---|---|---|---|---|
| Intercept | −3.24 | 0.05 | −61.27 | <0.001 | ||
| Operating Room C | 0.18 | 0.06 | 3.01 | 0.003 | 1.20 | (1.06, 1.35) |
| Operating Room B | −0.16 | 0.09 | −1.79 | ns | ||
| Equipment Tasks | 0.91 | 0.07 | 13.10 | <0.001 | 2.49 | (2.17,2.85) |
| Patient Tasks | 0.44 | 0.09 | 5.11 | <0.001 | 1.56 | (1.31, 1.84) |
| Materials Tasks | 1.24 | 0.06 | 19.97 | <0.001 | 3.44 | (3.05, 3.88) |
| Surgery 4 | −0.36 | 0.12 | −3.13 | 0.002 | 0.70 | (0.55, 0.87) |
| Surgery 7 | −0.34 | 0.10 | −3.46 | <0.001 | 0.71 | (0.59, 0.86) |
| Surgery 18 | 0.55 | 0.18 | 2.98 | 0.003 | 1.73 | (1.19, 2.46) |
|
| ||||||
| Dispersion | 5.059 | |||||
| Deviance at convergence | 5358.2 | df=1465 | ||||
| Deviance at intercept | 7949.3 | df=1473 | ||||
The research team conducted a similar analysis for the transitional zones only (Table 3). This analysis found significant differences between OR C and the other ORs (odds ratio=1.53, 95%CI: 1.34, 1.75). Additionally, equipment (odds ratio=2.61, 95%CI: 2.27, 3.00) and materials tasks (odds ratio=3.56, 95%CI: 3.14, 4.03) required significantly more crossing of transitional zones. Similarly, to the overall zones model, this model includes covariates for surgeries that were significantly different from the other surgeries in the sample. Surgeries 4 (OR A, Open Inguinal Hernia Repair), 7 (OR A, Laparoscopic Band Removal & Lap. Gastric Bypass), 15 (OR C, Pediatric Broviac Catheter Insertion), and 16 (OR C, Pediatric Gastrocutaneous Fistula Closure) required less movement than the other surgeries in this sample.
Table 3.
Quasi-Poisson regression model predicting the number of transitional zones that the CN traveled through during each PEMSI task
| Coefficient | Estimate | Std. Error | t-value | p-value | Odds Ratio | 95% CI on Odds Ratio |
|---|---|---|---|---|---|---|
| Intercept | −3.90 | 0.05 | −74.32 | <0.001 | ||
| Operating Room C | 0.43 | 0.07 | 6.23 | <0.001 | 1.53 | (1.34, 1.75) |
| Operating Room B | −0.13 | 0.09 | −1.45 | ns | ||
| Equipment Tasks | 0.96 | 0.07 | 13.46 | <0.001 | 2.61 | (2.27, 3.00) |
| Material Tasks | 1.27 | 0.06 | 20.21 | <0.001 | 3.56 | (3.15, 4.03) |
| Surgery 4 | −0.41 | 0.13 | −3.14 | 0.002 | 0.67 | (0.51, 0.85) |
| Surgery 7 | −0.46 | 0.11 | −4.06 | <0.001 | 0.63 | (0.50, 0.78) |
| Surgery 16 | −0.49 | 0.18 | −2.78 | 0.005 | 0.61 | (0.42, 0.85) |
| Surgery 17 | −0.48 | 0.16 | −2.96 | 0.003 | 0.62 | (0.45, 0.84) |
|
| ||||||
| Dispersion | 3.095 | |||||
| Deviance at convergence | 3317.1 | df=1465 | ||||
| Deviance at intercept | 5051.9 | df=1473 | ||||
Since the distribution of the estimates of distance travelled was heavily left skewed, an ordered logistic regression model (Table 4) was used to predict the likelihood of the CNs traveling longer distances during each task, based on the categories of no movement, movement less than 10 meters, or movement greater than 10 meters. The CNs were more likely to travel longer distances in OR C (odds ratio=1.41, 95% CI: 1.10, 1.81) than in the other ORs and were 1.53 times (95% CI: 1.07, 2.19) more likely to travel longer distances during patient tasks than during any other tasks. Surgery 9 (OR A, Gastrostomy Tube Replacement) reflected significantly less distance travelled than other surgeries.
Table 4.
