Abstract
Background:
Annually, about 44,000 maternal deaths occur in India, which is 20% of the global burden. Despite persistent efforts, India failed to meet the fifth millennium development goal by 2015. Lack of reliable data on maternal mortality demands utilization of tools for counting maternal deaths which is vital to implement preventative actions.
Objectives:
Our study aims to determine health system-related issues of maternal mortality using the WHO validated tool – Maternal Death Review and demonstrates usefulness of maternal death surveillance and review as a monitoring tool.
Methods:
Fourteen maternal deaths were evaluated through community based and facility-based audits from July 2013 to June 2014 in three districts of Gujarat. Pathways to death were traced through Global Positioning System (GPS). Factors contributing to the three delays were analyzed.
Results:
Type III delay, that is, delay in receiving adequate care was frequently observed in our review including weak referral linkages, lack of blood banking services, inadequate surgical facilities. and staff shortages. Mothers succumbed, not because they did not seek treatment or reach facilities in time but because facilities were incapable of providing appropriate medical care.
Conclusion:
Scaling up of maternal death audits and subsequent use of these findings will help to reduce maternal mortality in India. As we continue to push for institutional deliveries, we need to reevaluate if our health system is prepared to manage an increasing number of facility births and obstetric complications.
Keywords: Health systems, India, maternal death review, maternal mortality, three delays
INTRODUCTION
Globally, 287,000 maternal deaths occur each year and 99% of these occur in developing countries.[1] The lifetime risk of maternal mortality ranges from 1 in 36 in low-income countries against 1 in 4900 in high-income countries.[2] This difference highlights inequity unlike any other public health indicator. While maternal mortality is a priority under sustainable development goals (SDG), it is one of the 169 targets. This is unfortunate as only 10 countries achieved millennium development goal 5 (MDG 5) and maternal mortality remains alarmingly high in South Asia.[3,4] In spite of tremendous global efforts to heighten awareness of maternal health challenges, the issue has failed to garner the political and health system support it needs.
The WHO, UNICEF, UNFPA, and World Bank have made concerted endeavors to address maternal health problems by developing tools to make every death count. Continuous investment in maternal health with increased funding is essential to improve quality of care and enhance health systems capacity which includes reviewing every death to prevent future tragedies. Countries with high maternal mortality have poor death surveillance systems. Consequently, the magnitude of underreported maternal deaths precludes efficient investigations to elicit the causes of such deaths on a national or global level. The WHO launched “maternal death surveillance and review” (MDR) so that countries are in a position to take intensified actions.[5] MDR monitors maternal deaths and the subsequent lessons learned help health managers and administrators in making recommendations to prevent future deaths. Hence, it is essential that countries with high maternal mortality utilize this tool to discern evidence for effective solutions and to build a strong national database.
There are five approaches for reviewing maternal deaths: (1) Facility-based maternal death review, (2) community-based maternal death review (verbal autopsy), (3) confidential inquiries into maternal deaths, (4) survey of severe morbidity (near misses), and (5) clinical audit. A facility-based MDR involves auditing at health facilities while community-based audit entails interviewing family members about circumstances surrounding the death.[6,7] A combination of these two approaches would give a comprehensive picture of the contributory medical and social factors of maternal deaths. The third approach requires a committee to make confidential inquiries into maternal deaths. The fourth approach investigates events in which a mother has nearly died, and a clinical audit reviews obstetric care provided against established protocols. In addition, clinical and health systems records can identify the causes of maternal deaths, thereby, guiding health personnel to make contextual evidence-based interventions to reduce maternal mortality.[8]
India was not able to achieve MDG 5 and maternal mortality varies across different Indian states due to differences in access to care, level of literacy, socioeconomic factors, a wide chasm between urban and rural populations, nutritional status among women, and proficiency of the health personnel among several others.[9] This diversity leads to divergence in the burden of maternal mortality and requires political and technical commitment to bridge the health equity gap.[10] States like Tamil Nadu, Kerala, and West Bengal effectively made use of MDR in the last few years to address maternal health issues. Gujarat also adopted MDR in 2006; no results have been published by the government yet.[11] It is uncertain whether MDR is successfully implemented. Absence of analytical reports indicates that the information derived is not used to make amendments in the existing health system.
