Abstract
Background:
Synovial cysts of the hip are relatively rare lesions comparing to other joints. Patients are usually asymptomatic, but in some cases symptoms such as pain and/or compression of vessels or nerve could be present. Purpose of the study was to define clinical features and optimal management of synovial cyst of the hip joint through an accurate review of the literature.
Methods:
We present three consecutive cases treated with three different therapeutic strategies: surgical excision, wait-and-see and needle aspiration. An accurate review of the literature has been performed to identify patients who had been treated for synovial cyst of the hip.
Results:
Due to the rarity of the disease, there are no significant data in literature supporting the gold standard of treatment. Treatment of the synovial cyst depends on their size, symptoms and comorbidities.
Conclusions:
Most of the Authors recommend surgical treatment for symptomatic synovial cysts and needle aspiration as an option treatment in asymptomatic patients without vessel or nerve compression. In patients that referred symptoms in correspondence with the hip joint, not strictly related with radiograph findings, a CT or MRI examinations should be performed to exclude possible differential diagnosis. (www.actabiomedica.it)
Keywords: benign, arthritis, joint, ganglion cyst, iliopsoas bursitis
Introduction
Synovial cysts may occur around any of the joints, but are commonly found in the knee, shoulder and elbow, whereas those of the hip joint are less frequent (1-6). Development of cyst associated with the hip joint pose difficult problems in diagnosis and surgical treatment (7). Synovial cysts of the hip are usually associated with degenerative joint disease (6-8), rheumatoid arthritis (RA) (9-10), trauma (4-5) and tumors (11-13). Clinical symptoms include pain, limited joint mobility, and compression on adjacent structures, such as the bowels, urinary tract, bladder, extrailiac vessels, femoral vessels (with limb edema), and femoral nerve, entering in differential diagnosis with other diseases (1, 4-5, 8, 14-19). In this paper, we report three consecutive patients that showed symptoms ranging from femoral neuropathy, compression of femoral vessels and stiffness caused by a synovial cyst of the hip joint. The patients have been treated in the same Institution with three different modalities: surgical excision, wait- and-see and needle aspiration based on size of the cyst, their symptoms and comorbidities. The rarity of this condition has prompted us to carefully evaluate the literature in order to define clinical features and optimal management of synovial cyst of the hip joint
Material and methods
We reviewed all the cases of synovial cysts of the hip treated at our Institution from January 2010 to July 2016. Three patients were selectively studied retrospectively. All cystic lesions were confirmed by imaging and histologically in one case. All patients gave written informed consent at the time of admission and last follow-up to be included in scientific studies. IRB approval was not necessary considering the policy of the Ethical Committee of our Institute for retrospective study. Moreover, we performed a search of the literature to identify patients who had been treated for synovial cyst of the hip. English language and non-English language literature were searched in Pubmed using the terms “cyst”, “hip”, “synovial cyst”, “joint” in different combinations and in ISI Web of Knowledge database. The search was done using literature of the past 50 years (from 1966 to 2016), resulting in 36 articles (mainly case reports) describing 39 cases (3-5, 8, 14-45) (Table 1).
Table 1.
Cases of synovial or ganglion cyst of the hip reported in literature
| Autors | Year | n. pts | Age/gender | Symptoms | Comorbidities | Treatment | LR |
|---|---|---|---|---|---|---|---|
| Melamed et al (8) | 1967 | 1 | 71/M | EIV compr. | OA | Surgery | - |
| Armstrong et al (14) | 1972 | 1 | 66/F | FV compr. | - | NA | Y (1 year) |
| Chilton et al (20) | 1980 | 1 | 62/M | EIV compr. | RA | Surgery | - |
| Ford et al (16) | 1981 | 1 | 64/F | EIV, FV compr. | RA | NA | - |
| Grindulis et al (21) | 1982 | 1 | 37/F | EIV compr. | RA | Surgery | - |
