Abstract
Background and aim of the work: The management of displaced 2- and 3-part fractures of the proximal humerus is controversial, both in younger and in elderly patients. The purpose of this paper is to evaluate the functional results of the Contours Proximal Humerus Plate (OrthofixR, Bussolengo,Verona, Italy), for the treatment of displaced 2- and 3-part fractures of the proximal humerus. Methods: We retrospectively reviewed 55 patients with proximal humerus fractures, who underwent osteosynthesis with Contours Proximal Humerus Plate from December 2011 to March 2015. We had 21 patients with 2-part fractures and with an average age of 67.1 years and 34 patients with 3-part fractures, with average age of 63.6 years. Results: The average union time was 3 months. The mean Constant score was 67 for 2-part fracture group and 64.9 for 3-part fracture group. The difference was not statistically significant (p = 0.18). The overall complication rate was 14.5 %. Six patients underwent additional surgery (10.9%). Conclusions: The most frequent major complication was secondary loss of reduction following varus collapse of the fracture (2 cases). In these patients, there was loss of medial hinge integrity due to impaction and osteoporosis. The placement of the main locking screw in the calcar area to provide inferomedial support is the rational of the Contours Proximal Humerus Plate. Osteosynthesis with Contours Proximal Humerus Plate is a safe system for treating displaced 2- and 3-part fractures of the proximal humerus, with good functional results and complication rates comparable to those reported in the literature. (www.actabiomedica.it)
Keywords: shoulder fractures, humeral fractures, osteoporotic fractures, 2-part fracture, 3-part fracture
Background and aim of the work
The incidence of proximal humerus fracture is between 4% and 5% of all fractures (1). They represent the third most common fracture in elderly patients after fractures of the hip and distal radius (2) and are strongly associated with osteoporosis. The vast majority are low-energy osteoporotic fractures resulting from simple falls from standing height (3) with a 2-3 to 1 female to male preponderance (4-6). In younger patients they are often the result of high energy trauma. Most of these fractures, in younger patients as well as in the elderly, are stable and minimally displaced and can be treated conservatively (7). The most frequently used classification is the Neer classification (8). This classification is based on the 4 anatomical segments of the proximal humerus (the humeral head, shaft, the greater and lesser tubercles) and whether these segments are fractured and displaced. According to Neer, “significant displacement” is defined as more than 1 centimeter of translation or 45 degrees of angulation of the respective fracture part.
The management of displaced fractures, however, remains controversial. Treatment of displaced fractures depends on various elements, such as type of fracture, age of patient, associated diseases and level of activity of the patient. While shoulder replacement for 4-part fractures is universally accepted, 2-part and 3-part fractures still create debate, almost of all in elderly patients. Several approaches have been described for the treatment of displaced proximal humerus fractures, including conservative treatment (9), closed reduction and percutaneous Kirschner wire fixation, open reduction followed by fixation with bone sutures, tension band, T-plate, intramedullary nails, locking plates and prosthetic replacement (10-13). Nowadays, the most widely method of treatment for displaced fractures is open reduction and internal fixation (ORIF) with locking plates. Several complications have been reported, such as plate loosening, nonunion, avascular necrosis (AVN), impingement syndrome and rotator cuff syndrome (14,15).
The purpose of this paper is to evaluate the functional results of a new dedicated plate, the Contours Proximal Humerus Plate (PHP, OrthofixR, Bussolengo,Verona, Italy), in the treatment of displaced 2-part and 3-part fractures of the proximal humerus.
Methods
We retrospectively reviewed 55 patients with proximal humerus fractures, who underwent ORIF with dedicated plate (PHP) from December 2011 to March 2015. Inclusion criteria were: closed proximal humerus fractures; displaced 2- and 3-part fractures according to Neer classification (8); patients older than 18 years of age and ability of the patient to co-operate. Exclusion criteria were: open fractures; pathological fractures; concomitant disease likely to influence the end result.
There were 32 women and 13 men, with an average age of 64.9 years (26-82 years). We divided patients in 2 groups, according to the type of fracture. Fractures were classified based on preoperative plain radiographs. Computed Tomography (CT) was performed only in selected cases (3-part fractures with severe osteoporosis). We had 21 patients with 2-part fractures and with an average age of 67.1 years and 34 patients with 3-part fractures, with average age of 63.6 years. We recorded average time to surgery, operative time, functional outcome, complications, management of complications and follow-up.
A deltopectoral approach was used in all cases. The biceps tendon was identified and retracted, the fracture was exposed between the tuberosities and behind the bicipital groove. If the greater tuberosity was displaced posteriorly, attempts were made to reduce it anatomically with non-absorbable wires. The fracture was reduced and temporarily held with K-wires. The reduction was checked fluoroscopically and then a PHP was applied, below the greater tuberosity and lateral to the bicipital groove. Only in selected cases, such as 3-part fractures in elderly patients with osteoporosis and loss of the medial hinge integrity, we used bone grafts.
