Abstract
Phenytoin is normally used in epilepsy treatment. One of the side effect affecting a significative part of the treated patients is the gingival overgrowth. It could surely be a correlation between this stimulatory effect and the assessment of phenytoin in wound healing. In fact, some studies of the literature have shown that topical phenytoin promotes healing of traumatic wounds, burns and ulcers by decubitus or stasis (diabetic or venous) and we emphasize, in vitiligo, a particular attention into repigmentation. The related mechanism of action seems to be multifactorial. In the present paper topical phenytoin has been used as wound-healing agent in 19 documented cases of bedsores, divided in treated and placebo group. The used concentration of phenytoin was 5 mg/L dissolved in a water solution of 9 g NaCl/L (0.9% P/V of NaCl). Patches soaked with phenytoin solution were applied over the bedsores along 3 hours every 12 hours. Results showed that phenytoin treated patients healed their wounds significantly before (p<0.001) with respect to controls. (www.actabiomedica.it)
Keywords: wound healing, topical phenytoin, bedsores
Background
Researches for better wound-healing agents is an old challenge in medical practice and the healing or chronic wounds remain today a significant healthcare problem. Introduced for the effective control of convulsive disorders in 1937 (1), phenytoin (diphenylhydantoin) has to day the best challenge in wound healing as, in some patients treated with phenytoin, was first observed gingival hyperplasia. This aspect stimulated Bathia (1939) to use phenytoin in wound healing (2).
The first controlled clinical trial was conducted by Shapiro in 1958 where he found that periodontal patients with surgical wounds, pretreated with oral phenytoin, had reduced inflammatory reactions, reduced pain and accelerated healing compared to controls (3).
In a subsequent work with phenytoin Goebil promoted the healing of dental extraction sockets (4) and Shafer increased the tensile strength of experimental skin and corneal wounds (5).
Recently, a paper by Teo SY et al. (6) showed that phenytoin-loaded alkyd nanoemulsions show potential for promoting topical wound healing through enhanced proliferation of epidermal cells.
Finally, preliminary studies by Hemmati AA et al (7) established that phenytoin, especially together with calcium channel blockers, can be used to enhance wound healing. Further studies are, anyway, needed to find out the multifactorial mechanism of this healing effect.
Based on several incomes with positive results after topical treatment with phenytoin, in this work our purpose was to demonstrate the validity of the topical treatment with phenytoin in bedsores, a pathology afflicting a lot of people forced to lie in bed for a long time.
Materials and methods
Preparation and administration
Studies investigating the effect of topical phenytoin on wound healing suggest that phenytoin could bring positive effect in a large variety of wounds (8) and phenytoin powder could be also applied directly to wounds in a thin, uniform layer and then covered with gauze (9) but the actual best procedure involves the dissolution of th Sodium phenytoin powder (USP) ref. standard cod. 1535008, had been supplied to UNIBA (Dept of Biom. Sci & Human Oncology) from Levanchimica srl Bari, Italy, cod CUP H93G13000170005, cod CIG Z7F14558C6.e phenytoin sodium powder in NaCl (0.9%) and applying the solution with gauze on the bedsores.
Patients were not instructed for self administration of phenytoin due to obliged prone position. Therefore, a nurse or relative had been instructed for the application of patches which had to remain on bedsores for 3 hours and replicated every 3 hours.
Patients
Nineteen old age patients (not at term), forced to lie into bed for a long time because of marrow transplantation due a Hodgkin’s or a kidney disease were enrolled in the present study. Patients suffering from serious diseases (advanced diabetes, intractable cancers) were not included. The enrolled patients were randomly divided in 2 groups.
1st group: 11 patients, 7 males and 4 females, (age from 63 to 77) treated with topical gauzes soaked with a solution (sodium phenytoin 0.5 mg % diluted in NaCl 0.9 g% in water solution)
2nd group: 8 patients, 3 males and 5 females (age from 61 to 80), treated with topical gauzes soaked with NaCl 0.9 g% in water solution(controls).
