Abstract
Background:
Tuberculosis (TB) is first opportunistic infection and leading cause of death among human immunodeficiency virus (HIV)/AIDS. Certainly, the prevalence of TB is expected to differ between general population and HIV-infected persons. This study was conducted to determine the prevalence of TB among newly diagnosed HIV-infected adults attending antiretroviral therapy (ART) center in the state of Gujarat, India.
Materials and Methods:
Cross-sectional study was carried out among newly diagnosed HIV-infected persons attending ART center from July 2012 to September 2012. Screening of TB symptoms and chest X-ray was done for those who consented. Sputum samples were collected for microscopy with Ziehl–Neelsen method for all presumptive TB cases and those diagnosed as pulmonary TB, culture, and drug susceptibility test was done. Blood samples were collected for CD4+ T-cells count and hemoglobin.
Results:
Out of 2021 eligible HIV-infected persons, 63.5% were males and 68.2% were in the age group of 26–45 years. The prevalence of TB was 17.8%. Among 360 patients with TB, 102 (28%) had smear positive TB, 86 (24%) had smear-negative TB, and 172 (48%) were diagnosed as extrapulmonary TB. Two hundred and thirty-eight (27%) TB patients with CD4+ T-Cell count below 200 compared to 122 (11%) patients above 200.
Conclusion:
A high prevalence of TB was found among newly diagnosed HIV-infected adults attending ART center for care and treatment. The prevalence of pulmonary and extrapulmonary TB was almost equal. Chances of TB disease were more with depletion of CD4 counts. The study highlights urgent need of intensive case finding as well as periodic screening of newly diagnosed HIV-infected individuals.
Keywords: Antiretroviral therapy, Gujarat, human immunodeficiency virus, prevalence, tuberculosis
INTRODUCTION
Mycobacterium tuberculosis (TB) and Human immunodeficiency virus (HIV) infection are continues to be a major public health challenge in India.[1,2] TB is the most common opportunistic infection and leading cause of death among people living with HIV (PLHIV)/AIDS.[3] With an estimated 2–2.3 million in 2014, India alone accounted for an estimated one quarter (27%) of all TB cases worldwide.[4] Estimated population living with HIV/AIDS is 2.1–2.4 million in India with an estimated adult HIV prevalence of 0.27% (range: 0.2%–0.4%).[5,6,7] TB alone accounted for about 13% of all HIV-related death across the world and approximately 25%–65% of PLHIV/AIDS have any forms of TB.[8,9,10,11,12]
HIV-infected persons have approximately 8 times higher risk of developing TB than persons without HIV. Early diagnosis and prompt initiation of TB treatment help to reduce the burden of TB in HIV people. However, presentation of TB may varies in the HIV-infected patients with a degree of immune suppression also a diagnosis of TB in HIV persons can be difficult and confused with other systemic infections.[7] Unusual clinical presentation, smear-negative in nature and atypical radiological findings can result in miss or delay in diagnosis and can lead to higher morbidity and mortality.[7,13,14]
National framework for joint TB-HIV collaborative activities recommends intensified TB case findings at Integrated HIV counseling and testing centers (ICTCs), antiretroviral therapy (ART) Centers and Community support centers.[1,7] The prevalence of TB among HIV-infected individual attending ART center is high.[1] However, very little information is available about TB prevalence among newly diagnosed HIV-infected persons globally, and it is unknown in Gujarat state. Hence, it would be very important to assess the prevalence of TB among newly diagnosed HIV-infected persons attending ART centers and its relation with CD4 Cell counts.
MATERIALS AND METHODS
Study design
A cross-sectional study was conducted in the State of Gujarat which is situated in the western part of India with approximately 60 million population. The State has HIV seroprevalence of <1% among antenatal women and more than 5% among high-risk group.[6] Under the National AIDS Control Programme (NACP), across India, all PLHIV are registered for care, support, and treatment at ART centers. The State has 24 such NACP approved ART centers, and all of them were included in the study.
The study was designed to measure the prevalence of symptoms suggestive of pulmonary TB, smear-positive pulmonary TB and extrapulmonary TB in newly diagnosed HIV-infected persons of 18 years and above.
All newly diagnosed HIV-infected persons attending for care and treatment during 3 months from July 2012 to September 2012 in the state of Gujarat were included in the study. Those persons found as an HIV reactive at ICTCs and registered at ART centers on the first visit considered as a newly diagnosed HIV person. No sampling strategy was employed, and 100% enrollment was done. Eligible participants were those aged more than 18 years and agreed to give consent to participate in the study. Pregnant females were excluded from the study.
