Abstract
Background:
Paralleling the growth of bariatric surgery, the demand for post-bariatric body-contouring surgery is increasing. Weight loss is the main cause, although not the only one, that drives patients to arm lift surgery. Several surgical techniques have been proposed over the years. Our aim was to consider the complications and outcomes according to the performed technique, through a wide review of the literature.
Methods:
A search on PubMed/Medline was performed using “brachioplasty”, “upper arm lifting”, and “techniques” as key words. Embase, Medline (OvidSP), Web of Science, Scopus, PubMed publisher, Cochrane, and Google Scholar were searched as well. As inclusion criteria, we selected the clinical studies describing techniques of brachioplasty. We excluded the papers in which complications related to brachioplasty were not specified. We also excluded literature-review articles.
Results:
We found 27 studies from 1995 to 2015. Overall, 1065 patients were treated. Different techniques were applied. Complications were observed in 308/1065 patients (28.9%). The most frequent complications were hypertrophic scarring, seroma and hematoma. Surgical revision rate ranged from 0 to 21 percent. Nerve damage occurred in a modest percentage of patients (16/1065, 1.5%). No major complications, such as thromboembolism and sepsis, were observed.
Conclusions:
Brachioplasty is a safe surgical procedure. All the brachioplasty techniques showed positive outcomes, in term of patients’ satisfaction and clinical results. Nevertheless, minor complications occurred in a high percentage of patients, regardless the performed surgical procedure. Patients should be informed about the possible formation of hypertrophic scars and nerve injuries. (www.actabiomedica.it)
Keywords: arm lifting, body contouring surgery, brachioplasty, upper arm deformities
Introduction
Arm lift surgery was born to correct aesthetic deformity of the arm. Patients that seek arm-lift procedures are particularly distressed due to the large segment of ‘bat-wing-like’ lax tissue extending on the upper arm (Fig. 1-2). The request for brachioplasty has increased in recent years, mainly because of the growing number of bariatric procedures. Brachioplasty is often performed within 2-3 years after the execution of a bariatric surgery, which resulted in a significant weight loss. Other causes are senile elastosis (Fig. 3) and massive weight loss due to diet and exercise. El Khattib, in 2007, proposed a classification system of the contour deformity of the arm, based on the amount of lipodystrophy and degree of ptosis (measuring the vertical distance between the brachial sulcus and the inferior curve of the arm). Five stages of brachial ptosis were established (1).
Figure 1.
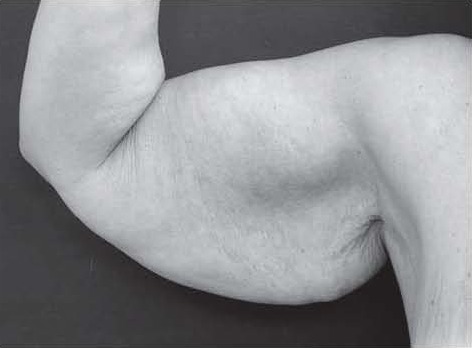
Typical ‘bat wing’ deformity of the upper arm
Figure 2.

Typical ‘bat wing’ deformity of the upper arm
Figure 3.

Deformity of the upper arm due to senile elastosis
Brachioplasty, as a global term, should deal with all of these types of deformities in addition to the surgically induced massive weight loss patients, as all are categories of arm contour deformities. Brachioplasty was first described in 1930, by Thorek (2). Techniques have evolved over time to address changing needs of the patient population (table 1). Modifications based upon individual patient needs are necessary and must be applied carefully to ensure a good result.
Table 1.
Developments in brachioplasty techniques
| Author | Year | Technique |
|---|---|---|
| Thorek(2) | 1930 | Described as a form of pendulous arm reduction for obese women |
| Posse (4) | 1943 | Elliptical incision |
| Correa-Iturraspe and Fernandez (5) | 1954 | First description of aesthetic brachioplasty |
| Pitanguy (6) | 1975 | S-shaped incision |
| Franco and Rebello (7) | 1977 | L-shaped incision |
| Guerrero-Santos J (8) | 1979 | Lenticular excision |
| Juri(9) | 1979 | Quadrangular flap and T-closure |
| Borges (10) | 1982 | W-plasty incision |
| Regnault (11) | 1983 | Axilloplasty |
| Goddio (12) | 1989 | Deepithelialization of the posterior flap, repositioned to create a bicipital sulcus |
| Lockwood (13) | 1995 | Suspension of the fascial system |
| Marques (14) | 1996 | Treatment of brachial, axillary, and elbow segments |
| Gilliland (15) | 1997 | Circumferential para-axillary superficial tumescent (CAST) liposuction |
| de Souza Pinto (16) | 2000 | Brachioplasty technique with the use of molds (S-shaped) |
| Richiards (17) | 2001 | Minimal-incision brachioplasty |
| Strauch (18) | 2004 | Sinusoidal incision |
| Chandawarkar (19) | 2006 | Fish-incision |
| Aly (20) | 2006 | Double ellipse |
| Hurwitz (21) | 2006 | Inverted L-shaped |
| Aly (22) | 2006 | T-type brachioplasty |
| Aboul Wafa (23) | 2013 | S-shaped |
| Bracaglia (24) | 2013 | “Kris Knife” brachioplasty |
| Knotts (25) | 2014 | Avulsion brachioplasty |
| Fantozzi (26) | 2014 | Brachial lifting using the balanced triple-vector (BTV) technique with dual opposing flaps |
| Kornstein (27) | 2014 | Silk-derived surgical scaffold (SERI) as an adjunct to conventional brachioplasty |
| Ferraro (28) | 2015 | Modified fish-incision |
Complications that can occur after brachioplasty include small wound separations, dehiscence (Fig. 4), seroma, lymphocele/lymphedema, inability to close the arm, bad scarring (Fig. 5), infection, bleeding, nerve compression/compartment syndrome, neuromas, and sensory loss.