| Janus et al (22) | 1982 | 1 | 74/F | EIV, FV compr. | RA | Surgery | - |
| Benichou et al (23) | 1985 | 1 | 78/M | FV compr. | - | Surgery | - |
| 1 | 51/F | EIV compr. | - | Surgery | - | ||
| Atkinson et al (17) | 1986 | 1 | 67/F | EIV compr. | RA | Surgery | Y (1 year) |
| Tebib et al (24) | 1987 | 1 | 72/F | EIV compr. | RA | NA | Y |
| Harris et al (25) | 1987 | 1 | 35/M | FV compr. | - | Surgery | - |
| Binek et al (15) | 1987 | 1 | 80/M | FV compr. | OA | Surgery | - |
| 1 | 58/F | FV compr. | OA | NA | - | ||
| White et al (3) | 1988 | 1 | n/a | Pain | RA | n/a | n/a |
| Duato Janè et al (26) | 1989 | 1 | 56/M | FV compr. | - | Surgery | - |
| Forster et al (27) | 1989 | 1 | 58/M | Swelling | - | n/a | n/a |
| Gale et al (28) | 1990 | 1 | 46/F | FV compr. | - | Surgery | - |
| Bolhuis et al (29) | 1990 | 1 | 76/F | FV compr. | OA | Surgery | - |
| Endo et al (19) | 1990 | 1 | 54/F | FV compr. | - | Surgery | - |
| Savarese et al (30) | 1991 | 1 | 62/F | EIV, FV compr. | - | NA | Y |
| Stadelmann et al (31) | 1992 | 1 | n/a | FN compr. | OA | NA | - |
| Bystrom et al (4) | 1995 | 1 | 75/F | FV compr. | - | Surgery | - |
| Legaye et al (32) | 1995 | 1 | 45/F | FV compr. | - | Surgery | - |
| De Smedt et al (33) | 1996 | 1 | 71/M | EIV compr. | OA | Surgery | - |
| Tamai et al (34) | 1998 | 1 | 83/M | Swelling | - | Surgery | n/a |
| Patkar et al (35) | 1999 | 1 | 50/M | Swelling | RA | Surgery | - |
| Vohora et al (36) | 2000 | 1 | 50/F | FV compr. | OA | NA | - |
| Akman et al (37) | 2002 | 1 | 36/F | Pain | - | Surgery | - |
| O’Riordan et al (38) | 2002 | 1 | 77/F | Pulsating swelling | RA | None | - |
| Julien et al (39) | 2003 | 1 | 49/M | FV compr. | - | Surgery | - |
| Gupta et al (40) | 2003 | 1 | 70/M | meralgia paraesthetica | RA | Surgery | - |
| Rodriguez-Gomez et al (41) | 2004 | 1 | 69/M | EIV compr. | RA | NA | - |
| Sugiura et al (18) | 2004 | 1 | 77/F | EIV compr. | OA | NA | - |
| Stuplich et al (5) | 2005 | 1 | 57/M | FN + FV compr. | - | Surgery | - |
| Colasanti et al (42) | 2006 | 1 | 69/M | FV compr. | OA | Surgery | - |
| Robinson et al (43) | 2007 | 1 | 46/M | FN palsy | Hip contractures | NA + injection | Y* |
| Botchu et al (44) | 2013 | 1 | 67/F | Pain | - | NA + injection | - |
| 1 | 38/M | Pain | - | NA + injection | - | ||
| Kawasaky et al (45) | 2013 | 1 | 67/F | FN neuropathy | RA | Surgery THA | - |
OA: osteoarthritis; RA: rheumatoid arthritis; EIV: external iliac vein; FV: femoral vein; compress: compression; FN: femoral nerve; NA: needle aspiration; LR: local recurrence; n/a: not available
* recurrence cyst was finally treated with surgical excision
Case 1
An 83-year-old man presented with a 1-year history of symptomatic osteoarthritis of the right hip. He became to our attention because in the last months he has exhibited symptoms of anterior thigh pain and paresthesia without trauma. The symptoms have gradually worsened over time. A physical examination showed the following multidirectional limits of motion; flexion, 85°; extension, -10°; abduction, 25°; adduction, 30°; internal rotation, 25°; and external rotation, 50°. Laboratory tests of the blood and urine did not suggest any other underlying disease states. The initial radiographs showed joint space narrowing and joint erosion in both hip joints compatible with hip osteoarthritis. Magnetic resonance imaging (MRI) showed a cystic mass with abnormal intensities in correspondence with the right hip and revealed a communication between the cystic mass and the hip joint (Fig. 1). The mass was close to the proximal insertion of the rectus femoral muscle, strictly associated with the femoral nerve and femoral vessels (Fig. 2).
Figure 1.
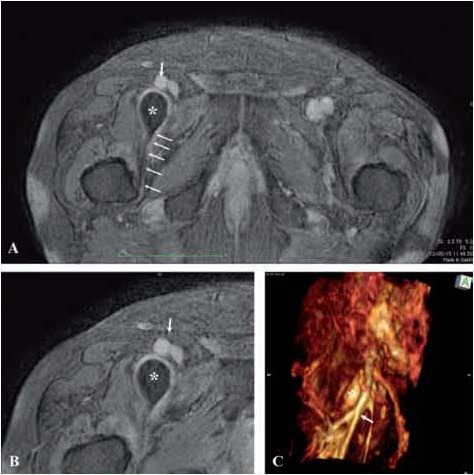
Case 1. Magnetic resonance imaging (MRI) examination findings. A,B) Axial T1-weighted images showed low-intensity area, in front of the right hip joint (asterisk). It appears as a soft cystic lesion near the vascular bundle (white arrow). A communication with joint capsule is clearly identifiable (small white arrows). C) Tridimensional reconstruction has been performed to evaluate preoperatively the relations between cystic lesion (asterisk) and vascular bundle (white arrow)
Figure 2.
