Abstract
Objective:
We conducted our study involving 1400 peri- and post-menopausal women who live in a slum area of Mumbai to determine the prevalence of osteoporosis, awareness about osteoporosis, education (knowledge regarding osteoporosis), treatment and prevention of osteoporosis.
Material and Methods:
A detailed medical, surgical, obstetrical & gynecological, menstrual, and drug history was recorded in a predesigned questionnaire designated for the study. Height and weight and body mass index were measured, physical activity level especially load bearing exercise was recorded, and amount of sunlight exposure per day was also recorded. Food intake was estimated using the 24 h dietary recall method and calcium and Vitamin D consumption pattern was assessed. We used calcaneum quantitative ultrasound to assess bone mineral density (BMD) for such large population.
Results:
The prevalence of low BMD was found in more than half of this population (81%). The mean age in Group I was found to be 36.50 ± 2.74 years as compared to 37.5 ± 3.44 years in Group II with low BMD, which was statistically significant (P = 0.02). The average age at menopause was 51.62 ± 5.72 years in Group I and 49.43 ± 4.52 years in Group II. The number of children and type of menopause has been found to be associated with low BMD in our study. Lack of physical exercise and low-calcium diet were significantly associated with low BMD.
Conclusion:
Our study showed that there is a high prevalence of Vitamin D deficiency and Osteoporosis even in adult women who live in a slum area. The findings from the study also suggest the need for large community-based studies so that high-risk population can be picked up early and early interventions and other lifestyle changes can be instituted so that no delay in implementing state and national or international health policy to tackle this increasing global health problem. The public awareness is important, and strategies to identify and manage low BMD in the primary care setting needs to be established and implemented.
KEYWORDS: Bone mineral density, calcaneum ultrasound, calcium, menopause, osteoporosis, quantitative ultrasound
INTRODUCTION
Osteoporosis is a systematic bone disease characterized by low bone mass and deterioration of microarchitecture of the bone, leading to bone fragility and eventually fractures. It is invariably associated with Vitamin D deficiency which is most common and pandemic, and it is the most under-diagnosed and under-treated nutritional deficiency in the world.[1,2,3] Vitamin D deficiency is widespread especially in developing country like India, and it is irrespective of their age, sex, race, and geography. Vitamin D is photosynthesized in the skin on exposure to ultraviolet B rays. Sun exposure alone is not sufficient for Vitamin D sufficiency. Vitamin D deficiency is widely prevalent in Indian population despite of adequate sun exposure. The sun exposure and inadequate calcium and Vitamin D intake and lack of physical activity are major causes of development of osteoporosis. It is a major global public health problem associated with significant morbidity, mortality, and socioeconomic burden. Osteoporosis is defined as a skeletal disorder characterized by low bone strength, leading to an increased risk of fragility fractures. The greatest bone loss occurs in women mainly during perimenopause and is associated with estrogen insufficiency. SRL Diagnostics has released a 3-year long pan-India data mining survey from 2012 to 2014 on Vitamin D and found that about 80.63% had Vit D deficiency in approximate 73 lakh samples of men screened during this period. Eastern part of India had the highest with 86.6% being detected with lower levels of Vitamin D while northern and southern part had 81.3% and 85.6%, respectively. However western part of India showed the lowest percentage of abnormality with 69.8%. According to the World Health Organization, osteoporosis is second tocardiovascular disease as a global health problem as it is silent and insidious in nature. According to WHO statistics, one out of eight men and one out of three women in India are affected by osteoporosis.[4]
Vitamin D deficiency has an effect not only on skeletal but also on extraskeletal diseases. Because of its multifarious implications on health, the epidemic of Vitamin D deficiency in India is likely to significantly contribute to the enormous burden on the health-care system of India. The main reason for lack of sun exposure in India is cultural and social taboos which often dictate lifestyle patterns such as clothing that may limit sun exposure. Many studies indicate that most Indians are vegetarians either by choice or bonded by custom and culture which limits vitamin D-rich dietary options. The socioeconomically backward people comprises of a large percentage of the population in India which lives in a village or outskirt of major cities. The underprivileged people usually suffer from overall poor and inadequate nutrition. Vitamin D-rich dietary sources are limited and unaffordable to most Indians, and also they do not know about the same. There are multiple Vit D supplements available, but most Indians are not aware that they need additional Vitamin D. A survey done by the National Health and Nutrition Examination-III, an estimated 14 million American women over the age of 50 years are affected by low density at the hip. The prevalence of osteoporosis increases with age for all sites, and by the World Health Organization (WHO) definition, up to 70% of women over the age of 80 years have osteoporosis.[5] Since Indian subcontinent is located between 8.4° and 37.6°N latitude, majority of the population living here experience good and adequate sunlight throughout the year and Vitamin D through this adequate sun exposure. Expert groups estimated the number of osteoporosis patients in India at approximately 26 million (by 2003), with the numbers projected to increase to 36 million by 2013.[6] Osteoporosis has numerous medical and surgical implications and imposes a huge economic burden on the family. Hence, it is of utmost importance that citizens, government, and health organization take immediate steps to create awareness, treatment, and prevention of this silent disease.
