Short abstract
Objective
The use of wide-awake local anesthesia with no tourniquet (WALANT) is becoming an excellent alternative for elective hand surgeries and hand surgeries involving minor trauma. Although the use of WALANT for some soft tissue surgeries has become the state of the art, data regarding bony procedures, such as fracture management, under WALANT are limited. This study was performed to assess the WALANT technique for open reduction and internal fixation of distal radius fractures.
Methods
Five patients with displaced distal radius fractures were enrolled in the study. WALANT was carried out about 30 minutes prior to the first incision. Surgery was performed in the normal fashion, and the fractures were fixed using anatomic locking plates. After surgery, the patients were admitted overnight for observation and pain assessment, and they were discharged within 24 hours postoperatively. Intraoperative and postoperative complications were recorded. Follow-up was performed in our outpatient clinic. No abnormalities were recorded.
Results
All patients underwent a successful painless surgery. No extra bleeding or other complications were recorded.
Conclusion
The WALANT technique offers a simple and safe alternative to traditional anesthetic techniques for open reduction and plating of distal radius fractures.
Keywords: Distal radius fracture, epinephrine, lidocaine, wide-awake local anesthesia, open reduction and internal fixation, anesthesia
Introduction
Distal radius fractures are the most common upper extremity fractures in adults.1 The indications for operative management continue to evolve based on outcomes from the most recent clinical studies. Advancements during the past decade have expanded the variety of available fixation options; however, the clinical superiority of a particular treatment modality remains without consensus.2 General anesthesia and regional nerve blocks have been described as anesthetic techniques for open reduction and internal fixation of distal radius fractures.3 The Bier block was also described as an alternative for anesthesia in upper limb surgeries with some limitations.4 The use of wide-awake local anesthesia with no tourniquet (WALANT) was described by Donald H. Lalonde for many elective hand and wrist elective and for surgeries involving minor trauma, such as tendon ruptures and phalangeal and metacarpal fractures.5–7 The technique has become popular in the last decade and appears to be a safe and effective anesthetic technique for many hand and wrist surgeries. Patient satisfaction is high because preoperative testing and hospital admission are not required. Postoperative recovery is rapid, and procedures can be performed in the outpatient setting, resulting in substantial savings in time and money.8 Additionally, anesthesiologists are unavailable in some institutions, and the experience with and results of regional blocks may be rather poor in these institutions. We performed a literature review and found no description of the use of WALANT for distal radius fractures. Therefore, the present study was performed to assess the use of the WALANT technique in five cases of open reduction and internal fixation (plating) of distal radius fractures.
Patients and methods
Five patients with displaced distal radius fractures that required surgery were enrolled in the study. Informed consent was obtained from all patients. Demographic data and fracture characteristics are shown in Table 1. The five patients presented to our emergency department with distal radius fractures; a cast was applied, and the patients were referred to our orthopedic department for operative treatment. WALANT was carried out in the waiting room about 30 to 40 minutes prior to the first incision. Surgery was carried out in the normal fashion, and the fractures were fixed using anatomic locking plates. After surgery, the patients were instructed to practice full range of movements. The patients were discharged within 24 hours postoperatively. No intraoperative or postoperative complications were recorded. Follow-up was performed in our outpatient clinic and included assessment of radiographs, range of motion, complications, and patient satisfaction.
Table 1.
Demographic data and fracture characteristics.
| Patient number | Age (years) | Side | Sex | Fracture type | Approach |
|---|---|---|---|---|---|
| 1 | 31 | L | Male | Volar Barton | Volar |
| 2 | 32 | R | Male | Volar Barton | Volar |
| 3 | 22 | L | Male | Smith | Volar |
| 4 | 52 | R | Male | Intra-articular, comminuted | Dorsal |
| 5 | 64 | L | Male | Dorsal “die punch” | Dorsal |
This study was approved by the local institutional review board.
Anesthetic technique
The injection solution was prepared prior to cast removal. The injected solution comprised 50 mL of 0.9% normal saline and 50 mL of 1% lidocaine with 1:1,000,000 epinephrine. The cast was removed and the hand was prepped using a sterile alcohol solution. We chose the surgical approach according to the fracture configuration, and this choice of approach eventually dictated the location of the injections. In Patients 1, 2, and 3, we chose the classic volar flexor carpi radialis (FCR) approach, whereas in Patients 4 and 5, we chose the dorsal approach. Although the locations of the injections are different for the volar and dorsal approaches, the principles remain the same.