Figure 4.

Proximal wound dehiscence after brachioplasty
Figure 5.

Wide and hypertrophic scar after brachioplasty
A recent review showed that brachioplasty is associated with significant complication (25 to 40 percent) and revision rates (3 to 25 percent) (3).
The aim of this paper was to perform a review of the available literature on surgical techniques, with particular attention to the complications occurred.
Materials and methods
In order to verify the complications of brachioplasty techniques, we selected the studies dealing with the use of this kind of surgery for the treatment of excessive amount of soft tissue and skin.
A literature search of the PubMed database was performed using the key words ‘’brachioplasty”, ‘’upper arm lifting”, ‘’technique”. Embase, Medline (OvidSP), Web of Science, Scopus, PubMed publisher, Cochrane, and Google Scholar were searched as well. Additional articles were selected reviewing the references of the papers identified using this key words.
Inclusion criteria among these papers were:
paper is a case study, case report, clinical trial, open label prospective study, case series, retrospective study
brachioplasty is used as a surgical therapy
complication rates related to the brachioplasty can be delineated
Exclusion criteria were:
paper doesn’t treat brachioplasty under a surgical point of view
paper is a review of literature
The entire databases were considered, without restrictions of time. Both English and not-English language papers were included. Each article was tabulated as follows: authors, year of the study, number of patients, location, demographic data, surgical technique, follow-up time and complications.
All kind of brachioplasty techniques were considered. We included patients regardless of the cause that prompted the patient to this surgical procedure; not only post-bariatric patients were included.
The publications were manually screened and reviewed to identify reports for brachioplasty techniques. Three investigators independently reviewed and extracted data from the papers according to the predetermined criteria.
Results
We identified 93 full-text articles; 66 did not meet inclusion criteria, leaving 27 studies available from 1995 to 2015 (Fig. 6, table 2).
Figure 6.
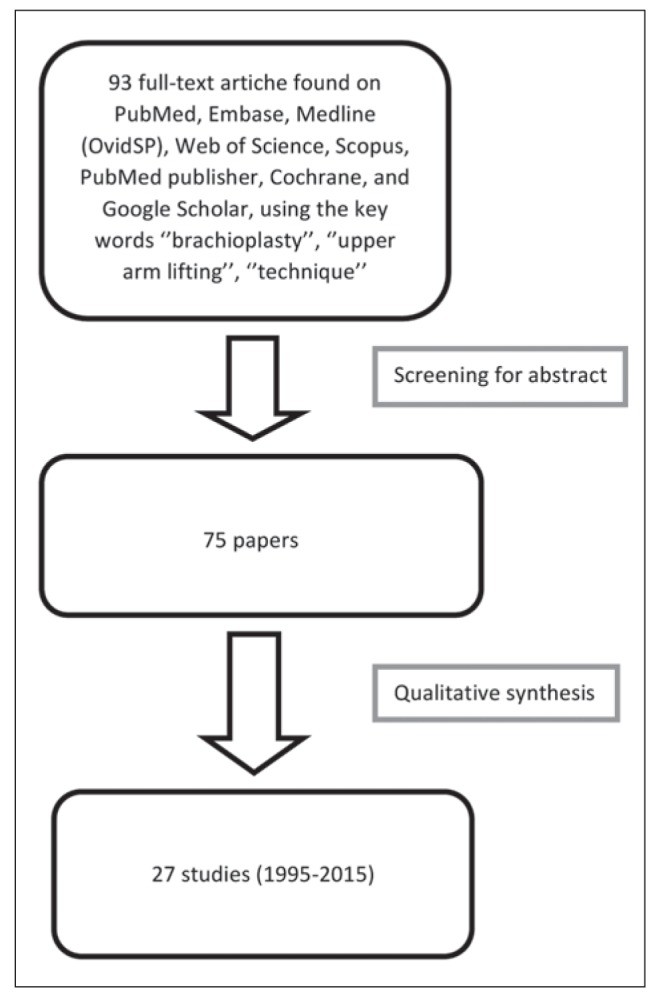
Flow-chart of the studies’ selection
Table 2.
