Abstract
Pectoralis major tendon (PMT) rupture is a rare event, and it was originally described by Patisser in 1822. The PMT is a thick lamina, which has two origins, one from the clavicle and the other from the ribcage sternum. PMT lesions are classified according to 3 levels of severity: Type 1 is contusions and strains, Type 2 is a partial tear and Type 3 is a complete tear. Diagnosis is made through a clinical examination which comprises a positive response to pain upon pressure over the axilla recess, the presence of bruising and limited motion, and is completed with an MRI. Type 3 injuries are treated exclusively through surgery, while Type 1 and 2 lesions are treated conservatively. In this article, we describe a rare case of PMT rupture in a 39-year-old weight lifter, the surgical treatment that was carried out through an open access at the Pectoralis and Deltoid junction and anchor suture, the post-surgical rehabilitation program and a 1-year follow-up assessment at which point return to sport was achieved. (www.actabiomedica.it)
Keywords: tendon rupture, pectoralis major, sport, weight lifter
Introduction
Pectoralis major tendon (PMT) rupture was originally described by Patisser in 1822 amongst craftspeople afflicted by diseases related to noxious labor choirs (1). There is paucity in the literature of such cases because of its rare incidence. Its manifestation usually occurs in the third decade of life with a higher prevalence in men (2). The PMT is a thick lamina, which has two origins, one from the inferior aspect of the clavicle and the other from the ribcage sternum, and represents the anterior region of the axillary recess. The muscle fibers converge and insert into the greater tubercle of the humerus (3). The Pectoralis major muscle acts primarily as a flexor and adductor of the humerus, and is also activated during the last degrees of internal rotation of the upper limb (4). Subjects affected by Pectoralis Major muscle agenesis in Marmor’s study demonstrated a greater loss of adduction and internal rotation during upper limb motion than the normal population (5). Injuries of the PMT are classified according to 3 levels of severity (Type 1: contusions and strains, Type 2: partial tear, Type 3: complete tear) or according to its location (tendon, myotendon juncture, muscle) (6). The mechanism of injury is usually related to an excessive muscle contraction during bench-press in young weight lifters (7,8). McEntire ascribes the rare incidence of the PMT rupture to its stratified muscle fibers and complex insertion (9). Wolfe believes that the great majority of these lesions occur during bench-press when the shoulders are extended to 30° while sustaining the barbell, thus placing a great deal of stress on the lower portion of the sternal muscle fibers, which are overly stretched, leading to rupture (10). The patient feels a sharp pain in the area of the sternum; bruising and limitation in shoulder adduction and internal rotation against resistance are observed. During the clinical examination, pain is perceived when pressure is applied over the area of lesion. The recommended clinical sign described by Andrews is obtained by asking the patient to place both hands over the anterior iliac crest and comparing tenderness of the bilateral insertion areas using the evaluator’s fingers (4). Diagnosis is later confirmed through an MRI with both arms placed alongside of the patient’s body while in supine position. In Type 1 and 2 lesions, conservative treatment is the preferred choice. The affected limb is held in a shoulder girdle orthosis keeping the arm adducted for approximately 3 weeks. In complete ruptures (Type 3), surgery is mandatory as ruptures left unrepaired may cause an important reduction in upper extremity strength. Reported complications in PMT ruptures left untreated include sepsis related to the associated hematoma (1,11,12) and compartment syndrome (13).