Volar approach
The FCR was palpated under the skin, and points were marked using a sterile marker. In the same manner, the distal third of the radial bone was palpated, and four skin points were marked from about 10 cm proximal to the wrist crease and distal to the radial styloid process (Figure 1). Fifteen milliliters of the injection solution was subcutaneously injected along the course of the FCR (along the planned incision) and distal to the wrist crease.
Figure 1.
Skin marks: volar approach.
To eliminate pain and bleeding with bone maneuvers and drilling, adequate infiltration of the periosteum was performed as follows. At each radial skin point, 2 mL of the solution was injected subcutaneously. We then used the needle to palpate the bone, and 4 mL was injected volarly and 4 mL dorsally to the bone in a fan shape. The same technique was applied to all four radial skin points.
Because Patients 1 and 3 presented with a fracture of the ulnar styloid process, 3 mL of the solution was injected as a hematoma block directly into the ulnar styloid fracture site to diminish pain on hand maneuvers.
Dorsal approach
Lister’s tubercle and the extensor pollicis longus were palpated under the skin, and skin points were marked using a sterile marker. In the same manner, the distal third of the radius was palpated under the skin, and points were marked over the skin (Figure 2). Fifteen milliliters of the solution was subcutaneously injected along the course of the extensor pollicis longus (along the planned incision) and distally to the wrist joint. Injection over the distal radial third was performed in the same manner as for the volar approach, apart from the fact that less soft tissue was present between the skin and the radius dorsally and the dorsal periosteum was partially anesthetized by the dorsal injections; this resulted in injection of a smaller amount of material dorsally with injection mainly occurring over the radial aspect.
Figure 2.
Skin marks: dorsal approach.
Operative procedure
After 20 minutes, the injected area became rather pale with a yellowish appearance (Figure 3) and the patient entered the operating room. The hand was draped and wrapped in the normal fashion. All patients had a visual analogue scale score of 0 at the beginning of the surgery. A tourniquet was applied but not inflated. Three milligrams of midazolam was intravenously administered to Patient 1, and 1 mg was administered to Patient 3. We expected some inconvenience due to the motionless supine position in Patient 1; therefore, the midazolam was given prior to the first incision. Patient 3 expressed some inconvenience and complained of a backache after about 30 minutes. However, both patients were alert and cooperative during the entire procedure. Patient 4 described some pain dorsally in the radioulnar joint. Eight mg of pure 1% lidocaine was injected directly into the painful area, and surgery was continued without interruptions after 1 minute. Patients 2 and 5 were not given any further medication except for the described local injections. The surgeries were carried out in the normal fashion, and no excessive bleeding was recorded (Figures 4–6).
Figure 3.
Preoperative view: volar approach.
Figure 4.
First volar incision: volar approach.
Figure 5.
Intraoperative view: volar approach.
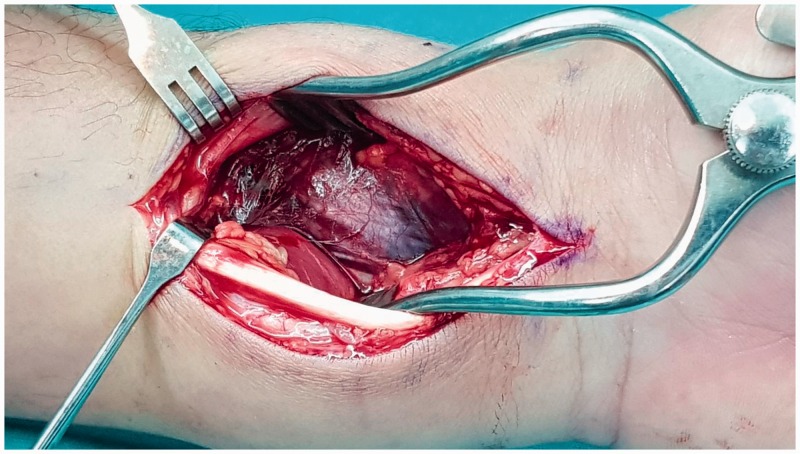
Figure 6.
Intraoperative view: dorsal approach.
After definitive fixation, the patients were asked to actively flex and extend their wrists and fingers to examine the stability of the fixation and identify any tendon disorders. Fracture fixation was stable, and no tendon abnormalities were noted. The skin was sutured and a soft dressing was applied.
Postoperative course
The patients returned to the orthopedic department for pain control and further supervision. Skin color, finger temperature, and capillary refill normalized. The patients were provided instructions by our hand therapist and discharged within 24 hours postoperatively. Postoperative follow-up was performed in our outpatient clinic, and no abnormalities were recorded.