MATERIAL AND METHODS
In our study, a total of 1400 women aged between 23–50 years who live in a slum area of Mumbai, India were included in the study. The study was conducted in the biggest slum area (Dharavi) in Mumbai, India, with collaboration with INHS Asvini Colaba Mumbai, India, between January 2017 and July 2017. Informed consent was obtained from them, and they participated in the study on a voluntary basis. Total, 1650 women were randomly selected, and finally, 1400 women were included in the study as rest of them were excluded as they did not fulfill the inclusion criteria.
Inclusion criteria were as follows:
Age group 23–50 years
Married otherwise healthy woman.
Exclusion criteria were as follows:
Woman suffering from renal diseases, rheumatoid arthritis, diabetes mellitus, chronic liver disease, chronic malabsorption syndrome, current or past treatment with glucocorticosteroids, oral contraceptive pills, and thyroid hormones, hormone replacement therapy
Any medication that interferes with calcium and Vitamin D metabolism such as diuretic, digoxin
Pregnancy, documented osteoporosis, or osteopenia
Neurological condition and nonambulatory women.
A detailed medical, surgical, obstetrical and gynecological, menstrual, and drug history was recorded in a proforma designated for the study. Particular focus was laid on the medical conditions such as renal diseases, diabetes mellitus, hyperparathyroidism, rheumatoid arthritis, chronic liver disease, chronic malabsorption syndrome, current or past treatment with steroids, hypo and hyper-thyroidism, use of oral contraceptive pills and hormone replacement therapy. Information regarding history of fracture, repeated history of fracture on trivial fall, family history of fracture, osteoporosis, socioeconomic status, educational level, occupation, and load-bearing exercises was noted. Load bearing exercise was assessed by inquiring about regular weight-bearing exercise for the past 2 years, and the number of sessions of weight-bearing exercise of at least 30 min was noted. Their physical standard was noted in the form of height, and weight was measured by a trained person, with the women in light cloth and without footwear. Body mass index (BMI) was calculated using the formula: weight (kg)/height (cm)2. Data regarding sunlight exposure in a day for each woman were noted using the (rules of nines) Barger-Lux-Heaney index (sun index = hours of sun exposure in a week multiply by a fraction of body surface area exposed to sunlight); this was further classified as low, medium, and high sun exposure.[7] Food intake was estimated using the 24 h dietary recall method, and nutrients of each meal were assessed by applying the Indian database of nutritive value of each cooked food.[8] Calcium and Vitamin D intake in diet was assessed using a short food frequency questionnaire.
Quantitative ultrasound (QUS) is a bone health assessment technique which has gained much popularity in recent years since its introduction in 1984. Compared to dual-X-ray absorptiometry (DXA), QUS offers wider accessibility to the public because it is portable, easier to handle, lower in cost and does not emit ionizing radiation. This technology has been used to determine the bone health status in women, men, and children and certain cases, infants. We have used the same QUS in our study. The QUS scanner used in this study was a UBIS 5000 bone sonometer (Diagnostic Medical Systems, Montpellier, France), with a center frequency of 0.5 MHz and broadband emission capability with a frequency range of 200–600 kHz). Women were considered at moderate risk if T–score was between < −1 and −2.5 and at high risk if T–score was < −2.5, as per WHO classification. After finishing the test, the women were informed about the results of their investigations and counseled regarding risk of the development of osteoporosis and its complication. The public education regarding the screening results and standard information on dietary recommendations and lifestyle modification was provided to them based on the National Osteoporosis Foundation guidelines.[9] Women found to have osteopenia and osteoporosis were treated by the endocrinologist and orthopedic surgeons.
Statistical analysis
In our study, data were calculated as percentage and mean (standard deviation [SD]). Student's t-test was applied to examine the differences in the prevalence of osteoporosis. Multiple logistic regression analysis was used for associations between osteoporosis and data presented as odds ratio and 95% confidence intervals. Associations were considered statistically significant when P < 0.05.