Overview of studies on brachioplasty
| Author, year | No. Pts | Location | Demographic data | Brachioplasty surgical technique | Follow-up | Complications (pt=patient; pts=patients) |
|---|---|---|---|---|---|---|
| Lockwood T, 1995 (13) | 5 | USA | Not specified | Fascial anchoring | 6-12 months (average: 8 months) | Under-resection (1 pt) Small distal seroma (1 pt) |
| De Souza Pinto EB, 2000(16) | 20 | Brazil | Female (40-60 years) | S-shape (with or without liposuction) | 24 months | Hypertrophic scarring (2 pts) |
| Richiards ME, 2001 (17) | 9 | USA | Female (25-75 years) | Minimal-incision brachioplasty | Not specified | Skin wrinkling (1 pt) |
| Pascal JF, 2005 (37) | 21 | France | Not specified | Single ellipse with liposuction (resection only of the skin layer) | Not specified | None |
| Hurwitz DJ, 2006 (21) | 24 | USA | Female | Inverted L-shaped | 6-28 months | Delayed healing at the tip of the triangular flap due in part to pressure from elastic sleeves (3 pts) Seroma near the elbow responded to multiple aspirations (4 pts) Hypertrophic scar (1 pt) |
| Knoetgen J 3rd, 2006(38) | 40 | USA | Female Average age: 47 years (20-61 years) | Resection of medial upper arm skin and subcutaneous fat, placing the scar in the intermuscular septum. (7.5% of pts had simultaneous arm liposuction) | Average 50 months | The overall complication rate was 25%. Seroma (4 pts) Hypertrophic scar (4 pts) Cellulitis (3 pts) Wound dehiscence (3 pts) Subcutaneous abscess (1 pt) Medial antebrachial cutaneous nerve injury (1 pt) Medial antebrachial cutaneous nerve injury (1 pt) |
| Cannistra C, 2007 (34) | 50 | France | 25-60 years | It was applied an algorithm for marking a surgical plane to avoid postoperative arm asymmetry and to reduce surgical complications | 12 months | Large scars (20% of pts) |
| Wolf AM, 2007 (31) | 7 | Germany | Female | T-type brachioplasty | Not specified | In one patient, a neurolysis of the ulnar nerve became necessary due to postoperative edema |
| El Khatib HA, 2007 (1) | 60 | Qatar | 24-56 years | 7 pts (stage 1 brachial ptosis): circumferential liposuction 13 pts (stage 2a brachial ptosis): staged circumferential liposuction 12 pts (stage 2b brachial ptosis): liposuction of the lower posterior and medial arm assisted short longitudinal scar brachioplasty 17 pts (stage 3 brachial ptosis): liposuction of the lower posterior and medial arm assisted short longitudinal scar brachioplasty 11 pts (stage 4 brachial ptosis): traditional brachioplasty |
12-38 months | None Postoperative brachial ptosis (1 pt) None Hypertrophic scar (1 pt) Distal edema (1 pt) Postoperative skin laxity in the axillary region (2 pts) Distal edema (1 pt) |
| Gusenoff JA, 2008 (39) | 101 | USA | 97 female, 4 male. 45110.1 years | Brachioplasty (inverted L-shaped) alone or in combination with other procedures | 6 months - 2 years | 36 pts had complications related to their arms Seroma (24 pts) Dehiscence (9 pts) Infection (3 pts) |
| Migliori FC, 2009 (36) | 29 | Italy | Female Average age 41 (35-48 years) | Personal technique based on a careful preoperative evaluation and markings, followed by an intraoperative skillful handling | 6-36 months | Scar Hypertrophies/keloids (12 pts) Edema (4 pts) Seroma (3 pts) Section of cutaneous branches of the anterior medial brachial nerve (2 pts) Ulnar nerve compression (1 pt) Wound dehiscence (1 pt) |
| SymbasJD, 2010 133) | 31 | USA | Not specified | Inverted L-shaped (16 pts) and double ellipse (15 pts) | 2-42 months (average: 16 months) | Hematoma (2 pts) Lymphocele (2 pts) Revisions: dog ears (2 pts) Cellulitis (1 pt) Infection (1 pt) Delayed healing (1 pt) scar contracture (1 pt) Scarring (1 pt) Re-excision (1 pt) |
| Nguyen AT, 2010 140) | 21 | USA | 35-59 years | Posterior Brachioplasty Liposuction-Assisted (elliptical incision) | 3 months - 3 years | Small wound dehiscence (2 pts) Slightly hypertrophic scar (1 pt) |
| Modolln ML, 2011 130) | 18 | Brazil | 49.2±11.3 years | Fish-incision 19 and, in cases of excess skin extending to the lateral chest wall, the skin fragment excision was prolonged towards that direction, with the aid of a Z-plasty | 6 months | Seroma (1 pt) Damage to the medial cutaneous nerve of the forearm (1 pt) Scar imperfection (1 pt) |
| Aboul Wafa AM, 2013(23) | 18 | Egypt | Female | S-shaped | 3-24 months (average: 11 months) | Seroma (1 pt) Scar hypertrophy (1 pt) Contour irregularities (1 pt) |