The Contours PHP is a titanium anatomically shaped plate. It has to be used in combination with at least two diaphyseal screws, a main locking screw and at least two fine threaded screws. The main stabilization of the humeral head is achieved with a cannulated main locking screw to be inserted in the calcar area. To complete the stabilization and fix fracture fragments, minimum two crossing polyaxial fine threaded screws are inserted and locked in the appropriate threaded holes. Distal locking is made in the three distal holes. The plate provides four suture holes to allow a needle insertion and facilitate sutures and cerclage procedures.
Post-operatively the arm was supported in a sling. Pendular movements were started from the second post-operative day and the shoulder was mobilized with active assisted exercises, followed after 4 weeks by active exercises. Each patient was followed up in the outpatient clinic at 1, 3, 6 and 12 months after operation with standard x-rays. Callus formation and bridging trabecular bone were assessed in the follow-up radiographs for verification of radiological union. Functional evaluation was assessed with the Constant score system (16). The scoring system is constituted from 4 categories of interest: pain, activities of daily leaving, range of motion and strength. Score ranges from 0 to 100. Scores below 50 are considered to be a poor result, between 50 and 75 a satisfactory result and above 75 to be an excellent result. Student’s/-test was used to compare the groups, with statistical significance set at p = 0.05.
Results
No patients were lost to follow-up. Patient characteristics are represented in Tables 1 and 2. The fractures were stabilized either acutely or after failure of conservative management in four cases (1 in 2-part fracture group and 3 in 3-part fracture group). Primary surgery was delayed at a median interval of 5 days (range 2-20 days) for 2-part fracture group and 5.4 days (range 1-19 days) for 3-part fracture group. The mean operative time was 84 minutes (range 60170 minutes) for 2-part fracture group and 90 minutes (range 60-130 minutes) for 3-part fracture group. The difference was not statistically significant (p=0,16). One patient had fracture dislocation. One patient had an associated fracture of the omolateral distal radius.
Table 1.
General data of 2-part fracture group
| Case | Sex | Age | Side | Type of fracture | Dislocation | Time to surgery (days) | Surgery | Operative time (minutes) | Complications | Management of complications | Constant score | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 80 | R | 2-part | No | 5 | ORIF | 95 | No | / | 58 | 14 |
| 2 | F | 76 | L | 2-part | No | 6 | ORIF | 100 | No | / | 55 | 14 |
| 3 | F | 60 | L | 2-part | No | 5 | ORIF | 135 | No | / | 65 | 12 |
| 4 | F | 63 | R | 2-part | No | 4 | ORIF | 85 | No | / | 88 | 25 |
| 5 | F | 65 | R | 2-part | No | 4 | ORIF | 170 | No | / | 66 | 21 |
| 6 | F | 71 | R | 2-part | No | 20 | ORIF | 80 | No | / | 63 | 13 |
| 7 | F | 57 | R | 2-part | No | 7 | ORIF | 60 | No | / | 65 | 24 |
| 8 | F | 70 | L | 2-part | No | 2 | ORIF | 70 | No | / | 71 | 12 |
| 9 | F | 59 | R | 2-part | No | 8 | ORIF | 75 | No | / | 77 | 22 |
| 10 | F | 53 | L | 2-part | No | 5 | ORIF | 75 | No | / | 73 | 13 |
| 11 | F | 79 | R | 2-part | No | 4 | ORIF | 95 | No | / | 65 | 18 |
| 12 | F | 58 | L | 2-part | No | 2 | ORIF | 70 | No | / | 61 | 12 |
| 13 | F | 75 | L | 2-part | No | 5 | ORIF | 80 | No | / | 58 | 20 |
| 14 | M | 67 | R | 2-part | No | 5 | ORIF | 70 | No | / | 71 | 12 |
| 15 | F | 77 | L | 2-part | No | 5 | ORIF | 80 | No | / | 65 | 17 |
| 16 | F | 64 | R | 2-part | No | 5 | ORIF | 85 | No | / | 71 | 11 |
| 17 | F | 67 | R | 2-part | No | 3 | ORIF | 60 | No | / | 63 | 8 |
| 18 | F | 77 | R | 2-part | No | 2 | ORIF | 60 | No | / | 61 | 12 |
| 19 | F | 70 | R | 2-part | No | 3 | ORIF | 65 | No | / | 65 | 12 |
| 20 | F | 46 | L | 2-part | No | 2 | ORIF | 60 | No | / | 90 | 10 |
| 21 | M | 75 | L | 2-part | No | 5 | ORIF | 100 | No | / | 58 | 9 |
Abbreviations. F: female; M: male; L: left; R: right; ORIF: open reduction internal fixation
Table 2.
