Abstract
Background
This study was conducted to evaluate the performance of multislice computed tomography (MSCT) to diagnose high‐density thymic cysts and thymomas in lesions measuring < 3 cm.
Methods
The records of 42 patients admitted to Ningbo No. 2 Hospital with an anterior mediastinal mass (diameter < 3 cm) suspected of carcinoma originating from the thymus were retrospectively analyzed. All patients underwent surgery and pathological examination. Twenty‐eight were diagnosed with thymic cysts and 14 with thymoma. The features of thymic cysts and thymomas revealed on MSCT were compared.
Results
Mediastinal masses with a triangular or teardrop shape and a straight mediastina–lung border were more likely to be diagnosed as thymic cysts (P < 0.05), while those with a bulging nodule–lung border were more likely thymomas (P < 0.05). Using the CT value as a reference for differential diagnosis, the diagnostic sensitivity, specificity, and area under the receiver operating characteristic curve for CT values of non‐contrast CT images, enhanced CT values, and ΔCT values were 0.65 (0.47–0.84), 0.95(0.86–1.00), and 0.96 (0.89–1.00), respectively.
Conclusion
MSCT of high‐density thymus gland nodules (maximum diameter ≤ 3 cm) can reveal specific features that could be helpful for differential diagnosis.
Keywords: Differential diagnosis, MSCT, thymic cyst, thymoma
Introduction
Thymoma is the most common carcinoma of the anterior mediastinum.1, 2 With the application of advanced imaging techniques, such as multislice computed tomography (MSCT) and magnetic resonance imaging (MRI), clinical discovery and surgical resection has gradually increased over the past 20 years.3 About half of these early thymomas showed no clinical symptoms and were accidentally discovered when the patients were subjected to other unrelated examinations.4 In a study by Henschke et al., 77% of mediastinal tumors were identified in a group of individuals with high‐risk factors for lung cancer after a chest CT scan, 58% of whom were thymus‐derived, and postoperative pathology confirmed that a significant proportion of the thymic cysts were misdiagnosed as thymoma.5 Given a lack of understanding, misdiagnosis of benign thymic cysts as thymoma occasionally occurs.6, 7 Clinical misdiagnosis increases unnecessary surgical treatment and leads to related complications. In this retrospective study we collected the CT data of 42 patients with solid‐density thymic cysts and low‐risk thymoma confirmed by surgical pathology. The differences in CT findings were analyzed to improve the accuracy of preoperative diagnosis and to reduce unnecessary surgery.
Methods
General information of included patients
The records of 42 patients (25 male, 59.5%; 17 female, 40.5%) admitted to Ningbo No. 2 Hospital with anterior mediastinal masses (maximum diameter ≤ 3 cm) suspected of carcinoma originating from the thymus were retrospectively analyzed. All patients had undergone surgery and pathological examination. Twenty‐eight patients were diagnosed with thymic cyst and 14 with thymoma. The features of thymic cyst and thymoma were compared by MSCT. The median age of the patients was 54.07 ± 10.41 years (range: 26–72). The mediastinal mass was determined by chest computed tomography in 57.1% (24/42) of patients to diagnose respiratory symptoms, while the mass in the remaining patients was observed accidentally during physical examination. None of the patients exhibited any symptoms of myasthenia gravis, and complete imaging and clinicopathologic data were obtained.
Computed tomography (CT) scan
PHILIPS Brilliance 16‐layer helix CT (Philips Healthcare, Cleveland, OH, USA) and Siemens 64 dual‐source CT (Munich, Germany) were used for imaging. For supine position inspiration and breath‐hold scanning, the scan range spanned from the lung tip to the lung base (scanning layer thickness/layer spacing: 5/5 mm; tube voltage: 120 kV; tube current: 160 mA; and matrix: 512 × 512). A plain scan was initially conducted, followed by an enhanced scan (non‐ionic contrast agent, iopamidol at a dose of 1.5 mL/kg; bolus injection through the cubital vein with a high‐pressure syringe, 2.6–3.0 mL/s; at a two‐phase scan time window of 25–30 and 65–80 seconds) using a standard reconstruction algorithm and a layer thickness of 1 > 2 mm. The reconstructed thin‐layer data were applied for multiplanar reformation to observe lesion characteristics from multi‐angle and multidimensional perspectives, making the structure display of lesion characteristics and surrounding tissue more intuitive. CT image observation indexes include nodule boundary, shape, lung–mediastina border, plain scan CT value, and enhanced scan difference (ΔCT value). Two chief physicians used the double‐blind method to analyze the images and diagnose lesions. If the results were inconsistent, the results were negotiated and unified.
