Abstract
Background:
The immunization coverage in India is far away from satisfactory with full immunization coverage being only 62% at national level. Targeting the intensive efforts to poor performing areas and addressing the determinants of nonimmunization and dropouts offers a quick solution. In this paper, we assess the inter-district variations in Haryana state, and the association of social determinants with partial and no immunization.
Methodology:
This analysis is based on data collected as part of a large household survey undertaken in the state of Haryana to measure the extent of Universal Health Coverage. A multistage stratified random sampling design was used to select primary sampling units (i.e., subcenters), villages, and households. A total of 11,594 mothers with a child between 12 and 23 months were interviewed on receipt of immunization services. Determinants of nonimmunization and partial immunization were assessed using multiple logistic regression.
Results:
About 21% of children aged 12–23 months were partially immunized, while 4.3% children aged 12–23 months had received “no immunization.” While the coverage of full immunization was 74.7% at the state level, it varied from 95% in best performing district to 38% in poorest performing district. Odds of a partially immunized child were significantly higher in urban area (odds ratio [OR] = 1.23; 95% confidence interval [CI] = 1.1–1.38), among Muslim household (OR = 3.52; 95% CI = 3.03–4.11), children of illiterate parents (OR = 1.58; 95% CI = 1.22–2.05), and poorest quintile (OR = 1.61; 95% CI = 1.36–1.89).
Conclusions:
Wide interdistrict variations call for a need to consider changes in resource allocation and strengthening of the government initiatives to improve routine immunization in these districts.
Keywords: Immunization, India, social determinants, vaccination
INTRODUCTION
Vaccination is one of the most cost-effective child survival intervention.[1] This also has the current policy impetus in the country, as the Government has aggressively launched Mission Indradhanush to target vaccination dropouts. Successful implementation of this requires district level information, as in a decentralized health system, districts prepare program implementation plan on which budgets are released. Data on vaccine coverage at this level, however, remains scarce. Most of the national surveys such as the National Family Health Survey (NFHS) or Coverage Evaluation Survey (CES) provide estimates at the state level.[2,3] District Level Household Survey (DLHS) although provides district-level coverage has a long recall period which may lead to bias.[4] Public health system's records and reports have been repeatedly reported to be inaccurate and incomplete by various researchers.[5] Therefore, there is an urgent need to generate concurrent data for immunization coverage at the district level, which may better contribute to policy planning. To bridge this gap, we undertook the current study in Haryana state, with an aim to assess district level immunization coverage and identify interdistrict inequalities, along with determinants of partial and nonimmunization.
METHODOLOGY
Study setting and sampling
This present analysis is based on data collected as part of a large household survey undertaken in the state of Haryana to measure the extent of Universal Health Coverage.[6] Haryana state in north India has 95 Community Health Centres, 440 Primary Health Centres (PHCs), and 2630 Subcentres (SCs) for the provision of primary healthcare services.[7] As part of this survey, 30 graduate-level field investigators collected household-level information from a randomly selected sample of SCs in all 21 districts of the state. A multistage stratified random sampling design was used in the selection of primary sampling units (PSUs), i.e., SCs in rural areas and polio post in the urban area, villages, and households.
Using the list of SCs and urban polio posts obtained from the National Health Mission (NHM), PSUs were selected randomly. The data regarding population and villages under each SC was obtained from SC and Anganwadi center records. These data were then used by the investigators for subdivision of SC level targets into village level. The 1st household in each village was selected randomly followed by consecutive sampling till deserved sample size was completed. The detailed methodology regarding procedure of data collection is mentioned elsewhere.[6,8]
Sample size determination
With an average population of 906 of children aged 12–23 months at PHC level in Haryana state, assuming full immunization coverage as 71.7% and absolute error to be 11%, 95% confidence interval (CI), and an effect size of 1.5, a sample size of 70 was considered appropriate at PHC level. Since there were 4 SCs in each PHC, a sample size of 19 children aged 12–23 months per SC was estimated.
Data collection procedure and quality management
The data were collected from October 2012 to April 2014. A total of 79,742 households were enrolled in the study. A pretested, semistructured questionnaire, translated into Hindi language was used to collect the data. Data regarding immunization card and receipt of different vaccines were collected besides general demographic information of households and other social determinants. The data were collected through face-to-face interview with the mothers/caregivers.