Case report
P.M., 39 years old, right-handed weight lifter, reported a sharp pain while bench-pressing at the gym. His right arm was unable to sustain the barbell and a hematoma quickly formed in vicinity of his armpit. The patient came to our attention 4 days later with a complaint of persistent pain, a marked reduction of his right arm strength while resisting adduction and internal rotation, and a noticeable hematoma that extended from his armpit to his upper arm (Fig. 1). An MRI was ordered (Fig. 2, 3) and a massive lesion of his right PMT was observed along with retraction of the tendon stump towards his armpit, where he felt pain upon applying pressure. P.M. was operated 5 days later using the beach chair position with a deltopectoral incision. The Deltoid muscle and cephalic vein were separated and moved laterally. The retracted PMT (Fig. 4, 5) was cleaned from adhesions and reinserted laterally onto the greater tuberosity of the humerus with a Healix Ti 6.5 anchor guided with 4 needles (Fig. 6). Cephalosporin antibiotics were prescribed post-operatively. The surgery lasted approximately 50 minutes and was executed under general anesthesia without blood loss. The patient was discharged the following day and a shoulder brace immobilizing the arm into 30 degrees of abduction was applied for 35 days. Suture removal was performed 15 days later, without any wound complication. A focal mechanical vibrator device (Equistasi® Srl, Milan, Italy) was used to maintain muscle trophy and tone during the immobilization period and neuro-facilitating maneuvers were done during this period. A physical rehabilitation program began at 35 days from surgery, which consisted in passive mobilization and scar massage. The patient began isometric exercises at 60 days post-operative (Fig. 7). Strengthening and resistive exercises began 30 days later and he returned to weight lifting at 3.5 months from surgery without any functional limitations or pain (Fig. 8).
Figure 1.

Figure 2.
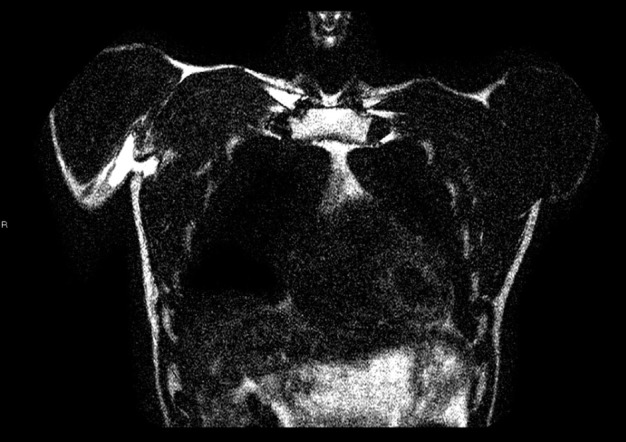
Figure 3.
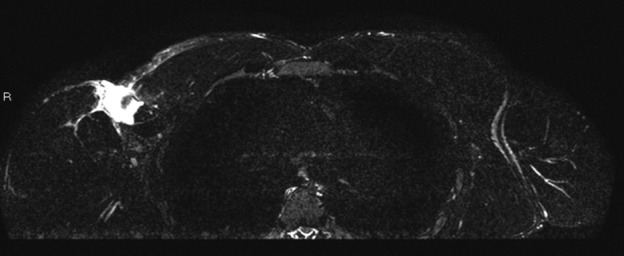
Figure 4.
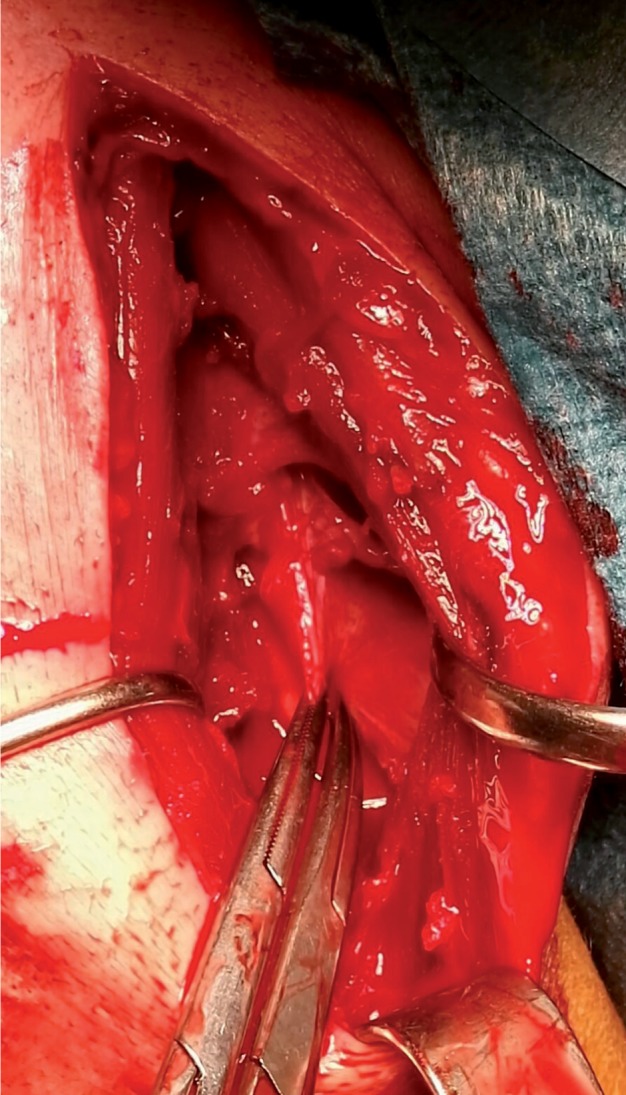
Figure 5.