Statistical analysis
All data was analyzed using SPSS version 18.0 (SPSS Inc., Chicago, IL, USA). The measurement data were expressed with and comparison between groups was made based on the Student's t‐test of the sample mean (paired Student's t‐test for replicated data). The enumeration data were expressed with a relative number, and comparison between groups was made based on χ2 or Fisher's exact tests. The area under the receiver operating characteristic (ROC) curve was used to evaluate the feasibility of CT value for the differential diagnosis of thymic cysts and thymoma. P < 0.05 was considered to indicate a statistical difference.
Results
General characteristics of included patients
Of the 42 included patients, 28 (21 men, 7 women) were diagnosed with thymic cysts and 14 (4 men, 10 women) with thymoma after pathological examination. The mean ages of the thymic cyst and thymoma groups were 53.46 ± 10.85 and 55.29 ± 9.35, respectively, without any statistical difference (P > 0.05) (Table 1).
Table 1.
General patient characteristics
| Characteristics | Thymic cyst (n = 28) | Thymoma (n = 14) |
|---|---|---|
| Gender N (%) | ||
| Male | 21(75.0) | 4(28.6) |
| Female | 7(25.0) | 10(71.4) |
| Age (year) | 53.46 ± 10.85 | 55.29 ± 9.35 |
Imaging features
Mediastinal masses with a triangular or teardrop shape (Fig 1) and a straight mediastina–lung border were mostly likely to be diagnosed as thymic cysts (P < 0.05). Those with a bulging nodule–lung border were mostly likely thymomas (P < 0.05) (Fig 2, Table 2). Using the CT value as the differential diagnosis reference, the diagnostic sensitivity, specificity, and area under the receiver operating characteristic curve (AUC) for CT values of non‐contrast CT images, enhanced CT values, and ΔCT values were 0.65 (0.47–0.84), 0.95 (0.86–1.00), and 0.96 (0.89–1.00), respectively.
Figure 1.
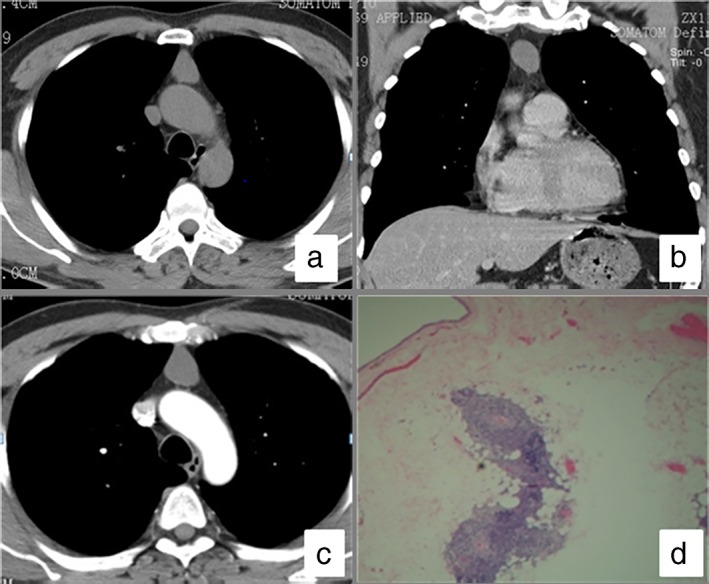
Computed tomography (CT) scan of a thymic cyst. (a) A plain CT scan of the chest demonstrated an anterior mediastinal node with a triangular shape; (b) coronal view of the chest demonstrated an ovate‐shaped node; (c) an enhanced CT scan demonstrated the node was not significantly enhanced; and (d) post surgery pathology showed a thymic cyst.
Figure 2.