| Bossert RP, 2013 135) | 144 | USA | 139 female, 5 male | Sixty-four patients had concomitant arm liposuction at the time of brachioplasty. The remaining 80 patients underwent excisional brachioplasty alone | 6-24 months | Overall complication rate: 46%. No significant differences in complication rates were seen between the liposuction and excision-alone cohorts for seroma (19.1 percent versus 23.1 percent), wound dehiscence (7.9 percent versus 2.6 percent), infection (4.8 percent versus 6.4 percent), hematoma (3.2 percent versus 0 percent), or lymphedema (3.2 percent versus 1.3 percent). Revision rates were similar between the two groups (9.5 percent with liposuction and 8.9 percent without liposuction) |
| Bracaglia R, 2013 (24) | 41 | Italy | Female Mean age: 47 years (39 ± 10 years) | "Kris knife" technique (because of the incision similarity to the wavy blade of the Asian dagger kris) | 36 months | Delayed healing (4 pts) Seroma (1 pt) Hypertrophic scarring (2 pts) |
| Elkhatib H, 2013 (41) | 205 | Qatar | 21-66 years | Posterior Scar Brachioplasty with Fascial Suspension | 29-98 months | Hypertrophied scar (5 pts) Postoperative distal edema (3 pts) Dysesthesia due to skin tightness (1 pt) |
| Zomerlei TA, 2013 (42) | 96 | USA | 95 female, 1 male Average age: 51 years (26.5-76.5 years) | Single ellipse (75 pts) Fish mouth (14 pts) l-pattern (5 pts) Z-plasty (2 pts) | Not specified | Total complication rate was 53.1% (51 pts) Hypertrophic scarring (23 pts) Seroma (6 pts) Dehiscence (6 pts) Hematoma (2 pts) Stitch abscess (5 pts) Infection (14 pts) Revision (12 pts, 12.5%) |
| Fantozzi F, 2014 (26) | 23 | Italy | 20 female, 3 males Median age: 55.4 years (36-77 years) | Brachial lifting using the balanced triple-vector (BTV) technique with dual opposing flaps | At least 20 months | Temporary paraesthesia (5 pts) Temporary loss of sensation (2 pts) Temporary swelling of hands (2 pts) Seroma (1 pt) Scar revision procedures (2 pts) Patient unsatisfied with final scar quality (1 pt) |
| Kornstein AN, 2014 (27) | 1 | USA | 46-years-old female | Silk-derived surgical scaffold (SERI) as an adjunct to conventional brachioplasty | 6 months | None |
| Hurwitz D, 2014 (32) | 1 | USA | 33-years-old female | Inverted L-shaped | 3 months | Dehiscence (2 cm, along the apex of the right axillary closure) |
| Knotts CD, 2014 (25) | 44 | USA | Female Average age 53 years (33-75 years) | Avulsion brachioplasty | average: 446 days | Wound dehiscence (14 pts) Seroma (1 pt) Widened/hypertrophic scar (9 pts) |
| Han HH, 2014 (29) | 1 | Korea | 31-years-old female | Traditional brachioplasty (single ellipse) | Not specified | None |
| de Runz A, 2015 (43) | 24 | France | Mean age: 44.4 years | Liposuction-assisted medial brachioplasty (single ellipse) | There were 10 patients (41.7 percent) with at least one complication Revision scar (1 pt) Paraesthesia (1 pt) Second operation for scar correction (4 pts) Under-resection (2 pts) Wound dehiscence (3 pts) Bad scarring (hypertrophy/widening) (6 pts) |
|
| Ferraro GA, 2015 (28) | 30 | Italy | Female Average age: 51 years (45-58 years) | Modified fish-incision | 1 year | None |
| Thawani SP, 2015 (44) | 1 | USA | 49-years-old female | Liposuction and brachioplasty | 10 months | Significant right partial proximal median neuropathy Mild right ulnar neuropathy Left medial antebrachial cutaneous nerve neuropathy |
Four were case reports and 23 were retrospective studies. Overall, 1065 patients (age: 24-77 years) were treated in the 27 studies. Different surgical techniques were used for brachioplasty: traditional brachioplasty (elliptical incision) (29), Kris Knife technique (24), brachial lifting using the balanced triple-vector technique with dual opposing flaps (26), fish-incision brachioplasty (30), T-brachioplasty (31), L-brachioplasty (21,32,33), S-brachioplasty (16,23) and personal techniques. Follow-up ranged from two to 36 months. Pooling the data, complications were observed in 308/1065 patients (28.9%). The most frequent complications are summarized in table 3. They were: hypertrophic scarring (115 patients, 10.79%) (1,16,21,23-26,30,34), seroma and lymphocele (74 patients, 6.94%) (13,21,23-26,30,35,36), delayed healing (21,24,33) and wound dehiscence (25,32,35) (61 patients, 5.72%), infection (34 patients, 3.19%), hematoma (8 patients, 0.75%). Nerve damage, proven by electromyography or clinical signs that lasted at least one year, occurred in 16/1065 patients (1.5%).
Table 3.