Immunization cards were first checked manually to validate information and confirm the correct date of vaccination. Where immunization card was not available for verification, responses based on mother's recall were recorded. Completeness and consistency of the collected data were checked each day by the senior investigators followed by senior staff at the regional office. At regional office, if any error was found by research officer after validating the data, the copy of the data was then forwarded to investigators, so that these errors were corrected at investigator end by visiting households again.
The study was approved by the Institute Ethics Committee of the Post Graduate Institute of Medical Education and Research, Chandigarh. A written informed consent was taken from the mothers (or caregiver) of all the study children. Administrative approval of the NHM, Government of Haryana was obtained.
Data analysis
Measure of the study
On the basis of the information on vaccination, we categorized the child as fully immunized, partially immunized, or not immunized at all based on the following standard definitions:[4]
Full immunization
Defined as a child, who has received one dose of Bacillus Calmette–Guérin (BCG), 3 doses of Diphtheria, Pertussis, Tetanus (DPT)/Pentavalent vaccine and oral polio vaccine and one dose of measles vaccine within the age of 1 year. Either DPT or pentavalent was considered since there was a switch between from DPT to pentavalent vaccine in the state immunization policy during data collection. Hence, while the earlier cohort of children was eligible for DPT, the subsequent cohort was provided with the pentavalent vaccine.
Partial immunization
A child who has received at least one vaccine but has not completed the entire set of vaccines. This is similar to drop out.
Nonimmunization
A child who has not received any vaccine as per Universal Immunization Programme schedule.
District wise and state level weighted coverage of immunization was calculated. Appropriate sampling weight is applied at district level as well as state level as discussed in supplement material.[6] A bivariate analysis was conducted to examine the association of vaccination status with each of the potential predictor variables. Further, we employed multiple logistic regression to see the association of no-immunization and partial immunization with their social determinants. The dependent variables were status of immunization, i.e., partial immunization and no immunization;while independent variables were gender of child (boy and girl), area of residence (rural and urban), religion, caste (SC and ST, other backward class/general), education of head of household occupation of head of household, and wealth quintile of the household. Wealth status was assessed using household assets by applying principal component analysis.[9] The adjusted odds ratio (OR) is reported as a measure of association along with the 95% confidence limits and P. Data analysis was done using SPSS version 21.0 (Armonk, NY: IBM Corp) statistical software.
RESULTS
Sample characteristics
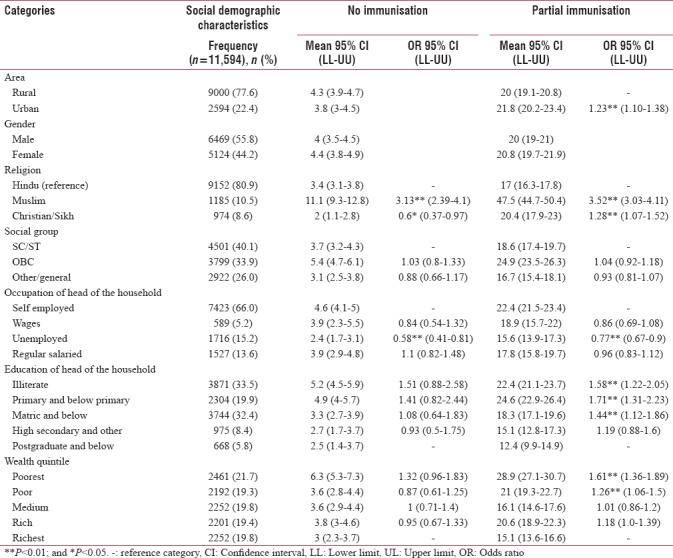
The overall sample included 11,594 children aged 12–23 months belonging to 446 rural and 124 urban PSUs across all 21 districts of Haryana state. Out of all these children, 56% were male, 77.6% were from rural areas, 80.9% were Hindus, and 40.1% belonged to SC category [Table 1].
Table 1.