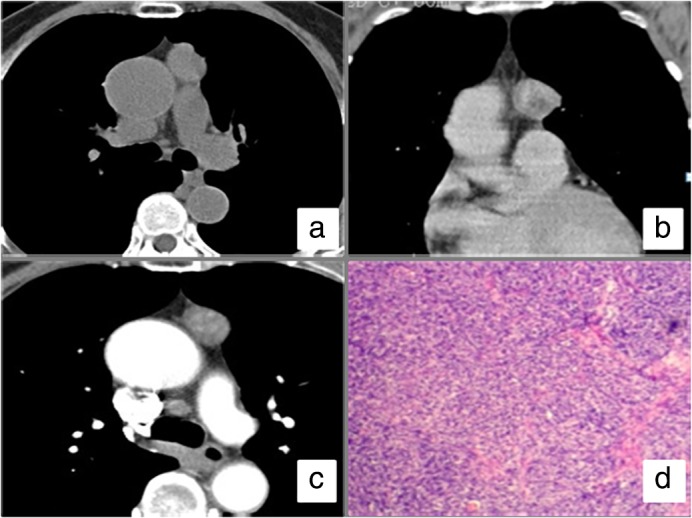
Computed tomography (CT) scan of a thymoma. (a) A plain CT scan of the chest demonstrated an irregular node located in the anterior mediastinum; (b) coronal view of the chest demonstrated an irregular node next to the aorta; (c) an enhanced CT scan showed the node was significantly enhanced compared to the plain CT scan; (d) post surgery pathology showed thymoma.
Table 2.
Thymic cyst and thymoma features on MSCT (n, %)
| Features | Thymic cysts (n = 28) | Thymoma (n = 14) |
|---|---|---|
| Lesion edge | ||
| Smooth | 28 (100.0) | 14 (100.0) |
| Unsmooth | 0 (0.0) | 0 (0.0) |
| Lesion shape | ||
| Round or oval | 16 (57.1) | 12 (85.7) |
| Trigonometric or teardrop shape | 9 (32.1) | 0 (0.0) |
| Irregular or lobulated | 3 (10.7) | 2 (14.3) |
| Relation to lung and mediastinum | ||
| Straight edge sign | 19 (67.9) | 2 (14.3) |
| Bulging | 0 (0.0) | 10 (71.4) |
| No contact | 9 (32.1) | 2 (14.3) |
MSCT, multislice computed tomography.
CT value of thymic cyst and thymoma in plain and enhanced scans
The average density of thymic cysts on plain scan (38.61 ± 15.01 Hu) was slightly lower than that of thymomas (41.92 ± 9.97 Hu), but the difference in CT values was not statistically significant (P > 0.05). After the enhanced scan, no significant enhancement of thymic cysts was observed (ΔCT value 1.91 ± 4.81 Hu), whereas thymomas showed significant enhancement (ΔCT value 32.22 ± 20.36 Hu), with partially enhanced heterogeneity (Table 3).
Table 3.
CT value to detect thymic cysts and thymoma
| CT value | Thymic cysts (n = 28) | Thymoma (n = 14) |
|---|---|---|
| Plain CT scan (Hu) | 38.61 ± 15.01 | 45.56 ± 4.88 |
| Enhance CT scan (Hu) | 40.52 ± 14.17 | 77.78 ± 19.78 |
| ΔCT value (Hu) | 1.91 ± 4.81 | 32.22 ± 20.36 |
CT, computed tomography.
Differential diagnostic performance of CT and ΔCT value
The differential diagnosis of thymic cysts and thymomas was determined by the difference between the CT values of non‐contrast CT images, enhanced CT values, and ΔCT values. The diagnostic sensitivity, specificity, and AUC are shown in Table 4 and Figure 3.
Table 4.
Differential diagnostic performance of CT and ΔCT value
| Diagnostic reference | Sensitivity | Specificity | AUC | Cutoff |
|---|---|---|---|---|
| Plain CT scan (Hu) | 88.89% (51.75–99.72%) | 60.87% (38.54–80.29%) | 0.65 (0.47–0.84) | 41.5 |
| Enhance CT scan (Hu) | 88.89% (51.75–99.72%) | 95.65% (78.05–99.89%) | 0.95 (0.86–1.00) | 60.50 |
| ΔCT value (Hu) | 77.78% (39.99–97.19%) | 100% (86.18–100%) | 0.96 (0.89–1.00) | 17.50 |
AUC, area under the receiver operating characteristic curve; CT, computed tomography.
Figure 3.
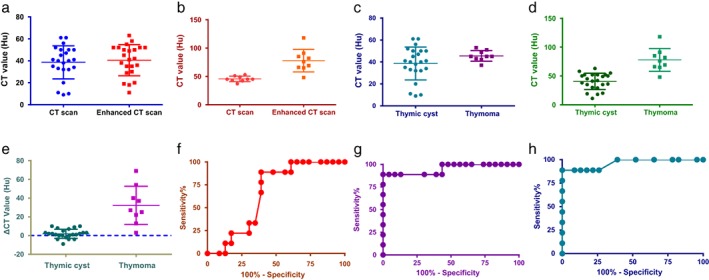
Scatter plots and receiver operating characteristic (ROC) curves of the value of computed tomography (CT) for the differential diagnosis of thymic cysts and thymomas. Scatter plots of plain and enhanced CT scans of (a) thymic cyst and (b) thymoma. Value of (c) plain CT, (d) enhanced CT, and (e) ΔCT to diagnose thymic cysts and thymomas. ROC curves of (f) plain CT, (g) enhanced CT, and (h) ΔCT value for the differential diagnosis of thymic cysts and thymomas.