Primary objective of this study was to understand the determinants of maternal deaths among rural/tribal women, and health systems' issues leading to maternal deaths. Our study is unique in that it draws on the lived experiences of pregnant rural/tribal women and follows the path to death for such mothers.
METHODS
This study was a subset of the MATIND project, which was conducted to evaluate the Chiranjeevi Yojana Programme in Gujarat.[12] A community- and facility-based audit was conducted for the study. Data were collected in tribal and/or backward districts from July 2013 to November2014.
Maternal death cases were tracked and community based and facility-based audits were conducted for all 14 deaths identified during the survey. The WHO validated MDR tool was utilized and locations of the women and the facilities they visited were mapped using Global Positioning System (GPS) to trace the pathway to death. Historically, MDR has been an efficient tool to support improvements in health systems by analyzing the key causes of maternal deaths.[5] MDR data is used to delineate the health systems issues using a framework. The underlying premise is that national and international health agencies continue to push for institutional deliveries while we need to reevaluate if public health facilities are prepared to manage obstetric complications. Therefore, we adopted the “Three Delays” framework to analyze the outcomes.
Delays in accessing specialized maternal care happen at all levels, beginning with family, when relatives of the patient do not know when and where to refer the case with obstetric complications (Type I delay). Next, time is unduly lost in organizing transport to shift the patient to a referral hospital (Type II delay). Even after reaching the hospital or first referral unit, there may be delays in administering standard treatment to patient by hospital authorities (Type III delay).[13] Type III delay is one of the most complex problems affecting maternal survival and is a direct reflection of the quality of care emergency obstetric care.
Details of the data collection methodology can be referred to in “Community Based Survey Methodology for Maternal Healthcare Utilization: Gujarat, India.”[12]
RESULTS
The descriptive findings such as sociodemographic characteristics and maternal health utilization of surveyed women are summarized in Table 1.
Table 1.
Characteristics of surveyed mothers (n=14)
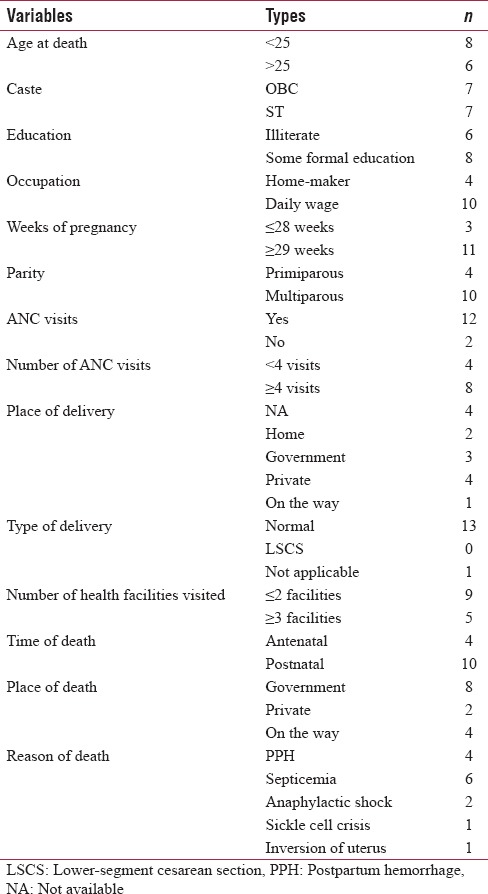
Twelve out of 14 women received antenatal care (ANC) and anemia was detected among some mothers during ANC. Eight women had at least 4 ANC visits; two women had 2–3 visits and two women visited an ANC clinic once. Nine women delivered in a health facility out of which one woman with twin pregnancy delivered one baby in transit. Twelve women died in health facilities while two women died during interfacility transfer. Ten deaths occurred during postnatal period, whereas, four occurred during antenatal period. Septicemia (4/14), postpartum hemorrhage (PPH) (3/14), and anemia (3/14) were common causes of maternal deaths. Twelve women who died sought care in more than one health facility. One mother sought care for delivery and was sent home citing the absence of labor pains. She delivered at home on the same day and developed PPH, She died on the way to the facility. One woman died at home after visiting two facilities for medical care.