Statistical comparisons, performed between healing times of treated subjects with respect to control subjects, were made using the Student’s t test. Data were presented as means ±SD. Differences were considered significant if p<0.05
Results
11 patients treated with topical phenytoin healed their bedsores in a significant shorter time (19.36±3.0 Sd days) (Figure 1) compared to the 8 patients treated with NaCl 0.9 % solution (28.75±2.43 SD days; p<0.001). Mainly, the long period of immobility in bed of the enrolled patients was related to traumatic diseases. During the experiment no side effects were detected in patients with a presumable relationship with phenytoin treatment. Each patient admission to the present experiment was consequent to the release of a written spontaneous consent. Patients at term were not enrolled into the present experiment. We followed the health conditions of the enrolled patients for a month, at least, after the healing process of their bedsores highlighting no health problems.
Figure 1.
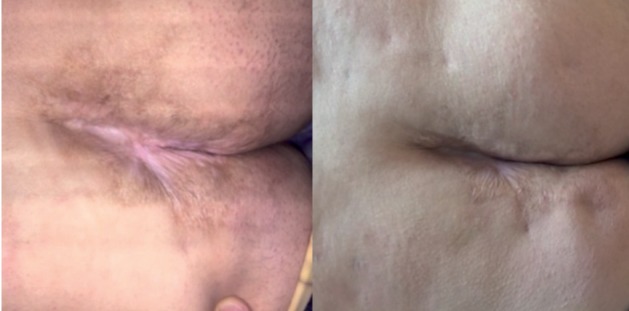
(patient n. 3, male) Bedsores before phenytoin treatment (left) and after 20 days treatment (right)
Discussion
A number of clinical studies indicate that phenytoin decreases the bacterial load of wounds (10, 11, 12). Biopsies of phenytoin treated open wounds show neovascularization, collagenization and decreased polymorphonuclear and eosinophil cell infiltration (13). Topical phenytoin was reported to eliminate Staphylococcus aureus, E. coli, Klebsiella spp. and Pseudomonas spp. from wounds within 7-9 days (14, 15). The effectiveness of topical phenytoin in wound-bed preparation (WBP) for split thickness skin grafting has been examined in 16 patients with large diabetic foot ulcers. Topical phenytoin (10% w/w ointment) was applied for 2-8 weeks prior to performance of autografting. The authors conclude that phenytoin ointment is a safe and efficacious treatment to enhance the survival of split-thickness skin grafts in large chronic diabetic ulcers (16). Absoul-Younes et al examined in rats the effectiveness of topical phenytoin in preserving the skin viability and increasing acceptance rate of autograft. Twenty-one rats were treated with phenytoin (10% w/w ointment) while the other 21 (control) were treated with standard dressing and vaseline. An autograft was performed one week after treatment. Phenytoin appears to be an effective method for enhancing the take of the full-thickness skin graft (17).
Phenytoin also showed a facilitation of nerve regeneration and used both topically or systemically in some dermatological disorders. As the drug has been shown to significantly suppress mitogeninduced activation of lymphocytes and cytotoxic T lymphocyte activity, it polarizes the immune response toward the type-2 pathway and significantly decreases suppressor T cells while increasing the helper/suppressor ratio. At high concentrations, the drug inhibits the release of norepinephrine and the activity of MAO. Moreover, phenytoin is suggested to interact with membrane lipids, which may promote stabilization of the membrane exerting a direct stimulatory action on melanocytes promoting the disappearance of vitiligo affecting dermatologic areas. Soft tissue wounds such as leprosy trophic ulcers, bedsores, diabetic foot ulcers, burns, traumatic wounds, venous stasis ulcers and abscesses could be treated with topical phenytoin, which resulted potentially useful in healing a wide variety of wounds. Appearing a “very important application”, topical use of phenytoin for wound healing is within the guidelines set forth by the FDA. Our clinical studies using topical phenytoin therapy suggest, in comparison to similar patients treated with placebo, that phenytoin treatment may be useful for the treatment of bedsores, usually suffered during the old age, but mainly related to traumatic diseases, which are linked to a long period of immobility in bed.
