To the Editor: Hyperhomocysteinemia (HHcy) is an important risk factor for atherothrombotic disease and venous thrombosis.[1] Normally, homocysteine (Hcy) is either remethylated to methionine (Met) by a Vitamin B12-dependent reaction or betaine as the methyl donor, or trans-sulfurated to cysteine through a pyridoxine-dependent reaction. Based on plasma level of total Hcy, HHcy is typically classified into three groups as follows: mild (tHcy 15–30 μmol/L), moderate (tHcy 30–100 μmol/L), and severe (tHcy >100 μmol/L).[2] Severe HHcy is rare and most commonly caused by inherited deficiency of cystathionine beta-synthase (CBS), or less frequently, of methylenetetrahydrofolate reductase (MTHFR) genes. The presentations of this metabolic disorder include developmental delay, intellectual disability, epilepsy, ectopia lentis, myopia, hypopigmentation of the skin and hair, marfanoid habitus, and thromboembolic disorders.[3] These manifestations are often overlooked in the early stage until the occur of thrombotic events like cerebral venous sinus thrombosis (CVST).
A 16-year-old boy was admitted because of intense global headache accompanied by nausea, vomiting, and generalized tonic-clonic seizure episodes for 7 months. Seven months ago (May 28, 2014), he started with complaints of headache. The symptoms gradually aggravated and he developed nausea and vomiting. In addition, he experienced frequent generalized tonic-clonic seizure episodes which lasted 2–3 min each, and occurred up to 4 times in a day. The interictal period lasted about half an hour, during which he remained in a subconscious state. Lumbar puncture indicated increased cerebrospinal fluid pressure (initial pressure >330 mmH2O). Brain magnetic resonance imaging (MRI) revealed diffuse abnormal signal over the splenium of the corpus callosum, bilateral frontal and parietal lobes, bilateral basal ganglia, and corona radiata [Figure 1a and 1b]. Magnetic resonance venography (MRV) revealed thrombosis in the straight sinus and right transverse sinus [Figure 1c and 1d]. Then, the diagnosis of CVST was established at local hospital. On treatment with low molecular weight heparin followed by oral warfarin, mannitol, phenobarbital, and sodium valproate, his symptoms improved gradually. During warfarin therapy, the international normalized ratio was within the therapeutic range 2–3. About 15 days ago (December 25, 2014), he developed insomnia, euphoria, talkative behavior, exaggerated expressions, and coupled with headache and dizziness. The MRV examination was performed at local hospital and the results were similar to the previous one. Diffuse abnormal signals over bilateral cerebral white matters, and multiple lacunar infarcts in the right frontal and parietal lobes were observed on MRI.
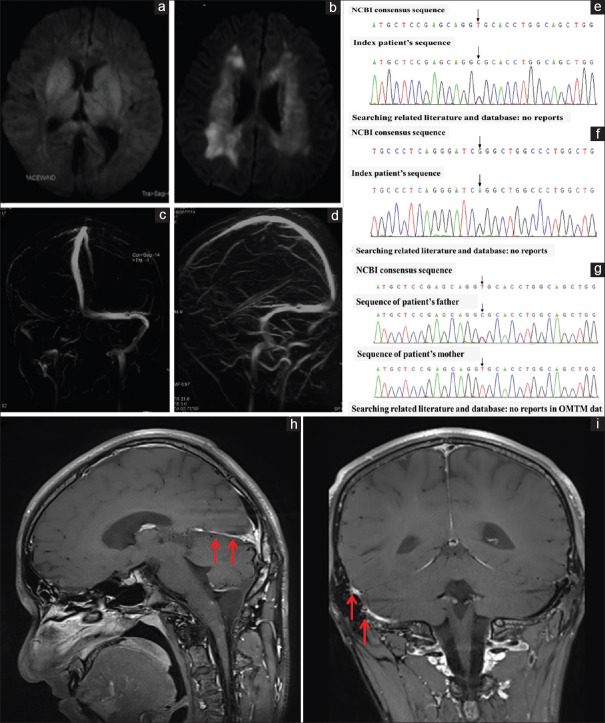
Figure 1.
Diffusion-weighted MRI at initial presentation showed high-intensity signal over bilateral basal ganglia and thalamus, and extensive bilateral subcortical white matter abnormalities (a and b). MRV demonstrated thrombosis in the straight sinus and right transverse sinus (c and d). Our patient was carrying two heterozygous nucleotide variations of CBS gene: c.154T>C (p. C52R) (e) and c.457G>A (p.G153R) (f). c.154 T>C was inherited from his father and c.457G>A was inherited from his mother (g). Magnetic resonance black blood thrombus imaging demonstrated hyper-intense signal intensity in the straight sinus (h) (arrowheads), the right transverse and sigmoid sinuses (arrowheads) (i). MRI: Magnetic resonance imaging; MRV: Magnetic resonance venography; CBS: Cystathionine beta-synthase.