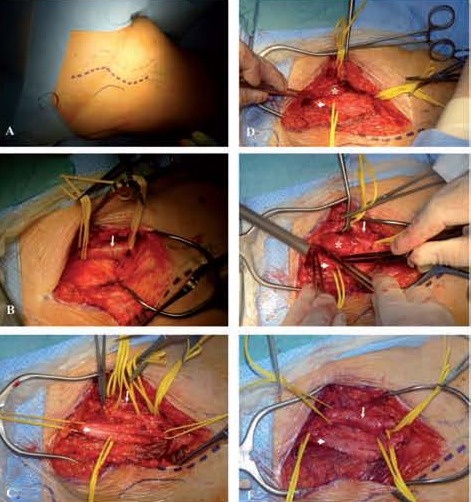
Case 1. Intraoperative phases of surgical removal of the synovial cyst. A) patient in supine position. The longitudinal surgical approach has been drawn on the cutis. B) Surgical isolation of the femoral artery (white arrow) that appeared dislocated superficially. C) Surgical isolation of the femoral nerve (white head-arrow) that also appeared to be compressed by the mass. D) The synovial cyst (asterisk) has been detected deeper to femoral nerve and femoral vessels. E) Marginal excision of the synovial cyst through the cystic wall up to the joint capsule. F) Surgical field after excision of the synovial cyst
Surgical excision was performed through a longitudinal incision over the swelling (Fig. 2A), with the patient in the supine position. The subcutaneous fat and fascia were incised, revealing the vascular bundle dislocated superficially (Fig. 2B). The femoral nerve also appeared to be compressed by the mass and has been adequately exposed and protected (Fig. 2C). A cystic mass has been detected deeper to femoral nerve and femoral vessels (Fig. 2D) and has been isolated up to the joint capsule (Fig. 2E). The hip joint was not opened and the entire mass was excised (Fig. 2F). The cyst was opened and it was filled with synovial fluid. Microscopically, the cyst wall was composed of vascular synovial tissue which contained loose fibrous tissue and aggregates of lymphocytes and plasma cells. All histopathologic findings were consistent with the diagnosis of a synovial cyst. At the time of this report, the clinical course has been uneventful and there was no evidence of recurrence of the hip pain and paresthesia of the right thigh at 1 year of follow-up.
Case 2
A 65-year-old female presented with a 2-year history of painless right-sided inguinal mass associated with lower limb edema. There was no history of rheumatoid arthritis, pelvic trauma or inflammatory disease of the pelvis. At clinical examination, a tender mass measuring about 12 cm in its greatest diameter, localized at the level of right groin was noted. The arterial pulse was present in correspondence with the mass, whereas range of motion of the hip was not limited. Laboratory investigations including red and white blood count with differential count, erythrocyte sedimentation rate, C-reactive protein, rheumatoid factor, liver and renal function tests, and tumours markers (CEA, CA19-9) were normal. The patient was initially evaluated with radiographs of the pelvis that showed minor changes in both hip joints. MRI demonstrated a cystic lesion originating from the hip joint (Fig. 3). The patient has been informed about type of lesion and modalities of treatment and she opted for a conservative approach and follow-up considering the complete absence of symptoms. After one year, a new MRI evaluation has been performed confirming the stationarity of the findings.
Figure 3.