General data of 3-part fracture group
| Case | Sex | Age | Side | Type of fracture | Dislocation | Time to surgery (days) | Surgery | Operative time (minutes) | Complications | Management of complications | Constant score | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 22 | F | 54 | L | 3-part | No | 9 | ORIF | 80 | Delayed callus formation | None | 58 | 12 |
| 23 | F | 65 | L | 3-part | No | 16 | ORIF | 130 | No | / | 63 | 15 |
| 24 | M | 42 | R | 3-part | No | 3 | ORIF | 65 | Intolerance | Hardware removal | 80 | 21 |
| 25 | F | 75 | R | 3-part | No | 4 | ORIF | 105 | No | / | 65 | 22 |
| 26 | F | 70 | L | 3-part | No | 2 | ORIF | 75 | No | / | 66 | 19 |
| 27 | F | 69 | R | 3-part | No | 1 | ORIF | 100 | No | / | 58 | 17 |
| 28 | F | 78 | R | 3-part | No | 6 | ORIF | 70 | No | / | 61 | 13 |
| 29 | M | 43 | L | 3-part | No | 3 | ORIF | 60 | No | / | 63 | 12 |
| 30 | F | 67 | R | 3-part | No | 19 | ORIF | 115 | Lesion of long head of biceps | Hardware removal | 65 | 12 |
| 31 | F | 78 | R | 3-part | No | 3 | ORIF | 80 | Avascular necrosis | Screw removal | 48 | 11 |
| 32 | F | 74 | L | 3-part | No | 4 | ORIF | 120 | No | / | 66 | 9 |
| 33 | F | 57 | R | 3-part | No | 4 | ORIF | 85 | No | / | 71 | 9 |
| 34 | F | 69 | L | 3-part | No | 4 | ORIF | 75 | No | / | 72 | 37 |
| 35 | F | 65 | L | 3-part | No | 4 | ORIF | 110 | No | / | 79 | 14 |
| 36 | F | 73 | L | 3-part | No | 4 | ORIF | 105 | No | / | 69 | 9 |
| 37 | M | 26 | R | 3-part | Yes | 5 | ORIF | 105 | No | / | 72 | 12 |
| 38 | M | 58 | L | 3-part | No | 5 | ORIF | 115 | No | / | 69 | 11 |
| 39 | M | 54 | R | 3-part | No | 3 | ORIF | 110 | No | / | 71 | 12 |
| 40 | M | 63 | R | 3-part | No | 6 | ORIF | 90 | Varus-collapse | Hardware removal | 58 | 23 |
| 41 | F | 48 | L | 3-part | No | 2 | ORIF | 75 | No | / | 61 | 10 |
| 42 | M | 82 | L | 3-part | No | 7 | ORIF | 90 | Penetration of screw through humeral head | New synthesis | 58 | 12 |
| 43 | F | 79 | L | 3-part | No | 4 | ORIF | 80 | No | / | 59 | 12 |
| 44 | F | 62 | R | 3-part | No | 7 | ORIF | 100 | No | / | 58 | 13 |
| 45 | F | 70 | L | 3-part | No | 5 | ORIF | 75 | No | / | 58 | 10 |
| 46 | F | 76 | L | 3-part | No | 4 | ORIF | 60 | No | / | 53 | 12 |
| 47 | M | 68 | R | 3-part | No | 3 | ORIF | 85 | No | / | 61 | 12 |
| 48 | M | 58 | R | 3-part | No | 3 | ORIF | 85 | Tenosynovitis long head biceps | / | 73 | 15 |
| 49 | M | 59 | R | 3-part | No | 3 | ORIF | 75 | No | / | 71 | 12 |
| 50 | F | 67 | L | 3-part | No | 3 | ORIF | 60 | No | / | 63 | 15 |
| 51 | M | 78 | R | 3-part | No | 8 | ORIF | 105 | No | / | 65 | 14 |
| 52 | F | 56 | L | 3-part | No | 7 | ORIF | 95 | No | / | 63 | 29 |
| 53 | F | 36 | R | 3-part | No | 15 | ORIF | 95 | No | / | 88 | 13 |
| 54 | F | 68 | L | 3-part | No | 8 | ORIF | 80 | No | / | 65 | 11 |
| 55 | F | 75 | R | 3-part | No | 2 | ORIF | 115 | Fracture collapse | Hardware removal | 58 | 12 |
Abbreviations. F: female; M: male; L: left; R: right; ORIF: open reduction internal fixation
The average union time was 3 months. The mean Constant score was 67 for 2-part fracture group (figure 1) and 64.9 for 3-part fracture group (figure 2). The difference was not statistically significant (p=0.18). In the 2-part fracture group 18 patients had satisfactory results and 3 had excellent results. In the 3-part fracture group 30 patients had satisfactory results, 3 had excellent results and only 1 patient had poor result (this was the only case of AVN). Average follow-up was 14.8 months for 2-part fracture group and 14.4 months for 3-part fracture group.