Complications associated with brachioplasty, obtained through the analysis of 27 clinical studies
| Complication | No of patients | Complications’ rate |
|---|---|---|
| Hypertrophic scarring | 115/1065 | 10.79% |
| Seroma/lymphedema | 74/1065 | 6.94% |
| Delayed healing/wound dehiscence | 61/1065 | 5.72% |
| Infection | 34/1065 | 3.19% |
| Nerve damage | 16/1065 | 1.5% |
| Hematoma | 8/1065 | 0.75% |
| Total | 308/1065 | 28.9% |
In all these studies, the surgical revision rate ranged from zero to 21 percent, with residual contour deformity and hypertrophic scarring representing the most common causes for revision.
No significant differences in complication rates were seen between the liposuction and excision-alone cohorts.
Discussion
Brachioplasty is one of the most commonly performed BCS. This surgical procedure requires a careful preoperative design that takes into account the extent of the arm deformity. Particularly close attention should be paid to the anatomical structures to be preserved (45-48); dissection surgery must be made paying greater attention to the muscular fascia of the upper arm and to the medial antebrachial cutaneous nerve which pierces the deep fascia to become subcutaneous in the distal or mid brachium and may include anatomical variants (38,44).
In the present review, an overall complication rate of 28.9 % and a surgical revision rate ranging from 0 to 21 % were observed. Any major complication, such as thromboembolic events or sepsis, were reported.
In some cases patients had temporary paresthesia, probably due to damage to the medial cutaneous nerve of the forearm by electrocautery (34,40,45). The paresthesia resolved naturally after some weeks in all patients; in one case (31), a neurolysis of the ulnar nerve became necessary because of the post-operative edema.
Liposuction was performed to reduce the volume without damaging lymphatics, other vessels, and nerves, and to give better tissue mobilization. It did not increase the risk of post-operative complications and does not significantly modify the outcome, in accordance with the literature data (35,42).
Knoetgen, in 2006, reported nerve injury in 2/40 (5%) patients (38). In both cases, medial antebrachial cutaneous nerve was damaged. They developed, respectively, paresthesia and complex regional pain syndrome type II. Treatment was hand therapy and gabapentin, with improvement-resolution of symptoms after 12 months.
Thawani et al. (44) recently reported a case of a 49-year-old female patient that developed multiple nerve injuries related to brachioplasty, including a significant right partial proximal median neuropathy, mild right ulnar neuropathy, and left medial antebrachial cutaneous nerve neuropathy. After 10 months, she had improved but persistent symptoms.
Knotts et al. (25), in 2014, reported the highest revision rate (21%) and a complication rate of 50%, using a single technique (avulsion brachioplasty) on 44 patients: wound dehiscence (14 patients) and hypertrophic scar (9 patients) were the reported complications.
Zomerlei et al. (42), in 2013, reported the highest complication rate (53.1%), reviewing the records of 96 patients who underwent a brachioplasty procedure from a multipractice medical center. The surgical technique performed were single ellipse (75 pts), fish mouth (14 pts), L-pattern (five pts), Z-plasty (two pts). The most common complication was hypertrophic scarring (23 pts, 24%).
Further analysis of the studies showed many critical points. Firstly, most of the studies took into account a small number of patients with a high variability (from 1 to 205 patients). Only nine collected studies took into account more than 40 patients. Seven studies considered less than 10 patients. The postoperative follow-up was not specified in six studies. The follow-up time was not homogeneous among the different studies. Only in 13/27 studies it was greater than 12 months. In most of the articles, comorbidities of patients were not taken into account.
Three studies (11,1 %) did not report any type of demographic data; in the remaining 24 papers: 4 (14,8%) reported only the gender; 14 (51,85 %) reported the gender and the age of patients; 6 (22,2 %) reported only the age. No study showed the race of the patients nor the presence of comorbidities (connective tissue diseases, diabetes, smoking, obesity) or pharmacological treatments that could affect wound healing. The most important critical issue emerging from the review is represented by the extreme variability in surgical techniques and especially the type of incision used. It was not possible to identify a statistically significant correlation between technique and complication rate. Each author in fact described the use of his personal surgical technique and clinical results, without uniformity. Five authors (18.5%) used personal techniques or significant modifications of existing techniques, 11 authors (40.7%) used the single ellipse incision. Two authors used the posterior scar brachioplasty, 2 s-shaped , 2 L-shaped, 1 minimal - incision brachioplasty, 2 fish incision, two studies took into account the use of multiple techniques (Symbas (33): inverted L-shaped and double ellipse; Zomerlei (42): single ellipse, fish, L-shaped, Z-plasty).
Scar location is a strongly debated point. Some surgeons prefer to place the suture line posterior to the medial bicipital groove to hide the scar on the frontal view. Other surgeons prefer to place it in the bicipital groove. A recent survey evaluation showed that the medially based straight scar is the most aesthetically acceptable option when performing a brachioplasty (49).
