ABSTRACT
Background
Urgent-start peritoneal dialysis (USPD) was designed to avoid temporary hemodialysis initiation with a hemodialysis catheter. In these patients, PD is initiated within 2 weeks of catheter placement, but typically these prescriptions utilize automated peritoneal dialysis (APD) with a cycler. Manual exchanges have not been reported previously for USPD. We hypothesize that using multiple, low-volume manual exchanges, patients will have similar rates of peritonitis, exit-site infection (ESI), pericatheter leaks and discontinuation of PD in the first 3 months after initiation.
Methods
This retrospective study included patients who initiated PD in our unit from May 2014 until August 2016 using our USPD protocol. Patients with a body surface area <1.7 m2 used 750 mL dwell volumes and those >1.7 m2 used 1000 mL dwell volumes during the first 7 days. Dwell times were 2–2.5 h for two to three exchanges per day. After 7 days of successful therapy, the dwell volumes were doubled. All patients were maintained on furosemide 160 mg twice daily.
Results
There were 20 patients enrolled in our USPD program. Our rates of peritonitis, ESI, pericatheter leak and discontinuation of PD were 5%, 0%, 5% and 5%, respectively.
Conclusions
Manual exchange during USPD is a viable modality with similar results as APD. Using manual exchanges allows patients to be more ambulatory during the day when they are not dwelling, allows nurses to evaluate the amount of ultrafiltration and effluent characteristics and allows for training in manual exchanges as well.
Keywords: cycler, ESRD, manual exchanges, peritoneal dialysis, urgent start
Introduction
Peritoneal dialysis (PD) is a type of renal replacement therapy for patients with end-stage renal disease (ESRD). It involves filling the peritoneal cavity with a dextrose-containing solution and using the peritoneal membrane as a filter to remove toxins, regulate electrolytes and remove volume. Peritoneal dialysis can be done with multiple daily manual exchanges or using a cycler for a fixed period of time every day of the week. Historically these patients would not be able to intiate PD until at least 2 weeks after placement of a PD catheter in order to avoid complications such as abdominal cavity or pericatheter leaks. Many patients who require urgent dialysis typically are started on hemodialysis (HD) with a central venous catheter (CVC) and PD is typically reserved for planned starts [1].
Urgent-start PD (USPD) was designed to avoid temporary HD initiation while awaiting approval to use a PD catheter. In these patients, PD is initiated 24–48 h after PD catheter placement, typically in the outpatient setting [2]. Patients are discharged after PD catheter placement and PD is initiated in the dialysis clinic, although this can also be done in the hospital dialysis unit setting. Various dialysis prescriptions have been described in the literature for USPD, but these prescriptions utilize automated PD (APD) with a cycler [3]. This requires patients to be connected to the cycler 5–12 h during each treatment in the supine position. The low dwell volumes while in the supine position during these protocols are particularly important to decrease the risk of developing a leak [4]. Other programs have reported their success rates with US PD previously, and rates of peritonitis and exit-site infection (ESI) are similar, with a slightly increased risk of pericatheter leaks that have been controlled with holding PD for a short period and then restarting therapy [5, 6]. In one study of 52 patients, rates of peritonitis, ESI and pericatheter leak were 15.4%, 3.9% and 7.7%, respectively [3].
While the majority of studies published on USPD programs use APD, we did find one study published in 2007 by Jo et al. [7] that evaluated 51 patients who had a PD catheter placed and initated on continuous ambulatory PD (CAPD) immediately after placement without a break-in period. The patients had 500 mL instilled every 3 h for the first 3 days and patients were kept in the supine position during this time with minimal ambulation. They then increased the dwell volume to 1 L every 4 h for the next 4 days. Seven 7 days after the catheter insertion, they began 2 L exchanges with a dwell time of 4 h. In this study the authors found only one pericatheter leak that occurred within the first month and catheter malfunction, ESI and peritonitis rates were 1.9%, 2.9% and 3.9%, respectively [7].
We hypothesized that using our protocol, which involved multiple, low-volume manual exchanges during the initiation period, patients would have similar rates of peritonitis, ESI and pericatheter leaks in the first 3 months after initiation compared with the data presented for the APD and CAPD programs. We also evaluated how many patients remained on PD 12 months after USPD for initiation.