Sociodemographic characteristics of study population, partial, and no immunization rates and its association with social determinants
Interdistrict variations in immunization coverage
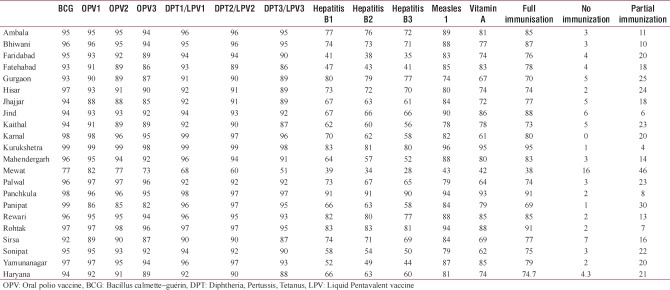
Full immunization coverage in Haryana was found to be 74.7%. While 20% were partially immunized and 4% children had received no immunization. Among the children with immunization card, coverage rate is even higher (81.8%). Kurukshetra district had highest full immunization coverage (95%) followed by Panchkula (91%) whereas Mewat, one of the backward districts of Haryana, had the lowest immunization coverage (38%). All other districts in Haryana had coverage in excess of 60%. Partial immunization coverage and no immunization were again highest in Mewat (46% and 16%, respectively) and lowest in Kurukshetra (4% and 1%, respectively) [Table 2].
Table 2.
District wise full immunization coverage rates in Haryana state, India (2012-2014)
Social determinants
Odds of partial immunization is significantly more in urban as compared to rural area (OR = 1.23; 95% CI = 1.1–1.38), among Muslims (OR = 3.52; 95% CI = 3.03–4.11), among children whose parents were self-employed (cultivator, own account worker, self-employed, and employer) (OR = 0.77; 95% CI = 0.67–0.9), and those with illiterate head of the family (OR = 1.58; 95% CI = 1.22–2.05). The odds of partial immunization are also strongly associated with wealth status with higher odds in the poorest (OR = 1.61; 95% CI = 1.36–1.89). Similarly, odds of no immunization is significantly more in Muslims (OR = 3.13; 95% CI = 2.39–4.1), parents who are self-employed (OR = 0.58; 95% CI = 0.41–0.81), and among the poorest wealth quintile (OR = 1.32; 95% CI = 0.96–1.83) [Table 1].
DISCUSSION
Overall, we found that almost one-fourth of the children in Haryana aged 12–23 months were “partially immunized” or had “no immunization.” The interdistrict variations were quite wide with Kurukshetra district having lowest percentage and Mewat district having the highest percentage of “partially immunized” or “no immunized” children. The partial immunization was significantly more among urban, Muslim, illiterate and in the poorest quintile and no immunization was significantly more among Muslims.
The findings of our study show an encouraging trend of reduced dropouts with 21% partially immunized children as compared to 25% and 42% in CES 2009 and DLHS 4 (2012–2013), respectively.[3,10] Dropouts have also declined as compared to what others have reported in studies from specific districts.[11] Furthermore, among those children with immunization card, the rates of partial (17.5%) and no immunization (0.7%) coverage were further low. We found a higher full immunization coverage in Haryana than NFHS 4 (62%).[2] Our study (n = 79,742 households) has a much larger sample size than NFHS. Second, we draw the sample from a representative set of state population covering all districts and have recorded information from immunization cards in the majority of cases. Finally, while NFHS uses a much longer recall period, we have used a shorter recall period. Hence, we believe that our estimates are more accurate.
Determinants of immunization coverage
Despite an increase in routine vaccination coverage of the state during the past decade, the percentage of children completing the recommended vaccination schedule remains below expected targets. The challenge of decreasing dropouts and enrolling the ones with no immunization at all becomes ever more daunting as the country adds a pool of 12.5 million partially immunized children each year.[12] Therefore, it is important to assess the determinants of partial and no immunization so that attention can be paid to overcome the factors or barriers impeding the compliance for full immunization. Moreover, it is well documented that the epidemiology of nonimmunization may differ substantially from the epidemiology of partial immunization.[13]
A number of studies have focused on individual predictive factors for vaccination including gender, age, and birth order, and others on household factors such as family size, number of children below the age 3 of years, household wealth, caste, and maternal education, but most of these studies categorize vaccination status into complete (i.e., full) versus incomplete (i.e., under- or non-vaccinated).[13] Only few studies[11,14] had used three distinct vaccination categories (i.e., full-, partial, and non-vaccination) to investigate determinants of childhood vaccination in India but was limited by small sample sizes drawn from narrowly defined geographic areas potentially impacting the generalizability to the national population.