All eligible enrolled in the study underwent TB symptomatic screening and chest radiography as part of baseline investigations at ART centers. Two (one early morning and one supervised spot) sputum samples of all individuals were collected from presumptive TB patients. Sputum samples were examined by sputum smear microscopy using Ziehl–Neelsen technique at Designated Microscopy Center (DMC) of ART Center. The DMC laboratory technician had preserved all smear slides for cross-examination by Senior TB Laboratory Supervisor for confirmation of the result. Blood sample of each eligible participant was collected in ethylene diamine tetraacetic acid tubes and was used for measurement of CD4+ T-cells and hemoglobin. Diagnosis and treatment of TB and HIV/AIDS were given free of cost as per national policy of RNTCP and NACP in India.[1]
Ethical considerations
Administrative approvals of state TB cell and Gujarat State AIDS Control Society were obtained for conducting this study. Individual informed consent from the participants were obtained before enrollment. Data were maintained securely by program staff.
The protocol was approved by Institutional Ethical Committee of the B. J. Medical College, Ahmedabad, Gujarat, India. Immunological status was assessed using CD4+ T-cells count, and patients with CD4+ T-cells <500 cells/mm3 were classified as having immunosuppression.[14]
Data collection and analysis
Information were collected in a pre-tested, semi-structured questionnaire by the RNTCP staff trained for study purpose. Completed questionnaires were collected, and double data entry was done. Both the database were compared and scrutinized for duplicate enrollment. Statistical analysis of data was done using EpiInfo™ 3.5.1. Software. The level of significance was set at P ≤ 0.05, and 95% confidence interval was used throughout. Categorical data were analyzed using Chi-square test.
RESULTS
During the study, 3231 newly diagnosed HIV-infected patients attended and registered at 24 ART centers of Gujarat. Out of them, 2021 patients were eligible for the study.
Baseline characteristics of study participants
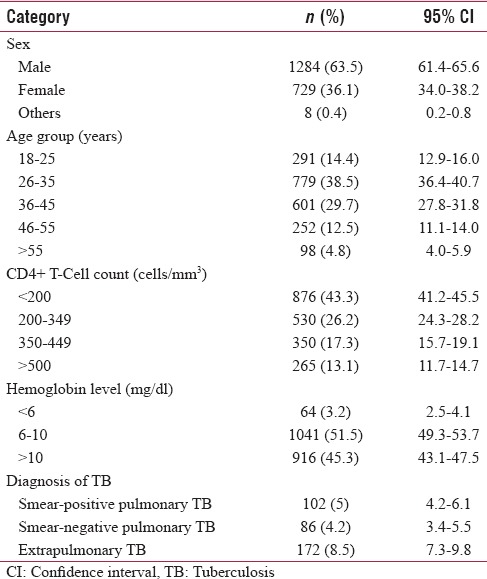
Mean age of study participants was 37 years (±10.3 standard deviation [SD]). Two-third participants were of the ages of 26–45 years. Among study participants, 63.5% were males. Out of 2012 HIV reactive patients, 876 (43.3%) had CD4+ T-cell count <200 cell/mm3 and 530 (26.2%) had CD4+ T-cell count between 200–349 cell/mm3. More than two-thirds of patients were found immunosuppression.
Among study participants, 55% had hemoglobin <10 mg/dl. Baseline characteristics of study participants are given in Table 1.
Table 1.
Baseline characteristic of study participants (n=2021)
Tuberculosis patients among newly diagnosed human immunodeficiency virus-infected patients
Out of 2021 eligible participants, 360 (17.8%) were diagnosed with any form of TB. Among these TB patients, 52% had pulmonary TB, and 48% had extrapulmonary TB. Also of patients with pulmonary TB, 54% had sputum smear-positive TB and 46% had sputum smear-negative TB. This has shown in Figure 1.
Figure 1.