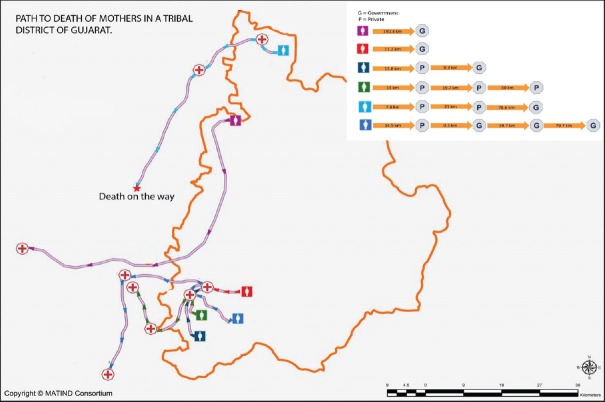
No time was wasted in deciding to seek care and arrange for transportation from home to facility for all except for two women. Barring three women, who were not attended by physicians on their first visit, all other women were immediately attended by physicians at both the first and second referral facilities. Figure 1 describes the pathway to death including number of facilities visited, distance traveled, and time spent at each facility.
Figure 1.
Path to maternal death
We found that women traveled between 8 km and 190 km for obstetric care (median = 14.25 km, mean = 34.5 km), and traveled between 300 m and 40 km to reach referred health facility (facilities) (median = 19.7 km, mean = 20.5 km). Table 2 describes factors leading to Type III delay in our study.[14]
Table 2.
Frequency of Phase III barriers observed in the study. Adopted from ‘A systematic Review of the Third Delay’ by Hannah Knight et al.
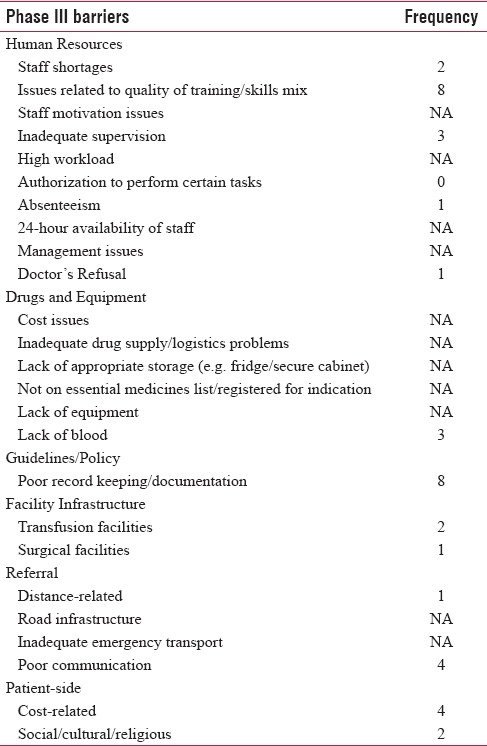
Both community based and facility-based audits indicate that providers were not always able to triage (i.e., identify emergencies and prioritize treatment/referral for them) to save the lives of these mothers. All mothers spent more than an hour for receiving care with some spending 6 or more hours in a facility before being transferred. Poor documentation was observed in eight instances. Two mothers faced delays in receiving care due to the absence of doctors while one was refused care by a doctor. Three women suffered because blood banking facilities were not available at all the facilities they were referred to. Financial constraints led to delay in receiving care for four mothers. Our observations throw light on the grave situation in rural India, thereby, calling for a scrutiny of the functioning of the health system to improve maternal health. Table 3 summarizes experiences of one mother as a case study.
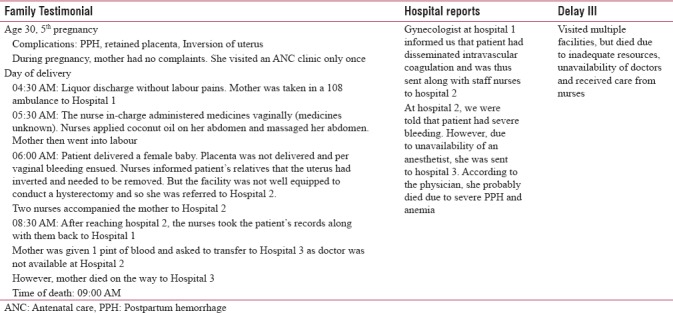
Table 3.