All statistical analyses were performed using SPSS version 19 statistical package (Chicago, IL, USA).
RESULTS
In our study, out of 1400 women studied, 1135 (81%) were found to have low BMD (osteopenia and osteoporosis). These low-BMD women were grouped as Group II in the analysis. Whereas women with normal BMD were placed in Group I. The prevalence of low BMD was found in alarming (81%).
The mean age in Group I was found to be 36.50 ± 2.74 years as compared to 37.5 ± 3.44 years in Group II with low BMD, which was statistically significant (P = 0.02). The average age at menopause was 51.62 ± 5.72 years in Group I and 49.43 ± 4.52 years in Group II. The average period since menopause was 5.8 ± 4.8 years in Group I and 5.06 ± 3.3 years in Group II. The two groups were similar with respect to parity, socioeconomic status, education, number of children, family history of osteoporosis, thyroid disorders, and hormone replacement therapy. None had a previous history of bone fractures. Mean age at menarche was 13.3 ± 1.9 years and 14.3 ± 1.8 years in Group I and Group II, respectively as shown in Table 1. About 69.5% of women in Group I and 54.9% of women in Group II had low physical activity, and there was no statistically significant difference in sunlight exposure between the groups as all were living in the same slum with equal sunlight exposure.
Table 1.
Demographic characteristics
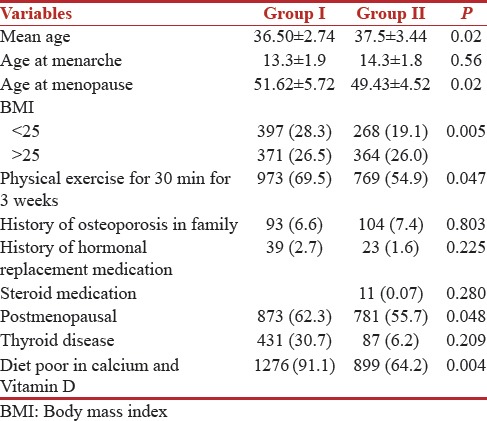
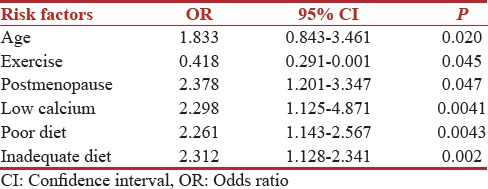
In our study population, the mean calorie and protein intake were 1012 ± 354 kcal and 28.01 ± 11.36 g, respectively, in Group I and 1346 ± 351 kcal and 29.48 ± 11.36 g, respectively, in Group II. About 48.35% of the women in Group I and 32.81% of the women in Group II had their total calorie intake below the recommended dietary intakes, while 34.81% of the women in Group I and 32.34% of the women in Group II had their total protein intake below the recommended protein intakes. The mean calcium intake for Group I and Group II was 214 ± 176 mg/day and 301 ± 158 mg/day, respectively. About 92.34% of the women in Group I and 87.12% of the women in Group II had calcium intake below the recommendations for daily intakes (RDIs), because of low economical status and poor and inadequate diet intake. Osteoporosis and osteopenia of lumbar spine, femoral neck, and total spine (T–score <−2.5 and T–score between −1 and −2.5) was seen in 89.49% (n = 1252) of the affected population. The prevalence of osteoporosis was seen to be high with increasing age and low BMD. The number of children and type of menopause was seen to have much association with low BMD in our study because women eat in last after all members have eaten. In our study population, lack of physical exercise and low-calcium diet were significantly associated with low BMD in women. In our study population, it was interesting to note that more number of patients in the premenopausal age group was found to be having low BMD than the postmenopausal women in this population. Multiple logistic regression analysis showed that age, menopause, physical exercise, and low-calcium diet acted as significant predictors of low bone density as shown in Table 2.
Table 2.
Multiple logistic regression analysis of risk factors considered in our study
In our study, that revealed a prevalence of osteoporosis in 81% and osteopenia in 19% of females in age between 23–50 years when measured by Calcaneum QUS [Figure 1].
Figure 1.