Materials and methods
Institutional review board approval (protocol #9567) was obtained for this study. We performed a retrospective review of our USPD patient records from May 2014 to August 2016 in our PD unit. All patients in our USPD program followed our protocol using manual exchanges. For our protocol, all patients were started on PD within 2 weeks of catheter placement (most patients within 48 h of catheter placement). Any patient who started PD ≥2 weeks after catheter placement were excluded from this study. Patients with a body surface area (BSA) <1.7 m2 used 750 mL dwell volumes and those with a BSA >1.7 m2 used 1000 mL dwell volumes during the first 7 days. Dwell times were 2–2.5 h for two to three exchanges per day, 4–5 days per week. After 7 days of successful therapy the dwell volumes were doubled (see Figure 1). All patients were maintained on furosemide 160 mg twice daily. There were no significant side effects with this dosage of furosemide, such as hearing loss. Urine output was not measured during the initiation period. One patient was initiated on PD secondary to loss of all vascular access after being on HD for >5 years and therefore she had no residual urine output. We had two PD nurses in our clinic who evaluated patients and performed all of the exchanges. Based on clinical assessments, patients would receive additional treatments (three per day) or additional days (6 per week) for reasons such as edema or uremic symptoms. We also evaluated the number of patients who developed peritonitis, ESI, abdominal or pericatheter leaks within the first 3 months of initiation, as well as whether the patient chose to continue PD after the initiation period.
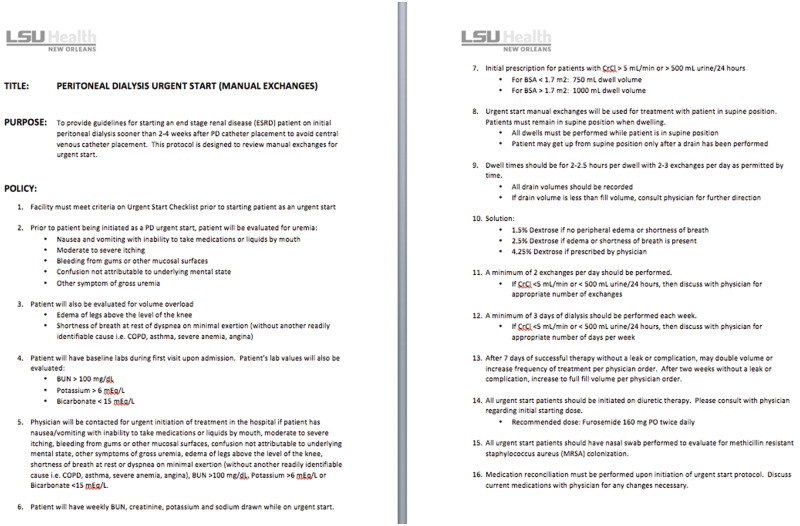
Fig. 1.
USPD manual exchange protocol. It includes a 16-step process that is followed in the clinic.
Results
There were 20 patients who were enrolled in our USPD program between May 2014 and August 2016. The group comprised 35% female patients and 65% male patients and the mean age was 48 years. The mean initial estimated glomerular filtration rate was 9.6 mL/min prior to starting PD. The majority of our patients initiated dialysis due to uremic symptoms (including but not limited to nausea, vomiting, loss of appetite and asterixis). The decision to initiate dialysis occurred as an inpatient for 80% of these patients. None of the patients required inpatient PD but were discharged after catheter placement and initiated in the outpatient PD unit within 48 h of catheter placement. General surgeons placed all of the catheters using a laparoscopic technique.
Baseline characteristics of the patients are listed in Table 1. A summary of baseline characteristics is listed in Table 2. Given the variability in patient schedules and transportation issues for some of the patients, the dialysis prescriptions varied day to day but stayed within our protocol. The dwell volumes were based on BSA (BSA <1.7 m2 used 750 mL dwell volumes and BSA >1.7 m2 used 1000 mL dwell volumes during the first 7 days and then doubled the second week) and were strictly adhered to by our protocols. The type of dextrose solution (1.5% versus 2.5%) was left to the discretion of the nurse and the nephrologist based on the patient’s volume status as assessed by blood pressure and edema.
Table 1.