The patient had no significant personal or family medical history except for having a cold few days prior to the onset. His parents were not consanguineous. His academic performance had been below average since primary school. On neurological examination, he only showed mild subnormal intelligence (WAIS-RC: VIQ: 68, PIQ: 79, FIQ: 70) and emotional euphoria without any other abnormalities. Fundus examination was normal. The patient had high myopia, subluxated lenses and decreased pigmentation of hair, which was consistent with the clinical characteristics of HHcy. He was tall and slender (body weight: 58 kg; height: 183 cm; BMI: 17.3 kg/cm2) with arachnodactyly which is considered as a marfanoid habitus. In addition, he had pes cavus. Biochemical examination showed high plasma total Hcy level (495 μmol/L [normal <15 μmol/L]). Plasma organic acid screening confirmed abnormal level of plasma Met (194.32 μmol/L; reference range: 10–50 μmol/L). Genetic analysis (including CBS, MTHFR, MTRR and MTR) by Sanger sequencing (Joy Orient Translational Medicine Research Center Co. Ltd., China) revealed two novel heterozygous nucleotide variations of CBS: c.154T>C (p. C52R) [Figure 1e] and c.457G>A (p.G153R) [Figure 1f]. None of these have been previously described as a pathogenic CBS mutation. Further testing identified c.154 T>C originated from his father and c.457G>A was inherited from his mother [Figure 1g]. MTHFR polymorphism screening revealed homozygous c.677C>T. These confirmed the diagnosis of HHcy. Magnetic resonance black blood thrombus imaging suggested chronic thrombus in the straight sinus [Figure 1h], the right transverse, and sigmoid sinuses [Figure 1i].
The patient was treated with long-term oral warfarin and sodium valproate along with supplementation of Vitamin B6, folic acid, and Vitamin B12. His symptoms improved gradually, and no further seizures occurred. Plasma Hcy was still at a high level (100.5 μmol/L) at discharge (January 16, 2015). Considering that, he is a partial responder to pyridoxine, administration of betain, and dietary restriction of Met were prescribed. No further thrombotic events occurred during the first 6 months of follow-up.
Increased plasma Hcy has been identified as an independent risk factor for CVST (odds ratio 4.6, 95% confidence interval 1.2–12.8).[4] Various experimental data suggest that Hcy can induce thrombosis by promoting expressions of adhesion molecules, blood coagulation factor V, tissue factor, and cytokines, by inhibiting fibrinolysis and by increasing platelet reactivity. Elevation of plasma Hcy is also associated with white matter hyperintensities (WMH) on MRI examination, as were observed in the present case. Unlike periventricular hyperintensities which are often associated with myelin pallor, WMH resulting from HHcy are generally located in the subcortex. A previous study suggests that these WMH are a consequence of microvascular disease or result from direct neurotoxic effect of Hcy mediated via excitotoxic and apoptotic mechanisms.[5]
The reported frequency of HHcy attributable to CBS deficiency, based on newborn screening, is about 1:65,000–1:900,000 worldwide. Till date, at least 181 mutations in the CBS gene have been identified worldwide (Human Genome Mutation Database: http://www.hgmd.cf.ac.uk/ac/index.php). Our patient was confirmed to carry three variants (c.154 T>C (p.C52R); c.457G>A (p.G153R); and IVS13,-111 G>C) of CBS gene on Sanger sequencing. Both of these had no minor allele frequency (MAF) in the dbSNP database. Computational analysis (Provean, SIFT, Polyphen2_HDIV, Polyphen2_HVAR, and mutationtaster software) suggested that the variants c.154 and c.457 were likely to have deleterious effects. These have been proven to be compound-heterozygous (one in cis and one in trans alignment). The findings were consistent with an autosomal recessive inheritance pattern of the corresponding disorder. Further genetic testing revealed that c.154 T>C and c.457G>A originated from his father and mother, respectively. Both parents were CBS mutation gene carriers. To the best of our knowledge, this case of CBS deficiency for Hcy metabolism heralded by CVST represents a very rare reported case with c.154 T>C (p.C52R) and c.457G>A (p.G153R) mutations.