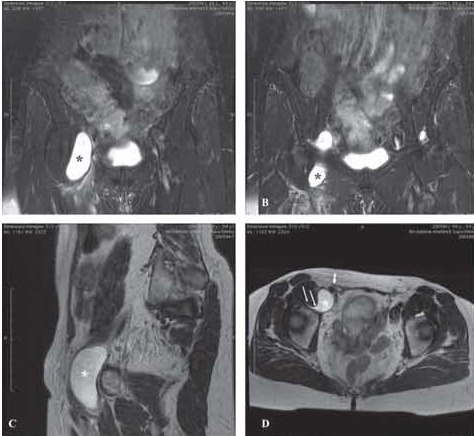
Case 2. Magnetic resonance imaging (MRI) examination findings. A,B) Coronal short tau inversion-recovery (STIR) image showing the full extent of a large synovial cyst arising from the right hip joints (asterisk). C) Sagittal T2-weighted MRI shows the extension of the cyst (asterisk) in the anterior part of the hip joint. D) Axial T2-weighted MRI shows the communication (small white arrows) between the cyst (asterisk) and the hip joint. The femoral vessels (white arrow) appear to be compressed and dislocated by the cyst, as evident comparing with the contralateral side
Case 3
A 56 years-old female was referred to our clinic because of a 6-months history of intermittent dysesthesia and numbness in the anterior part of the thigh. She reported increasing pain during walking, but it was present even at rest. Over the weeks, the walking distance became progressively reduced. There was no history of rheumatoid arthritis, metabolic or inflammatory disease, preceding pelvic trauma, or coagulation disorder. Laboratory investigations including red and white blood count with differential count, erythrocyte sedimentation rate, C-reactive protein, rheumatoid factor, liver and renal function tests, and tumours markers (CEA, CA19-9) were normal. On examination, the range of movement of the hip was complete and a tender, nonpulsatile mass was palpable in the proximal third of the right thigh. Conventional radiographs of the hip showed minor findings of degenerative osteoarthritis of the right hip. An abdominal ultrasonography was also performed because she had lower abdominal pain finding no abdominal abnormalities in the major organs (uterus, ovary, urinary bladder, kidney, liver, gallbladder, spleen, and pancreas). An MRI scan confirmed the presence of a cystic lesion very close to the femoral nerve that appears dislocated and compressed as well as femoral vein and artery. The cyst seems to be connected and originate from the hip joint. However, a ColorDoppler examination revealed no pathologic compression or blood-flow reduction of femoral vessels and the pulses in the distal leg were normal. The patient underwent ultrasound-guided aspiration of the cyst and injection of triamcinolone and bupivacaine. We confirmed a progressive reduction in size and a replacement of the femoral vessels and nerve in anatomic position. Up to 40 ml of fluid have been removed and analyzed. The examination of the fluid was unremarkable. After 6 months, there was no evidence of significant fluid re-accumulation with complete resolution of the symptoms. The patient was pain-free and able to return at her normal lifestyle.
Discussion
Synovial cyst formation is commonly associated with osteoarthritis, particularly in the knee and wrist. Synovial cysts of the hip joint are relatively rare and have been described in literature with different names, such as iliopectineal or iliopsoas bursitis (1, 3-5, 7, 10, 27, 46). These cases have been frequently associated with hip disease such as advanced rheumatoid arthritis, osteoarthritis, infections or trauma (1, 6, 8, 15-18, 20-22, 24, 29, 33, 36, 41.
Theories
Many theories about the synovial cyst development have been performed, even if most of the cases are reported as “idiopathic cysts” suggesting a subtle congenital or developmental defects of the capsule joint (1). One of these theories is that dynamic load produces the displacement of synovial fluid, which in turn may cause cyst development (42). Increased intraarticular pressure due to any kind of joint effusion (such as active synovitis or joint injury), may lead to a gradual formation and enlargement of synovial cysts (47). This is particularly evident in inflammatory disease such as rheumatoid arthritis, that is frequently associated. In this case the overproduction of synovial fluid may increase the intra-articular pressure creating an extension or herniation of the synovial membrane of the hip in a “locus minoris resistentia” of the capsule (1). The displacement of the synovium could be possible also in the embryonal stage (48-49). A second theory postulate that sometimes an anteromedial communication between the hip joint and the iliopsoas bursa may be present and involved in a rheumatoid process, with the subsequent formation of excessive quantities of fluid, enlargement of the bursa, and hypertrophic and villous proliferation of the bursal lining (6). The iliopsoas bursa (that is one of the largest bursae in the human body), is usually located in the anterior site of the hip joint, medially to the iliofemoral ligament, laterally to the pubofemoral ligament and posteriorly to the iliopsoas tendon (46). In 1934, Chandler reported an anatomic study on cadavers showing that a communication between the iliopsoas bursa and the hip joint was present in 15% of adult normal hips (50). This observation suggests that sometimes the bursae may act as volume reservoirs, facilitating joint decompression by allowing the escape of synovial fluid (51). A third theory has been postulated when a direct communication between the hip joint and iliopsoas bursa is not present. In these cases, the necrosis of periarticular tissue resulting from degenerative and rheumatoid changes possibly produce a juxtaarticular cyst or a communicating channel to the hip joint. A fourth reported theory included an iatrogenic cause of cyst formation after anterior soft-tissue surgical release of the hip with accidently joint capsule damage. Robinson et al (43) reported a representative case where it is possible that, at the time of the soft tissue release, the joint capsule was damaged but the active lifestyle of the patient may never have had the opportunity to heal properly, causing a cyst development. All of these theories are difficult to be confirmed and it is usually not possible to determine the exact cause of the cyst because it may be asymptomatic or unrecognized for many months.