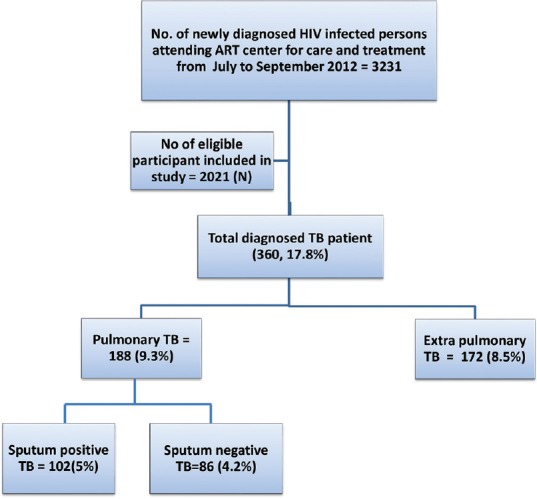
Prevalence of tuberculosis among newly diagnosed HIV-infected individuals
Tuberculosis symptomatic among newly diagnosed human immunodeficiency virus-infected patients
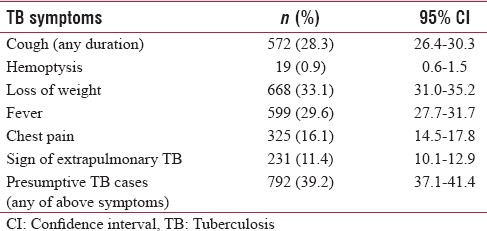
In the study, 572 (28.3%) patients had cough, 599 (29.6%) had fever, 19 (0.9%) had blood in sputum, 668 (33.1%) had loss of weight, 325 (16.1%) had chest pain and 231 (11.4%) had signs of extrapulmonary TB. The proportion of HIV-infected patients having any of above symptoms of TB was 39%. Clinical symptoms among HIV-infected patients have shown in Table 2.
Table 2.
Clinical symptom of tuberculosis among study participants (n=2021)
Relationship between tuberculosis, CD4 + T-cell and hemoglobin
Mean CD4 cell count of the study group was 278 cell/mm3 and mean CD4 cell count among HIV-infected TB patients were 185.5 cell/mm3. Two-third of HIV-infected TB patients had CD4 cell count <200 cell/mm3 (P < 0.0001). HIV-infected TB patients had lower CD4+ T-cells count than the HIV-infected patients without TB. The relationship between immune status and TB is shown in Table 3.
Table 3.
Association of tuberculosis with immunological status and hemoglobin (n=360)
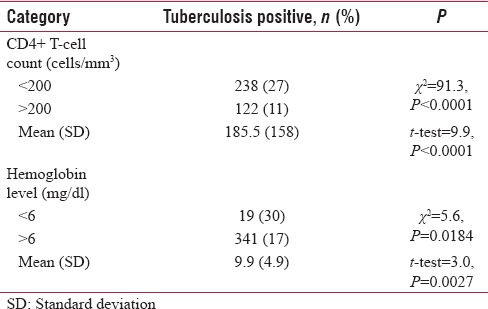
Mean Hemoglobin level was 9.9 mg/dl (SD – 4.9). 29.7% of HIV reactive patients had TB with hemoglobin level <6mg/dl (P = 0.0184). Hemoglobin level of HIV-infected TB patients is quite low compare to HIV-infected patients without TB. The relationship between hemoglobin level and HIV-TB co-infection is shown in Table 3.
DISCUSSION
This was the first attempt in the state to determine the prevalence of all form of TB among newly diagnosed HIV-infected patients. We observed a high prevalence of TB among newly diagnosed HIV people. The proportion of pulmonary and extrapulmonary TB was almost equal. Almost two-thirds of HIV-infected patients had low CD4 cell count (<350 CD4+ T cells/mm3). The CD4 cell count was lower in HIV-infected patients who had TB.
The proportion of TB was found to be 17.8% among newly diagnosed HIV-infected patients current study. Finding of study done in Telangana, India was prevalence of TB among HIV/AIDS patients was 29.6% which is very high compared to our study.[15] In our study, Pulmonary TB was diagnosed using smear microscopy and chest X-ray. A study conducted in Dar es salaam, Tanzania found 15% TB prevalence in patients attending HIV care and treatment clinics[16] which is similar to our study and another study conducted in Northern Tanzania showed the prevalence rate of TB was 8.5%[17] and study conducted in Cambodia found 12% prevalence of Pulmonary TB among HIV-infected patients was lower than present study.[18] Studies conducted in African Continent reported TB prevalence among HIV-infected patients ranged from 8.5% to 15%. The variation in the prevalence may be due to the inclusion of all forms of TB, exclusion of persons below 18 years.