Discussion
During the last decade, the use of WALANT has become widely accepted in hand surgery.6–8 Avoiding general anesthesia and sedation has many benefits, including no need for certain preoperative investigations, easier immediate postoperative patient recovery with no nausea or vomiting, a shorter hospital stay, and safe management of patients with multiple medical comorbidities such as morbid obesity and diabetes.9
The WALANT technique has been shown to be highly effective in carpal tunnel release,10,11 tendon repair,12,13 Dupuytren’s disease,14 trapeziectomy,9 tendon transfer,15 and finger fractures.16 Anesthesia for distal radius fractures traditionally includes a tourniquet and general or regional anesthesia with intravenous sedation. We performed a literature review and found no description of the use of WALANT anesthesia for open reduction and internal fixation of distal radius fractures.
Apart from the above-mentioned general advantages of WALANT,5–8 there might be some specific advantages of WALANT for open reduction and internal fixation of distal radius fractures. First, the patient is fully alert; therefore, the surgeon can test the stability of the fixation under physiological forces because the patient can actively flex and extend the wrist and fingers during the procedure. In addition, median nerve injury has been described as a consequence of volar plating of distal radius fractures17; using the WALANT technique, however, a median nerve block is not performed, and irritation of this nerve can therefore be identified intraoperatively. Flexor pollicis longus tendon rupture has been reported following volar plating of the distal radius.17,18 When performing WALANT surgery, tendon glide can be assessed under physiological tension, highlighting sites of potential tendon irritation.
We have herein described our technique for performing this procedure, which has not been specifically described for fractures of the distal radius. The widely quoted maximal dose of lidocaine with epinephrine is 7 mg/kg.19 Our patients weighed an average of 70 kg. Thus, we performed the following calculation: 7 mg/kg × 70 kg = 490 mg or 49 mL of 1% lidocaine with 1:1,000,000 epinephrine. Because a large area was to be covered, we diluted the solution with 50 mL of 0.9% normal saline. Overall, with the volar approach, about 15 mL of the solution was injected along the FCR course (over the planned skin incision), 40 mL was injected on the radial side of the radius for periosteal anesthesia, and 3 mL was injected to the ulna styloid fracture as a hematoma block. With the dorsal approach, as mentioned above, only 20 mL of the solution was injected on the radial aspect because of the thinner soft tissue layer between the skin and bone.
Some systemic adverse reactions should be taken into consideration while performing WALANT. Lidocaine is considered to have some cardiotoxic features,20 and anaphylactic shock as a consequence of lidocaine use has also been described.21 To prevent these adverse reactions, we kept the injected dosage within the “safe” range of 7 mg/kg.
Younge22 described compartment syndrome as a consequence of hematoma block for reduction of distal radius fractures. We did not expect compartment syndrome in our patients despite the large volume injected because, unlike hematoma block, our patients had undergone an open volar or dorsal approach with partial fasciotomy of the forearm. In addition, to reduce the probability of compartment syndrome, adequate hemostasis was performed intraoperatively and no tourniquet was used. However, the risk of compartment syndrome remained a major concern because the volar and dorsal approaches involve only partial forearm decompression. Therefore, adequate postoperative monitoring was performed, and no complications occurred.
There are some absolute limitations to our experience that should be emphasized before applying our technique to other distal radius fractures. The patient must be aware of the procedure and its consequences, including the drilling background noise and discomfort of being motionless while lying supine for a long period of time. Patient cooperation is highly important, and patients should be selected carefully.
Ahmad and Ikram23 thoroughly described the WALANT technique for isolated ulnar shaft fractures. However, WALANT is dictated by the fracture pattern; therefore, different fractures require different techniques that should be described separately. Regardless of whether the fragments were displaced volarly or dorsally, we noticed that fractures in which displacement of intra-articular fragments was the main component were easier to anesthetize than fractures in which displacement was mainly extra-articular and eccentric maneuvers were required to reduce the fracture. More complex distal radius fractures may require different anesthetic techniques, such as volar, dorsal, and radial injections.
Above all, the main limitation of our study is the small group of patients. Therefore, further experience and data are required.