Diagnosis
Cysts around the hip joint are often asymptomatic (48). Symptoms and clinical presentation range from inguinal mass to groin or thigh pain, and are always caused by local compression of the structures around the hip joint. A femoral vessel compression by synovial cysts of the hip presenting as deep vein thrombosis or painful lower limb swelling have been reported up-to-now in about 25 cases in literature (4-5, 8, 14-19, 2026, 28-30, 32-33, 36, 39, 41). In some cases radicular pain caused by compression of the femoral or obturator nerve could be present (4-5, 13, 24, 43, 48). Symptoms mimicking L2-L4 radiculopathy such as paresthesia in the groin radiating down to the medial thigh, the anterior aspect of the knee and the medial side of the leg and foot, may be reported. More rarely retroperitoneal extension of the cyst beneath the inguinal ligament may compress the colon, ureteres, or bladder (15). Rarely a synovial cyst over the femoral triangle could be misdiagnosed as a femoral hernia (48). Two of our patients had symptoms due to femoral nerve compression and one had compression of femoral vessels by a synovial cyst of the hip joint. However, in all our cases, the cyst dislocated both femoral nerve and vessels.
A high index of suspicion in patients presenting with persistent pain and without history of trauma, that is unresolved with conservative therapy should prompt further investigation. An adequate evaluation of the imaging should be attempted in order to avoid misdiagnosis (14, 22, 30, 33, 36). A plain radiograph of the pelvis is useful for showing underlying hip joint disorders, but sagittal CT scan or MRI should be performed when symptoms can not be easily explained by the radiographic findings. MRI is the imaging modality of choice in presence of cystic lesions around the hip joint, offering several advantages compared CT scan or ultrasound (47). A communication between cysts and the hip joint may not be demonstrated considering that is usually very narrow or the root has a check valve mechanism (48). Duplex ultrasound allows to differentiate synovial cysts from femoral aneurysm.
Histologically, synovial cysts are lined by synovial cells, contain fluid, may or may not communicate with the joint, and may grow quite rapidly. On the other hand, ganglion cyst histologically are lined by connective tissue probably because of the result of myxomatous tissue degeneration, contain clear high-viscosity mucinous fluid, and rarely communicate with adjacent joints (44,49).
Treatment and outcome
Numerous therapeutic strategies have been previously described ranging from wait-and-see approach to surgery, but the optimal therapy is still controversial. Treatment depends on the size of the cysts, the severity of symptoms, the underlying disease and the presence/absence of local compression. For accessible or smaller cysts, it would seem reasonable to perform a simple cyst aspiration of the cyst, anticoagulation, bed rest, and leg elevation (14-16, 18, 24, 30, 36, 41). However other Authors reported that puncture and fluid drainage did not provide a long-term effect, with a cyst recurrence (reaccumulation of synovial fluid) within few days (46). Ultrasonography is a useful imaging modality that may be used to guide needle aspirations and/or drug injections (43-44). Injections of nonsteroidal anti-inflammatory drugs, local anesthetic or corticosteroids following needle aspiration have been reported as a treatment option (1, 9, 14-15, 31). In synovial cyst caused by rheumatoid arthritis, prednisone and methotrexate may be effective for decreasing the symptoms (48). Yukata et al performed a review of the literature about cystic lesion around the hip joint and concluded that, in their experience, needle aspiration/puncture should be the first treatment choice because has been shown to decrease the cyst size and symptoms related to compression of vessels or nerves (48). However surgical removal of the cyst, associated with synovectomy or capsulectomy is a usually accepted option (4-5, 8, 15, 19-23, 25-26, 28-29, 32-33, 39). Moreover, in case of hip arthritis, surgical treatment with total hip arthroplasty associated with resection of the cyst is a good curative option (52). Other Authors suggested instillation of steroid therapy or sclerosing agents with contradictory results (1, 5, 14-15, 47).
Conclusions
In conclusion, we describe three relatively rare cases of synovial cyst in the hip managed with three different strategies of treatment (surgical excision, wait-and-see approach and needle aspiration). Due to the rarity of the disease, there are no significant data in literature supporting the gold standard of treatment. Most of the Authors recommend surgical treatment for symptomatic synovial cysts and needle aspiration as an option treatment in asymptomatic patients without vessel or nerve compression. In patients that referred symptoms in correspondence with the hip joint, not strictly related with radiograph findings, a CT or MRI examinations should be performed to exclude possible differential diagnosis.