Discussion
Previous literature has reported that thymoma is the most common space‐occupying lesion of the thymus and is often complicated by myasthenia gravis,2, 8, 9 whereas thymic cysts are rare, with an incidence rate of < 1% of mediastinal masses.10, 11 With the widespread use of MSCT, asymptomatic anterior mediastinal nodules with a diameter < 3 cm are more commonly detected, and thymic cysts account for a large proportion of these. Given the limitations of pathological examinations (e.g. a biopsy of the mass), imaging inspections, particularly CT examinations, are the most important basis for preoperative diagnosis.12 However, thymic cysts and thymoma are often incorrectly identified, causing patients to undergo unnecessary surgical treatment.13 The major reason for misdiagnosis is that thymic cysts have a greater density than cysts of general significance, that is, a measurement > 20 Hu, which is a solid density in the conventional definition, resulting in a false diagnosis of thymoma before surgery.
Thymic cystic disease can be congenital or postnatal.14 The capsules often contain a high level of protein, which can cause secondary bleeding. The higher protein level primarily accounts for the higher density of thymic cysts than simple fluid cysts. In the present study, there was no statistically significant difference between the CT values of thymic cysts and thymomas; therefore, the value of nodule density cannot be used as the basis for determining thymic cysts and tumors.
The features displayed via MSCT had good spatial and density resolution. The shape, edge, and surrounding tissues of nodules can be clearly and completely displayed with precision and reliability through thin‐layer reconstruction, providing important information for diagnosis.15 This study shows that thymic cysts and low‐risk thymomas with a maximum diameter of the anterior mediastinum of ≤ 3 cm possess smooth borders, indicating that they are more likely benign lesions. A considerable number of lesions are round and oval, but both types exhibit certain morphological differences. The thymic cyst, which is characterized by soft‐tissue density, retains the characteristics of cystic lesions. When thymic cysts grow on the mediastina–lung border, they are blocked by another relatively fixed mediastina–lung border, and the contact surface will show a straight edge appearance.16 When the contact surface is large, the whole shape appears as a triangle or a teardrop, and a sharp corner appears. This morphology shows that small cysts are thin and soft with tension but feature no high‐performance characteristics. The thymoma is a tumor originating from the thymic epithelial tissue with high tension and is expressed as a bulge when located in the mediastina–lung border. Thymomas reveal certain characteristics in the differential diagnosis of the two lesions.
However, the regular morphological features of the two lesions may overlap. It is often difficult to distinguish the morphology and density of high‐density small cysts and small thymomas in plain CT scans. Dynamic enhancement CT can reflect the hemodynamic characteristics of lesions. The pathophysiological characteristics of thymomas and thymic cysts completely differ. The observations in our patient sample showed a statistically significant difference between thymic cyst and thymoma (P < 0.05): thymic cysts were not substantially enhanced or only showed marginal enhancement, whereas thymomas presented a more uniform or uneven enhancement, consistent with the results of previous literature.17, 18, 19, 20
Our study sample included a larger proportion of male patients with thymic cysts, while the majority of patients with thymomas were women. However, relevant statistical reports in the literature are rare, and the significance of patient gender requires further observation and analysis.
This study had several limitations. The selected cases were thymic cysts and thymomas with solid density. Because of the low incidence of other tumor‐like lesions and the similar clinical treatment to thymic cysts, no other thymic tumor‐like lesions with solid density were included in the study. If no clinical symptoms are observed, follow‐up observations can be made. This study also only included low‐risk thymomas, excluding high‐risk ones.
In summary, sporadic anterior mediastinal nodules with a solid density that exhibit a triangular or teardrop shape or a straight‐edge appearance are easier to diagnose in terms of density and morphology, as such features are specific to thymic cysts. The identification of thymic cysts and low‐risk thymoma remains difficult; thus, routine enhancement scans should be used to reduce instances of misdiagnosis. If a diagnosis of thymic cyst can be confirmed before surgery, unnecessary surgery and injury can be avoided.