Figure 1.
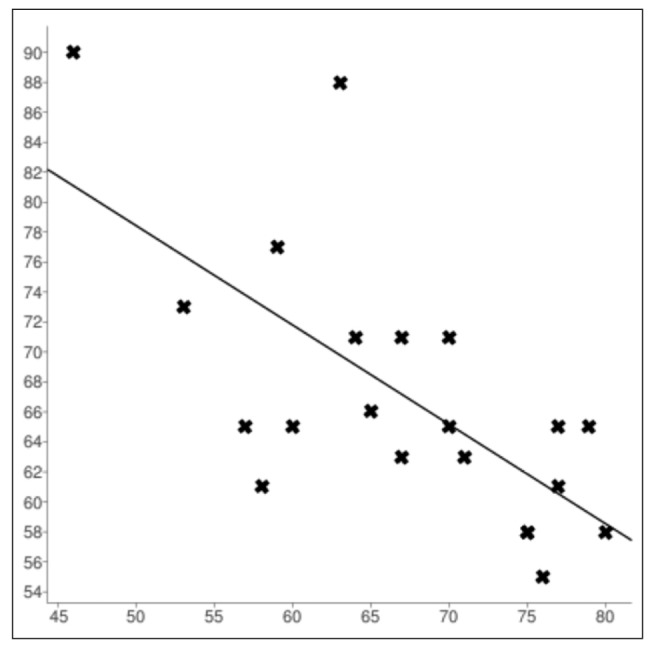
Scatter plot of the age of the patients with 2-part fracture versus Constant score, showing the line of best fit. X = age, y = Constant score
Figure 2.
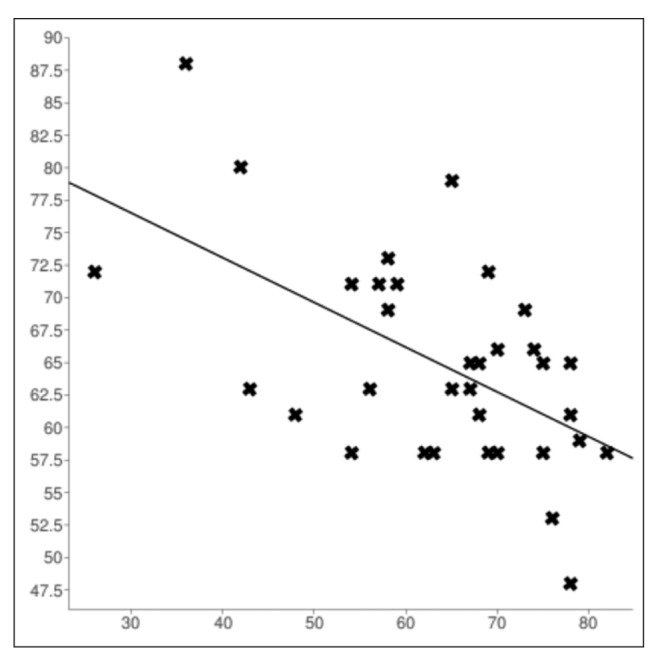
Scatter plot of the age of the patients with 3-part fracture versus Constant score, showing the line of best fit. X = age, y = Constant score
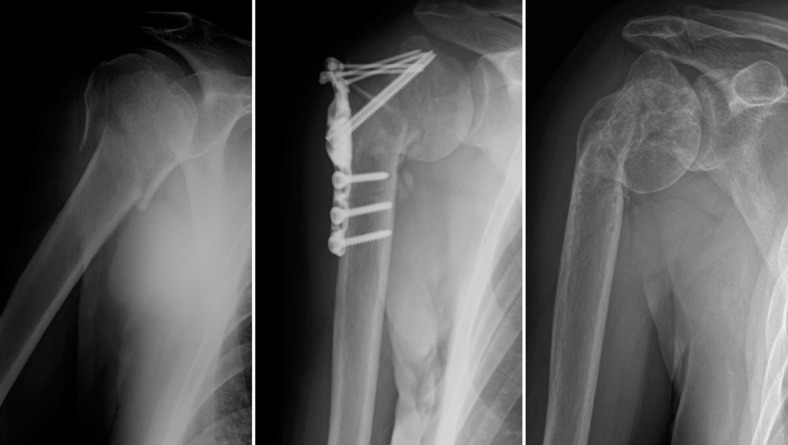
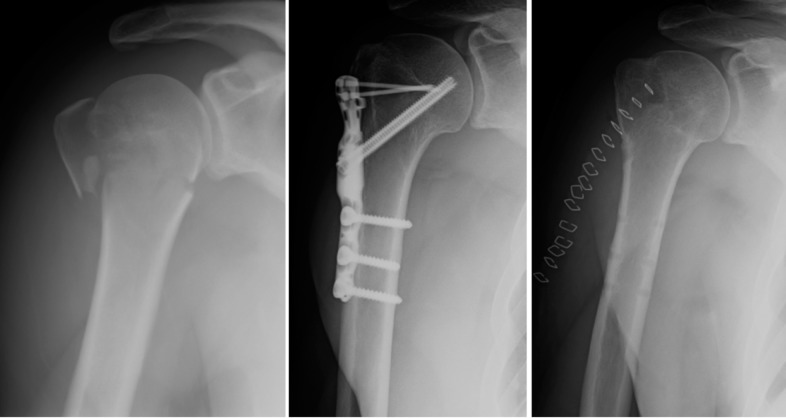
Two-part fracture group did not experience complications. In 3-part fracture group we recorded 4 major complications and 4 minor complications. Major complications were: one case of AVN (case 31), which was managed with partial hardware removal; two cases of varus-collapse [cases 40 (figure 3) and 55], both treated with hardware removal; one case of screw penetration into the humeral head, treated with new synthesis (case 42). Among minor complications we reported: one case of delayed callus formation, treated conservatively with sling for one month (case 22); one case of hardware intolerance, which was removed [case 24 (figure 4)]; one case of lesion of the long head of the biceps, which was managed with hardware removal (case 30) and finally one case of tenosynovitis of the long head of the biceps treated conservatively with laser-therapy (case 48). The overall rate of major complications was 7.2%. The overall rate of minor complications was 7.2%. Six patients underwent additional surgery (10.9%). All major complications occurred in elderly patients (over 60 years).
Figure 3.
Three-part fracture of the proximal humerus in a 63-year-old man who was treated with osteosynthesis with PHP. He developed varus collapse and he underwent hardware removal after 12 months. Although last x-ray shows varus collapse of the humeral head, the patient does not feel pain and he is independent in daily-life activities. His Constant score is 58
Figure 4.
Three-part fracture of the proximal humerus in a 42-year old male. After ORIF with PHP, the patient experienced discomfort and he underwent plate removal after 12 months. At last follow-up he was satisfied with functional result. His Constant score was 80
Discussion
Operative treatment of displaced 2-part and 3-part fractures in younger patients is not controversial. The main controversy pertains to elderly patients with varying degrees of osteoporosis and displaced fractures sustained after low-energy trauma. In this patient group there is little evidence and poor consensus regarding the optimal treatment modality (17).
