ABSTRACT
Peripheral arterial disease and diabetic foot syndrome are common comorbidities in dialysis patients. These conditions are treated with intermittent vacuum therapy in order to increase angiogenesis and perfusion. Some devices encase the lower extremities up to the abdomen. Here we report the case of a patient who had performed peritoneal dialysis for 2 years without complications. Following postoperative intermittent vacuum therapy, he presented with extensive catheter leakage. Ultimately the patient had to be switched to haemodialysis and the catheter had to be removed. This case exemplifies that peritoneal dialysis patients have a substantial risk for noninfectious catheter-related complications using vacuum therapy.
Keywords: continuous ambulatory peritoneal dialysis (CAPD), end-stage renal disease (ESRD), intermittent negative-pressure therapy (INPT), noninfectious PD complications, wound healing
Background
Negative pressure therapy is a widely accepted therapeutic approach and has traditionally been applied in vascular and orthopaedic surgery to improve healing of chronic wounds [1, 2]. Recently, new intermittent negative-pressure devices have been introduced to the market [intermittent vacuum therapy (IVT)]. Applications range from treatment of diabetic foot syndrome and peripheral arterial occlusive diseases to lymph-oedema [3–5]. Moreover, it has been used in orthopaedic rehabilitation in order to accelerate subsiding of postoperative swelling and wound healing. For post-traumatic oedema, daily IVT treatment with a duration of 30 min [implying alternating 20 s of negative-pressure phases (varying from −20 to −70 mbar) and 5 s of atmospheric pressure phases] is recommended. The intervals and intensity of negative-pressure phases are variable and little is known about the effects of interchangeable therapeutic parameters. We here in report the case of a 61-year-old male dialysis patient who presented with leakage of his peritoneal dialysis (PD) catheter as a complication of post-operative IVT.
Case presentation
A 61-year-old dialysis patient with end-stage renal disease due to IgA nephropathy was admitted to our hospital with leakage of his PD catheter. Until that time he had performed PD for 2 years without any complications. In 2015, the present catheter was implanted using a laparoscopic technique after one episode of peritoneal infection.
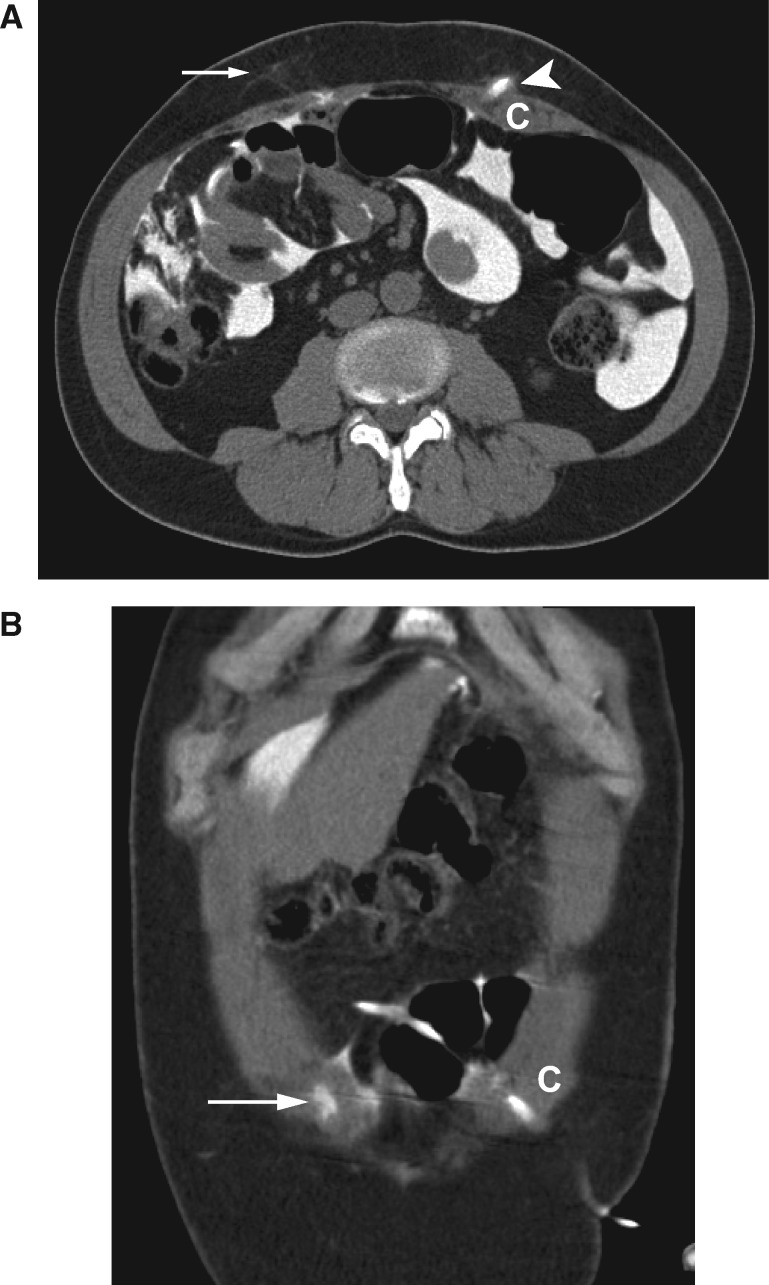
The patient had recently been treated with IVT in a rehabilitation clinic following knee surgery. In this context, not only his lower extremities but also his lower abdomen, including the catheter exit, were inserted into the negative pressure device. Subsequently, alternating negative pressure up to −70 mbar and atmospheric pressure was applied. Following the second IVT treatment session, the patient recognized leaking of clear dialysis fluids at the exit site while dwelling. Nevertheless, therapy was continued for two more sessions and leaking increased. The patient was not undressed for IVT and reliably reported no event of manual traction of the catheter during or after treatment. On arrival at our hospital his vital signs were normal and the abdomen was found to be tender, not painful and without clinical signs of inflammation. The dressing of the catheter was wet. Blood examinations showed no signs of inflammation. Assuming that IVT led to a reversible leakage of the tunnel, PD was paused for 4 days. After resuming dialysis, volumes were slowly titrated up from 500 to 1000 mL. When leakage recurred at