Baseline characteristics
| Patient | Age (years) | Sex | Race | ESRD etiology | eGFR (mL/min) | Reason to initiate | Setting |
|---|---|---|---|---|---|---|---|
| 1 | 25 | Male | Black | HIV nephropathy | 4 | Uremia/volume overload | Inpatient |
| 2 | 46 | Female | White | PKD | 12 | Uremia | Outpatient |
| 3 | 38 | Female | Black | Lupus nephritis | 4 | Uremia/volume overload | Inpatient |
| 4 | 44 | Female | Black | Diabetes and hypertension | 12 | Uremia | Inpatient |
| 5 | 51 | Male | Black | Hypertension | 10 | Hyperkalemia | Inpatient |
| 6 | 47 | Male | Black | Hypertension | 7 | Uremia | Inpatient |
| 7 | 40 | Male | Black | Diabetes and hypertension | 7 | Uremia/volume overload | Inpatient |
| 8 | 65 | Female | Black | Hypertension | 11 | Uremia | Inpatient |
| 9 | 47 | Female | Black | Diabetes and hypertension | 14 | Uremia/volume overload | Outpatient |
| 10 | 43 | Male | Black | Hypertension | 6 | Uremia | Inpatient |
| 11 | 41 | Female | Black | Hypertension | 0 | Loss of vascular access | Inpatient |
| 12 | 53 | Male | Black | Hypertension | 13 | Uremia/volume overload | Inpatient |
| 13 | 42 | Male | Black | Hypertension | 12 | Uremia/volume overload | Inpatient |
| 14 | 39 | Male | Black | Diabetes and hypertension | 10 | Uremia/volume overload | Inpatient |
| 15 | 46 | Male | Black | Diabetes and hypertension | 9 | Uremia/volume overload | Inpatient |
| 16 | 61 | Male | Black | Diabetes and hypertension | 18 | Uremia/hyperkalemia | Inpatient |
| 17 | 64 | Female | Black | Diabetes and hypertension | 6 | Uremia | Outpatient |
| 18 | 51 | Male | Black | Hypertension | 11 | Uremia | Outpatient |
| 19 | 57 | Male | Black | Hypertension | 2 | Uremia | Inpatient |
| 20 | 60 | Male | Black | Hypertension | 24 | Volume overload (systolic CHF) | Inpatient |
eGFR, estimated glomerular filtration rate; PKD, polycystic kidney disease; CHF, congestive heart failure.
Table 2.
Summary of baseline characteristics
| Age (years) | 48 (range 25–65) |
| Sex, n (%) | |
| Male | 13 (65) |
| Female | 7 (35) |
| Race or ethnic group, n (%) | |
| Black | 19 (95) |
| White | 1 (5) |
| Diabetes mellitus, n (%) | 7 (35) |
| Estimated glomerular filtration rate (mL/min) | 9.6 |
| Setting (inpatient versus outpatient), n | 16 versus 4 (80% inpatient) |
Most treatments included two exchanges a day and most patients received dialysis at least 4 days each week, with >90% of patients receiving therapy 5 days a week. Only one patient (5%) received three exchanges a day and 6 days a week due to severe uremic symptoms and marked volume overload with no residual renal function, as this patient had transitioned from HD to PD after losing all vascular access options. This was based on the clinical judgement of the nephrologist and the PD nurse.
Our rates of peritonitis, ESI and abdominal or pericatheter leaks were 5%, 0% and 5%, respectively (Table 3). One patient did not continue PD due to housing issues (95% continued PD), otherwise all patients remained on PD at least 12 months after initiation. All patients initially remained on CAPD until those patients who requested a cycler were able to obtain a cycler. Five of the 20 patients (25%) continued on CAPD without choosing to start cycler therapy after training was complete. No catheter revisions or removals were required.
Table 3.
Complications
| Type of complication | n (%) |
|---|---|
| Abdominal/pericatheter leak | 1 (5) |
| Exit-site infection | 0 (0) |
| Peritonitis | 1 (5) |
| Discontinuation of PD therapy | 1 (5) |
| Patients who remained on CAPD | 5 (25) |
The one patient with peritonitis developed a Pseudomonas peritonitis that was treated for 21 days with intraperitoneal ceftazidime and oral ciprofloxacin with resolution of the peritonitis. Catheter removal was not necessary.
For the single patient with the pericatheter leak, we noted the leak on Day 2 of dialysis. PD was discontinued for 2 weeks, while monitoring laboratory results every 4 days, and then restarted with low volumes following the USPD protocol without any further leak. Backup HD was never necessary.