Twenty years ago the enthusiasm for early mobilization and the availability of better fixation devices popularized treatment of proximal humerus fractures by ORIF. ORIF with locking plates have the potential to restore the anatomy in an excellent manner; but there is a risk of complications related to both the implant (18-21) and the surgery itself (22,23). One of the most used fixation devices for ORIF is the Philos plate, which has been developed by AO to improve screw fixation in osteoporotic bone and to minimize soft-tissue dissection. One of the first studies reporting Philos plate results was published by Moonot et al. in 2007 (24). They presented a series of 32 patients with 3- and 4-part fractures of the proximal humerus successfully treated with Philos plate. Three patients developed impingement and one nonunion with associated AVN. Later, Kumar et al. (25) reported the results of 51 patients with 2-, 3- and 4-part fractures of the proximal humerus treated with Philos plate. Although mean Constant score was 79, they had an overall complication rate of 16.3%, including varus malunion, deep infection, subacromial impingement, fixation failure and intra-articular screw penetration. Jaura et al. (26) compared the results of Philos plate versus percutaneous fixation in proximal humerus fractures in the elderly. They concluded that ORIF with Philos plate had the advantages of accurate reduction, early mobilization, better fixation in osteoporotic bones (due to the locking screws) and ease of reconstruction of comminuted irreducible fractures. On the other hand the technique had the disadvantages of excessive soft tissue dissection and blood loss, risk of injury to the neurovascular structures and increased risk of AVN of the humeral head.
Recently, in order to reduce soft tissue dissection and the risk of AVN, a new minimally invasive technique of open reduction and plate osteosynthesis (MIPO) has been proposed. Fracture is reduced through an anterolateral deltoid splitting approach, providing better visualization of the posterolateral aspect of the shoulder without extensive soft tissue dissection; however there is an increased risk of injuring the axillary nerve as compared to the conventional deltopectoral approach (27-29). Lin et al. (30) reported the results of a comparative study between MIPO with locking compression plate and ORIF in 2 groups of 43 patients. They concluded that MIPO with locking compression plate had good functional results and required less surgical time, caused less blood loss and shorten hospital stay compared to ORIF.