Summary of a case study
DISCUSSION
Maternal mortality represents an overall loss to the society as women are lost to their families, especially their surviving children.[15] India demonstrated an impressive decline of maternal mortality ratio (MMR) from 398 in 1997–1998 to 167 in 2017.[16] To achieve the SDG 3.1, we need to accelerate the pace of decline of MMR through systematic planning and implementation of contextually appropriate strategies such as MDR for the betterment of maternal health.
MDR in Malawi unveiled poor recordkeeping, fear of blame, and lack of knowledge and skills to conduct reviews.[17] Similar outcomes were observed in a Nigerian study along with shortage of staff and inadequate supervision.[18] A study in Senegal showed that after the implementation of MDR in a district hospital, maternal mortality declined over a period by improving resource management.[19] A facility-based audit conducted in Bangladesh highlighted that 47.8% deaths occurred in facilities that were preventable. Further, they also determined challenges in improving quality of care such as poor documentation and inadequate human resources.[20] The importance of such audits in exploring gaps and delays in health systems cannot be stressed enough.
In our study, maternal death cases were below 30 years of age, but most were multigravida indicating that they had marriage and childbirth at early age. Most of them earned their livelihood through daily wages. Our findings show that seven mothers were illiterate and all the cases belonged to socially backward castes (ST/OBC), suggesting that socioeconomic status and literacy are negatively correlated with maternal health issues. Remainder of the discussion section targets Type III delay factors.
Type III delay factors
Delay III is largely on account of deficiencies in the system in terms of skilled human resources, referral linkages, and noncompliance with standard treatment protocols. More often than not, too little is done in rural and tribal communities due to inadequate resources and lack of skilled and qualified professionals leading to critical loss of time in delivering services.[21] Maternal mortality represents the overall effectiveness of a country's health-care delivery system through assessments of general medical care, especially obstetric care.[5] MDR sheds light on the “gaps” in those systems.
Antenatal care
Anemia and other blood-borne diseases were common in this review; these deficiencies indicate severe maternal undernutrition. Four mothers died as a result of complications due to severe anemia. However, there is no information regarding the steps taken to correct the deficiency. It may be due to lack of nutritional counseling during ANC as the focus is mainly on the distribution of iron and folic Acid tablets. In high-risk pregnancies (50%), there were no reports of increased vigilance exercised by providers during ANC. For ANC visits to be effective, it is necessary to ensure timely communication between the patients and medical personnel so that appropriate action can be taken to prevent complications.
Human resources
Inability of health personnel to manage complications is reflected in the number of referrals recommended. More often than not, we observed that documents had either been misplaced or there were no records. In addition to poor recordkeeping, this illustrates lack of respectful care.[22] In our study, a doctor's refusal to treat a case was a classic example of denial of care sending the mother and family on a whirlwind of trips to facilities. Often, families were not informed about the cause of death (57%). Most deaths were clustered around labor and postdelivery indicating the value of time and life-saving efforts required during this phase.
Except for one woman who underwent medical termination of pregnancy, all the other women had normal deliveries. At two facilities, cesarean sections were not performed and women were referred to other facilities because of the absence of qualified health personnel at one facility, and lack of availability of blood at both facilities. These issues raise significant questions about capabilities of the attending health personnel, along with motivation issues and lack of resources.[21]
At times, unqualified or inadequately trained staff at health centers facilitated deliveries, potentially contributing to adverse pregnancy outcomes (21%). Women who died in the postnatal period did not report any visit by health workers postdelivery to assess the mother and baby's health status. We observed a lack of understanding of complications at lower levels of the health-care system, nonavailability of necessary resources and poor performing medical personnel.
Health systems and referral linkages
Most of the mothers' medical records were not found. While the Government and international organizations have teamed up to increase community demand for services, the quality of care delivered has not been evaluated. The proportion of institutional deliveries (~86%) was very high among the cases. In spite of high ANC coverage and institutional deliveries, mothers died. PPH was one of the most common causes of maternal death, partly due to inappropriate delivery practices by providers, compounded by ineffective treatment [Tables 2 and 3]. Our audits revealed some instances where women were sent home in spite of symptomatic complaints; nonremoval of the placenta, or deliveries conducted by the staff in the absence of the doctor, and ineffective treatment for convulsions at multiple facilities.