Level of Evidence: Therapeutic study, Level IV (case series - no, or historical control group).
Ethical Board Review statement: Each author certifies that his institution has approved the reporting of these cases and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Coventry MB, Polley HF, Weiner AD. Rheumatoid synovial cyst of the hip; report of three cases. J Bone Joint Surg Am. 1959;41-A:721–30. passim. [PubMed] [Google Scholar]
- 2.Ehrlich GE. Antecubital cysts in rheumatoid arthritis—a corollary to popliteal (Baker’s) cysts. J Bone Joint Surg Am. 1972;54:165–9. [PubMed] [Google Scholar]
- 3.White TK, Incavo SJ, Moreland MS. Giant synovial cyst of the hip joint. Orthop Rev. 1988;17:609–12. [PubMed] [Google Scholar]
- 4.Bystrom S, Adalberth G, Milbrink J. Giant synovial cyst of the hip: an unusual presentation with compression of the femoral vessels. Can J Surg. 1995;38:368–70. [PubMed] [Google Scholar]
- 5.Stuplich M, Hottinger AF, Stoupis C, Sturzenegger M. Combined femoral and obturator neuropathy caused by synovial cyst of the hip. Muscle Nerve. 2005;32:552–4. doi: 10.1002/mus.20364. [DOI] [PubMed] [Google Scholar]
- 6.Warren R, Kaye JJ, Salvati EA. Arthrographic demonstration of an enlarged iliopsoas bursa complicating osteoarthritis of the hip. A case report. J Bone Joint Surg Am. 1975;57:413–5. [PubMed] [Google Scholar]
- 7.Palmer DG. Synovial cysts in rheumatoid diseases. Ann Intern Med. 1969;70:61–68. doi: 10.7326/0003-4819-70-1-61. [DOI] [PubMed] [Google Scholar]
- 8.Melamed A, Bauer CA, Johnson JH. Iliopsoas bursal extension of arthritic disease of the hip. Radiology. 1967;89:54–8. doi: 10.1148/89.1.54. [DOI] [PubMed] [Google Scholar]
- 9.Levy RN, Hermann G, Haimov M, Sherry HS, Train JS, Davison S. Rheumatoid synovial cyst of the hip. Arthritis Rheum. 1982;25:1382–4. doi: 10.1002/art.1780251118. [DOI] [PubMed] [Google Scholar]
- 10.Torisu T, Chosa H, Kitano M. Rheumatoid synovial cyst of the hip joint: a case report. Clin Orthop Relat Res. 1978;137:191–4. [PubMed] [Google Scholar]
- 11.Ruggieri P, Angelini A, Montalti M, Pala E, Calabrò T, Ussia G, Abati CN, Mercuri M. Tumours and tumour-like lesions of the hip in the paediatric age: a review of the Rizzoli experience. Hip Int. 2009 Jan-Mar;19(Suppl 6):S35–45. doi: 10.1177/112070000901906s07. [DOI] [PubMed] [Google Scholar]
- 12.Eisenberg KS, Johnston JO. Synovial chondromatosis of the hip joint presenting as an intrapelvic mass: a case report. J Bone Joint Surg Am. 1972;54:176–8. [PubMed] [Google Scholar]
- 13.Kim DH, Murovic JA, Tiel RL, Kline DG. Intrapelvic and thigh level femoral nerve lesions: management and outcomes in 119 surgically treated cases. J Neurosurg. 2004;100:989–996. doi: 10.3171/jns.2004.100.6.0989. [DOI] [PubMed] [Google Scholar]
- 14.Armstrong P, Saxton H. Ilio-psoas bursa. Br J Radiol. 1972;45:493–5. doi: 10.1259/0007-1285-45-535-493. [DOI] [PubMed] [Google Scholar]
- 15.Binek R, Levinsohn EM. Enlarged iliopsoas bursa. An unusual cause of thigh mass and hip pain. Clin Orthop Relat Res. 1987;224:158–63. [PubMed] [Google Scholar]
- 16.Ford MJ, Martynoga AG, Nuki G. Iliopsoas bursitis in rheumatoid arthritis: an unusual cause of leg oedema. Br Med J (Clin Res Ed) 1981;282:947–8. doi: 10.1136/bmj.282.6268.947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Atkinson MH. Rheumatoid synovial cyst of the hip: an unusual cause of leg swelling. J Rheumatol. 1986;13:986e988. [PubMed] [Google Scholar]