ORIF complications are well known and reported by several authors (31-33) and include infection, intra-articular screw penetration, subacromial impingement, varus collapse of the fracture, AVN and osteoarthritis. These may lead to unplanned reoperations in 13% (32) to 19% (33) of patients, with a predilection for those older than 60 years of age with unstable 3- and 4-part fractures. In some patient series with high rates of 3- and 4-part fractures, revision surgery to arthroplasty was required in more than 50% of the patients, whilst screw penetration-mediated glenoid erosion, significantly limited revision options and adversely affected long-term outcomes (34).
Conservative treatment with short immobilization and early physiotherapy is a noninvasive, simple and safe option, and acceptable results after nonoperative treatment have been reported (5, 35,36). Zyto et al. (9) randomized 40 elderly patients of mean age of 74 years with 3- and 4-part fractures of the proximal humerus to either conservative treatment or tensionband osteosynthesis. At 1 year and after 3 to 5 years, clinical follow-up showed no functional differences between the two groups of patients. There were major complications (AVN and nonunion) only in the surgically-treated group. Olerud et al. (37) presented a randomized controlled trial comparing internal fixation versus nonoperative treatment of displaced 3-part fractures of the proximal humerus in elderly patients: they found an advantage in functional outcome in favor of the locking plate compared to nonoperative treatment, but at the cost of additional surgery in 30% of the patients. However, conservative treatment is also characterized by some complications, such as malunion, subacromial impingement, AVN, shoulder pain and stiffness secondary to osteoarthritis and rotator cuff deficiency (38).
Neither systematic reviews have solved the great debate of displaced proximal humerus fracture treatment. The latest Cochrane review regarding this topic (17) concludes that there is insufficient evidence from randomized controlled trials to determine which interventions are the most appropriate for the different types of proximal humeral fractures.
According to Constant score, we had excellent results in 6 patients, satisfactory results in 48 and poor result in only one patient. These results are comparable to those previously reported (24,26). In our study, the overall complication rate of 14.5% is comparable to other rates reported in the literature. The most frequent major complication was secondary loss of reduction following a varus collapse of the fracture (2 cases). In these patients, there was loss of medial hinge integrity due to impaction and osteoporosis, causing the fractures to be unstable. Recent studies have already demonstrated a direct association between medial support and subsequent reduction loss in complex humeral fractures (39,40). The placement of the main locking screw in the calcar area to provide inferomedial support is the rational of the Contours PHP plate presented in this study.
Conclusions
ORIF with Contours PHP is a safe system for treating displaced 2- and 3-part fractures of the proximal humerus, with good functional results. In 2-part fracture group we did not report complications. Complication rates for 3-part fractures are comparable to the other reconstructive methods reported in the literature and are more related to the age of the patients and quality of bone rather than a specific surgery approach or fixation device. The problem of surgical indication in elderly patients is still open. We believe in these patients treatment should be planned according general status and functional demanding.
References
- 1.Habermeyer P, Schweiberer L. Fractures of the proximal humerus. Orthopade. 1989;18(3):200–7. [PubMed] [Google Scholar]
- 2.Barrett JA, Baron JA, Karagas MR, Beach ML. Fracture risk in the U.S. Medicare population. J Clin Epidemiol. 1999;52(3):243–9. doi: 10.1016/s0895-4356(98)00167-x. [DOI] [PubMed] [Google Scholar]
- 3.Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury. 2006;37(8):691–7. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 4.Lind T, Kroner K, Jensen J. The epidemiology of fractures of the proximal humerus. Arch Orthop Trauma Surg. 1989;108(5):285–7. doi: 10.1007/BF00932316. [DOI] [PubMed] [Google Scholar]