Findings of our study showed that almost equal proportion of patients had pulmonary TB and extrapulmonary TB among HIV patients. It showed high proportion of extrapulmonary TB which otherwise is 20% in non-HIV patients.[7,19] A study conducted in Gujarat, India earlier reported 43% of HIV-TB co-infected patients with extrapulmonary TB which is close to present study findings.[20] Moreover, among pulmonary TB patients in HIV-infected patients, 46% were smear negative. Paucibacillary nature of TB in PLHIV may lead to high proportion of smear-negative TB patients. Similar findings were reported in study in Ethiopia which reported 60%[21] and in Gujarat where it was reported to be 37%.[20]
A symptom of cough was less common (28%) compared to symptoms of fever (30%) and loss of weight (33%). Among the study group, 792 (39%) had at least one symptom suggestive of TB. Similar findings were observed in Karnataka.[22] This uncommon clinical picture suggests that all HIV patients should be routinely screened using symptom complex (cough, fever, weight loss and night sweat) as recommended by technical and operational guideline of Government of India[1,7] as well as by chest radiography.
43% of newly diagnosed HIV-infected adults had very low CD4 cell count (<200 cell/mm3) and 1756 (87%) patients were classified as an immunosuppression (<500 cell/mm3).[18] Mean CD4 cell count of the study group was 278 which is close to Telangana study which had 260.[15] Findings suggest the late diagnosis of HIV infection in community which may be strengthen by innovative health promotion approach and focused awareness activity for general as well as hard to reach populations.
Of 360 HIV-TB patients, 88% had <350 CD4 count and mean CD4 count was 185.5 (SD; ±157.95) while in HIV-positive TB-negative patients, 66% had <350 CD4 count and mean was 298.2 (SD; ±203.46). A study conducted in Masih Daneshvari Hospital, Tehran reported similar low CD4 count. It reported 78.6% had CD4 counts <350 (mean ± SD; 229.15 ± 199.45).[23] Low CD4 count among newly infected HIV patients with TB in our study suggests that chances of TB increasing with depletion of CD4 counts.
Almost half of the study participants had <10 mg/dl hemoglobin level. Among HIV-TB patients, 68% (mean 9.9; SD ± 4.9) had <10 mg/dl hemoglobin level while in HIV-positive TB-negative patients, it was 52% (mean 10.8; SD ± 5.2). This indicated hemoglobin level was little lower in HIV-TB patients.
The strength was relatively large number of HIV-infected patients were studied. The study was conducted under programmatic conditions, so findings are likely to reflect the operational reality on the ground.
Limitations
A limitation of our study was HIV-infected patients diagnosed but not attended ART center were not included. In that case, we might have missed some TB patients.
CONCLUSION
TB prevalence was high among newly diagnosed HIV-infected adults attending ART center for care and treatment. The prevalence of pulmonary and extrapulmonary TB was almost equal. At the time of diagnosis of HIV infection, low CD4 counts were reported and even lower in TB patients. The study highlighted urgent need of intensive case finding as well as periodic screening of TB among HIV-infected individuals. Efforts should focus on early diagnosis of HIV infection with intensive health promotion strategy and early diagnosis of TB among HIV/AIDS people using higher sensitivity diagnostics.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.National Framework for Joint TB/HIV Collaborative Activities. New Delhi, India: Ministry of Health and Family Welfare, Government of India; 2013. [Google Scholar]
- 2.Friedland G, Churchyard GJ, Nardell E. Tuberculosis and HIV coinfection: Current state of knowledge and research priorities. J Infect Dis. 2007;196(Suppl 1):S1–3. doi: 10.1086/518667. [DOI] [PubMed] [Google Scholar]
- 3.Fujiwara PI, Dlodlo RA, Ferroussier O, Nakanwagi-Mukwaya A, Cesari G, Boillot F, et al. Implementing collaborative TB-HIV activities: A programmatic guide. Paris, France: International Union against Tuberculosis and Lung Disease; 2012. [Google Scholar]
- 4.World Health Organization. Global Tuberculosis Report 2015. Geneva, Switzerland: World Health Organization; 2015. [Google Scholar]
- 5.HIV/AIDS Health profile 2010. India, U.S. Embassy, New Delhi, India: USAID; 2010. [Google Scholar]