Discussion
USPD has become a mainstay of PD initiation and decreases the need for CVC placement for urgent initiation of renal replacement therapy. To date, most USPD programs utilize an APD protocol that requires patients to lay supine for 5–12 h while dwelling. If a patient needs to get up to use the bathroom or eat, then the nurse must drain the patient and pause the cycler therapy. Using manual exchanges as in our protocol, patients only need to lie supine 2–4 h depending on the prescribed dwell time. Patients can then be ambulatory between exchanges. This allows for natural breaks throughout the day to allow patients to eat, use the restroom and take breaks.
Since our patients are trained in manual exchanges during this initiation period, this allows for a higher degree of familiarity and comfort performing manual exchanges. In areas where patients may have frequent weather disturbances, electricity outages or cycler malfunctions, being proficient in manual exchanges is extremely important. Within our patient population, 25% of patients opted to remain on CAPD rather than transition to cycler-based therapy (Table 3). Our nurses also preferred using manual exchanges, as it allowed them to evaluate fill and drain times of the catheter and ultrafiltration volume with each dwell, and there are no alarms due to cycler issues. This protocol also limits the need for cyclers to be used during training, particularly in areas where obtaining a cycler may be difficult.
We acknowledge that a major limitation of our study is the relatively small sample size of 20 patients and limited to one center. We believe one strength of our study is that five various surgeons placed these PD catheters, which leads us to believe our success in manual exchanges for initiation was independent of surgeon variability. Future directions would include increasing the sample size or the number of programs utilizing this method to evaluate outcomes and performing a large randomized clinical trial comparing manual exchanges and cycler therapy for USPD. Another future direction would be to evaluate patient and nurse satisfaction with manual versus cycler training during initiation and to evaluate how many patients remain on CAPD versus APD due to initial manual exchange training. We recognize that this is a retrospective study and realize a randomized and controlled study would better elucidate differences in outcomes in cycler versus manual exchanges in USPD. Using our protocol, we believe other centers can develop their own USPD programs using CAPD if they felt this to be an option. Further utilization of these CAPD protocols will increase the likelihood of future studies in this area.
Conclusions
Our study shows that using manual exchanges for USPD leads to similar or better outcomes as compared with previously reported data in peritonitis, ESI and pericatheter leak rates. Manual exchanges are a viable option for US PD and allows for flexibility in the training schedule. We believe that this method allow programs to utilize either APD or manual exchanges for a successful USPD program. Further prospective studies are needed to better evaluate CAPD compared to APD as a method of USPD initiation.
Authors’ contributions
M.N. and F.Y. were responsible for the research idea, study design, data acquisition, data analysis and statistical analysis. E.R. was responsible for supervision and mentorship. Each author contributed important intellectual contact during manuscript drafting and revision and accepts responsibility for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Conflict of interest statement
M.N. has received fees as a medical director for DaVita Kidney Care.
References
- 1. Van Biesen W, Vanholder R, Lameire N.. The role of peritoneal dialysis as the first-line renal replacement modality. Perit Dial Int 2000; 20: 375–383 [PubMed] [Google Scholar]
- 2. Ghaffari A, Kumar V, Guest S.. Infrastructure requirements for an urgent-start peritoneal dialysis program. Perit Dial Int 2013; 33: 611–617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Povlsen JV, Ivarsen P.. How to start the late referred ESRD patient urgently on chronic APD. Nephrol Dial Transplant 2006; 21: ii56–ii59 [DOI] [PubMed] [Google Scholar]
- 4. Arramreddy R, Zheng S, Saxena AB. et al. Urgent-start peritoneal dialysis: a chance for a new beginning. Am J Kidney Dis 2014; 63: 390–395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ghaffari A. Urgent-start peritoneal dialysis: a quality improvement report. Am J Kidney Dis 2012; 59: 400–408 [DOI] [PubMed] [Google Scholar]
- 6. Casaretto A, Rosario R, Kotzker WR. et al. Urgent-start peritoneal dialysis: report from a U.S. private nephrology practice. Adv Perit Dial 2012; 28: 102–105 [PubMed] [Google Scholar]
- 7. Jo Y, Sin S, Lee J. et al. Immediate initiation of CAPD following percutaneous catheter placement without break-in procedure. Perit Dial Int 2007; 23: 179–183 [PubMed] [Google Scholar]