MTHFR is another critical enzyme that participates in Hcy metabolism. The most common polymorphisms are known as MTHFR C677T and MTR A2756G. These polymorphisms occur in about 10% of the world's population.[6] of MTHFR gene. Patients who are homozygous for MTHFR c.677C>T have elevated plasma Hcy levels, but are not at an increased risk of ischemic cardiovascular disease or venous thromboembolism. However, as a risk factor for CBS deficiency, it can aggravate plasma Hcy levels, and, thereby, indirectly increase the risk of vascular events.[7]
The early manifestations of our patient including severe myopia, hypopigmentation of hair, marfanoid habitus, and intellectual disability provided a clue to Hcy metabolic abnormalities. Because vascular events are the main life-threatening complications in these patients, clinicians should be aware of these nonspecific symptoms. Early metabolic screening and timely treatment may help reduce the risk of thrombotic events to some extent. Patients with more severe, pyridoxine partial or nonresponsive forms of this disease are generally treated with a Met restricted diet in combination with folic acid, Vitamin B6 and Vitamin B12 supplementation. Furthermore, treatment with betaine, a methyl donor, is recommended.[8]
In conclusion, it is important to consider the diagnosis of CVST in young patients with recent onset of severe headache and to proactively look for possible causes. As one of the most important risk factors for CVST, HHcy should always be considered, especially in patients with unexplained pathogenesis. Patients with inherited HHcy require lifelong medication. In addition, we identified two novel mutations [c.154 T>C (p.C52R) and c.457G>A (p.G153R)] of CBS gene, which led to severe homocysteinemia. Our findings extend the gene spectrum of Hcy metabolism.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This work was supported by grants from Cheung Kong (Chang Jiang) Scholars Program (No. T2014251), National Key R&D Program of China (No. 2017YFC1308401), Fundamental Clinical Research Cooperation Project of Capital Medical University (No: 17JL-02, 201611-201911), and National Science Foundation for Distinguished Young Scholars (No. 81325007).
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank the patient and his family for granting permission to publish this information.
Footnotes
Edited by: Yi Cui
REFERENCES
- 1.Cattaneo M. Hyperhomocysteinemia and venous thromboembolism. Semin Thromb Hemost. 2006;32:716–23. doi: 10.1055/s-2006-951456. doi: 10.1055/s-2006-951456. [DOI] [PubMed] [Google Scholar]
- 2.Welch GN, Loscalzo J. Homocysteine and atherothrombosis. N Engl J Med. 1998;338:1042–50. doi: 10.1056/NEJM199804093381507. doi: 10.1056/NEJM199804093381507. [DOI] [PubMed] [Google Scholar]
- 3.Magner M, Krupková L, Honzík T, Zeman J, Hyánek J, Kožich V. Vascular presentation of cystathionine beta-synthase deficiency in adulthood. J Inherit Metab Dis. 2011;34:33–7. doi: 10.1007/s10545-010-9146-y. doi: 10.1007/s10545-010-9146-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cantu C, Alonso E, Jara A, Martínez L, Ríos C, Fernández Mde L, et al. Hyperhomocysteinemia, low folate and vitamin B12 concentrations, and methylene tetrahydrofolate reductase mutation in cerebral venous thrombosis. Stroke. 2004;35:1790–4. doi: 10.1161/01.STR.0000132570.24618.78. doi: 10.1161/01.STR.0000132570.24618.78. [DOI] [PubMed] [Google Scholar]
- 5.Sachdev P, Parslow R, Salonikas C, Lux O, Wen W, Kumar R, et al. Homocysteine and the brain in midadult life: Evidence for an increased risk of leukoaraiosis in men. Arch Neurol. 2004;61:1369–76. doi: 10.1001/archneur.61.9.1369. doi: 10.1001/archneur.61.9.1369. [DOI] [PubMed] [Google Scholar]
- 6.Liew SC, Gupta ED. Methylenetetrahydrofolate reductase (MTHFR) C677T polymorphism: Epidemiology, metabolism and the associated diseases. Eur J Med Genet. 2015;58:1–10. doi: 10.1016/j.ejmg.2014.10.004. doi: 10.1016/j.ejmg.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 7.Lai WK, Kan MY. Homocysteine-induced endothelial dysfunction. Ann Nutr Metab. 2015;67:1–2. doi: 10.1159/000437098. doi: 10.1159/000437098. [DOI] [PubMed] [Google Scholar]
- 8.Huemer M, Kožich V, Rinaldo P, Baumgartner MR, Merinero B, Pasquini E, et al. Newborn screening for homocystinurias and methylation disorders: Systematic review and proposed guidelines. J Inherit Metab Dis. 2015;38:1007–19. doi: 10.1007/s10545-015-9830-z. doi: 10.1007/s10545-015-9830-z. [DOI] [PMC free article] [PubMed] [Google Scholar]