The main limits of this analysis were the high heterogeneity of the study populations. Selection bias and lack of common outcome measures were some of the problems that prevented a proper meta-analysis. Although this review is not a meta-analysis, we critically assessed the literature and tried to identify high-quality studies. Moreover, many of the technique papers showing favorable results are biased from authors promoting their preferred techniques.
Sixty-six papers were not included in the review because they did not respect the inclusion criteria. However, in the articles included, the BMI of patients was not always specified and we do not know if the brachioplasty was performed in post-bariatric patients or for aesthetic purpose. This is a limitation of our work because we cannot perceive the importance of the scar.
Furthermore, there was not an evaluation of the scar with questionnaire or similar. This is important because the aesthetic result of a scar in obese patients is very different respect patient who undergoes cosmetic surgery. The lack of information on the type of patients did not allow us to clearly correlate some complications, such as surgical wound diastases: such events certainly occur more often in people with diabetes or vascular disease, but this information are not expressed in some analyzed works.
The percentage of seroma is not related to the BMI of patients in all the analyzed papers and this is another limitation of the review: seroma appears more frequently in patients with high BMI. Finally, the bleeding is not carefully evaluated in all the papers, as they does not specify whether there was an important bleeding diathesis treated with transfusions or it was just a localized and self-limited hematoma.
The presence of comorbidities should always be highlighted, as these can affect the results and the development of postoperative complications.
Conclusions
There is no definitive best method of brachioplasty. The multiplicity of the performed techniques reveal lack of consensus. Therefore, the surgical approach will depend on the extent and the degree of arm lipodystrophy, the extent of skin laxity, and the amount of excess fat deposits such that there is no universal technique. Minor complications occurred in a high percentage of patients, regardless the performed surgical procedure. The most frequent complication of the procedure is undesirable, visible scarring (Fig. 3). This complication is not due either to poor pre-surgical planning by the physician nor the surgical technique used, but depend on the extent of deformity and personal skin regenerative capacity of each patient.
Nerve injury can occur during skin and fat resection. To avoid this damage, the surgeon should pay close attention to respect the deep fascia of the upper arm and the medial antebrachial cutaneous nerve.
Most of the studies considered a small number of patients, and there were often absent or partial information about demographics, comorbidities and pharmacological treatment in progress. There was extreme variability of the techniques and the type of incision used. The follow-up time was not homogeneous and in some cases absent. The heterogeneity of techniques and the lack of data in the scientific literature do not allow scientifically correct conclusions. The literature’s data appear to be strongly inhomogeneous and cannot be uniformly assessed.
References
- 1.El Khatib HA. Classification of brachial ptosis: strategy for treatment. Plastic and reconstructive surgery. 2007;119:1337–42. doi: 10.1097/01.prs.0000254796.40226.92. [DOI] [PubMed] [Google Scholar]
- 2.Thorek M. Esthetic surgery of the pendulous breast, abdomen and arms in females. Illinois Medical Journal. 1930;3:48–57. [Google Scholar]
- 3.Shermak MA. Aesthetic refinements in body contouring in the massive weight loss patient: Part 2. Arms. Plastic and reconstructive surgery. 2014;134:726e–35e. doi: 10.1097/PRS.0000000000000627. [DOI] [PubMed] [Google Scholar]
- 4.Posse P. Buenos Aires: Athenue; 1943. Cirurgia Estetica. [Google Scholar]
- 5.Correa-Iturraspe M FJ. Dermatolipectomia braquial. Prensa Med Argent. 1954:2432. [PubMed] [Google Scholar]
- 6.Pitanguy I. Abdominal lipectomy. Clinics in plastic surgery. 1975;2:401–10. [PubMed] [Google Scholar]
- 7.Franco T. Rio De Janeiro: Atenueu; 1977. Cirurgia Estetica. [Google Scholar]
- 8.Guerrero-Santos J. Brachioplasty. Aesthetic plastic surgery. 1979;3:1–14. doi: 10.1007/BF01577832. [DOI] [PubMed] [Google Scholar]