- 5.Court-Brown CM, Garg A, McQueen MM. The epidemiology of proximal humeral fractures. Acta Orthop Scand. 2001;72(4):365–71. doi: 10.1080/000164701753542023. [DOI] [PubMed] [Google Scholar]
- 6.Roux A, Decroocq L, El Batti S, Bonnevialle N, Moineau G, Trojani C, et al. Epidemiology of proximal humerus fractures managed in a trauma center. Orthop Traumatol Surg Res. 2012;98(6):715–9. doi: 10.1016/j.otsr.2012.05.013. [DOI] [PubMed] [Google Scholar]
- 7.Young TB, Wallace WA. Conservative treatment of fractures and fracture-dislocations of the upper end of the humerus. J Bone Joint Surg Br. 1985;67(3):373–7. doi: 10.1302/0301-620X.67B3.3997943. [DOI] [PubMed] [Google Scholar]
- 8.Neer CS 2nd. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52(6):1077–89. [PubMed] [Google Scholar]
- 9.Zyto K, Ahrengart L, Sperber A, Törnkvist H. Treatment of displaced proximal humeral fractures in elderly patients. J Bone Joint Surg Br. 1997;79(3):412–7. doi: 10.1302/0301-620x.79b3.7419. [DOI] [PubMed] [Google Scholar]
- 10.Park MC, Murthi AM, Roth NS, Blaine TA, Levine WN, Bigliani LU. Two-part and three-part fractures of the proximal humerus treated with suture fixation. J Orthop Trauma. 2003;17(5):319–25. doi: 10.1097/00005131-200305000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Ogiwara N, Aoki M, Okamura K, Fukushima S. Ender nailing for unstable surgical neck fractures of the humerus in elderly patients. Clin Orthop Relat Res. 1996;330:173–80. doi: 10.1097/00003086-199609000-00021. [DOI] [PubMed] [Google Scholar]
- 12.Resch H, Povacz P, Fröhlich R, Wambacher M. Percutaneous fixation of three- and four-part fractures of the proximal humerus. J Bone Joint Surg Br. 1997;79(2):295–300. doi: 10.1302/0301-620x.79b2.6958. [DOI] [PubMed] [Google Scholar]
- 13.Robinson CM, Page RS, Hill RM, Sanders DL, CourtBrown CM, Wakefield AE. Primary hemiarthroplasty for treatment of proximal humeral fractures. J Bone Joint Surg Am. 2003;85-A(7):1215–23. doi: 10.2106/00004623-200307000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Sadowski C, Riand N, Stern R, Hoffmeyer P. Fixation of fractures of the proximal humerus with the PlantTan Humerus Fixator Plate: early experience with a new implant. J Shoulder Elbow Surg. 2003;12(2):148–51. doi: 10.1067/mse.2003.11. [DOI] [PubMed] [Google Scholar]
- 15.Björkenheim JM, Pajarinen J, Savolainen V. Internal fixation of proximal humeral fractures with a locking compression plate: a retrospective evaluation of 72 patients followed for a minimum of 1 year. Acta Orthop Scand. 2004;75(6):741–5. doi: 10.1080/00016470410004120. [DOI] [PubMed] [Google Scholar]
- 16.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;(214):160–4. [PubMed] [Google Scholar]
- 17.Handoll HH, Gibson JN, Madhok R. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev. 2003;(4) doi: 10.1002/14651858.CD000434. CD000434. [DOI] [PubMed] [Google Scholar]
- 18.Brunner F, Sommer C, Bahrs C, Heuwinkel R, Hafner C, Rillmann P, et al. Open reduction and internal fixation of proximal humerus fractures using a proximal humeral locked plate: a prospective multicenter analysis. J Orthop Trauma. 2009;23(3):163–72. doi: 10.1097/BOT.0b013e3181920e5b. [DOI] [PubMed] [Google Scholar]
- 19.Fankhauser F, Boldin C, Schippinger G, Haunschmid C, Szyszkowitz R. A new locking plate for unstable fractures of the proximal humerus. Clin Orthop Relat Res. 2005;430:176–81. doi: 10.1097/01.blo.0000137554.91189.a9. [DOI] [PubMed] [Google Scholar]
- 20.Handschin AE, Cardell M, Contaldo C, Trentz O, Wanner GA. Functional results of angular-stable plate fixation in displaced proximal humeral fractures. Injury. 2008;39(3):306–13. doi: 10.1016/j.injury.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 21.Hirschmann MT, Quarz V, Audige L, Ludin D, Messmer P, Regazzoni P, et al. Internal fixation of unstable proximal humerus fractures with an anatomically preshaped interlocking plate: a clinical and radiologic evaluation. J Trauma. 2007;63(6):1314–23. doi: 10.1097/01.ta.0000240457.64628.38. [DOI] [PubMed] [Google Scholar]
- 22.Clavert P, Adam P, Bevort A, Bonnomet F, Kempf JF. Pitfalls and complications with locking plate for proximal humerus fracture. J Shoulder Elbow Surg. 2010;19(4):489–94. doi: 10.1016/j.jse.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 23.Olerud P, Ahrengart L, Soderqvist A, Saving J, Tidermark J. Quality of life and functional outcome after a 2-part proximal humeral fracture: a prospective cohort study on 50 patients treated with a locking plate. J Shoulder Elbow Surg. 2010;19(6):814–22. doi: 10.1016/j.jse.2009.11.046. [DOI] [PubMed] [Google Scholar]