In conclusion, our study provides a description of an easily applied, safe, and efficient anesthetic technique for open reduction and internal fixation of distal radius fractures. This technique might be a useful alternative to the traditional anesthetic technique, especially in patients with comorbidities or when an anesthesiologist is not available.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Mosenthal WP, Boyajian HH, Ham SA, et al. Treatment trends, complications, and effects of comorbidities on distal radius fractures. Hand (N Y) 2018; ▪: 1558944717751194. doi: 10.1177/1558944717751194. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alluri RK, Hill JR, Ghiassi A. Distal radius fractures: approaches, indications, and techniques. J Hand Surg Am 2016; 41: 845–854. [DOI] [PubMed] [Google Scholar]
- 3.Egol KA, Soojian MG, Walsh M, et al. Regional anesthesia improves outcome after distal radius fracture fixation over general anesthesia. J Orthop Trauma 2012; 26: 545–549. [DOI] [PubMed] [Google Scholar]
- 4.Haghighi M, Mardani-Kivi M, Mirbolook A, et al. A comparison between single and double tourniquet technique in distal upper limb orthopedic surgeries with intravenous regional anesthesia. Arch Bone Jt Surg 2018; 6: 63–70. [PMC free article] [PubMed] [Google Scholar]
- 5.Al Youha S, Lalonde DH. Update/review: changing of use of local anesthesia in the hand. Plast Reconstr Surg Glob Open 2014; 2: e150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lalonde D, Bell M, Benoit P, et al. A multicenter prospective study of 3,110 consecutive cases of elective epinephrine use in the fingers and hand: the Dalhousie project clinical phase. J Hand Surg Am 2005; 30: 1061–1067. [DOI] [PubMed] [Google Scholar]
- 7.Lalonde D, Martin A. Tumescent local anesthesia for hand surgery: improved results, cost effectiveness, and wide-awake patient satisfaction. Arch Plast Surg 2014; 41: 312–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Steiner MM, Calandruccio JH. Use of wide-awake local anesthesia no tourniquet in hand and wrist surgery. Orthop Clin North Am 2018; 49: 63–68. [DOI] [PubMed] [Google Scholar]
- 9.Farhangkhoee H, Lalonde J, Lalonde DH. Wide-awake trapeziectomy: video detailing local anesthetic injection and surgery. Hand (N Y) 2011; 6: 466–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lalonde DH. “Hole-in-one” local anesthesia for wide-awake carpal tunnel surgery. Plast Reconstr Surg 2010; 126: 1642–1644. [DOI] [PubMed] [Google Scholar]
- 11.Leblanc MR, Lalonde J, Lalonde DH. A detailed cost and efficiency analysis of performing carpal tunnel surgery in the main operating room versus the ambulatory setting in Canada. Hand (N Y) 2007; 2: 173–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Higgins A, Lalonde DH, Bell M, et al. Avoiding flexor tendon repair rupture with intraoperative total active movement examination. Plast Reconstr Surg 2010; 126: 941–945. [DOI] [PubMed] [Google Scholar]
- 13.Lalonde D, Higgins A. Wide awake flexor tendon repair in the finger. Plast Reconstr Surg Glob Open 2016; 4: e797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nelson R, Higgins A, Doumit J, et al. Erratum to: the wide-awake approach to Dupuytren’s disease: fasciectomy under local anesthetic with epinephrine. Hand (N Y) 2010; 5: 213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lalonde DH. Wide-awake extensor indicis proprius to extensor pollicis longus tendon transfer. J Hand Surg Am ▪; 39: 2297–2299. [DOI] [PubMed] [Google Scholar]
- 16.Gregory S, Lalonde DH, Fung Leung LT. Minimally invasive finger fracture management: wide-awake closed reduction, K-wire fixation, and early protected movement. Hand Clin 2014; 30: 7–15. [DOI] [PubMed] [Google Scholar]
- 17.Rampoldi M, Marsico S. Complications of volar plating of distal radius fractures. Acta Orthop Belg 2007; 73: 714–719. [PubMed] [Google Scholar]
- 18.Tarallo L, Mugnai R, Zambianchi F, et al. Volar plate fixation for the treatment of distal radius fractures: analysis of adverse events. J Orthop Trauma 2013; 27: 740–745. [DOI] [PubMed] [Google Scholar]
- 19.Lalonde DH, Wong A. Dosage of local anesthesia in wide awake hand surgery. J Hand Surg Am 2013; 38: 2025–2028. [DOI] [PubMed] [Google Scholar]
- 20.Horacek M, Vymazal T. Lidocaine not so innocent: cardiotoxicity after topical anaesthesia for bronchoscopy. Indian J Anaesth 2012; 56: 95–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Specjalski K, Kita-Milczarska K, Jassem E. The negative predictive value of typing safe local anesthetics. Int Arch Allergy Immunol 2013; 162: 86–88. [DOI] [PubMed] [Google Scholar]
- 22.Younge D. Haematoma block for fractures of the wrist: a cause of compartment syndrome. J Hand Surg Br 1989; 14: 194–195. [DOI] [PubMed] [Google Scholar]
- 23.Ahmad AA, Ikram MA. Plating of an isolated fracture of shaft of ulna under local anaesthesia and periosteal nerve block. Trauma Case Rep 2017; 12: 40–44 [DOI] [PMC free article] [PubMed] [Google Scholar]