- 9.Juri J, Juri C, Elias JC. Arm dermolipectomy with a quadrangular flap and “T” closure. Plastic and reconstructive surgery. 1979;64:521–5. doi: 10.1097/00006534-197910000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Borges AF. W-plastic dermolipectomy to correct “bat-wing” deformity. Annals of plastic surgery. 1982;9:498–501. [PubMed] [Google Scholar]
- 11.Regnault P. Brachioplasty, axilloplasty, and pre-axilloplasty. Aesthetic plastic surgery. 1983;7:31–6. doi: 10.1007/BF01570533. [DOI] [PubMed] [Google Scholar]
- 12.Goddio AS. A new technique for brachioplasty. Plastic and reconstructive surgery. 1989;84:85–91. doi: 10.1097/00006534-198907000-00016. [DOI] [PubMed] [Google Scholar]
- 13.Lockwood T. Brachioplasty with superficial fascial system suspension. Plastic and reconstructive surgery. 1995;96:912–20. doi: 10.1097/00006534-199509001-00022. [DOI] [PubMed] [Google Scholar]
- 14.Marques B AA. Dermolipectomia braquial. Rev Soc Bras Cir Est Reconst. 1996;11 [Google Scholar]
- 15.Gilliland MD, Lyos AT. CAST liposuction: an alternative to brachioplasty. Aesthetic plastic surgery. 1997;21:398–402. doi: 10.1007/s002669900144. [DOI] [PubMed] [Google Scholar]
- 16.de Souza Pinto EB, Erazo PJ, Matsuda CA, et al. Brachioplasty technique with the use of molds. Plastic and reconstructive surgery. 2000;105:1854–60. doi: 10.1097/00006534-200004050-00037. discussion 61-5. [DOI] [PubMed] [Google Scholar]
- 17.Richards ME. Minimal-incision brachioplasty: a first-choice option in arm reduction surgery. Aesthetic surgery journal / the American Society for Aesthetic Plastic surgery. 2001;21:301–10. doi: 10.1067/maj.2001.117695. [DOI] [PubMed] [Google Scholar]
- 18.Strauch B, Greenspun D, Levine J, Baum T. A technique of brachioplasty. Plastic and reconstructive surgery. 2004;113:1044–8. doi: 10.1097/01.prs.0000105648.54174.11. discussion 9. [DOI] [PubMed] [Google Scholar]
- 19.Chandawarkar RY, Lewis JM. ‘Fish-incision’ brachioplasty. Journal of plastic, reconstructive & aesthetic surgery: JPRAS. 2006;59:521–5. doi: 10.1016/j.bjps.2005.04.035. [DOI] [PubMed] [Google Scholar]
- 20.Aly A, Pace D, Cram A. Brachioplasty in the patient with massive weight loss. Aesthetic surgery journal/the American Society for Aesthetic Plastic surgery. 2006;26:76–84. doi: 10.1016/j.asj.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 21.Hurwitz DJ, Holland SW. The L brachioplasty: an innovative approach to correct excess tissue of the upper arm, axilla, and lateral chest. Plast Reconstr Surg. 2006;117:40311. doi: 10.1097/01.prs.0000200800.81548.37. discussion 12-3. [DOI] [PubMed] [Google Scholar]
- 22.Aly AS CA. St Louis (Missouri): Quality Medical Publishing, Inc; 2006. Brachioplasty. Body Contouring after massive weight loss 1st ed: pp. 303–33. [Google Scholar]
- 23.Aboul Wafa AM. S-shaped brachioplasty: an effective technique to correct excess skin and fat of the upper arm. Plastic and reconstructive surgery. 2013;131:661e–3e. doi: 10.1097/PRS.0b013e318282793e. [DOI] [PubMed] [Google Scholar]
- 24.Bracaglia R, D’Ettorre M, Gentileschi S, Mingrone G, Tambasco D. “Kris knife” brachioplasty after bariatric surgery and massive weight loss. Aesthetic Plast Surg. 2013;37:640–2. doi: 10.1007/s00266-013-0101-9. [DOI] [PubMed] [Google Scholar]
- 25.Knotts CD, Kortesis BG, Hunstad JP. Avulsion brachioplasty: technique overview and 5-year experience. Plastic and reconstructive surgery. 2014;133:283–8. doi: 10.1097/01.prs.0000437261.31693.3c. [DOI] [PubMed] [Google Scholar]
- 26.Fantozzi F. Brachial lifting using the balanced triple-vector (BTV) technique with dual opposing flaps. European journal of plastic surgery. 2014;37:95–102. doi: 10.1007/s00238-013-0901-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kornstein AN. SERI Surgical Scaffold as an Adjunct to Conventional Brachioplasty. Plastic and reconstructive surgery Global open. 2014;2:e190. doi: 10.1097/GOX.0000000000000155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ferraro GA, De Francesco F, Razzano S, D’Andrea F, Nicoletti G. Modified Fish-Incision Technique in Brachioplasty: A Surgical Approach to Correct Excess Skin and Fat of the Upper Arm (Restoring the Armpit Contour) Aesthetic plastic surgery. 2015 doi: 10.1007/s00266-015-0452-5. [DOI] [PubMed] [Google Scholar]
- 29.Han HH, Lee MC, Kim SH, Lee JH, Ahn ST, Rhie JW. Upper arm contouring with brachioplasty after massive weight loss. Archives of plastic surgery. 2014;41:271–6. doi: 10.5999/aps.2014.41.3.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Modolin ML, Cintra W Jr.,, Faintuch J, et al. Improved double-fuse technique for post-bariatric brachioplasty. Revista do Colegio Brasileiro de Cirurgioes. 2011;38:217–22. doi: 10.1590/s0100-69912011000400003. [DOI] [PubMed] [Google Scholar]