The ordered logistic regression model predicting the distance traveled during each PEMSI task
| Estimate | Std. Error | t-stat | p-value | Odds Ratio (95% CI) | |
|---|---|---|---|---|---|
| None (baseline) | |||||
| <10m | −1.73 | 0.08 | −20.97 | <0.001 | |
| >10m | 0.94 | 0.07 | 13.71 | <0.001 | |
|
| |||||
| Operating Room C | 0.34 | 0.13 | 2.71 | 0.007 | 1.41 (1.10, 1.81) |
| Patient tasks | 0.43 | 0.18 | 2.36 | 0.020 | 1.53 (1.07, 2.19) |
| Surgery 9 | −0.88 | 0.21 | −4.28 | <0.001 | 0.41 (0.28, 0.62) |
|
| |||||
| Convergence Residual Deviance | 2789.21 | ||||
| AIC: | 2799.21 | ||||
| Intercept Residual Deviance | 2823.33 | ||||
| AIC: | 2827.33 | ||||
3.2. Flow Disruptions
A total of 584 CN-related FDs were observed in the 25 surgeries, of which 74% were layout FDs and 26% were environmental hazard FDs. For the analysis, binary dummy variables were used to identify when a CN was involved in any type of FD during a task. Additional binary dummy variables were created for CN-involved environmental hazard FDs and CN-involved layout FDs. The analysis (see Table 5) found that when working in OR C, the CN was 2.11 times more likely to be associated with FDs than the other ORs (95%CI: 1.55, 2.78). FDs were also more likely to occur for equipment, patient, or materials tasks (odds ratio=5.41, 95%CI: 3.76, 7.81), 3.23, (95%CI: 1.99, 5.22), and 4.55 (95%CI: 3.25, 6.41), respectively. As in the previous models, Surgery 4 experienced less FDs overall.
Table 5.
Logistic regression model predicting the occurrences of a CN-involved SFD during each of the CN’s PEMSI tasks across all surgeries
| Coefficient | Estimate | Std. Error | t-value | p-value | Odds Ratio (95% CI) |
|---|---|---|---|---|---|
| Intercept | −6.27 | 0.14 | −44.65 | <0.001 | |
| Operating Room C | 0.75 | 0.16 | 4.75 | <0.001 | 2.11(1.55, 2.87) |
| Equipment Tasks | 1.69 | 0.19 | 9.06 | <0.001 | 5.41(3.76, 7.81) |
| Patient Tasks | 1.17 | 0.25 | 4.76 | <0.001 | 3.23(1.99, 5.22) |
| Materials Tasks | 1.52 | 0.17 | 8.74 | <0.001 | 4.55(3.25, 6.41) |
| Surgery 4 | −1.94 | 0.45 | −4.28 | <0.001 | 0.14(0.05, 0.32) |
|
| |||||
| Deviance at convergence | 1462.5 | df=1468 | |||
| Deviance at intercept | 1622.3 | df=1473 | |||
Focusing only on environmental hazard FDs, similar patterns were present (see Table 6). The CN encountered more environmental hazard FDs when working in OR C (odds ratio=2.62, 95%CI: 1.48, 4.58) and OR B (odds ratio=2.77, 95%CI: 1.40, 5.27) than in OR A. Patient tasks were most disrupted (odds ratio=12.75 95%CI: 6.12, 27.45), followed by equipment (odds ratio=7.01, 95%CI:3.44, 14.75), and material tasks (odds ratio=5.77, 95%CI: 2.85, 12.07), which were more likely to experience FDs than information tasks. This is independent of the surgeries conducted, that is, there were no significant effects of individual surgeries in the model.
Table 6.
Logistic regression model predicting the occurrences of a CN-involved environmental hazard during each of the CN’s PEMSI tasks across all surgeries
| Coefficient | Estimate | Std. Error | t-value | p-value | Odds Ratio (95%CI) |
|---|---|---|---|---|---|
| Intercept | −8.93 | 0.33 | −27.30 | <0.001 | |
| Operating Room C | 0.97 | 0.29 | 3.36 | <0.001 | 2.62 (1.48, 4.58) |
| Operating Room B | 1.02 | 0.34 | 3.03 | 0.002 | 2.77 (1.40, 5.27) |
| Equipment Tasks | 1.95 | 0.37 | 5.28 | <0.001 | 7.01 (3.44, 14.75) |
| Patient Tasks | 2.55 | 0.38 | 6.69 | <0.001 | 12.75 (6.12, 27.45) |
| Materials Tasks | 1.75 | 0.37 | 4.80 | <0.001 | 5.77 (2.85, 12.07) |
|
| |||||
| Deviance at convergence | 547.43 | df=1468 | |||
| Deviance at intercept | 612.51 | df=1473 | |||
Finally, FDs to CN tasks caused by OR layout were more likely to occur in OR C (odds ratio=2.77, 95%CI: 1.95, 3.91) than in ORs B or A (see Table 7). Similar to previous models, CN-involved, layout-related FDs were most likely to occur during equipment tasks, (odds ratio=6.81, 95%CI: 4.48, 10.41), followed by material tasks (odds ratio=5.30, 95%CI: 3.57, 7.91), and patient tasks (odds ratio=3.93, 95%CI: 2.28, 6.72). Surgeries 4 and 10 (OR A, Laparoscopic Cholecystectomy) were the only specific surgeries that were significant in the statistical model, reflecting significantly less FDs than other procedures.