Figure 6.
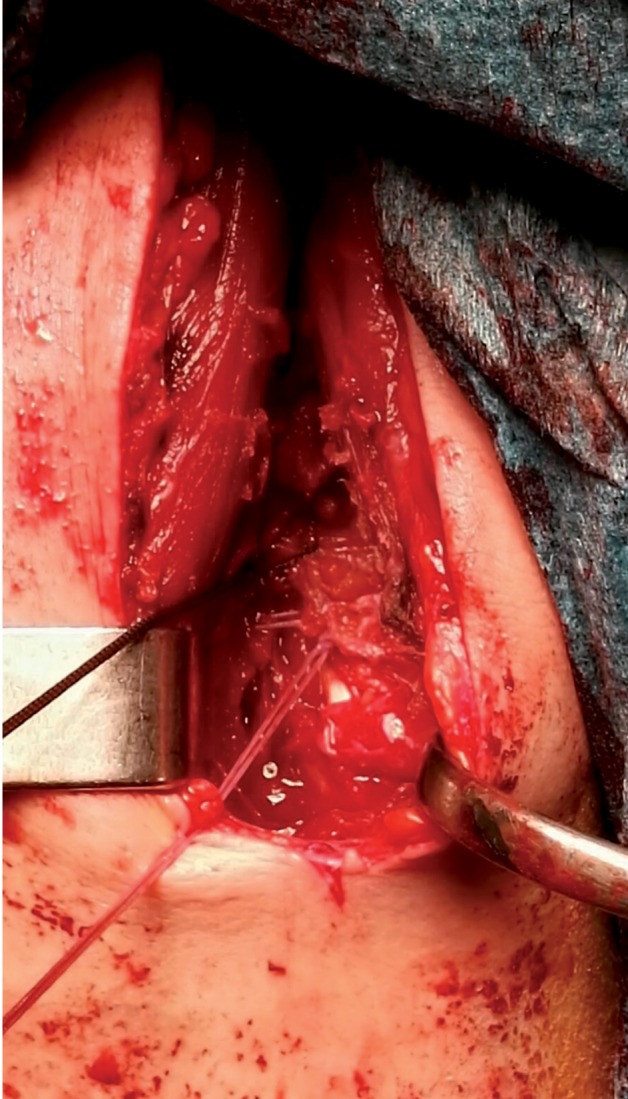
Figure 7.

Figure 8.

Discussion
PMT ruptures are a rare event, which normally occur in young right-handed men practicing weight lifting. This trauma is related to the extreme and unique position adopted while holding the barbell. Some correlate this injury to the use of anabolic steroids (14), but our case was not related to this condition. Diagnosis is made clinically and backed up with an MRI. Type 1 and 2 lesions can be treated conservatively, while Type 3 lesions require direct repair surgery with anchoring to avoid permanent loss of function during arm adduction and internal rotation. Good outcomes have also been reported when reinserting the PMT through humeral trans-osseous foraging (16). Post-operative immobilization should not last less than 30 days and rehabilitation should progress from passive mobilization towards gradual strengthening and return-to-sport at no less than 3 months from surgery. Pool therapy is also recommended but not begun before 45 days postsurgery (15). Outcomes following surgery are clearly superior to the conservative approach in Type 3 lesions as reported by many studies (4,6,15).