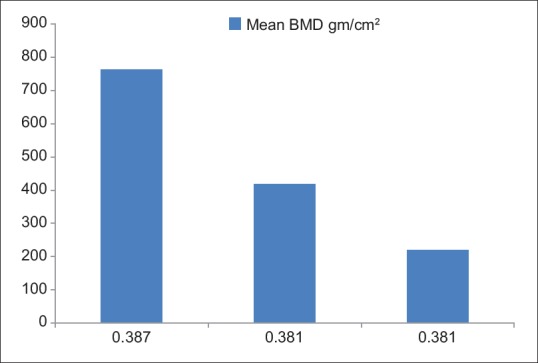
Number of women and mean bone mineral density
In 762 (54.4%) women, BMD g/cm2 was 0.387 ± 0.034 and the T–score was 0.21 ± 1.41 as shown in Table 3.
Table 3.
Number of patients and mean BMD

In 419 (29.9%) women, the BMD g/cm2 was 0.381 ± 0.089 with the T–score of 1.09 ± 2.97, and in remaining 219 (15.6%) women the BMD g/cm2 was 0.342 ± 0.025 and the calculate T–score was 1.93 ± 1.25.
DISCUSSION
Osteoporosis is a now well-known systematic bone disease characterized by low bone mass and deterioration of microarchitecture of the bone, leading to bone fragility and eventually fractures. The gold standard method recommended by the WHO in the diagnosis of osteoporosis is DXA. By this method, osteoporosis is defined by a bone mineral density (BMD) lower than −2.5 SDs of the reference BMD of Caucasian women aged 20–29 years. This simplified definition of osteoporosis eases the physicians, orthopedician, and endocrinologist in diagnosing and initiating treatment for osteoporotic patients. However, there are several limitations of DXA which prevent it from being used in the mass screening of osteoporosis, which is currently a rising health-care medical condition in the developing countries.
Vitamin D deficiency is a very common endocrine and medical problem throughout the world. It has been predicted that one billion people throughout the world are Vitamin D deficient.[10] The prevalence of Vitamin D deficiency in the countries where food is enriched by Vitamin D is 1.6%–14.8%.[11] In other European countries, among middle-aged and elderly people, 59.6%[12] in Boston was 24.1%[13] and in Tunisia 47.6%[14] among young adults.
The prevalence of Vitamin D deficiency is much higher in Asia including India. About 30%–50% of people in India, Lebanon, and Turkey[10] and also 45.2% of females in China[15] were Vitamin D deficient.
In India, many studies have been done still the precise figures on the prevalence of osteoporosis are not available at present. However, it is estimated that more than 61 million Indians have osteoporosis; of these, 80% of patients are females.[13,16,17] In a study done by Pande et al.[18] an age-dependent decline in BMD was seen in both women and men over the age of 50 years. A large single- center study by Patni in 2010[19] in Jaipur, India was done to establish normative database for BMD in Indian population using Dual Energy X-ray Absorptiometry. This study showed that the mean Indian BMD is about 2 SDs lower than the western BMD.
Our study was a cross-sectional study to assess the prevalence of osteoporosis in a selected population in a selected locality, i.e., slum of Mumbai. In our study, it is clear that almost 81% of the women in peri- and post-menopausal age group were found to have low BMD. Other high-risk factors associated with low BMD were found to be low BMI, lack of physical exercise, poor diet, poor protein intake, poor dietary calcium intake, and multiple children and more so low economical status. The Indian Council of Medical Research recommendation for calcium and Vitamin D for Indian is much lower when compared to the RDI of developed nations.[20,21] Vitamin D sufficiency through sun exposure is untenable for most Indians, especially for those living in slums where congestion is big issue. Vitamin D (relatively) rich dietary sources are unaffordable and mostly limited in low socioeconomical strata people. Most women living in slum are vegetarians as they cannot afford nonvegetarian diet. Vitamin D supplements are unaffordable and not feasible and beyond their reach. Fortification of widely consumed staple foods with Vitamin D is the only viable option towards attaining Vitamin D sufficiency in slums.