Vaccination coverage in children from urban areas has been reported to be better than the ones in rural areas.[15,16] However, our study findings indicated significantly more number of partial immunized children in urban as compared to rural. The higher proportion of the partially immunized might be attributed to the migratory population of urban slums. Migration is an important determinant of child immunization and various studies have supported the fact of increase dropouts in the urban migrant population.[17,18,19] Moreover, there is an extensive network of health-care centers and health workforce (Accredited Social Health Activists) in rural areas of India to mobilize children and pregnant women to provide health-care services; however, a comparable network does not exist in urban areas.[13] Thus, these findings could partially account for lower chances of urban children to be fully vaccinated and thus lay, significant implications for targeted immunization intervention programs such as Mission Indradhanush and related policies.
Researchers have noted that lack of attention to social determinants of health, including gender, education, employment, and the failure of the health-care system to deliver to those in need lead to existing health inequities in India.[8] The odds of partial or no immunization is significantly lower as we move to the higher level of wealth quintile, in children with more educated parents and lower in male child, thus in concordant with the findings in the previous literature.[11,15,20,21,22] Profound visible inequity in the utilization of services among religious groups has been reported in India.[13] More unimmunized children and partially immunized children are found among Muslim families. The finding was concordant with other previous surveys in India.[23,24] Religious disparities affecting immunization coverage is seen in low-income, middle-income countries, as well as in high-income countries.[25] This finding also explains higher rate of under-vaccination (46%) in Mewat district of Haryana as the almost three-fourth population in Mewat belongs to Muslim religion.[26]
Implications for mission Indradhanush Programme
Mission Indradhanush Programme launched by Central Government targeted the five high priority districts in Haryana (Faridabad, Gurgaon, Mewat, Palwal, and Panipat) but, the state had launched this targeted program in all 21 districts. This has led to wastage of resources in those districts where the partially immunized and no immunized children were very low. In addition, this also led to gap in paying attention on the focused interventions for addressing the social determinants in high priority districts of Haryana. Resources should be allocated equitably so that the high priority districts get benefits. Thus, the program should specifically target children in lower wealth quintiles pockets, slum populations, Muslim dominated areas, as these are more vulnerable to partial immunization.
CONCLUSIONS
Our findings suggest that there is considerable interdistrict variations in routine vaccination coverage in Haryana state. Immunization program should prioritize efforts to address the determinants of dropout and no immunization at the community level. More formative research could be done at the subdistrict level and thoughts should be put on to tackle the barriers to achieve high coverage before implementing the policies and targeted programs. Equitable resource allocation should be ensured in the state to tackle the supply side gaps in providing immunization services.
Financial support and sponsorship
This study was funded by the National Rural Health Mission, Department of Health and Family Welfare, Government of Haryana.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank the National Rural Health Mission, Department of Health and Family Welfare, Government of Haryana for their support.
REFERENCES
- 1.Maurice JM, Davey S. State of the World's Vaccines and Immunization. Geneva: World Health Organization; 2009. [Google Scholar]
- 2.State Fact Sheet-Haryana. Mumbai: International Institute for Population Sciences, Ministry of Health and Family Welfare, Government of India; 2015-16. National Family Health Survey-4. [Google Scholar]
- 3.UNICEF. Coverage Evaluation Survey 2009, All India Report. New Delhi: Ministry of Health and Family Welfare, Government of India; 2011. [Google Scholar]
- 4.IIPS. District Level Household and Facility Survey (DLHS-4), 2012-13: India. Haryana. Mumbai: International Institute for Population Sciences; 2014. [Google Scholar]