- 31.Wolf AM, Kuhlmann HW. Reconstructive procedures after massive weight loss. Obesity surgery. 2007;17:355–60. doi: 10.1007/s11695-007-9064-8. [DOI] [PubMed] [Google Scholar]
- 32.Hurwitz D. Brachioplasty. Clinics in plastic surgery. 2014;41:745–51. doi: 10.1016/j.cps.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 33.Symbas JD, Losken A. An outcome analysis of brachioplasty techniques following massive weight loss. Ann Plast Surg. 2010;64:588–91. doi: 10.1097/SAP.0b013e3181c6cde8. [DOI] [PubMed] [Google Scholar]
- 34.Cannistra C, Valero R, Benelli C, Marmuse JP. Brachioplasty after massive weight loss: a simple algorithm for surgical plane. Aesthetic plastic surgery. 2007;31:6–9. doi: 10.1007/s00266-006-0101-0. discussion 10-1. [DOI] [PubMed] [Google Scholar]
- 35.Bossert RP, Dreifuss S, Coon D, et al. Liposuction of the arm concurrent with brachioplasty in the massive weight loss patient: is it safe? Plastic and reconstructive surgery. 2013;131:357–65. doi: 10.1097/PRS.0b013e3182789de9. [DOI] [PubMed] [Google Scholar]
- 36.Migliori FC, Ghiglione M, D’Alessandro G, Serra Cervetti GG. Brachioplasty after bariatric surgery: personal technique. Obesity surgery. 2008;18:1165–9. doi: 10.1007/s11695-008-9496-9. [DOI] [PubMed] [Google Scholar]
- 37.Pascal JF, Le Louarn C. Brachioplasty. Aesthetic plastic surgery. 2005;29:423–9. doi: 10.1007/s00266-005-0058-4. discussion 30. [DOI] [PubMed] [Google Scholar]
- 38.Knoetgen J 3rd, Moran SL. Long-term outcomes and complications associated with brachioplasty: a retrospective review and cadaveric study. Plastic and reconstructive surgery. 2006;117:2219–23. doi: 10.1097/01.prs.0000218707.95410.47. [DOI] [PubMed] [Google Scholar]
- 39.Gusenoff JA, Coon D, Rubin JP. Brachioplasty and concomitant procedures after massive weight loss: a statistical analysis from a prospective registry. Plastic and reconstructive surgery. 2008;122:595–603. doi: 10.1097/PRS.0b013e31817d54a9. [DOI] [PubMed] [Google Scholar]
- 40.Nguyen AT, Rohrich RJ. Liposuction-assisted posterior brachioplasty: technical refinements in upper arm contouring. Plastic and reconstructive surgery. 2010;126:1365–9. doi: 10.1097/PRS.0b013e3181ebe23c. [DOI] [PubMed] [Google Scholar]
- 41.Elkhatib H. Posterior Scar Brachioplasty with Fascial Suspension: A Long-term Follow-up of a Modified Technique. Plastic and reconstructive surgery Global open. 2013;1:e38. doi: 10.1097/GOX.0b013e3182a71465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zomerlei TA, Neaman KC, Armstrong SD, et al. Brachioplasty outcomes: a review of a multipractice cohort. Plastic and reconstructive surgery. 2013;131:883–9. doi: 10.1097/PRS.0b013e3182827726. [DOI] [PubMed] [Google Scholar]
- 43.De Runz A, Colson T, Minetti C, et al. Liposuction-assisted medial brachioplasty after massive weight loss: an efficient procedure with a high functional benefit. Plastic and reconstructive surgery. 2015;135:74e–84e. doi: 10.1097/PRS.0000000000000845. [DOI] [PubMed] [Google Scholar]
- 44.Thawani SP, Bieri P, Herskovitz S. Brachioplasty-associated multiple mononeuropathies. Muscle & nerve. 2015 doi: 10.1002/mus.24617. [DOI] [PubMed] [Google Scholar]
- 45.Chowdhry S, Elston JB, Lefkowitz T, Wilhelmi BJ. Avoiding the medial brachial cutaneous nerve in brachioplasty: an anatomical study. Eplasty. 2010;10:e16. [PMC free article] [PubMed] [Google Scholar]
- 46.Aly AS, Cram AE, Chao M, Pang J, McKeon M. Belt lipectomy for circumferential truncal excess: the University of Iowa experience. Plastic and reconstructive surgery. 2003;111:398–413. doi: 10.1097/01.PRS.0000037873.49035.2A. [DOI] [PubMed] [Google Scholar]
- 47.Dellon AL, MacKinnon SE. Injury to the medial antebrachial cutaneous nerve during cubital tunnel surgery. Journal of hand surgery. 1985;10:33–6. doi: 10.1016/s0266-7681(85)80011-5. [DOI] [PubMed] [Google Scholar]
- 48.Lowe JB 3rd, Maggi SP, Mackinnon SE. The position of crossing branches of the medial antebrachial cutaneous nerve during cubital tunnel surgery in humans. Plastic and reconstructive surgery. 2004;114:692–6. doi: 10.1097/01.prs.0000130966.16460.3c. [DOI] [PubMed] [Google Scholar]
- 49.Samra S, Samra F, Liu YJ, Sawh-Martinez R, Persing J. Optimal placement of a brachioplasty scar: a survey evaluation. Annals of plastic surgery. 2013;71:329–32. doi: 10.1097/SAP.0b013e31824ca73e. [DOI] [PubMed] [Google Scholar]