References
- 1.Kimball OP, Horan TN. The use of Dilantin in the treatment of epilepsy. Ann Intern Med. 1939;13:787–93. [Google Scholar]
- 2.Bhatia A, Prakash S. Topical phenytoin for wound healing. Dermatology Online Journal. 2004;10(1):5. [PubMed] [Google Scholar]
- 3.Shapiro M. Acceleration of gingival wound healing in nonepileptic patients receiving diphenylhydantoin sodium. Exp Med Surg. 1958;16:41–53. [PubMed] [Google Scholar]
- 4.Goebil RW. Sodium diphenylhydantoin association with oral healing. J Oral Surg. 1972;30:191–5. [PubMed] [Google Scholar]
- 5.Shafer WG, Beatty RE, Davis WB. Effect of Dilantin sodium on tensile strength of healing wounds. Proc Soc Exp Biol Med. 1958;98:348–50. doi: 10.3181/00379727-98-24040. [DOI] [PubMed] [Google Scholar]
- 6.Teo SY, Yew MY, Lee SY, Rathbone MJ, Gan SN, Coombes AG. In vitro evaluation of novel phenytoin-loaded alkyd nanoemulsions designed for application in topical wound healing. J Pharm Sci. 2016 doi: 10.1016/j.xphs.2016.06.028. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 7.Hemmati AA, Forushani HM, Asgari HM. Wound healing potential of topical amlodipine in full thickness wound of Rabbit. Hundishapur J Nat Pharm Prod. 2014;9(3):E 15368. doi: 10.17795/jjnpp-15638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moy LS, Tan EML, Holness R, Uitto J. Phenytoin modulates connective tissue metabolism and cell proliferation in human skin fibroblast cultures. Arch Dermatol. 1985;121:79–83. [PubMed] [Google Scholar]
- 9.Shaw J, Hughes CM, Lagan KM, Bell PM. The clinical effect of topical phenytoin on wound healing: a systematic review. Br J Dermatol. 2007;157(5):997–1004. doi: 10.1111/j.1365-2133.2007.08160.x. [DOI] [PubMed] [Google Scholar]
- 10.Muthukumarasamy MG, Sivakumar G, Manoharan G. Topical phenytoin in diabetic foot ulcers. Diabetes Care. 1991;14:909–11. doi: 10.2337/diacare.14.10.909. [DOI] [PubMed] [Google Scholar]
- 11.Pendse AK, Sharma A, Sodani A, Hada S. Topical phenytoin in wound healing. Int J Dermatol. 1993;32:214–7. doi: 10.1111/j.1365-4362.1993.tb02799.x. [DOI] [PubMed] [Google Scholar]
- 12.Oluwatosin OM, Olabanji JK, Oluwatosin OA, Tijani LA, Onyechi BA. A comparison of topical honey and phenytoin in the treatment of chronic leg ulcers. Afr J Med Med Sci. 2000;29:31–4. [PubMed] [Google Scholar]
- 13.Mendiola-Gonzalez JF, Espejo-Plascencia I, Chapa-Alvarez JR, Rodriguez-Noriega E. Sodium diphenylhydantoin in burns: effects on pain and healing (letter) Invest Med Int. 1983;10:449–51. [Google Scholar]
- 14.Yadav JK, Singhvi AM, Kumar N, Garg S. Topical phenytoin in the treatment of split-thickness skin autograft donor sites: a comparative study with polyurethane membrane drape and conventional dressing. Burns. 1993;19:306–10. doi: 10.1016/0305-4179(93)90118-r. [DOI] [PubMed] [Google Scholar]
- 15.Younes N, Albsoul A, Badran D, Obedi S. Wound bed preparation with 10-percent phenytoin ointment increases the take of split-thickness skin graft in large diabetic ulcers. Dermatol Online J. 2006;12(6):5. [PubMed] [Google Scholar]
- 16.Albsoul-Younes A, Younes NA, Badran DH. Topical phenytoin ointment increases autograft acceptance in rats. Saudi Med J. 2006;27(7):962–6. [PubMed] [Google Scholar]
- 17.Namazi MR. Phenytoin as a novel anti-vitiligo weapon. Journal of Autoimmune Diseases. 2005;2:11. doi: 10.1186/1740-2557-2-11. doi:10.1186/1740-2557-2-11. [DOI] [PMC free article] [PubMed] [Google Scholar]