- 6.National HIV Sentinel Surveillance and HIV Estimation 2006. New Delhi, India: National AIDS Control Organization, Ministry of Health and Family Welfare, Government of India; 2008. [Google Scholar]
- 7.RNTCP Technical and Operational Guideline for Tuberculosis Control in India 2016. New Delhi, India: Central TB Division, Ministry of Health and Family Welfare, Government of India; 2016. [Google Scholar]
- 8.Sharma SK, Kadhiravan T, Banga A, Goyal T, Bhatia I, Saha PK, et al. Spectrum of clinical disease in a series of 135 hospitalised HIV-infected patients from North India. BMC Infect Dis. 2004;4:52. doi: 10.1186/1471-2334-4-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sharma SK, Mohan A, Kadhiravan T. HIV-TB co-infection: Epidemiology, diagnosis and management. Indian J Med Res. 2005;121:550–67. [PubMed] [Google Scholar]
- 10.Arora VK, Kumar SV. Pattern of opportunistic pulmonary infections in HIV sero-positive subjects: Observations from Pondicherry, India. Indian J Chest Dis Allied Sci. 1999;41:135–44. [PubMed] [Google Scholar]
- 11.Gothi D, Joshi JM. Clinical and laboratory observations of tuberculosis at a Mumbai (India) clinic. Postgrad Med J. 2004;80:97–100. doi: 10.1136/pmj.2003.008185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Corbett EL, Watt CJ, Walker N, Maher D, Williams BG, Raviglione MC, et al. The growing burden of tuberculosis: Global trends and interactions with the HIV epidemic. Arch Intern Med. 2003;163:1009–21. doi: 10.1001/archinte.163.9.1009. [DOI] [PubMed] [Google Scholar]
- 13.Lucas SB, De Cock KM, Hounnou A, Peacock C, Diomande M, Hondé M, et al. Contribution of tuberculosis to slim disease in Africa. BMJ. 1994;308:1531–3. doi: 10.1136/bmj.308.6943.1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jones BE, Young SM, Antoniskis D, Davidson PT, Kramer F, Barnes PF, et al. Relationship of the manifestations of tuberculosis to CD4 cell counts in patients with human immunodeficiency virus infection. Am Rev Respir Dis. 1993;148:1292–7. doi: 10.1164/ajrccm/148.5.1292. [DOI] [PubMed] [Google Scholar]
- 15.Reddy SG, Ali SY, Khalidi A. Study of infections among human immunodeficiency virus/acquired immunodeficiency syndrome patients in Shadan Hospital, Telangana, India. Indian J Sex Transm Dis. 2016;37:147–50. doi: 10.4103/2589-0557.192122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mtei L, Matee M, Herfort O, Bakari M, Horsburgh CR, Waddell R, et al. High rates of clinical and subclinical tuberculosis among HIV-infected ambulatory subjects in Tanzania. Clin Infect Dis. 2005;40:1500–7. doi: 10.1086/429825. [DOI] [PubMed] [Google Scholar]
- 17.Ngowi BJ, Mfinanga SG, Bruun JN, Morkve O. Pulmonary tuberculosis among people living with HIV/AIDS attending care and treatment in rural Northern Tanzania. BMC Public Health. 2008;8:341. doi: 10.1186/1471-2458-8-341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kimerling ME, Schuchter J, Chanthol E, Kunthy T, Stuer F, Glaziou P, et al. Prevalence of pulmonary tuberculosis among HIV-infected persons in a home care program in Phnom Penh, Cambodia. Int J Tuberc Lung Dis. 2002;6:988–94. [PubMed] [Google Scholar]
- 19.World Health Organisation. Interim WHO clinical staging of HIV/AIDS and HIV/AIDS case definitions for surveillance. Geneva, Switzerland: WHO; 2005. pp. 2–8. [Google Scholar]
- 20.Dave P, Kapadiya D, Modi B, Sinha L, Shah A, Vadera B, et al. Original article Impact of TB-HIV collaborative activities on case fatality among HIV-infected tuberculosis patients in Gujarat, India. J Res Med Den Sci. 2014;2:1–7. [Google Scholar]
- 21.Kassu A, Mengistu G, Ayele B, Diro E, Mekonnen F, Ketema D, et al. Coinfection and clinical manifestations of tuberculosis in human immunodeficiency virus-infected and -uninfected adults at a teaching hospital, Northwest Ethiopia. J Microbiol Immunol Infect. 2007;40:116–22. [PubMed] [Google Scholar]
- 22.Padmapriyadarsini C, Bhavani PK, Sekar L, Anandhachitra J, Selvaraj M, Poornagangadevi N, et al. Effectiveness of symptom screening and incidence of tuberculosis among adults and children living with HIV infection in India. Natl Med J India. 2016;29:321–5. [PubMed] [Google Scholar]
- 23.Bakhshayesh-Karam M, Tabarsi P, Mirsaiedi SM, Amiri MV, Zahirifard S, Mansoori SD, et al. Radiographic manifestations of tuberculosis in HIV positive patients: Correlation with CD4+T-cell count. Int J Mycobacteriol. 2016;5(Suppl 1):S244–5. doi: 10.1016/j.ijmyco.2016.11.027. [DOI] [PubMed] [Google Scholar]