- 18.Sugiura M, Komiyama T, Akagi D, Miyata T, Shigematsu H. Compression of the iliac vein by a synovial cyst. Ann Vasc Surg. 2004;18:369e371. doi: 10.1007/s10016-004-0025-6. [DOI] [PubMed] [Google Scholar]
- 19.Endo M, Sato H, Murakami S, Kidani M, Noto T. A case of pseudothrombophlebitis due to inguinal synovial cyst. Am Surg. 1990;56:533e534. [PubMed] [Google Scholar]
- 20.Chilton CP, Darke SG. External iliac venous compression by a giant iliopsoas rheumatoid bursa. Br J Surg. 1980;67:641. doi: 10.1002/bjs.1800670911. [DOI] [PubMed] [Google Scholar]
- 21.Grindulis KA, McConky B, Norcross K. Iliopsoas bursitis: a surgically correctable cause of lower limb oedema. Practitioner. 1982;226:1336e1337. [PubMed] [Google Scholar]
- 22.Janus C, Hermann G. Enlargement of the iliopsoas bursa: unusual cause of cystic mass on pelvic sonogram. J Clin Ultrasound. 1982;10:133e135. doi: 10.1002/jcu.1870100310. [DOI] [PubMed] [Google Scholar]
- 23.Benichou M, Joyeux A, Mary H, Thevenet A. Synovial cyst of the hip. 2 cases presenting with vascular symptomatology. J Mal Vasc. 1985;10:209e211. [PubMed] [Google Scholar]
- 24.Tebib JG, Dumontet C, Carret JP, Coloson F, Bouvier M. Synovial cyst of the hip causing iliac vein compression and femoral nerve compression. Clin Exp Rheumatol. 1987;5:92e93. [PubMed] [Google Scholar]
- 25.Harris RW, Andros G, Dulawa LB, Oblath RW, Horowitz R. Iliofemoral venous obstruction without thrombosis. J Vasc Surg. 1987;6:594e599. doi: 10.2196/39512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Duato Jane A, Azcona Elizalde JM, Lorente Navarro MC, Ortiz De Solorzano J. Compression of the femoral vein caused by a synovial cyst of the hip. Angiologia. 1989;41:156e160. [PubMed] [Google Scholar]
- 27.Forster BB, Connell DG, Scudamore CH. Synovial cyst of the hip: an unusual cause of an inguinal mass. Can J Surg. 1989 Mar;32(2):133–4. [PubMed] [Google Scholar]
- 28.Gale SS, Fine M, Dosick SM, Whalen RC. Deep vein obstruction and leg swelling caused by femoral ganglion. J Vasc Surg. 1990;12:594e595. [PubMed] [Google Scholar]
- 29.Bolhuis HW, Van der Werf TS, Tjabbes T, Ponsen RJ, Van De Loo RA. Giant synovial cyst of the hip joint presenting with femoral vein compression. Neth J Surg. 1990;42:88e91. [PubMed] [Google Scholar]
- 30.Savarese RP, Kaplan SM, Calligaro KD, De Laurentis DA. Iliopectineal bursutis: an unusual case of iliofemoral vein compression. J Vasc Surg. 1991;13:725e727. [PubMed] [Google Scholar]
- 31.Stadelmann A, Waldis M, von Hochstetter A, Schreiber A. [Nerve compression syndrome caused by synovial cyst of the hip joint] Z Orthop Ihre Grenzgeb. 1992;130:125–128. doi: 10.1055/s-2008-1040125. [DOI] [PubMed] [Google Scholar]
- 32.Legaye J, Redier S. Synovial cyst of the hip. Apropos of a case manifested by venous compression. Acta Orthop Belg. 1995;61:140e143. [PubMed] [Google Scholar]
- 33.De Smedt M, Lechien P. Synovial cyst of the hip: a rare cause of iliac vein compression. Acta Orthop Belg. 1996;62:238e240. [PubMed] [Google Scholar]
- 34.Tamai O, Mamadi T, Muto Y, Toda T. Large synovial cyst of the pelvis containing rice bodies. A case report. International Orthopaedics (SICOT) 1998;22:325–327. doi: 10.1007/s002640050270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Patkar D, Shah J, Prasad S, Patankar T, Gokhale S, Krishnan A, et al. Giant rheumatoid synovial cyst of the hip joint: diagnosed by MRI. J Postgrad Med. 1999;45:118–119. [PubMed] [Google Scholar]