Conclusion
PMT ruptures are a rare event, which normally occur in men aged between 20 and 30 years of age and practicing weight lifting. Complete ruptures (Type 3) require early surgery, no later than 15 days from injury, in order to maximize outcomes. Return-to-sport must be gradual following a specific rehabilitation program. Weight bearing against resistance shall begin after 90 days from repair, which is preferable to accomplish with anchors or trans-osseous foraging. Conservative treatment is, on the other hand, preferable for Type 1 and 2 lesions.
References
- 1.Patissier P. Traite des maladies des artisans. Paris. 1822:162–4. [Google Scholar]
- 2.Jobe FW, Moynes DR, Tibone JE, Perry J. An EMG analysis of the shoulder in pitching, a second report. Am J Sport Medicine. 1984;12:218. doi: 10.1177/036354658401200310. [DOI] [PubMed] [Google Scholar]
- 3.Romanes GJ. New York: Oxford University Press; 1981. Cunningham’s textbook of Anatomy. [Google Scholar]
- 4.Andrews JR, Wilk KE. La spalla dell’atleta. Antonio Delfino Editore. 1998:246–9. [Google Scholar]
- 5.Marmor L, Becthol CO, Hall CR. Pectoralis major muscle-function of sternal portion and mechanism of rupture of normal muscles: case report. J Bone Joint Surgery. 1961;43A:81. [Google Scholar]
- 6.Rocwood CA, Matsen FA. La spalla, seconda edizione. Verduci Editore. 1999:1098. [Google Scholar]
- 7.Zeman SC, Rosenfeld RT, Lipscomb PR. Tears of the pectoralis major muscle. Am J Sport Med. 1979;7:343–7. doi: 10.1177/036354657900700607. [DOI] [PubMed] [Google Scholar]
- 8.Kretzelr HH Jr, Richardson AB. Rupture of the pectoralis major muscle. Am J Sport Med. 1989;17:453–8. doi: 10.1177/036354658901700401. [DOI] [PubMed] [Google Scholar]
- 9.Mc Entire JE, Hess WE, Coleman S. Rupture of the pectoralis major muscle. J Bone Joint Surg. 1972;54-A:1040–6. [PubMed] [Google Scholar]
- 10.Wolfe SW, Wickviewicz TL, Cavanaugh JT. Ruptures of the pectoralis major muscle. An anatomic and clical analysis. Am J Sport Med. 1992;20:587–93. doi: 10.1177/036354659202000517. [DOI] [PubMed] [Google Scholar]
- 11.Moulonguet G. Rupturev spontaneedu grand pectoral chez’ un vieillard. Enorme hematoma. Mort Bull Mem See Anat Paris. 1927;94:24–8. [Google Scholar]
- 12.Pai VS, Simison AJ. A rare complication of pectoralis major rupture. Aust NZ J Surg. 1995;65:694–5. doi: 10.1111/j.1445-2197.1995.tb00685.x. [DOI] [PubMed] [Google Scholar]
- 13.Smith AJ, Bajada S, Wardle P, Morgan D. Compartment Syndrome secondary to acute pectoralis tendon rupture. J Shoulder Elbow Surg. 2015 Mar;24(3):78–81. doi: 10.1016/j.jse.2014.10.023. [DOI] [PubMed] [Google Scholar]
- 14.Aarimaa V, Rantanen J, Heikkila J, Helttula I, Orava S. Rupture of the pectoralis major muscle. Am J Sports Med. 2004;32:1256–62. doi: 10.1177/0363546503261137. [DOI] [PubMed] [Google Scholar]
- 15.Merolla G, Campi F, Paladini P, Porcellini G. G Chir. 2006;30:53–7. [PubMed] [Google Scholar]
- 16.Samitier GS, Marcano AI, Farmer KW. Pectoralis major transosseus equivalent repair with knothless anchors: tecnical note and literature review. Int J Shoulder Surg. 2015 Jan Mar;9(1):20–3. doi: 10.4103/0973-6042.150219. [DOI] [PMC free article] [PubMed] [Google Scholar]