- 5.Sharma A, Rana SK, Prinja S, Kumar R. Quality of health management information system for maternal & child health care in Haryana state, India. PLoS One. 2016;11:e0148449. doi: 10.1371/journal.pone.0148449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prinja S, Gupta R, Bahuguna P, Sharma A, Kumar Aggarwal A, Phogat A, et al. A composite indicator to measure universal health care coverage in India: Way forward for post-2015 health system performance monitoring framework. Health Policy Plan. 2017;32:43–56. doi: 10.1093/heapol/czw097. [DOI] [PubMed] [Google Scholar]
- 7.Prinja S, Kanavos P, Kumar R. Health care inequities in North India: Role of public sector in universalizing health care. Indian J Med Res. 2012;136:421–31. [PMC free article] [PubMed] [Google Scholar]
- 8.Prinja S, Bahuguna P, Gupta R, Sharma A, Rana SK, Kumar R. Coverage and financial risk protection for institutional delivery: How universal is provision of maternal health care in India? PLoS One. 2015;10:e0137315. doi: 10.1371/journal.pone.0137315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vyas S, Kumaranayake L. Constructing socio-economic status indices: How to use principal components analysis. Health Policy Plan. 2006;21:459–68. doi: 10.1093/heapol/czl029. [DOI] [PubMed] [Google Scholar]
- 10.IIPS. District Level Household and Facility Survey (DLHS-4), 2012-13: State Fact Sheet. Haryana. Mumbai: International Institute for Population Sciences; 2014. [Google Scholar]
- 11.Nischal T, Bhattacharya M. Utilization of immunization services in two districts of Haryana: Beneficiaries' perspectives. Health Popul Perspect Issues. 2016;36:45–56. [Google Scholar]
- 12.Laxminarayan R, Ganguly NK. India's vaccine deficit: Why more than half of Indian children are not fully immunized, and what can – And should – Be done. Health Aff (Millwood) 2011;30:1096–103. doi: 10.1377/hlthaff.2011.0405. [DOI] [PubMed] [Google Scholar]
- 13.Shrivastwa N, Gillespie BW, Kolenic GE, Lepkowski JM, Boulton ML. Predictors of vaccination in India for children aged 12-36 months. Am J Prev Med. 2015;49:S435–44. doi: 10.1016/j.amepre.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 14.Agrawal SC, Kumari A. Immunization status of children and the influence of social factors: A hospital based study in western Uttar Pradesh. Pediatr Infect Dis. 2014;6:25–30. [Google Scholar]
- 15.Lauridsen J, Pradhan J. Socio-economic inequality of immunization coverage in India. Health Econ Rev. 2011;1:11. doi: 10.1186/2191-1991-1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mathew JL. Inequity in childhood immunization in India: A systematic review. Indian Pediatr. 2012;49:203–23. doi: 10.1007/s13312-012-0063-z. [DOI] [PubMed] [Google Scholar]
- 17.Nath B, Singh JV, Awasthi S, Bhushan V, Kumar V, Singh SK. A study on determinants of immunization coverage among 12-23 months old children in urban slums of lucknow district, India. Indian J Med Sci. 2007;61:598–606. [PubMed] [Google Scholar]
- 18.Kusuma YS, Kumari R, Pandav CS, Gupta SK. Migration and immunization: Determinants of childhood immunization uptake among socioeconomically disadvantaged migrants in Delhi, India. Trop Med Int Health. 2010;15:1326–32. doi: 10.1111/j.1365-3156.2010.02628.x. [DOI] [PubMed] [Google Scholar]
- 19.Antai D. Migration and child immunization in Nigeria: Individual- and community-level contexts. BMC Public Health. 2010;10:116. doi: 10.1186/1471-2458-10-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dalal A, Silveira MP. Immunization status of children in Goa. Indian Pediatr. 2005;42:401–2. [PubMed] [Google Scholar]
- 21.Som S, Pal M, Chakrabarty S, Bharati P. Socioeconomic impact on child immunisation in the districts of West Bengal, India. Singapore Med J. 2010;51:406–12. [PubMed] [Google Scholar]
- 22.Prusty RK, Kumar A. Socioeconomic dynamics of gender disparity in childhood immunization in India, 1992-2006. PLoS One. 2014;9:e104598. doi: 10.1371/journal.pone.0104598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chaudhary V, Kumar R, Agarwal V, Joshi H, Sharma M. Evaluation of primary immunization coverage in an urban area of Bareilly city using cluster sampling technique. NJIRM. 2010;1:10–5. [Google Scholar]
- 24.Kulkarni SV, Chavan MK. A study to assess the immunization coverage in an urban slum of Mumbai by lot quality. Int J Med Public Health. 2013;3:21–5. [Google Scholar]
- 25.Glatman-Freedman A, Nichols K. The effect of social determinants on immunization programs. Hum Vaccin Immunother. 2012;8:293–30. doi: 10.4161/hv.19003. [DOI] [PubMed] [Google Scholar]
- 26.Mewat Religion Census. 2011. [Last cited on 2017 Aug 21]. Available from: http://www.census2011.co.in/data/religion/district/226-mewat-.html .