Mothers traveled to higher centers, but facilities did not provide any assistance in transportation arrangements, adding to the economic burden borne by families. Referral linkages were very weak. Most women were referred multiple times to higher centers to avail blood transfusion services or due to the absence of physicians or low capacity to manage complications. Private banks are not affordable or accessible to the rural poor population.[23] Patients were referred to higher centers without referral notes or any explanation regarding their diagnoses.
Mothers were not accompanied by any health workers. There was no communication between health personnel at the intended facility and referral units leading to further delays in procuring blood and losing invaluable time in reordering diagnostics. Sometimes, due to financial constraints, patients were unable to get the necessary care at the right time. Availability of basic services such as blood banks and provision of emergency services such as cesarean sections is imperative. It is equally essential to focus on effective referral systems, ensuring seamless coordination and transportation during and between facilities.[24]
There was a huge gap in the narration by family and hospital records. Mismatch between community and facility audits posits challenges in understanding potential channels to rectify flaws in the health system. Certainly, this crucial gap does not lend external validity to our claims.
Recommendations
Enhancing skills of providers to identify and manage obstetric complications need to be strengthened through practical training programs. To enable the accurate detection of high-risk pregnancies, ANC must be comprehensive assessments including counseling that go beyond self-reports by women. Monitoring of risk management requires more meaningful follow-up than that is currently prevalent so that there is no disconnect between the magnitude of problems and the proposed strategies and solutions. Sensitivity training needs to be incorporated so that women and newborns are treated with respect. Issues identified in referral linkages need to be ironed out beginning with the provision of interfacility transfers and transparent processes. Finally, the death review process needs to be bolstered through external reviews and the involvement of independent experts.
CONCLUSION
Scaling up the use of MDR on a national and global level, specifically in low-resource settings and developing countries, forms an important maternal health strategy to end preventable maternal mortality. MDRs are instrumental in determining challenges to improving maternal health care and unraveling pathways for reducing barriers and facilitators to care. Successful implementation of MDRs will improve the response of the health system by guiding the development of actionable plans relevant to the underlying causes of maternal deaths. It is time that maternal health problems are resolved by engineering programs that are tailored to transform the lives of our primary stakeholders: Patients and providers.
Financial support and sponsorship
The research is funded by the European Community's Seventh Framework Programme under grant agreement no. 261304.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, Daniels J, et al. Global causes of maternal death: A WHO systematic analysis. Lancet Glob Health. 2014;2:e323–33. doi: 10.1016/S2214-109X(14)70227-X. [DOI] [PubMed] [Google Scholar]
- 2.Trends in Maternal Mortality: 1990 to 2010 The World Bank WHO Library Cataloguing-in-Publication Data. [Last accessed on 2018 Feb 19]. Available from: http://www.who.int/about/licensing/
- 3.WHO | Millennium Development Goals (MDGs) WHO. 2016. [Last accessed on 2018 Feb 19]. Available from: http://www.who.int/mediacentre/factsheets/fs290/en/
- 4.GBD 2015 Maternal Mortality Collaborators. Global, regional, and national levels of maternal mortality, 1990-2015: A systematic analysis for the global burden of disease study 2015. Lancet. 2016;388:1775–812. doi: 10.1016/S0140-6736(16)31470-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO | Maternal Death Surveillance and Response. WHO. 2017. [Last accessed on 2018 Feb 20]. Available from: http://www.who.int/maternal_child_adolescent/epidemiology/maternal-death-surveillance/en/
- 6.Soleman N, Chandramohan D, Shibuya K. Verbal autopsy: Current practices and challenges. Bull World Health Organ. 2006;84:239–45. doi: 10.2471/blt.05.027003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mills S, Williams JE, Wak G, Hodgson A. Maternal mortality decline in the Kassena-Nankana district of Northern Ghana. Matern Child Health J. 2008;12:577–85. doi: 10.1007/s10995-007-0289-x. [DOI] [PubMed] [Google Scholar]
- 8.World Bank & WHO. Maternal Death Audit as a Tool Reducing Maternal Mortality. World Bank & WHO. 2011:1–5. [Google Scholar]
- 9.Maternal Death Review Department of Health and Family Welfare Government of Punjab (July 2010) Guidelines For Rolling Out. [Last accessed on 2018 Feb 20]. Available from: http://www.pbnrhm.org/docs/mdr.pdf .