- 24.Moonot P, Ashwood N, Hamlet M. Early results for treatment of three- and four-part fractures of the proximal humerus using the PHILOS plate system. J Bone Joint Surg Br. 2007;89(9):1206–9. doi: 10.1302/0301-620X.89B9.18528. [DOI] [PubMed] [Google Scholar]
- 25.Kumar GN, Sharma G, Sharma V, Jain V, Farooque K, Morey V. Surgical treatment of proximal humerus fractures using PHILOS plate. Chin J Traumatol. 2014;17(5):279–84. [PubMed] [Google Scholar]
- 26.Jaura G, Sikdar J, Singh S. Long Term Results of PHILOS Plating and Percutaneous K-Wire Fixation in Proximal Humerus Fractures in The Elderly. Malays Orthop J. 2014;8(1):4–7. doi: 10.5704/MOJ.1403.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Robinson CM, Khan L, Akhtar A, Whittaker R. The extended deltoid-splitting approach to the proximal humerus. J Orthop Trauma. 2007;21(9):657–62. doi: 10.1097/BOT.0b013e3180ce833e. [DOI] [PubMed] [Google Scholar]
- 28.Roderer G, Erhardt J, Graf M, Kinzl L, Gebhard F. Clinical results for minimally invasive locked plating of proximal humerus fractures. J Orthop Trauma. 2010;24(7):400–6. doi: 10.1097/BOT.0b013e3181ccafb3. [DOI] [PubMed] [Google Scholar]
- 29.Acklin YP, Sommer C. Plate fixation of proximal humerus fractures using the minimally invasive anterolateral delta split approach. Oper Orthop Traumatol. 2012;24(1):61–73. doi: 10.1007/s00064-011-0051-9. [DOI] [PubMed] [Google Scholar]
- 30.Lin T, Xiao B, Ma X, Fu D, Yang S. Minimally invasive plate osteosynthesis with a locking compression plate is superior to open reduction and internal fixation in the management of the proximal humerus fractures. BMC Musculoskelet Disord. 2014;15:206. doi: 10.1186/1471-2474-15-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Krappinger D, Bizzotto N, Riedmann S, Kammerlander C, Hengg C, Kralinger FS. Predicting failure after surgical fixation of proximal humerus fractures. Injury. 2011;42(11):1283–8. doi: 10.1016/j.injury.2011.01.017. [DOI] [PubMed] [Google Scholar]
- 32.Owsley KC, Gorczyca JT. Fracture displacement and screw cutout after open reduction and locked plate fixation of proximal humeral fractures [corrected] J Bone Joint Surg Am. 2008;90(2):233–40. doi: 10.2106/JBJS.F.01351. [DOI] [PubMed] [Google Scholar]
- 33.Konrad G, Bayer J, Hepp P, Voigt C, Oestern H, Kaab M, et al. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Surgical technique. J Bone Joint Surg Am. 2010;92(Suppl 1) doi: 10.2106/JBJS.I.01462. Pt 1 85-95. [DOI] [PubMed] [Google Scholar]
- 34.Jost B, Spross C, Grehn H, Gerber C. Locking plate fixation of fractures of the proximal humerus: analysis of complications, revision strategies and outcome. J Shoulder Elbow Surg. 2013;22(4):542–9. doi: 10.1016/j.jse.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 35.Hanson B, Neidenbach P, de Boer P, Stengel D. Functional outcomes after nonoperative management of fractures of the proximal humerus. J Shoulder Elbow Surg. 2009;18(4):612–21. doi: 10.1016/j.jse.2009.03.024. [DOI] [PubMed] [Google Scholar]
- 36.Zyto K. Non-operative treatment of comminuted fractures of the proximal humerus in elderly patients. Injury. 1998;29(5):349–52. doi: 10.1016/s0020-1383(97)00211-8. [DOI] [PubMed] [Google Scholar]
- 37.Olerud P, Ahrengart L, Ponzer S, Saving J, Tidermark J. Internal fixation versus nonoperative treatment of displaced 3-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elbow Surg. 2011;20(5):747–55. doi: 10.1016/j.jse.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 38.Murray IR, Amin AK, White TO, Robinson CM. Proximal humeral fractures: current concepts in classification, treatment and outcomes. J Bone Joint Surg Br. 2011;93(1):1–11. doi: 10.1302/0301-620X.93B1.25702. [DOI] [PubMed] [Google Scholar]
- 39.Zhang L, Zheng J, Wang W, Lin G, Huang Y, Zheng J, et al. The clinical benefit of medial support screws in locking plating of proximal humerus fractures: a prospective randomized study. Int Orthop. 2011;35(11):1655–61. doi: 10.1007/s00264-011-1227-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Osterhoff G, Ossendorf C, Wanner GA, Simmen HP, Werner CM. The calcar screw in angular stable plate fixation of proximal humeral fractures-a case study. J Orthop Surg Res. 2011;6:50. doi: 10.1186/1749-799X-6-50. [DOI] [PMC free article] [PubMed] [Google Scholar]