Table 7.
Logistic regression model predicting the occurrences of a CN-involved layout SFD during each of the CN’s PEMSI tasks across all surgeries
| Coefficient | Estimate | Std. Error | t-value | p-value | Odds Ratio (95% CI) |
|---|---|---|---|---|---|
| Intercept | −7.00 | 0.18 | −38.61 | <0.001 | |
| Operating Room C | 1.02 | 0.18 | 5.76 | <0.001 | 2.77 (1.95, 3.91) |
| Operating Room B | 0.19 | 0.24 | 0.77 | NS | |
| Equipment Tasks | 1.92 | 0.21 | 8.93 | <0.001 | 6.81 (4.48, 10.41) |
| Patient Tasks | 1.37 | 0.28 | 4.96 | <0.001 | 3.93 (2.28, 6.72) |
| Material Tasks | 1.67 | 0.20 | 8.22 | <0.001 | 5.30 (3.57, 7.91) |
| Surgery 4 | −1.88 | 0.55 | −3.44 | <0.001 | 0.15 (0.04, 0.40) |
| Surgery 10 | −1.31 | 0.55 | −2.39 | 0.02 | 0.27 (0.08, 0.71) |
|
| |||||
| Deviance at convergence | 1220.8 | df=1466 | |||
| Deviance at intercept | 1385.6 | df=1473 | |||
4. DISCUSSION
Video observation and analysis of CN movement activities demonstrated consistent effects of OR layout, tasks, and specific surgeries on zones crossed, distances travelled, and the FDs they experienced. CNs working in OR C generally had to travel across more OR zones, travelled further distances, and experienced more FDs compared to the other two ORs studied. While the CN in OR B generally had to transition through fewer zones, they experienced more FDs. Materials and equipment tasks consistently required greater movement across the ORs than patient and information tasks, though patient tasks were frequently disrupted with environmental hazard FDs. Although the data sample did not have a balance of surgery types across different ORs, it was possible to account for this balance within the statistical model, which revealed certain surgeries to be more or less affected. In particular, Surgery 4 appeared to be less demanding in terms of CN movement and the CN generally experienced fewer FDs. While this study cannot address why these differences occurred, it is interesting that the OR associated with the longest distances walked is associated with the fewest zones traveled through. Though the results may not be definitive, they are among the first to demonstrate the impact of different tasks, surgeries, and OR layouts on the work of the CN.
It is not surprising that patient, equipment, and material tasks involved more movement and encountered more FDs than information-related tasks, since the subcategories of these tasks involve moving items or collecting items around the OR. Information-related tasks typically involve computer work at the CN workstation. Patient-related tasks were not significantly different from the other tasks in terms of the number of transitional zones passed through. However, the CN was more likely to walk longer distances when completing patient-related tasks. This suggests that there may be differences in how the location or the arrangement of the room affects the CN’s patient-related tasks. Patient-related tasks were also more disrupted by environmental hazards (bumping into equipment; tension on patient lines). Across all ORs, CNs were more likely to be involved in layout and environmental hazard FDs when involved in patient, material, or equipment-related tasks compared to information tasks. There were also differences between the ORs as the CN was more likely to be involved in environmental hazard FDs in OR C and OR B and was more likely to be involved in layout FDs in OR C. This suggests that even when accounting for other covariates, the environment and the specific tasks within which the work is being done impact the likelihood of the CN being involved in environmental hazard and layout FDs.