- 36.Vohara HA, Jones B. Femoral vein obstruction with an arthritic hip. J R Soc Med. 2000;93:594e595. doi: 10.1177/014107680009301112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Akman F, Gur B, Sulun T, Aksoy B. A case of a ganglion cyst originating from the hip joint and surgical outcome. Acta Orthop Traumatol Turc. 2002;36:76–78. [PubMed] [Google Scholar]
- 38.O’Riordan CO, Ahmed W, Grace P, Burke T. Synovial cyst of the hip joint: an unusual cause of a pulsating groin mass. Ir Med J. 2002 Jan;95(1):24–25. [PubMed] [Google Scholar]
- 39.Julien Y, Favoulet P, Mistrih R, Dompsure R, Trouilloud P, Cougard P. Synovial cyst of the hip: a misleading strangulated crural hernia diagnosis. Ann Chir. 2003;128:554e556. doi: 10.1016/s0003-3944(03)00222-0. [DOI] [PubMed] [Google Scholar]
- 40.Gupta R, Stafford S, Cox N. Unusual cause of meralgia paraesthetica. Rheumatology. 2003;42:1005. doi: 10.1093/rheumatology/keg241. [DOI] [PubMed] [Google Scholar]
- 41.Rodriguez-Gomez M, Willish A, Luis F, Lopez-Barros G, Abel V, Monton E. Bilateral giant iliopsoas bursitis presenting as refractory edema of lower limbs. J Rheumatol. 2004;31:1452e1454. [PubMed] [Google Scholar]
- 42.Colasanti M, Sapienza P, Moroni E, Mosiello G, Postacchini F, Marzo L. An Unusual Case of Synovial Cyst of the Hip Joint Presenting as Femoral Vein Compression and Severe Lower Limb Edema. Eur J Vasc Endovasc Surg. 2006;32:468e470. doi: 10.1016/j.ejvs.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 43.Robinson KP, Carroll FA, Bull MJ, McClelland M, Stockley I. Transient femoral nerve palsy associated with a synovial cyst of the hip in a patient with spinal cord injury. J Bone Joint Surg [Br] 2007;89-B:107–8. doi: 10.1302/0301-620X.89B1.18273. [DOI] [PubMed] [Google Scholar]
- 44.Botchu R, Esler CN, Lloyd DM, Rennie WJ. Ganglia arising from the transverse acetabular ligament: a report of two cases. Journal of Orthopaedic Surgery. 2013;21(3):380–2. doi: 10.1177/230949901302100324. [DOI] [PubMed] [Google Scholar]
- 45.Kawasaki M, Inoue H, Sabanai K, Sawai T, Sato K. Synovial cyst of the hip in a patient with rheumatoid arthritis. Mod Rheumatol. 2013;23:587–592. doi: 10.1007/s10165-012-0697-7. [DOI] [PubMed] [Google Scholar]
- 46.Tokita A, Ikari K, Tsukahara S, Toki H, Miyawaki M, Mochizuki T, et al. Iliopsoas bursitis-associated femoral neuropathy exacerbated after internal fixation of an intertrochanteric hip fracture in rheumatoid arthritis: a case report. Mod Rheumatol. 2008;18:394–8. doi: 10.1007/s10165-008-0060-1. [DOI] [PubMed] [Google Scholar]
- 47.Sartoris DJ, Danzig L, Gilula L, Greenway G, Resnick D. Synovial cyst of the hip joint and iliopsoas bursitis. A spectrum of imaging abnormalities. Skeletal Radiol. 1985;14(2):85–94. doi: 10.1007/BF00349741. [DOI] [PubMed] [Google Scholar]
- 48.Yukata K, Nakai S, Goto T, Ikeda Y, Shimaoka Y, Yamanaka I, Sairyo K, Hamawaki J. Cystic lesion around the hip joint. World J Orthop. 2015 October 18;6(9):688–704. doi: 10.5312/wjo.v6.i9.688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Steiner E, Steinbach LS, Schnarkowski P, Tirman PF, Genant HK. Ganglia and cysts around joints. Radiol Clin North Am. 1996;34:395–425. xi-xii. [PubMed] [Google Scholar]
- 50.Chandler SB. The iliopsoas bursa in man. Anat Rec. 1934;58:235–40. [Google Scholar]
- 51.Gerber NJ, Dixon ASJ. Synovial cysts and juxta-articular bone cysts (geodes) Semin Arthritis Rheum. 1974;3:323–48. [Google Scholar]
- 52.Matsumoto T, Juji T, Mori T. Enlarged psoas muscle and iliopsoas bursitis associated with a rapidly destructive hip in a patient with rheumatoid arthritis. Mod Rheumatol. 2006;16:52–4. doi: 10.1007/s10165-005-0449-z. [DOI] [PubMed] [Google Scholar]