Disclosure
No authors report any conflict of interest.
References
- 1. Qu L, Xiong Y, Yao Q, Zhang B, Li T. Micronodular thymoma with lymphoid stroma: Two cases, one in a multilocular thymic cyst, and literature review. Thorac Cancer 2017; 8: 734–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Engels EA. Epidemiology of thymoma and associated malignancies. J Thorac Oncol 2010; 5 (10 Suppl 4): S260–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tan A, Holdener GP, Hecht A, Gelfand C, Baker B. Malignant thymoma in an ectopic thymus: CT appearance. J Comput Assist Tomogr 1991; 15: 842–4. [DOI] [PubMed] [Google Scholar]
- 4. Scorsetti M, Leo F, Trama A et al Thymoma and thymic carcinomas. Crit Rev Oncol Hematol 2016; 99: 332–50. [DOI] [PubMed] [Google Scholar]
- 5. Henschke CI, Lee IJ, Wu N et al CT screening for lung cancer: Prevalence and incidence of mediastinal masses. Radiology 2006; 239: 586–90. [DOI] [PubMed] [Google Scholar]
- 6. Singh G, Rumende CM, Amin Z. Thymoma: Diagnosis and treatment. Acta Med Indones 2011; 43: 74–8. [PubMed] [Google Scholar]
- 7. Suster S. Diagnosis of thymoma. J Clin Pathol 2006; 59: 1238–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Carter BW, Benveniste MF, Truong MT, Marom EM. State of the art: MR imaging of thymoma. Magn Reson Imaging Clin N Am 2015; 23: 165–77. [DOI] [PubMed] [Google Scholar]
- 9. Detterbeck FC, Zeeshan A. Thymoma: Current diagnosis and treatment. Chin Med J (Engl) 2013; 126: 2186–91. [PubMed] [Google Scholar]
- 10. Marom EM. Advances in thymoma imaging. J Thorac Imaging 2013; 28: 69–80. [DOI] [PubMed] [Google Scholar]
- 11. Brown LR, Aughenbaugh GL. Masses of the anterior mediastinum: CT and MR imaging. AJR Am J Roentgenol 1991; 157: 1171–80. [DOI] [PubMed] [Google Scholar]
- 12. Scagliori E, Evangelista L, Panunzio A et al Conflicting or complementary role of computed tomography (CT) and positron emission tomography (PET)/CT in the assessment of thymic cancer and thymoma: Our experience and literature review. Thorac Cancer 2015; 6: 433–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bruyère PJ, Moreau P, Ghaye B. Congenital thymic cyst. JBR‐BTR 2007; 90: 178–9. [PubMed] [Google Scholar]
- 14. Davis JW, Florendo FT. Symptomatic mediastinal thymic cysts. Ann Thorac Surg 1988; 46: 693–4. [DOI] [PubMed] [Google Scholar]
- 15. Priola AM, Priola SM, Gned D, Giraudo MT, Fornari A, Veltri A. Comparison of CT and chemical‐shift MRI for differentiating thymoma from non‐thymomatous conditions in myasthenia gravis: Value of qualitative and quantitative assessment. Clin Radiol 2016; 71: e157–69. [DOI] [PubMed] [Google Scholar]
- 16. Burton EM, Mercado‐Deane MG, Howell CG et al Cervical thymic cysts: CT appearance of two cases including a persistent thymopharyngeal duct cyst. Pediatr Radiol 1995; 25: 363–5. [DOI] [PubMed] [Google Scholar]
- 17. Yuhua W. [CT diagnosis of primary mediastinal tumors]. J Pract Radio 2001; 17: 92–4 (In Chinese.) [Google Scholar]
- 18. Matsumoto T, Shimabukuro M, Okita I et al [CT findings of malignant lymphoma of the anterior mediastinum‐‐differentiation from invasive thymoma]. Nihon Igaku Hoshasen Gakkai Zasshi 1989; 49: 414–22 (In Japanese.) [PubMed] [Google Scholar]
- 19. Sone S, Higashihara T, Morimoto S et al [CT of thymoma]. Nihon Igaku Hoshasen Gakkai Zasshi 1982; 42: 731–9 (In Japanese.). [PubMed] [Google Scholar]
- 20. Moore AV, Korobkin M, Powers B et al Thymoma detection by mediastinal CT: Patient with myasthenia gravis. AJR Am J Roentgenol 1982; 138: 217–22. [DOI] [PubMed] [Google Scholar]