Not all OR layouts or sizes are the same. In this study, we examined three different ORs that had different sizes and layouts. OR A is newer and is the largest OR in our sample and experienced greater CN movements than the smallest, older OR (OR B). However, OR C was associated with more zone transitions and the most FDs. Thus, size alone cannot account for the differences observed. One key difference between the layouts appears to be the space available in the transition zone at the foot of the surgical table. While functional zones require equipment and/or workspace, these transitional zones indicate open space. Both ORs B and C have narrow transitional zone spaces available at the foot of the surgical table compared to OR A. The CN workstation is located near the foot of the surgical table in all three layouts but with considerably more space in OR A. Separating our analysis into these transitional zones allowed us to explore the relationship between space and tasks more in depth. Presumably, there is a trade-off between the size of the OR and the ability to work within it. A large OR may facilitate movement and be less cluttered, but it requires the CN to travel longer distances between tasks. On the other hand, although a small OR may require travelling shorter distances, it may impose difficulties on performing tasks within smaller zones. Interestingly, FDs were higher in the two older, smaller ORs suggesting that the extra space in OR A may allow less inhibited movement. In other words, the trade-off between the room size and the ability to work within it shows that, despite greater freedom of movement, a larger room requires longer travel distance. This demonstrates why movements, activities, and the success of those activities may need to be explored together.
Different surgeries were studied across the three ORs. Though the effects of individual surgical requirements from the ORs in which they occurred cannot be entirely separated, the quasi-Poisson regression somewhat accounted for this co-variation, specifically identifying surgeries as outliers within the statistical models. Surgery 4 was significantly different from the other surgeries in most of the models presented here. While it was among the longer duration surgeries, it was not the longest in OR A or across the whole sample. It was an Open Inguinal Hernia Repair, so that surgery may have had characteristics that lead to different tasks and activities for the CN. Thus, while there may be a room layout that is optimal for most or all surgeries, there may be an interaction between surgical demands and room layout, as there are synergies between the layout configurations, tasks, and equipment locations, and outcomes such as FDs (Wiegmann, Eggman, ElBardissi, Parker, & Sundt, 2010). Eventually it may be possible to suggest generic design elements to suit all operations, with variations of designs for specific surgeries. To a gross extent, this has already happened with cardiac hybrid ORs, which have been specifically designed to house interventional catheter interventions and open cardiac surgery (Babaliaros et al., 2014). However, it is clear that these efforts have not always been successful (Babaliaros et al., 2014). Arguably, direct observation of ‘work as done’ will be critical for establishing better room designs that take into account the work demands of different surgeries.
The detailed video observations allowed for exploration of the interactions between OR design, tasks, and surgeries in more detail than has been possible before. Karsh et al. (2006) emphasized the importance of understanding different parts of a work system and the interdependencies which impact healthcare professionals. Our study further shapes human factors engineering paradigms for improving patient safety by demonstrating a comprehensive approach where both tasks and the space are broken down into low level units (e.g., seconds, zones). The statistical analyses also allowed for a detailed exploration of interactions in the OR, and although it was not possible to experimentally control for procedure types, researchers were able to control across task levels and thus compare directly within different tasks. This accounted for differences in some of the surgeries. Looked at cohesively, the statistical analyses provide a more sophisticated model of systems effects on FDs than many similar FD studies. Rather than just counting FD events, this is one of the first attempts to account for the environmental component of a model of surgical systems. The use of video, in particular, allowed the abstraction of the detailed dataset needed for this level of modeling. While this may not be suitable for all healthcare applications, surgery is especially amenable to this type of research.
A limitation of the current study was the reliance on a convenience sample of procedures from three different ORs. This was done due to the practical limitations associated with the time and effort required in repositioning video recording equipment and obtaining consents from surgical personnel between surgeries. As a result, the equipment was set up the night before and video recordings were conducted for all surgeries in the same OR for one or two consecutive days. Using another approach, such as direct observations, would have allowed for a more diverse set of surgeries, at the expense of specific and comprehensive data. Given the surgery schedules and availability of the ORs for video recording, the composition of surgical teams and familiarity of the surgical team members with one another may have played a role in synergies during surgery that were not controlled. Future research should evaluate a balanced sample of specific procedure types or target specific procedures and may seek to examine the same operations in different ORs or across different surgical teams or different surgeons. While the results would be expected to be similar, validating this work with a broader representative sample is an important next step in evaluating the work practices using a systems perspective. Graduate students coded the tasks and FDs and effort was taken to develop and maintain consistency in coding including verifying tasks and situations with clinical staff, but there may be some misclassifications or omissions in events and tasks categorizations due to human error. Therefore, while internally consistent, care should be taken in extrapolating this work to other OR layouts or work systems. A future extension of this study intends to examine observations of other team members and how surgical technologies (e.g., perfusion or surgical robotics) might impact these initial findings.