Many studies in the literature showed that the most important determinants of bone health are BMI which is again significantly lower in Indian women especially in lower socioeconomical status and even in the affluent category also as compared to developed country. Osteoporosis is extensively studied in the literature and many factors affect its development. Increasing age, especially when women become postmenopausal, low education level, frequent childbirth, low socioeconomic status, low education, and poor dietary intake have been associated with higher prevalence of osteoporosis. In developed countries also, still there is no formally accepted policy for population screening to identify individuals with osteoporosis. Patients are being detected using a case to case basis finding strategy based on a previous fragility fracture of distal radius, hip or the presence of significant clinical risk factors. Some of the risk factors act independently of BMD to increase fracture risk, whereas others increase fracture risk through their association with low BMD.[22]
The prevalence of osteoporosis in our study was found to be very high (81%) in peri- and post-menopausal women who were living in slum of Mumbai. There was a significant positive correlation between increasing age, low-calcium intake, low BMI, lack of physical exercise, and low BMD. Thus, the high prevalence of osteoporosis in peri- and post-menopausal women is a major health concern in low economical strata. Although no symptoms occur before fall or fracture following trivial injury or accidental detected because X-ray was taken for some other reason. In these populations, BMD and other risk factors can be used to identify high-risk patients, and because effective interventions exist, many of these fractures can be preventable. The implementation of the WHO technical report, assessment of osteoporosis at primary health care level, and the related web-based FRAX tool are the major milestones toward helping health professionals worldwide to improve identification of patients at high risk of fractures.[23] A risk assessment tool for osteoporosis developed by Sharma and Khandelwal[24] can be effective in a resource-poor and developing country like India, where they used a combination of questionnaire and ultrasonic measurement of BMD. In a recent study done by Nikose S, in 2015 a total of 3532 female patients were screened. In their study, it was noted that the a significant study population had lower BMD score, which suggest osteoporosis and had statistically significant correlation with their socioeconomic status, literacy rate, and emotional family backup.[25] Although DEXA scan is considered as a gold standard for BMD assessment, most of the Indian population is not covered under any kind of health insurance and so they cannot afford it due to the cost involved.
Although many studies have been published region wise in India that recommend regular screening of this silent epidemic but still it is not effective on ground as many women do not know the entity due to poor literacy rate and poor family support. In our study, it was observed that the women eat in the last whatever left at the end, after feeding husband, children, and in-laws if living together. This practice was deeply embedded in her mind that in spite of repeated advised and counseling it was very difficult to change.
CONCLUSION
Based on the study, we were able to identify a large problem for peri- and post-menopausal Indian women who live in slums and as a consequence a challenge for public health planners. It is, therefore, necessary to create awareness among these women, irrespective of their geographic location, about the risk of osteoporosis and educate those regarding preventive measures to avoid fractures secondary to osteoporosis and can avoid economical burden especially where there is no health insurance. There is also a need for large community-based studies so that high-risk population can be picked up, and early interventions such as awareness about this silence disease, adequate calcium intake, Vitamin D supplementation, and other lifestyle changes can be instituted if there is delay or even nonimplementation of state, national, or international health program to tackle this increasing global health problem.
QUS technology emerges as a convenient tool for osteoporosis screening for a large population. It provides additional information on bone microarchitectures as well as BMD. Several studies in the literature have indicated that it can predict fractures for both genders. In developing country like India with poor accessibility to DXA, QUS could be used as cost-effective screening tool for early detection of osteoporosis. Early detection would allow preventive measures to be taken to hinder the progression of the osteoporosis.
Limitation of study
This study was a cohort study without any follow-up, preventive, and therapeutic measures.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.van der Meer IM, Middelkoop BJ, Boeke AJ, Lips P. Prevalence of Vitamin D deficiency among Turkish, Moroccan, Indian and sub-Sahara African populations in Europe and their countries of origin: An overview. Osteoporos Int. 2011;22:1009–21. doi: 10.1007/s00198-010-1279-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van Schoor NM, Lips P. Worldwide Vitamin D status. Best Pract Res Clin Endocrinol Metab. 2011;25:671–80. doi: 10.1016/j.beem.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 3.National Institute of Nutrition. Dietary Guidelines for Indians – A Manual. Hyderabad, India: Indian Council of Medical Research; 1998. [Google Scholar]
- 4.Mithal A, Wahl DA, Bonjour JP, Burckhardt P, Dawson-Hughes B, Eisman JA, et al. Global Vitamin D status and determinants of hypovitaminosis D. Osteoporos Int. 2009;20:1807–20. doi: 10.1007/s00198-009-0954-6. [DOI] [PubMed] [Google Scholar]
- 5.High Prevalence of Osteoporosis among Indian Men: Survey, PTI. [Last updated on 2017 Jul 14]. Available from: https://food.ndtv.com/health/highprevalence-of-osteoporosis-among-indian-men-survey-1215079 .