- 10.Graham W, Woodd S, Byass P, Filippi V, Gon G, Virgo S, et al. Diversity and divergence: The dynamic burden of poor maternal health. Lancet. 2016;388:2164–75. doi: 10.1016/S0140-6736(16)31533-1. [DOI] [PubMed] [Google Scholar]
- 11.Maternal Death Review – A Tool for System Strengthening: Gujarat Experience. [Last accessed on 2018 Mar 01]. Available from: http://www.nhsrcindia.org/sites/default/files/MaternalDeathReview-AtoolforSystemStrengtheninginGujarat.pdf .
- 12.Vora KS, Annerstedt KS, Mavalankar DV, Dholakia NB, Sandul Y, Saiyed S, et al. Community based survey methodology for maternal healthcare utilization, Gujarat, India? IIPHG Health, 2016;8:1542–53. DOI: 10.4236/health.2016.814152. [Google Scholar]
- 13.Maine D, Akalin MZ, Ward VM, Kamara A. The Design and Evaluation of Maternal Mortality Programs. 1997. [Last accessed on 2018 Feb 19]. Available from: https://www.mailman.columbia.edu/sites/default/files/pdf/designevalmm-en.pdf .
- 14.Knight HE, Self A, Kennedy SH. Why are women dying when they reach hospital on time? A systematic review of the 'third delay'. PLoS One. 2013;8:e63846. doi: 10.1371/journal.pone.0063846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fathalla MF. On Women's Health and Rights Lectures, Speeches and Statements The Road to Maternal Death in Developing Countries. 1991. [Last accessed on 2018 Feb 27]. Available from: https://www.figo.org/sites/default/files/uploads/PublicationsandResourcesFathallafiles/c/31Theroadtomaternaldeathindevelopingcountries.pdf .
- 16.Maternal Mortality in 2005. [Last accessed on 2018 Feb 19]. Available from: http://www.who.int/whosis/mme_2005.pdf .
- 17.Kongnyuy EJ, van den Broek N. The difficulties of conducting maternal death reviews in Malawi. BMC Pregnancy Childbirth. 2008;8:42. doi: 10.1186/1471-2393-8-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Okonofua F, Imosemi D, Igboin B, Adeyemi A, Chibuko C, Idowu A, et al. Maternal death review and outcomes: An assessment in Lagos state, Nigeria. PLoS One. 2017;12:e0188392. doi: 10.1371/journal.pone.0188392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dumont A, Gaye A, de Bernis L, Chaillet N, Landry A, Delage J, et al. Facility-based maternal death reviews: Effects on maternal mortality in a district hospital in Senegal. Bull World Health Organ. 2006;84:218–24. doi: 10.2471/blt.05.023903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Biswas A, Rahman F, Eriksson C, Halim A, Dalal K. Facility death review of maternal and neonatal deaths in Bangladesh. PLoS One. 2015;10:e0141902. doi: 10.1371/journal.pone.0141902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miller S, Abalos E, Chamillard M, Ciapponi A, Colaci D, Comandé D, et al. Beyond too little, too late and too much, too soon: A pathway towards evidence-based, respectful maternity care worldwide. Lancet. 2016;388:2176–92. doi: 10.1016/S0140-6736(16)31472-6. [DOI] [PubMed] [Google Scholar]
- 22. [Last accessed on 2018 Feb 16];Quality, Humanized & Respectful Care for Mothers and Newborns: The Model Maternity Initiative. Available from: https://www.k4health.org/sites/default/files/figo_africa_mozambique.quality_respectful_care_for_mothers_newborns.pdf . [Google Scholar]
- 23.Bhatia V, Raghuwanshi B, Sahoo J. Current status of blood banks in India. Glob J Transfus Med. 2016;1:72. [Google Scholar]
- 24.Timor-Leste J. Reducing the Burden of the Three Delays on Maternal Health in Timor-Leste: Results from a Mixed-Methods Study on Individual-and Community-Level Factors Contributing to First and Second Delays in Ermera and Manatuto Municipalities and the Special Administrative Region of Oecusse Ambeno. Health Improvement Project. 2015. [Last accessed on 2018 Feb 27]. Available from: http://www.jsi.com/JSIInternet/Inc/Common/_download_pub.cfm?id=16404&lid=3 .