Another limitation of the current study was the boundaries of the system, the OR doors. This was an artifact of the video data collection and the analysis approach, in that there was no video data outside of the OR. This is a methodological limitation that potentially prevented accounting for the tasks that the CN performed outside of the OR. Future research may extend the system boundary to follow the CN both inside and outside of the OR.
5. Conclusion
Operating room design is an exercise in satisficing competing demands in terms of workspaces, storage capacity, maneuverability, and costs. Using a systems approach, this observational study sought to observe, capture, and analyze the impact of the OR layout on CNs’ activities and resulting disruptions in multiple ORs. This observational study confirms that within a surgery, the room layout can significantly affect CNs’ movement within the OR and their ability to complete tasks easily and successfully. This study contributes to the ongoing range of techniques available to describe the function of surgical systems from a human-centered perspective.
Highlights.
An operating room layout can influence work patterns of circulating nurses.
Smaller zones may predispose circulating nurses to more flow disruptions.
Layout can influence travel distance and number of zones travelled through.
Physical environment is an influential element of the work system.
Acknowledgments
The authors would like to thank the RIPCHD.OR Study Group for their contribution to the work supporting the effort in this study. This work was supported by the Agency for Healthcare Research and Quality [grant number P30HS0O24380, 2015].
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ahmad N, Hussein AA, Cavuoto L, Sharif M, Allers JC, Hinata N, Guru KA. Ambulatory movements, team dynamics and interactions during robot-assisted surgery. BJU International. 2016;118(1):132–139. doi: 10.1111/bju.13426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alfredsdottir H, Bjornsdottir K. Nursing and patient safety in the operating room. Journal of Advanced Nursing. 2007;61(1):29–37. doi: 10.1111/j.1365-2648.2007.04462.x. [DOI] [PubMed] [Google Scholar]
- Anderson O, Davis R, Hanna GB, Vincent CA. Surgical adverse events: a systematic review. The American Journal of Surgery. 2013;206(2):253–262. doi: 10.1016/j.amjsurg.2012.11.009. [DOI] [PubMed] [Google Scholar]
- Babaliaros V, Devireddy C, Lerakis S, Leonardi R, Iturra SA, Mavromatis K, Thourani VH. Comparison of Transfemoral Transcatheter Aortic Valve Replacement Performed in the Catheterization Laboratory (Minimalist Approach) Versus Hybrid Operating Room (Standard Approach): Outcomes and Cost Analysis. JACC: Cardiovascular Interventions. 2014;7(8):898–904. doi: 10.1016/j.jcin.2014.04.005. [DOI] [PubMed] [Google Scholar]
- Beyea SC, Hicks RW, Becker SC. Medication Errors in the OR—A Secondary Analysis of Medmarx. AORN Journal. 2003;77(1):122–134. doi: 10.1016/S0001-2092(06)61382-3. [DOI] [PubMed] [Google Scholar]
- Catchpole K, Ley E, Wiegmann D, Blaha J, Shouhed D, Gangi A, Gewertz B. A human factors subsystems approach to trauma care. JAMA Surgery. 2014;149(9):962–968. doi: 10.1001/jamasurg.2014.1208. [DOI] [PubMed] [Google Scholar]
- de Leval MR, Carthey J, Wright DJ, Farewell VT, Reason JT. Human factors and cardiac surgery: a multicenter study. The Journal of Thoracic and Cardiovascular Surgery. 2000;119(4):661–672. doi: 10.1016/S0022-5223(00)70006-7. [DOI] [PubMed] [Google Scholar]
- Gawande AA, Zinner MJ, Studdert DM, Brennan TA. Analysis of errors reported by surgeons at three teaching hospitals. Surgery. 2003;133(6):614–621. doi: 10.1067/msy.2003.169. [DOI] [PubMed] [Google Scholar]
- Greenberg CC, Regenbogen SE, Studdert DM, Lipsitz SR, Rogers SO, Zinner MJ, Gawande AA. Patterns of communication breakdowns resulting in injury to surgical patients. Journal of the American College of Surgeons. 2007;204(4):533–540. doi: 10.1016/j.jamcollsurg.2007.01.010. [DOI] [PubMed] [Google Scholar]