the exit during dwelling with volumes exceeding 750 mL, a computed tomography scan with instillation of contrast media via catheter was performed. It revealed diffuse contrast media accumulation around the catheter. Moreover, a substantial amount of contrast media was detected in the subcutaneous and intermuscular layers on the right side, unrelated to the catheter and the tunnel. This enhancement correlated to former puncture sites of the laparoscopic trocars (Figure 1). Continuous ambulatory peritoneal dialysis (CAPD) had to be stopped and placement of a tunnelled central venous catheter became necessary for a transient switch to haemodialysis. After 6 weeks, a renewed attempt to resume CAPD failed, again due to leakage. Another CT scan after 3 months showed no contrast media accumulation in the right rectus abdominis, indicating that leaking ceased with termination of IVT. However, due to continuous leakage, the PD catheter had to be explanted. According to the surgical report, catheter material was found to be intact at the time of explantation.
Fig. 1.
(A and B) Computed tomography with contrast media intraperitoneally demonstrates leakage of contrast media outside the PD catheter (C) into the tissue (arrowhead). Moreover, contrast media is detected in the tissue at the old trocar puncture sites (arrows).
Discussion
In this report we present a case of PD malfunction following IVT in a patient who was stably performing PD. We hypothesize that IVT not only caused tunnel leakage but also led to diffuse leakage into the abdominal muscles through the former trocar puncture sites. To support the hypothesis, we argue that shear forces in cutaneous and subcutaneous tissue layers caused by alternating pressures led to a reopening of scarred tissue around the old trocar puncture sites.
This case report highlights the importance of carefully choosing patients eligible for IVT. The fact that our patient had to be switched to haemodialysis due to the catheter complication caused by IVT emphasizes the need to critically review usual practices with regard to special patient groups, such as CAPD patients. Devices that encompass the abdomen have to be avoided in these patients. In light of the increased utilization of IVT, our case, which demonstrates a severe complication, is intended to alert physicians to potential detrimental effects and important contraindications of this new method.
Conflict of interest statement
None declared.
References
- 1. Gregor S, Maegele M, Sauerland S. et al. Negative pressure wound therapy. Arch Surg 2008; 143: 189–196 [DOI] [PubMed] [Google Scholar]
- 2. Tevanov I, Enescu DM, Bălănescu R. et al. Negative pressure wound therapy (NPWT) to treat complex defect of the leg after electrical burn. Chirurgia (Bucur) 2016; 111: 175–179 [PubMed] [Google Scholar]
- 3. Sundby ØH, Høiseth LØ, Mathiesen I. et al. The effects of intermittent negative pressure on the lower extremities’ peripheral circulation and wound healing in four patients with lower limb ischemia and hard to heal leg ulcers: a case report. Physiol Rep 2016; 4: e12998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Campisi CC, Ryn M, Campisi CS. et al. Intermittent negative pressure therapy in the combined treatment of peripheral lymphedema. Lymphology 2015; 48: 197–204 [PubMed] [Google Scholar]
- 5. Ubbink DT, van der Oord BM, Sobotka MR, Jacobs MJ. Effekte der Vakuum-Kompressions-Behandlung auf die Hautmikrozirkulation von Patienten mit peripherer arterieller Verschlußkrankheit. Vasa 2000; 29: 53–5710731889 [Google Scholar]