- 6.Gupta A. Osteoporosis in India – The nutritional hypothesis. Natl Med J India. 1996;9:268–74. [PubMed] [Google Scholar]
- 7.Barger-Lux MJ, Heaney RP. Effects of above average summer sun exposure on serum 25-hydroxyvitamin D and calcium absorption. J Clin Endocrinol Metab. 2002;87:4952–6. doi: 10.1210/jc.2002-020636. [DOI] [PubMed] [Google Scholar]
- 8.Chiplonkar SA, Agte VV. Extent of error in estimating nutrient intakes from food tables versus laboratory estimates of cooked foods. Asia Pac J Clin Nutr. 2007;16:227–39. [PubMed] [Google Scholar]
- 9.National Osteoporosis Foundation. Physician's Guide to Prevention and Treatment of Postmenopausal Osteoporosis. Washington DC, USA: National Osteoporosis Foundation; 2003. [Google Scholar]
- 10.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–81. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 11.Lips P. Which circulating level of 25-hydroxyvitamin D is appropriate? J Steroid Biochem Mol Biol. 2004;89-90:611–4. doi: 10.1016/j.jsbmb.2004.03.040. [DOI] [PubMed] [Google Scholar]
- 12.Souberbielle JC, Cormier C, Kindermans C, Gao P, Cantor T, Forette F, et al. Vitamin D status and redefining serum parathyroid hormone reference range in the elderly. J Clin Endocrinol Metab. 2001;86:3086–90. doi: 10.1210/jcem.86.7.7689. [DOI] [PubMed] [Google Scholar]
- 13.Gordon CM, DePeter KC, Feldman HA, Grace E, Emans SJ. Prevalence of Vitamin D deficiency among healthy adolescents. Arch Pediatr Adolesc Med. 2004;158:531–7. doi: 10.1001/archpedi.158.6.531. [DOI] [PubMed] [Google Scholar]
- 14.Meddeb N, Sahli H, Chahed M, Abdelmoula J, Feki M, Salah H, et al. Vitamin D deficiency in Tunisia. Osteoporos Int. 2005;16:180–3. doi: 10.1007/s00198-004-1658-6. [DOI] [PubMed] [Google Scholar]
- 15.Du X, Greenfield H, Fraser DR, Ge K, Trube A, Wang Y, et al. Vitamin D deficiency and associated factors in adolescent girls in Beijing. Am J Clin Nutr. 2001;74:494–500. doi: 10.1093/ajcn/74.4.494. [DOI] [PubMed] [Google Scholar]
- 16.Rao H, Rao N, Sharma LR. A clinical study of bone mineral density using heel ultra-densitometer in Southern Maharashtra. Indian J Orthop. 2003;37:9. [Google Scholar]
- 17.Joshi VR, Mangat G, Balakrishnan C, Mittal G. Osteoporosis – Approach in Indian scenario. J Assoc Physicians India. 1998;46:965–7. [PubMed] [Google Scholar]
- 18.Pande KC, Veeraji E, Pande SK. Normative reference database for bone mineral density in Indian men and women using digital X-ray radiogrammetry. J Indian Med Assoc. 2006;104:288–91. [PubMed] [Google Scholar]
- 19.Patni R. Normal BMD values for Indian females aged 20-80 years. J Midlife Health. 2010;1:70–3. doi: 10.4103/0976-7800.76215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Institute of Nutrition. Dietary Guidelines for Indians. Hyderabad, India: Indian Council of Medical Research; 1998. [Google Scholar]
- 21.Omdahl JL, Garry PJ, Hunsaker LA, Hunt WC, Goodwin JS. Nutritional status in a healthy elderly population: Vitamin D. Am J Clin Nutr. 1982;36:1225–33. doi: 10.1093/ajcn/36.6.1225. [DOI] [PubMed] [Google Scholar]
- 22.Compston J, Cooper A, Cooper C, Francis R, Kanis JA, Marsh D, et al. Guidelines for the diagnosis and management of osteoporosis in postmenopausal women and men from the age of 50 years in the UK. Maturitas. 2009;62:105–8. doi: 10.1016/j.maturitas.2008.11.022. [DOI] [PubMed] [Google Scholar]
- 23.Kanis JA. WHO Collaborating Centre for Metabolic Bone Diseases. England, UK: University of Sheffield; 2008. On behalf of the World Health Organization scientific group. Assessment of osteoporosis at the primary health care level. [Google Scholar]
- 24.Sharma S, Khandelwal S. Effective risk assessment tools for osteoporosis in the Indian menopausal female. J Midlife Health. 2010;1:79–85. doi: 10.4103/0976-7800.76217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nikose S, Singh P, Khan S, Arora M, Taywade S, et al. Prevalence of osteoporosis in female population in rural central India [By Calcaneal Ultrasound] J Women's Health Care. 2015;4:262. [Google Scholar]