- Kang E, Massey D, Gillespie BM. Factors that influence the non-technical skills performance of scrub nurses: a prospective study. Journal of Advanced Nursing. 2015;71(12):2846–2857. doi: 10.1111/jan.12743. [DOI] [PubMed] [Google Scholar]
- Karsh BT, Holden RJ, Alper SJ, Or CKL. A human factors engineering paradigm for patient safety: designing to support the performance of the healthcare professional. Quality and Safety in Health Care. 2006;15(suppl 1):i59–i65. doi: 10.1136/qshc.2005.015974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoshkenar A, Taaffe K, Muhs M, Fredendall L, Ferrand Y, San D, Joseph A. Simulation-based design and traffic flow improvements in the operating room Technical Report 2017 [Google Scholar]
- Morgan L, Pickering SP, Hadi M, Robertson E, New S, Griffin D, McCulloch P. A combined teamwork training and work standardisation intervention in operating theatres: controlled interrupted time series study. BMJ Quality & Safety. 2014 doi: 10.1136/bmjqs-2014-003204. bmjqs-2014. [DOI] [PubMed] [Google Scholar]
- Morgan L, Robertson E, Hadi M, Catchpole K, Pickering S, New S, McCulloch P. Capturing intraoperative process deviations using a direct observational approach: The glitch method. BMJ Open. 2013;3(11):e003519. doi: 10.1136/bmjopen-2013-003519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer G, Abernathy James H, III, Swinton G, Allison D, Greenstein J, Shappell S, Reeves ST. Realizing improved patient care through human-centered operating room design: A human factors methodology for observing flow disruptions in the cardiothoracic operating room. Anesthesiology. 2013;119(5):1066–1077. doi: 10.1097/ALN.0b013e31829f68cf. Retrieved from . [DOI] [PubMed] [Google Scholar]
- Persson J, Dalholm EH, Johansson G. Informing Hospital Change Processes through Visualization and Simulation: A Case Study at a Children’s Emergency Clinic. HERD: Health Environments Research & Design Journal. 2014;8(1):45–66. doi: 10.1177/193758671400800105. [DOI] [PubMed] [Google Scholar]
- Ritchie CR. Fundamental Perioperative Nursing: Decompartmentalizing the Scrub and Circulator Roles. Perioperative Nursing Clinics. 2009;4(2):167–180. doi: 10.1016/j.cpen.2009.01.001. [DOI] [Google Scholar]
- Simmons D, Graves K, Flynn EA. Threading Needles in the Dark. Critical Care Nursing Quarterly. 2009;32(2):71–74. doi: 10.1097/CNQ.0b013e3181a27d99. [DOI] [PubMed] [Google Scholar]
- Spry C. Essentials of perioperative nursing. Jones & Bartlett Learning; 2009. [Google Scholar]
- Weinger MB, Slagle J, Jain S, Ordonez N. Retrospective data collection and analytical techniques for patient safety studies. Journal of Biomedical Informatics. 2003;36(1-2):106–119. doi: 10.1016/j.jbi.2003.08.002. [DOI] [PubMed] [Google Scholar]
- Wheelock A, Suliman A, Wharton R, Babu ED, Hull L, Vincent C, Arora S. The Impact of Operating Room Distractions on Stress, Workload, and Teamwork. Annals of Surgery. 2015;261(6):1079–1084. doi: 10.1097/SLA.0000000000001051. Retrieved from http://journals.lww.com/annalsofsurgery/Fulltext/2015/06000/The_Impact_of_Operating_Room_Distractions_on.10.aspx. [DOI] [PubMed] [Google Scholar]
- Wiegmann DA, Eggman AA, ElBardissi AW, Parker SH, Sundt TM. Improving cardiac surgical care: A work systems approach. Applied Ergonomics. 2010;41(5):701–712. doi: 10.1016/j.apergo.2009.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiegmann DA, ElBardissi AW, Dearani JA, Daly RC, Sundt TM. Disruptions in surgical flow and their relationship to surgical errors: An exploratory investigation. Surgery. 2007;142(5):658–665. doi: 10.1016/j.surg.2007.07.034. [DOI] [PubMed] [Google Scholar]
- Yang YT, Henry L, Dellinger M, Yonish K, Emerson B, Seifert PC. The Circulating Nurse’s Role in Error Recovery in the Cardiovascular OR. AORN Journal. 2012;95(6):755–762. doi: 10.1016/j.aorn.2011.09.022. [DOI] [PubMed] [Google Scholar]


